Abstract
Insufficient sleep is a common occurrence in occupational settings (e.g. doctors, drivers, soldiers). The resulting sleep debt can lead to daytime sleepiness, fatigue, mood disorder, and cognitive deficits as well as altered vascular, immune and inflammatory responses. Short daytime naps have been shown to be effective at counteracting negative outcomes related to sleep debt with positive effects on daytime sleepiness and performance after a normal or restricted night of sleep in laboratory settings. However, the environmental settings in the workplace and the emotional state of workers are generally not conducive to beneficial effects. Here, we tested whether relaxation techniques (RT) involving hypnosis might increase total sleep time (TST) and/or deepen sleep. In this study, eleven volunteers (aged 37–52) took six early-afternoon naps (30 min) in their occupational workplace, under two different conditions: control ‘Naps’ or ‘Naps + RT’ with a within-subjects design. Our results demonstrate that adding RT to naps changes sleep architecture, with a significant increase in the TST, mostly due to N2 sleep stage (and N3, to a lesser extent). Therefore, the deepening of short naps with RT involving hypnosis might be a successful non-pharmacological way to extend sleep duration and to deepen sleep in occupational settings.
Keywords: Short napping, Relaxation, Hypnosis, Military setting, Sleep characteristics, EEG recording
Introduction
In western countries, sleep debt is frequently seen in professionally active populations (e.g. health care professions, drivers, soldiers)1,2,3,4). Consequences of this include daytime sleepiness, fatigue, mood disorder, and cognitive deficits, as well as altered vascular, immune and inflammatory responses5, 6). Such alterations of physiological responses related to sleep loss are associated with several major diseases including hypertension, cardiovascular disease, obesity, anxiety, depression, and bipolar disorders7, 8). One recent study, highlighting sleep as a target in mental health prevention programs in the workplace, reported that the sleep debt induced by insomnia in financial workers can be considered as a relevant clinical marker for occupational burnout9).
Napping seems to be an efficient way to counteract sleep loss effects on health, as well as a means to sustain alertness during an otherwise sleepless period10,11,12,13,14). In particular, short daytime naps of less than 30 min, which rarely contain non-REM sleep 3 (N3), have been shown to have positive effects on daytime alertness and/or performance after a normal night of sleep in young15, 16) and elderly individuals17), and after a night of restricted sleep18, 19). Specifically, a short nap of less than 30 min post-lunch (12:30 p.m.) or mid-afternoon (2:00 p.m.) has been shown to have positive effects on performance and self-confidence in university students, after a night’s sleep of 8 h20). In young subjects, Hayashi et al. demonstrated that non-REM sleep 2 (N2) during daytime naps has a recuperative power on subjective alertness and cognitive performance, while these effects are limited in non-REM stage 1 (N1) sleep21). Another study followed non-shift workers in a real work setting for three weeks, demonstrating that a 15-min post-lunch nap can significantly promote alertness in the afternoon, and particularly at the end of the week16).
Despite these findings, the environmental settings in the workplace (e.g. noise, heat, discomfort) and the emotional state of workers (or even their ability to nap) are not always conducive to a beneficial nap22). Due to these stated difficulties with napping, sleep onset may be delayed, thus reducing total sleep time (TST) and time spent in deeper sleep stages. Several studies have thus combined countermeasures aimed at enhancing and sustaining worker alertness in occupational settings, by improving sleep during naps and optimizing alertness upon awakening11).
A short daytime nap has been shown to have positive effects on the decline in mid-afternoon alertness, and the effects of such a nap can be enhanced by caffeine intake before napping, by exposure to bright light, or even by face-washing immediately after waking from a nap23). Furthermore, it was previously shown that flow scores assessing a positive emotional state at work become higher after a short (20-min) afternoon nap and under bright light exposure (>2,000 lux) during a contextual cueing task in healthy subjects24). Hypnotic suggestion, music, and progressive muscle relaxation techniques have also been found to improve objective and subjective sleep efficiency in young and middle-aged (mean=47 yr old) healthy women25, 26), as well as in posttraumatic stress disorder patients27).
The US and French Army medical departments have emphasized the need to include sleep education and management, which may help on-duty soldiers develop appropriate sleep practices as well as improve sleep during deployment, in order to directly improve operational readiness28, 29).
