Abstract
This study investigated the usefulness of continuous sensor data for improving occupational cold stress assessment. Eleven volunteer male subjects completed a 90–120-min protocol in cold environments, consisting of rest, moderate and hard work. Biomedical data were measured using a smart jacket with integrated temperature, humidity and activity sensors, in addition to a custom-made sensor belt worn around the chest. Other relevant sensor data were measured using commercially available sensors. The study aimed to improve decision support for workers in cold climates, by taking advantage of the information provided by data from the rapidly growing market of wearable sensors. Important findings were that the subjective thermal sensation did not correspond to the measured absolute skin temperature and that large differences were observed in both metabolic energy production and skin temperatures under identical exposure conditions. Temperature, humidity, activity and heart rate were found to be relevant parameters for cold stress assessment, and the locations of the sensors in the prototype jacket were adequate. The study reveals the need for cold stress assessment and indicates that a generalised approached is not sufficient to assess the stress on an individual level.
Keywords: Cold stress, Decision support, Wearable sensors, IREQ, Occupational health
Introduction
Outdoor workers in circumpolar areas are often exposed to harsh and extreme environments, especially during the winter months. Cold exposure challenges human heat balance and requires steps to be taken to control heat loss1). In addition to low ambient temperatures, workers in circumpolar areas are exposed to darkness, ice and snow, all of which increase the risk of accidents2). Skin cooling can lead to discomfort, which can affect arousal, vigilance and concentration3). The extremities experience more profound cooling than the torso, which may impair their function, and hands and fingers in particular are vulnerable to cooling2, 4). A review by Heus et al.5), found a reduction in manual performance at a finger skin temperature of 20–22°C, and a strong decrease at finger skin temperature of 15–16°C. A finger skin temperature of 15°C or below is therefore regarded as a critical threshold value, at which important loss of dexterity occurs. Furthermore, cold feet can affect both balance and locomotion, and thereby increase the risk of falling1). A low skin temperature causes pain, numbness and may lead to local frostbite1). Whole-body cooling is a more severe condition that may result in significant reductions in mental and physical performance, ultimately ending up in increased risk of death from hypothermia after long exposure, although this is unlikely to occur in normal occupational settings6).
Today, several international standards address cold risk assessment in occupational settings. With regards to physiological measurements and thermal stress, ISO 98867), ISO 89968) and ASTM F2732-169) describe methods for valid and reliable measurements. ISO 1574310) addresses cold stress from a risk management point of view, and presents a systematic approach to the evaluation and possible solution of challenges related to cold stress on a workplace. Protective clothing is our first line of defence against the cold environments. ISO 1107911) and ISO 992012) provides valuable insights into clothing and the required clothing insulation for different environmental exposures. Various indices for cold stress are described in the literature, of which Wind Chill Temperature (WCT) and Required Clothing Insulation (IREQ) are the most often used13); these are also central to ISO 11079. The WCT is based on a calculated air temperature that, in the absence of wind, would result in the same skin surface heat loss to the environment as in the actual windy environment14). IREQ15) is a model that calculates the clothing that would be needed to maintain body heat balance, and is based on measurements of air temperature, mean radiant temperature, humidity and air velocity and measurements or estimates of activity level (energy metabolism). IREQ is based on average values for an eight-hour work period, and includes both work intensity and environmental exposure. IREQ thus provides a good description of average exposure but do not take short time exposures and variations in work intensity into account. Once the insulation value of the clothing and work intensity are known, the IREQ model can be used to calculate the recommended maximum duration of cold exposure (Duration of Limited Exposure: DLE) at different ambient temperatures.