In the French armed forces, a set of techniques referred to Mental Skill Training (MST) is taught to improve and/or mobilize psycho-cognitive, emotional and behavioral skills, particularly during operations to ensure optimum performance30). These techniques encompass positive reinforcement, mental imagery, mental revitalization and muscle relaxation30). Despite the largely accepted benefits of these techniques in the military field, no study has yet investigated the effect of these techniques in sleep improvement. In the present study, we tested whether relaxation techniques involving hypnosis (as part of MST) could be effective in objectively improving the duration of TST and sleep stages during short early-afternoon naps in middle-aged military volunteers, in an occupational context. We hypothesized that RT, apart from lengthening sleep, may also change nap quality21). This study aims to provide new insight into simple methods that could improve napping in occupational and operational settings.
Subjects and Methods
Subjects
Eleven subjects (9 men and 2 women, aged 37–52) were recruited from the National Center for Military Sports (Centre national des sports de la défense, Fontainebleau, France). Subjects included both military enlisted personnel ranging in grade from OF-3 to OR-3 and civilian administrative personnel. For inclusion in this study, subjects were required to be 35–55 yr old, good sleepers, healthy, and non-habitual nappers. These requirements were made in order to be representative of the general worker population, but also to avoid any variability due to age by including younger participants. Routine questionnaires were performed to rule out medical conditions including sleep disorders. None of the subjects had participated in any shiftwork or had travelled across more than one time zone within the previous 4 wk. Subjects were asked to refrain from caffeine and alcohol during experiment days. One week prior to the first nap and during the whole experiment, subjects were asked to maintain regular sleep and awake patterns, with a daily nocturnal sleep of 7 h and “lights off” between 10 p.m. and midnight. Daily sleep and wakefulness data were assessed by a sleep diary and actimetry (Actiwatch AW7, CamNtech Ltd.; Cambridge, UK) one week prior to each condition and during experiment days. Subjects averaged a daily sleep time of 7.1 ± 1.3 h one week prior to and during the ‘Naps’ condition; average daily sleep time was 6.9 ± 1.1 h one week prior to and during the ‘Naps + RT’ condition. There was no statistical difference in TST at night between the two conditions.
All procedures were in accordance with the Declaration of Helsinki, and the study was approved by the ethical medical committee of the National Center for Military Sports. Subjects gave informed written consent before participating in the experiment.
Procedure
The cross-over protocol included six naps per subject in their occupational work place during weekdays. Naps were taken under two different conditions: 3 “control naps” (Naps) and 3 “naps with relaxation techniques (RT)” (Naps + RT). In the ‘Naps + RT’ condition, a military instructor who had received full training in hypnosis, relaxation techniques and mental skill training administered relaxation techniques during the whole nap duration30, 31). These techniques involved hypnosis, progressive muscle relaxation and paradoxical interventions; the latter is a therapeutic technique that uses contradictory instructions such as “Please try and stay awake for as long as possible rather than, please try and fall asleep as quickly as possible”31, 32). These techniques are part of the MST developed by the French armed forces and utilized since 1993.
All naps took place on the same days of the week (Tuesday, Wednesday, and Thursday). The 3 control ‘Naps’ occurred first, followed by a wash out period of one month and then 3 ‘Naps + RT’. This order was chosen by the study team because of the risk of self-application of RT during control naps if they occurred second in the order.
The naps were deliberately scheduled in a non-optimal environment for sleeping. Specifically, naps took place in a collective room on gym mats under natural daylight. The room was adjacent to a gymnasium where ball sports were played every day. Subjects were asked to arrive at 1:00 p.m. to prepare for the electroencephalography (EEG) hookup. Nap opportunities began at 1:30 p.m., when subjects were asked to lie down and rest next to the instructor. Naps ended 30 min later, at 2:00 p.m. The subjects were instructed to blink 5 times when they were authorized to nap, and to blink again 5 times when they heard the signal to wake up, in order to have objective triggers of the exact beginning and end of the nap. The sleep opportunity, referred here to the time in bed (TIB) was based on the time between the 5 blinks at the beginning and end of the nap. This resulted in a slight difference in TIB between subjects, depending on the time it took to become aware of the end signal. To assess subjective sleepiness, subjects were asked to fill out the Karolinska Sleepiness Scale (KSS)33) questionnaire prior to being hooked up for EEG and 15 min after awakening.
Materials
Polysomnography (PSG) recordings were obtained using a miniaturized EEG setup (Actiwave, CamNtech Ltd.; Cambridge, UK) including 3 EEG channels (F3, C3, O1) referenced to M234), as well as one electrooculogram (EOG), two electromyogram (EMG) and two electrocardiogram (ECG) channels. Ag-AgCl electrodes were used, and impedances were kept below 5 kΩ for EEG electrodes and below 10 kΩ for EOG and EMG electrodes. Signals were sampled at 128 Hz and filtered between 0.3 and 70 Hz. PSG recordings were scored by two trained sleep researchers in accordance with the American Academy of Sleep Medicine (AASM) criteria using the SOMNOLOGICA software (TM, Medcare; Reykjavik, Iceland)35). Sleep parameters such as TST, sleep onset latency (SOL; defined by three continuous epochs of N1 or the occurrence of one epoch of N2), the duration of wakefulness after sleep onset (WASO) and each sleep stage (rapid eye movement or REM sleep, N1 sleep, N2 sleep, and N3 sleep) were automatically provided by SOMNOLOGICA after scoring. The sleep efficiency (SE) was calculated as follows: [(TST/Time in bed) × 100].
Statistical analyses were performed using R 2.14.0 software. Data were analyzed using the non-parametric Wilcoxon test with a within-subject design. For each subject, the sleep parameters of the three naps were pooled together across days within each condition. Data were then averaged across all subjects and compared by condition. All data are expressed as means ± standard deviation, and p values<0.05 were considered as statistically significant.
Results
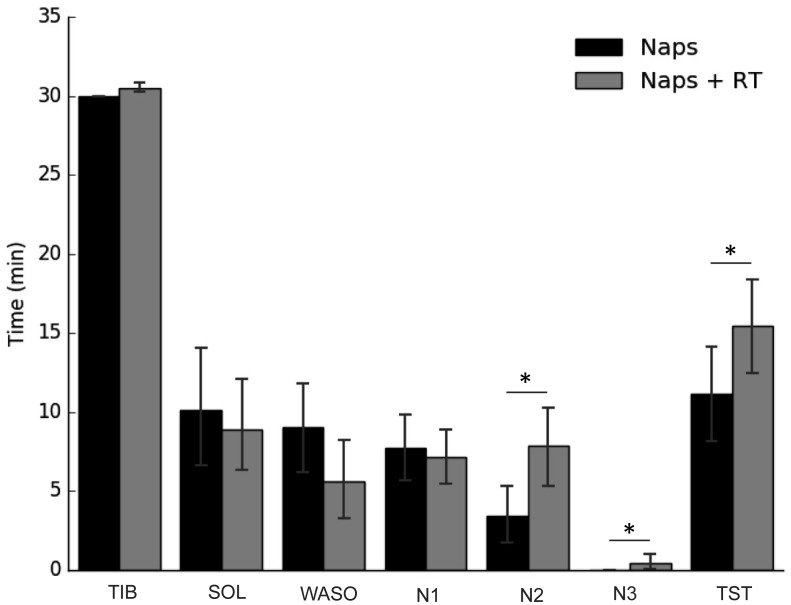
The TIB did not differ between the nap conditions. Nap sleep architecture included N1, N2, and N3. Because no REM sleep occurred in any of the conditions, REM could not be represented in any of the figures or tables. TST (p<0.01) and the durations of N2 (p<0.01) and N3 (p<0.05) were significantly increased when naps included RT, in comparison to the control naps. The SE (34.54 ± 23.70 for the ‘Naps’ condition and 49.76 ± 20.95 for the ‘Naps + RT’ condition) increased significantly by 44%. No differences were observed regarding sleep latency, WASO, or N1 duration (Fig. 1).
Fig. 1.
Sleep characteristics in the Naps and Naps + RT conditions. Time in bed (TIB), Sleep onset latency (SOL), Wake after sleep onset (WASO), N1, N2, N3, and total sleep time (TST) in Naps (■) and Naps + RT (relaxation techniques) (■). Results are expressed as the mean of the 3 naps opportunities averaged by subject and then averaged across all subjects ± standard deviation in minutes (min).
*p<0.05 (For a comparison between the two conditions).