When work intensity (metabolic energy production) increases, the cold stress can be tolerated for a longer period and DLE is extended. Traditionally, work intensity has been estimated using standard tables8) and then further establishing average values for the whole eight-hour work shift. However, wide variations in work intensity are normal in the course of a working day, and using average values will lead to a less reliable and valid description of the potential cold stress of individual workers. Additional factors such as fitness level, gender and body composition would introduce even more errors into estimates of cold stress. Local cooling of extremities that are often the limiting factor for cold stress in occupational settings4, 5) is not covered by the IREQ, and individual variations are even larger than for general cooling. WCT describes the risk for frostbite of exposed skin and does not take covered skin into account.
This study aims to contribute to improved occupational safety through continuous real-time personal cold stress assessment. Today’s international standards for occupational cold stress assessment are based on average values. Our hypotheses are that this limits the accuracy of risk assessment; that differences in physiology, experience, knowledge and resilience will vary between the workers, and that information available from the rapidly growing market of wearable sensors can be used to assess both general and local cooling with greater accuracy than current standards. It would therefore be valuable to develop a system capable of providing relevant real-time information for cold stress assessment. We have already16) demonstrated that sensors integrated into clothing can provide easy accessible information about both the wearer and work-site environmental conditions. Even though occupational thermal stress is an area in which extensive work has already been done4, 15, 17), to the best of our knowledge no studies have employed unobtrusive sensor systems, capable of providing a continuous evaluation of cold stress for decision support in ordinary daily work. The main objective of the present study was to justify the need for such a personalised system and to evaluate the applicability and relevance of suitable sensors and sensor locations to provide a valid estimate of general and local cooling of individual workers.
Subjects and Methods
Test subjects
Eleven male volunteers (age=24.8 ± 2.4 yr, height=181 ± 4 cm, mass=76.2 ± 6.7 kg, BMI=23.3 ± 2) participated in the study. The subjects had been informed of the aims of the project and had provided written consent. The study was performed according to the Helsinki Declaration and reported to the Norwegian Centre for Research Data. All subjects underwent a medical examination before they enrolled in the study. Inclusion criteria were; healthy male, between 170–190 cm, and 65–90 kg. Exclusion criteria were earlier cold-related injuries or Raynaud’s syndrome.
Experimental protocol
The tests were performed in a controlled-climate chamber set to −20 ± 0.2°C and wind speed 3 m·s−1, with a protocol consisting of moderate (walking on a treadmill at 5 km·h−1 and incline 0%) and hard work (walking at 5 km·h−1 and incline 5%) plus a rest period standing at the treadmill at the end (Table 1). The subjects walked with the wind in their back. The absolute termination criterion was set to a skin temperature of less than 8°C. All together 12 tests were executed. Different subjects were used in all tests except 3 and 9 where the same person was used for both protocols. In tests 1–6 the length of each work period was 30 min, and the total length of the test was 90 min. The subjects were dressed in wool underwear, with a wool jacket as middle layer. The outer layer consisted of a wind and waterproof pant and an insulated winter jacket. Head, hands and feet were dressed in wool balaclava, wool mittens and winter boots with wool socks, respectively. The subjects were allowed to move their fingers and clench their fists in order to keep their hands warm. During tests 7–12 the aim was to reach a lower finger temperature and the subjects were instructed not to move their fingers or clench their fists. The length of the rest period was increased to 60 min (or until the termination criterion was met). The maximum length of test was 120 min.
Table 1. Experimental protocol for the treadmill walking test in the climate chamber. For the second half of subjects the rest period at the end was prolonged from 30 to 60 min, or until the termination criteria of any skin temperature less than 8 °C was met.
| Work intensity | Wind and ambient temperature | Treadmill settings | Duration of work intensity | Total time in test | ||
|---|---|---|---|---|---|---|
| (m·s−1) | (°C) | Speed (km·h−1) | Incline (%) | (Min) | (Min) | |
| Moderate | 3 | −20 | 5 | 0 | 30 | 30 |
| Hard | 3 | −20 | 5 | 5 | 30 | 60 |
| Rest (Standing) | 3 | −20 | 0 | 0 | Test 1–6: 30 | 90 |
| Test 7–12: 60* | ≤120 | |||||
*or termination criterion (skin temperature less than 8 °C) met.
Equipment
Biomedical data were measured using a smart jacket with integrated sensors (skin temperature and movement data on the hand, temperature and humidity outside and inside the jacket)16, 18) in addition to a custom-made sensor belt (heart rate, skin temperature, air humidity and temperature on the chest/back)19). For reference, distributed skin temperature and environmental temperature and humidity were measured using commercially available reference sensors. All the sensors are listed in Table 2.
Table 2. Overview of the parameters measured by different sensors in the test.
| Parameter | Sensor type | Location | Measurement frequency |
|---|---|---|---|
| Heart Rate (HR) | 1 lead ECG, in pulse belt custom-made by SINTEF16) | Chest | Every 3 sec |
| Relative Humidity (RH) and Temperature | RH and temperature, custom-made by SINTEF 17) | Inner and outer surface of sleeve, integrated in jacket.Inside inner cloths back, at pulse belt | Every 3 sec |
| Relative Humidity and Temperature | OM-CP-MICRORHTEMP, Omega Engineering, Connecticut, USA (± 0.5°C and ± 3 RH) | Inner surface of sleeve, Outer surface of sleeve, Inside inner clothing back, Inner surface of jacket back | Each min |
| Skin temperature | Infrared sensor in sensors custom-made by SINTEF 16, 17) | Back of hand, integrated in jacket.Chest and back on pulse belt. | Every 3 sec |
| Skin temperature | Thermistors YSI-400, Yellow Spring Instruments, Ohio, USA, accuracy ± 0.15°C | Cheek, neck, chest, abdomen, back, finger, hand, forearm, upper arm, front of thigh, back of thigh shin, calf, | Every min |
| Activity | 3D accelerometer, 3D gyroscope, 3D magnetometer, in sensors custom-made by SINTEF 16, 17) | Back of hand, integrated in jacket. Chest and back at pulse belt. | 20 Hz |
| VO2 | Oxycon Pro, Jaeger, Hoechberg, Germany | Respiration | 5 min at each work intensity |
Relative humidity (RH) and temperature were measured with two different sensors located close to each other. As expected, the absolute values of the two sensors differed slightly, probably due to local variations in climate; however, the relative changes were comparable. Skin temperatures were measured with thermistors (at 12 different locations) and with infrared temperature sensors (hand, upper back and chest). In order to simplify the graphs, only humidity and temperature data from the OM-CP-MICRORHTEMP sensors, and the skin temperature measured by the thermistors are shown in the Results section.
Subjective evaluation
Perceived thermal sensation was measured for tests 2–12 using a modified version of the questionnaire developed by Nielsen et al20). Data were obtained before start and every 15 min throughout the experiment.
Calculation of metabolic energy production
VO2 was measured for five minutes once in every intensity period using indirect calorimetry (Oxycon Pro, Jaeger, Hoechberg, Germany). Metabolic energy production, M, was calculated from the VO2 measurements in accordance with ISO 98867).
Calculation of duration limited exposure (DLE) based on IREQ (ISO 11079)
Two different IREQ DLE values are usually given; DLEmin refers to a condition of high physiological strain and DLEneu refers to a condition with no physiological strain11). Table 3 gives an overview of the input parameters to the IREQ DLE calculation according to ISO 11079 using a DLE calculator with input parameters corresponding to moderate work intensity M= 165 W/m2 and chamber settings of −20°C and 3 m/s, resulting in DLEneu as 2 h and DLEmin as 8 h.