To assess a possible order effect of the nap, we compared the sleep architecture of each nap in the RT condition to the related control nap (i.e. the first control nap with the first RT nap) (Table 1). SOL was significantly reduced only in the first nap of the ‘Naps + RT’ condition, as compared to the control nap. In the ‘Naps + RT’ condition, the TST and the time spent in N2 were significantly higher than during the control condition for the three naps. While no N3 was observed in any control naps, the ‘Naps + RT’ condition significantly increased N3 in the first nap only. Surprisingly, whereas N1 was significantly higher in the first two naps of ‘Naps + RT’ as compared to the controls, it was lower in the third nap. This change in sleep architecture in the third nap of the ‘Naps + RT’ condition could be explained by a considerable increase in N2.
Table 1. Sleep characteristics of each naps in the Naps and Naps + RT conditions.
| Naps | Naps + RT | |||||
|---|---|---|---|---|---|---|
| Nap 1 | Nap 2 | Nap 3 | Nap 1 | Nap 2 | Nap 3 | |
| TIB (min) | 30.00 ± 0.00 | 30.0 ± 0.00 | 30.0± 0.00 | 30.00 ± 0.00 | 27.67. ± 0.4 | 31.75 ± 0.1 |
| SOL (min) | 15.35 ± 12.05 | 7.70 ± 8.56 | 6.70 ± 8.15 | 7.75 ± 8.75* | 7.11 ± 6.04 | 11.65 ± 7.62 |
| TST (min) | 10.15 ± 9.49 | 11.65 ± 7.86 | 12.55 ± 7.09 | 15.30 ± 7.79* | 16.72± 5.60* | 14.50 ± 9.14* |
| SE [TST (% of TIB)] | 33.83 ± 31.62 | 38.83 ± 26.18 | 41.83 ± 23.63 | 50.61 ± 25.43* | 55.74± 18.68* | 45.19 ± 28.36* |
| WASO (min) | 4.50 ± 6.66 | 10.65 ± 6.92 | 11.75 ± 7.27 | 7.25 ± 6.38 | 3.83 ± 8.89* | 5.60 ± 5.13* |
| WASO (% of TIB) | 16.67 ± 22.81 | 34.63 ± 24.18 | 37.50 ± 26.30 | 24.12 ± 21.29 | 12.78 ± 29.62* | 17.72 ± 16.37* |
| N1 (min) | 6.65 ± 6.57 | 8.45 ± 5.32 | 9.35 ± 5.52 | 8.15 ± 6.46* | 8.78± 2.91* | 4.65 ± 3.82* |
| N1 (% of TIB) | 22.17 ± 21.90 | 28.17 ± 17.74 | 31.17 ± 18.40 | 27.13 ± 21.59* | 29.26± 9.69* | 14.51 ± 11.85* |
| N2 (min) | 3.50 ± 4.67 | 3.20 ± 5.21 | 3.20 ± 4.85 | 6.40 ± 0.75* | 7.89± 6.65* | 9.30± 7.12* |
| N2 (% of TIB) | 11.67 ± 15.58 | 10.67 ± 16.6 | 10.67 ± 16.16 | 21.07 ± 17.54* | 26.30± 22.18* | 28.96± 22.25* |
| N3 (min) | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.75 ± 1.72* | 0.06 ± 0.16 | 0.55 ± 1.15 |
| N3 (% of TIB) | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | 2.41 ± 5.46* | 0.19 ± 0.52 | 1.72 ± 3.59 |
Sleep opportunity referred to the TIB: time in bed; SOL: Sleep onset latency; TST: Total sleep time; SE: Sleep efficiency; WASO: Wake after sleep onset, N1, N2, N3, and REM. Results are expressed as the mean ± standard deviation in minutes (min) or in percentage of the sleep opportunity (% of Sop).
*p<0.05 (For a comparison between conditions).