Table 3. Overview of the input parameters required for the IREQ DLE calculation. Average input parameters based test set-up are also given.
| Parameter | Unit | Description | Average values for DLE calculations |
|---|---|---|---|
| Metabolic energy production | M (W·m−2) | Standard values based on tables, 58 to 400 W/m2 | 165 W·m-2 |
| Rate of mechanical work | W (W·m−2) | Normally 0 | 0 |
| Ambient air temperature | Ta (oC) | < +10 oC | Chamber temp, −20oC |
| Mean radiant temperature | Tr (oC) | Often close to ambient air temperature | Chamber temp, −20oC |
| Air permeability | p (l·m−2·s−1) | Value based on clothing low <5, medium 50, high >100 l·m−2·s−1 | 25 l·m−2·s−1 |
| Walking speed | w (m·s−1) | Walking speed or calculated work created air movements | 0.7 m·s−1 and 0 m·s−1 |
| Relative air velocity | v (m·s−1) | 0.4 to 18 m·s−1 | 3 m·s−1 |
| Relative humidity | RH (%) | Relative humidity | 20 % |
| Available basic clothing insulation | Icl (clo) | 1 clo=0.155 W·m−2K | 2.5 clo |
| Results with average values | DLE | DLEneu | 2 h |
| DLEmin | 8 h |
Calculations and statistical methods
Descriptive statistics at both group and individual levels have been used to present the data.
A heart rate (HR) moving average (HRMA) of 1 min (20 samples) was used in figures and calculations. HRMA was calculated as:
(1)
Total acceleration of torso and hand were calculated as:(2) where t is time and Acc (x, t), Acc (y, t) and Acc (z, t) are the accelerations measured in the different directions. The amplitude, AccA (t), of the fluctuating AccT (t) signal was calculated as the difference between the upper and lower root-mean-square envelopes of AccT (t), using a sliding window of length S=600 samples (approximately 1 min) as shown by the equation 3, 4, and 5.
(3)
If the , the ACCT(t) element is part of the set upper. If the , it is part of the set lower. Nupper (t) is the number of elements in the upper set in the sliding window from t-tS/2 to t+tS/2, the Nlower (t) is the number for elements in the lower set in the sliding window.
(4)
The RMSlower(t) is calculated correspondingly for . (5) Differences in skin temperature between subjects at different locations on the body were calculated as the mean of the standard deviation values over the first 90 min of the test. Standard deviations were calculated for every t minutes (t ϵ {1, 2, 3, 90}) throughout the test, as shown in equation 6. Skin temperature at a given location at time t for test i, is given as T (t) i. (For t<74 min N=12, for t≥74 min N<12, since the first subject met the test abortion criterion 74 min into test).
(6)
The mean of the standard deviation throughout the first 90 min of the test was calculated as:
(7)
Correlation coefficients were calculated as the Pearson product-moment correlation coefficient, r.
(8)
Results
Subjective evaluation
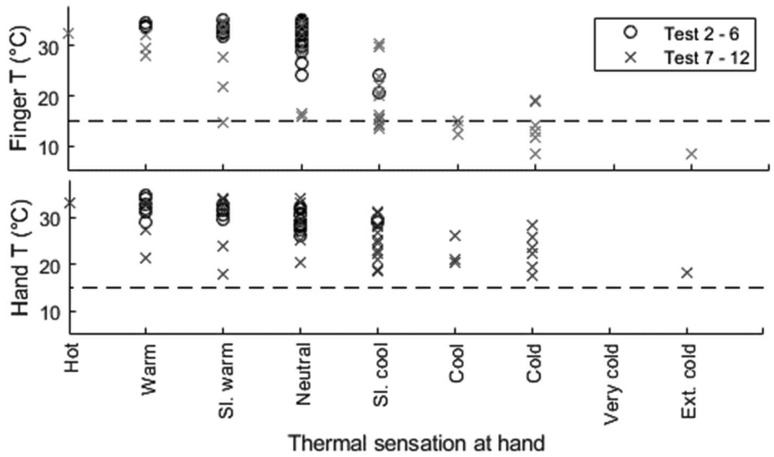
Every 15 min, the subjects answered questions about their subjective evaluation of thermal comfort and thermal sensation. At the end of the test, regarding the questions “How do you feel thermally?”, three out of 11 subjects answered Comfortable, six subjects responded Somewhat comfortable and two, Uncomfortable. Three tests were terminated due to low finger temperature, two that responded Somewhat comfortable and one that responded Uncomfortable. All except three subjects would have preferred the ambient temperature to be somewhat warmer. The exceptions were the Uncomfortable subjects, who would have preferred the ambient air temperature Much warmer, and one of the thermal Comfortable subjects who was Neutral as to preferred temperature. Figure 1 shows the response to the question about thermal sensation on hands and how it related to the measured skin temperature at finger and hand. The subjects evaluation of the thermal sensation in their hands showed wide variations between individuals, and the correlations with measured skin temperatures were poor.
Fig. 1.
Actual skin temperature at hand and finger related to thermal sensation at hand. Test 2–6 are shown with black circles, test 7–12 with grey crosses. Dashed line shows the critical threshold for finger skin temperature at 15 °C, regarded as a value in which important loss of dexterity occurs.
Metabolic energy production and DLE
Table 4 shows estimated metabolic energy production based on personal VO2 measurement and the variation of IREQ DLE throughout the test, depending on the different work intensities (moderate, high, rest). For all test subjects, DLE was more than eight hours in the “hard” intensity period and about 20 min during the “rest” period. However, during “moderate” work intensity DLENeu ranged from two to more than eight hours.
Table 4. Metabolic energy production (W/m2) and calculated IREQ delimiters (DLEMin and DLENeu, given in hours) for all subjects.
| Test No. | Moderate | Hard | Rest | Termi-nation | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| W·m−2 | DLEMin | DLENeu | W·m−2 | DLEMin | DLENeu | W·m−2 | DLEMin | DLENeu | (min) | |
| 1 | 199 | >8 | >8 | 285 | >8 | >8 | 49 | 0.4 | 0.3 | >90 |
| 2 | 204 | >8 | >8 | 297 | >8 | >8 | 63 | 0.4 | 0.3 | >90 |
| 3 | 220 | >8 | >8 | 295 | >8 | >8 | 51 | 0.4 | 0.3 | >90 |
| 4 | 268 | >8 | >8 | 343 | >8 | >8 | 71 | 0.4 | 0.3 | >90 |
| 5 | 222 | >8 | >8 | 311 | >8 | >8 | 51 | 0.4 | 0.3 | >90 |
| 6 | 228 | >8 | >8 | 336 | >8 | >8 | 51 | 0.4 | 0.3 | >90 |
| 7 | 208 | >8 | >8 | 275 | >8 | >8 | 40 | 0.4 | 0.3 | 83 |
| 8 | 232 | >8 | >8 | 322 | >8 | >8 | * | * | * | 75 |
| 9 | * | * | * | * | * | * | * | * | * | >120 |
| 10 | 204 | >8 | >8 | 290 | >8 | >8 | 49 | 0.4 | 0.3 | >120 |
| 11 | 243 | >8 | >8 | 316 | >8 | >8 | 45 | 0.4 | 0.3 | 100 |
| 12 | * | * | * | * | * | * | * | * | * | 74 |
*Missing VO2 measurements.
Values for DLE less than 8 hours in bold and italic.