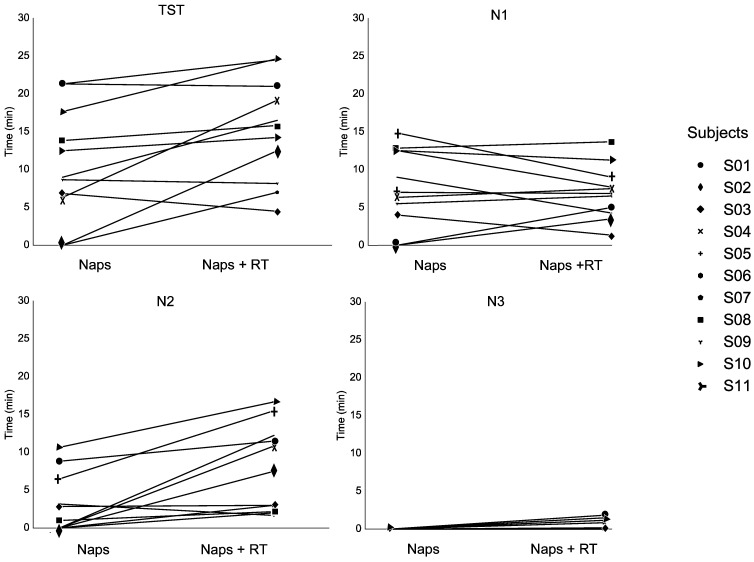
In order to examine the possibility of inter-individual variability in the sleep response, we compared sleep characteristics of each subject in the ‘Naps’ and ‘Naps + RT’ conditions (Fig. 2). TST was increased in 8 out of 11 subjects, and the time spent in N1, N2 and N3 was increased in 6 subjects, 9 subjects, and 5 subjects, respectively.
Fig. 2.
Individual sleep characteristics in the Naps and Naps + RT conditions.
Average Total sleep time (TST), N1, N2, and N3 (in min).
Overall, subjective sleepiness (pre-to-post KSS scores) following the two nap conditions was not significantly different, although a non-significant trend towards improved sleepiness was observed (Table 2) (p=0.055). Both the pre-KSS scores and the post-KSS scores were significantly different between conditions.
Table 2. Subjective sleepiness prior napping (pre KSS), after napping (post KSS) and the difference between the pre- and the post KSS (KSS Change) in the Naps and Naps + RT (relaxation techniques) conditions.
| Naps | Naps + RT | |
|---|---|---|
| Pre KSS | 4.70 ± 1.19 | 3.81 ± 1.26* |
| Post KSS | 4.47 ± 1.70 | 3.45 ± 1.40* |
| KSS Change | −0.21 ± 1.99 | −0.36 ± 1.88 |
The Karolinska Sleepiness Scale is scored as follows: 1. Extremely alert, 2. Very alert, 3. Alert, 4. Rather alert, 5. Neither alert nor sleepy, 6. Some signs of sleepiness, 7. Sleepy, but no difficulty remaining awake, 8. Sleepy, some effort to keep alert, 9. Extremely sleepy, fighting sleep. 1 to 6 are usually referred as active states, 7 to 9 as sleepy states.
*p<0.05 (For a comparison between the two conditions).
Discussion
In the present study, we evaluated the effectiveness of adding RT to an afternoon nap opportunity for its usefulness in optimizing sleep during napping in the work place. Indeed, many laboratory-based studies have shown that short daytime naps have positive effects on wakefulness, performance, and self-confidence in individual task performance even after sufficient sleep duration, which could be advantageous in real work situations10, 15, 16, 20). Our results show that the sleep duration and architecture of a short early-afternoon nap can be optimized by RT involving hypnosis among middle-aged volunteers in an occupational setting. Indeed, naps associated with RT led to a significant increase in TST duration, mostly due to N2 (and N3, to a lesser extent). This is particularly interesting, since it has been demonstrated that N2 plays an important role in the restorative function of sleep, and that only 3 min of N2 can lead to significant recuperative effects on daytime alertness and performance in young subjects after a slightly restricted night (1.5 h less than typical nocturnal sleep), whereas these effects are limited in N121).
One study of young women revealed a strong increase in N3 percentage during a nap following 13 min of hypnotic suggestions in comparison to a control condition, with no changes in the percentage of the N1, N2, or REM sleep stages25). The percentage of time awake after sleep onset was marginally reduced after the hypnosis condition, and total sleep time did not differ. In a subsequent study in elderly women, the increase in N3 after hypnotic suggestions was considered to be due to the suggestion’s effect to sleep deeper; however, the authors emphasized that they cannot rule out the possibility of a relaxing effect of the hypnotic test26), whereas their previous experimental protocol in young women25) allowed exclusion of the relaxing effect. Compared to the young population in Cordi et al.25), the results of our present study revealed significant increases in both SE and TST (mostly due to N2 sleep and N3 to a lesser extent) in the ‘Naps + RT’ condition as compared to the control naps, probably due to our decision to limit the nap duration to 30 min. The considerable time devoted to naps and previous hypnosis (90 min) in the protocol from Cordi et al.25) makes its implementation difficult under working conditions.
In our study, we cannot dismiss the idea that relaxation per se could lengthen an afternoon nap and deepen it directly by increasing the N2 and N3 durations. We gave a combined RT + hypnosis intervention and thus we cannot differentiate the relative effects on nap sleep caused by hypnosis versus the other relaxation techniques given during the nap. Progressive muscular relaxation reduces anxiety and depression, improves sleep quality, alleviates fatigue, and reduces pain27, 36). Recently, functional magnetic resonance imaging was used to show that progressive muscular relaxation can also potentially reduce brain activity in healthy adult men37). Specifically, brain activity changed only in small parts of the cerebral cortex and limbic system during the progressive muscular relaxation session, while it increased throughout the cerebral cortex, limbic system, and basal ganglia in the control session (consisting of simple skeletal muscle exercises). The authors conclude that progressive muscular relaxation may be able to induce a cerebral state appropriate for relaxation, concentration, and resistance to local environmental distractions.
Our results also highlight inter-individual response differences to this technique, since not all subjects responded to the relaxation techniques. These findings emphasize the two studies by Cordi et al., in which it was found that 13 min of hypnotic suggestions to “sleep deeper” prior to a midday 77-min nap specifically increased the duration and power of SWS in both young25) and elderly healthy suggestible women26), but failed to do so in marginally suggestible subjects. The fact that more than two-thirds of our subjects had longer and deeper naps in this study is encouraging, since suggestibility was not a selection criterion. Here, non-responders tended to be subjects with a high sleep time in the ‘control naps’ condition, suggesting a ceiling effect with this parameter. Therefore, the technique that we used appears to be most effective in subjects with lower TST during naps.
The absence of improvement in subjective sleepiness may be explained by the lack of sleepiness reported prior to naps; therefore, it is likely that this ceiling effect limited our ability to detect differences. In spite of this, we observed prior to the nap that subjective somnolence was significantly lower in the ‘Naps + RT’ condition in comparison to the ‘Naps’ condition, which does not prevent the ceiling effect from being present. Overall, our results reveal that RT as developed by the French military MST program might lengthen and deepen sleep during a short nap opportunity in an occupational setting. However, the 30-min sleep opportunity should be supervised, since deepening N3 sleep is associated with the risk of higher sleep inertia if awakened from this stage. This particularly concerns operational risks in the work place, as 20–30 min is the time needed to exit sleep inertia38, 39). Therefore, it would be interesting to energize the awakening after a nap by using countermeasures of sleep inertia (such as bright light exposure or face-washing) immediately after napping, or caffeine before napping, as previously described23).
In summary, our results indicate that relaxation techniques appear to be effective for improving nap architecture and duration in the workplace, although this study should be replicated with more subjects. These studies can be expanded to evaluate the role of RT in the prevention or management of professional burnout, which is another occupational risk associated with anxiety and sleep disorders. Finally, future studies should include cognitive tasks and biomarkers in order to verify whether this afternoon nap optimization could provide better restorative functions than a standard nap.
Funding
Research support was provided by the French General Directorate for Armament (DGA, Ministry of Defense), contract number: PDH-1-SMO-2-510. ED is supported by the ANRT CIFRE DGA PhD funding (002/2015/DGA).
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgments
We thank all subjects for their contribution to this work and Marine Herbo for technical assistance. The author contributions are as follows: ED, MC, AR, and EPP conceived and designed the study. ED, AR, ME, RD, MG, AP, and LR acquired the data. ED and FS analyzed the data. ED interpreted the data. ED and DGM wrote the manuscript. MC, DGM, AR, and DL revised the manuscript.