Heart-rate, relative humidity and temperature inside clothing
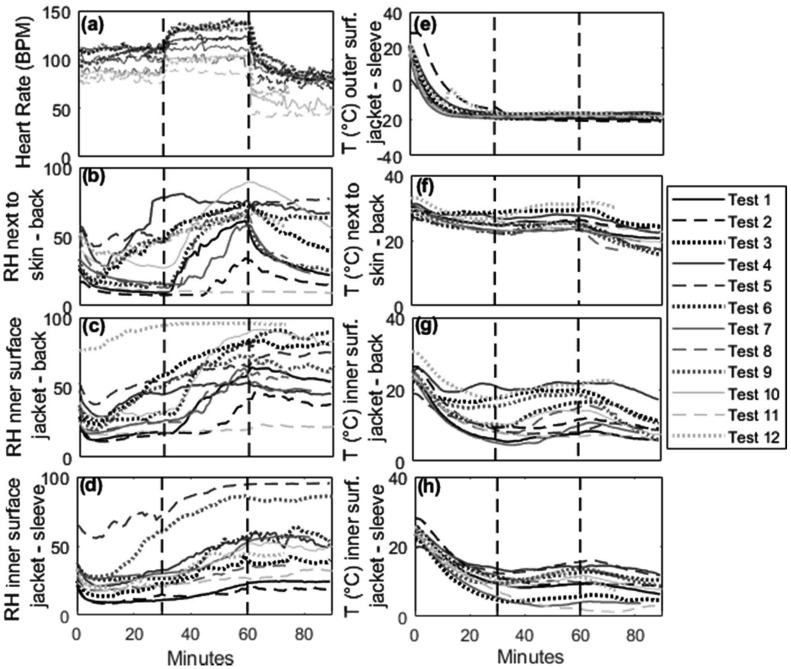
Figure 2 displays HRMA, RH and air temperature at different locations for all subjects. HR varied in the same way for all subjects during the protocol but the magnitude of the changes differed among the test subjects, due to differences in fitness level and physiology (Fig. 2a). The shape of the RH curve had a higher within-person variability than HR (Fig. 2b–d). In some subjects, the increase in humidity started during moderate work intensity, indicating that sweating took place in this phase. In others, there was a sudden increase that coincided with the change in work intensity (from moderate to high) and HR. The humidity close to the skin (Fig. 2b) decreased for most subjects during the rest period and was probably a combination of a fall in temperature (Fig. 2f) and transport of humidity away from the skin through the clothing. RH remained high in the outer layer of clothing (the sensors were placed between the inner and outer layer of clothing), both at the back (Fig. 2c) and inside the sleeve at the upper arm (Fig. 2d). The changes seen in RH inside the outer layer of cloths throughout the test were similar at the back and in the sleeve, but as expected, the magnitude of change was higher at the back, due to the limited circulation of humid air between the trunk and the sleeve. Figure 2e–h shows air temperature outside and inside the clothing. The temperature measured outside the clothing (Fig. 2e) stabilised after 20 mins to between −16 °C and −21°C. The variation probably reflects differences in the heat radiated from the jacket and ambient chamber temperature (target −20°C). The temperature at the back differed less between subjects inside the inner layer of clothing (Fig. 2f) than in the outer layer of clothing (Fig. 2g) and in the sleeve (Fig. 2h). For all subjects a temperature drop inside the inner layer of clothing (Fig. 2f) was seen at the start of the rest period (at 60 min).
Fig. 2.
For all subjects (a) Heart rate (b) Relative humidity (RH) next to skin at upper back (c) RH at inner surface of jacket at upper back (d) RH at inner surface of jacket sleeve (e) Temperature outside jacket sleeve (f) Temperature next to skin at upper back (g) Temperature at inner surface of jacket at upper back (h) Temperature at inner surface of jacket sleeve. Dashed vertical lines indicate changes in activity level according to the protocol (moderate, hard, rest).