References
- 1.Åkerstedt T, Wright KP., Jr2009) Sleep loss and fatigue in shift work and shift work disorder. Sleep Med Clin 4, 257–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peterson AL, Goodie JL, Satterfield WA, Brim WL. (2008) Sleep disturbance during military deployment. Mil Med 173, 230–5. [DOI] [PubMed] [Google Scholar]
- 3.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. (2010) Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep 33, 585–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barthe B, Tirilly G, Gentil C, Toupin C. (2016) Job demands and resting and napping opportunities for nurses during night shifts: impact on sleepiness and self-evaluated quality of healthcare. Ind Health 54, 157–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rabat A, Gomez-Merino D, Roca-Paixao L, Bougard C, Van Beers P, Dispersyn G, Guillard M, Bourrilhon C, Drogou C, Arnal PJ, Sauvet F, Leger D, Chennaoui M. (2016) Differential kinetics in alteration and recovery of cognitive processes from a chronic sleep restriction in young healthy men. Front Behav Neurosci 10, 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Faraut B, Nakib S, Drogou C, Elbaz M, Sauvet F, De Bandt JP, Léger D. (2015) Napping reverses the salivary interleukin-6 and urinary norepinephrine changes induced by sleep restriction. J Clin Endocrinol Metab 100, E416–26. [DOI] [PubMed] [Google Scholar]
- 7.Mullington JM, Simpson NS, Meier-Ewert HK, Haack M. (2010) Sleep loss and inflammation. Best Pract Res Clin Endocrinol Metab 24, 775–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bayon V, Leger D, Gomez-Merino D, Vecchierini MF, Chennaoui M. (2014) Sleep debt and obesity. Ann Med 46, 264–72. [DOI] [PubMed] [Google Scholar]
- 9.Metlaine A, Sauvet F, Gomez-Merino D, Elbaz M, Delafosse JY, Leger D, Chennaoui M. (2017) Association between insomnia symptoms, job strain and burnout syndrome: a cross-sectional survey of 1300 financial workers. BMJ Open 7, e012816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Takahashi M. (2003) The role of prescribed napping in sleep medicine. Sleep Med Rev 7, 227–35. [DOI] [PubMed] [Google Scholar]
- 11.Bonnefond A, Tassi P, Roge J, Muzet A. (2004) A critical review of techniques aiming at enhancing and sustaining worker’s alertness during the night shift. Ind Health 42, 1–14. [DOI] [PubMed] [Google Scholar]
- 12.Milner CE, Cote KA. (2009) Benefits of napping in healthy adults: impact of nap length, time of day, age, and experience with napping. J Sleep Res 18, 272–81. [DOI] [PubMed] [Google Scholar]
- 13.Faraut B, Boudjeltia KZ, Dyzma M, Rousseau A, David E, Stenuit P, Franck T, Van Antwerpen P, Vanhaeverbeek M, Kerkhofs M. (2011) Benefits of napping and an extended duration of recovery sleep on alertness and immune cells after acute sleep restriction. Brain Behav Immun 25, 16–24. [DOI] [PubMed] [Google Scholar]
- 14.Oriyama S, Miyakoshi Y, Kobayashi T. (2014) Effects of two 15-min naps on the subjective sleepiness, fatigue and heart rate variability of night shift nurses. Ind Health 52, 25–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Takahashi M, Fukuda H, Arito H. (1998) Brief naps during post-lunch rest: effects on alertness, performance, and autonomic balance. Eur J Appl Physiol Occup Physiol 78, 93–8. [DOI] [PubMed] [Google Scholar]
- 16.Takahashi M, Nakata A, Haratani T, Ogawa Y, Arito H. (2004) Post-lunch nap as a worksite intervention to promote alertness on the job. Ergonomics 47, 1003–13. [DOI] [PubMed] [Google Scholar]
- 17.Tamaki M, Shirota A, Hayashi M, Hori T. (2000) Restorative effects of a short afternoon nap (<30 min) in the elderly on subjective mood, performance and eeg activity. Sleep Res Online 3, 131–9. [PubMed] [Google Scholar]
- 18.Gillberg M, Kecklund G, Axelsson J, Akerstedt T. (1996) The effects of a short daytime nap after restricted night sleep. Sleep 19, 570–5. [DOI] [PubMed] [Google Scholar]
- 19.Brooks A, Lack L. (2006) A brief afternoon nap following nocturnal sleep restriction: which nap duration is most recuperative? Sleep 29, 831–40. [DOI] [PubMed] [Google Scholar]
- 20.Hayashi M, Watanabe M, Hori T. (1999) The effects of a 20 min nap in the mid-afternoon on mood, performance and EEG activity. Clin Neurophysiol 110, 272–9. [DOI] [PubMed] [Google Scholar]
- 21.Hayashi M, Motoyoshi N, Hori T. (2005) Recuperative power of a short daytime nap with or without stage 2 sleep. Sleep 28, 829–36. [PubMed] [Google Scholar]
- 22.Faraut B, Andrillon T, Vecchierini MF, Leger D. (2017) Napping: a public health issue. From epidemiological to laboratory studies. Sleep Med Rev 35, 85–100. [DOI] [PubMed] [Google Scholar]
- 23.Hayashi M, Masuda A, Hori T. (2003) The alerting effects of caffeine, bright light and face washing after a short daytime nap. Clin Neurophysiol 114, 2268–78. [DOI] [PubMed] [Google Scholar]
- 24.Kaida K, Takeda Y, Tsuzuki K. (2012) The relationship between flow, sleepiness and cognitive performance: the effects of short afternoon nap and bright light exposure. Ind Health 50, 189–96. [DOI] [PubMed] [Google Scholar]
- 25.Cordi MJ, Schlarb AA, Rasch B. (2014) Deepening sleep by hypnotic suggestion. Sleep 37, 1143–52, 1152A–1152F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cordi MJ, Hirsiger S, Mérillat S, Rasch B. (2015) Improving sleep and cognition by hypnotic suggestion in the elderly. Neuropsychologia 69, 176–82. [DOI] [PubMed] [Google Scholar]
- 27.Blanaru M, Bloch B, Vadas L, Arnon Z, Ziv N, Kremer I, Haimov I. (2012) The effects of music relaxation and muscle relaxation techniques on sleep quality and emotional measures among individuals with posttraumatic stress disorder. Ment Illn 4, e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sauvet F, Drogou C, Bougard C, Arnal PJ, Dispersyn G, Bourrilhon C, Rabat A, Van Beers P, Gomez-Merino D, Faraut B, Leger D, Chennaoui M. (2015) Vascular response to 1 week of sleep restriction in healthy subjects. A metabolic response? Int J Cardiol 190, 246–55. [DOI] [PubMed] [Google Scholar]
- 29.Mysliwiec V, Walter RJ, Collen J, Wesensten N. (2016) Military sleep management: an operational imperative. US Army Med Dep J 2, 128–34. [PubMed] [Google Scholar]
- 30.Perreaut-Pierre E .(2012) Comprendre et pratiquer les Techniques d’Optimisation, 2nd Ed. InterEditions. [Google Scholar]
- 31.Jacobson E .(1938) Progressive relaxation, Chicago, University of Chicago Press; You must relax, 1942, McGraw Hill Book Company, New York. [Google Scholar]
- 32.Espie CA, Lindsay WR. (1985) Paradoxical intention in the treatment of chronic insomnia: six case studies illustrating variability in therapeutic response. Behav Res Ther 23, 703–9. [DOI] [PubMed] [Google Scholar]
- 33.Åkerstedt T, Gillberg M. (1990) Subjective and objective sleepiness in the active individual. Int J Neurosci 52, 29–37. [DOI] [PubMed] [Google Scholar]
- 34.Sauvet F, Bougard C, Coroenne M, Lely L, Van Beers P, Elbaz M, Guillard M, Leger D, Chennaoui M. (2014) In-flight automatic detection of vigilance states using a single EEG channel. IEEE Trans Biomed Eng 61, 2840–7. [DOI] [PubMed] [Google Scholar]
- 35.Iber C, Ancoli-Israel S, Chesson A, Quan S .(2007) The AASM Manual for the Scoring of Sleep and Associates Events: Rules, Terminology and Technical Specifications.: American Academy of Sleep Medicine, Westchester. [Google Scholar]
- 36.Davis M, Robbins Eshelman E, McKay M. (1988) The Relaxation and Stress Reduction Workbook. Nature, 312–312. [Google Scholar]
- 37.Kobayashi S, Koitabashi K. (2016) Effects of progressive muscle relaxation on cerebral activity: an fMRI investigation. Complement Ther Med 26, 33–9. [DOI] [PubMed] [Google Scholar]
- 38.Ferrara M, De Gennaro L. (2000) The sleep inertia phenomenon during the sleep-wake transition: theoretical and operational issues. Aviat Space Environ Med 71, 843–8. [PubMed] [Google Scholar]
- 39.Tassi P, Muzet A. (2000) Sleep inertia. Sleep Med Rev 4, 341–53. [DOI] [PubMed] [Google Scholar]