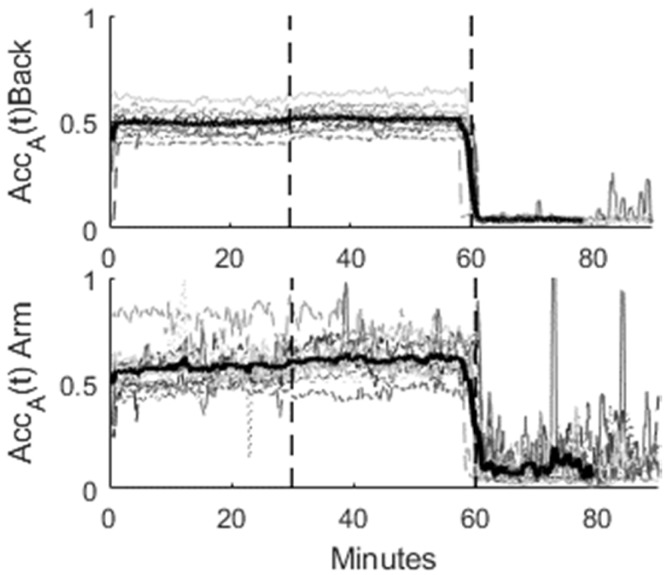
Activity
Total accelerations, ACCA (t), calculated according to equation 2 to 5, at the upper back and at the top of the hand are shown in Fig. 3. Both the in-subject and between-subjects differences were larger at the hand than at the back, reflecting more individual variation in movement of hands than back when walking. There were no pronounced differences in the accelerometer readings when the workload was increased by increasing the inclination of the treadmill 30 min into the test. This was as expected.
Fig. 3.
Activity from accelerometers, given as the amplitude of total acceleration, AccA(t), registered at upper back and back of hand. Black bold lines are average of all tests. Dashed vertical lines indicate changes in activity level according to the protocol (moderate, hard, rest).
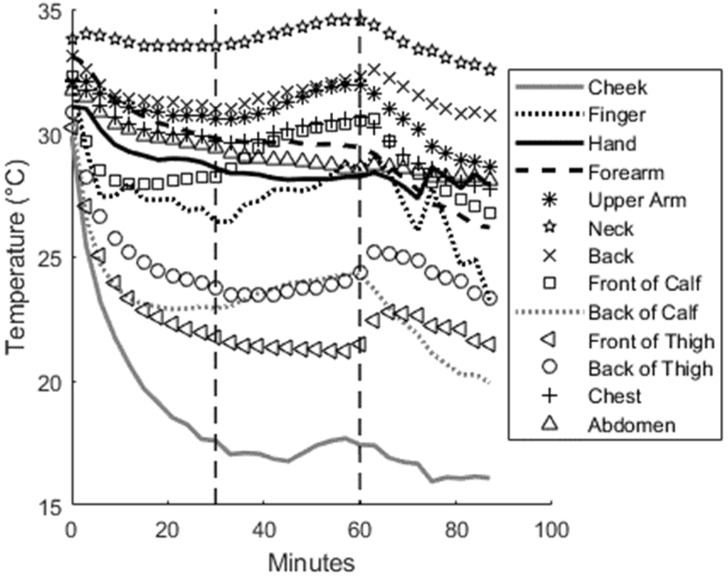
Skin temperature
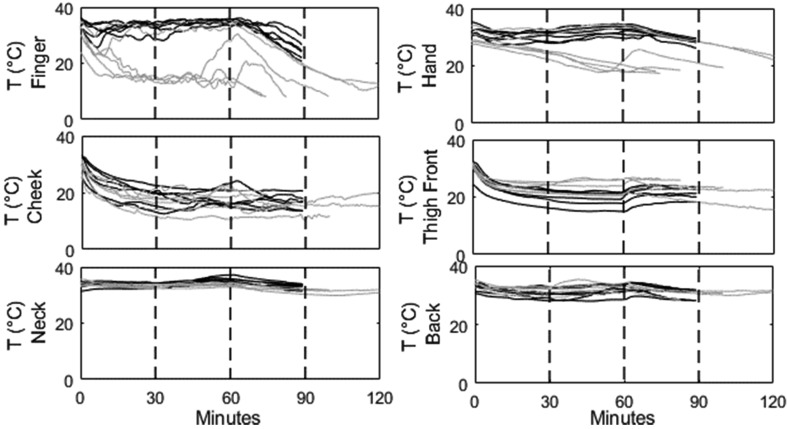
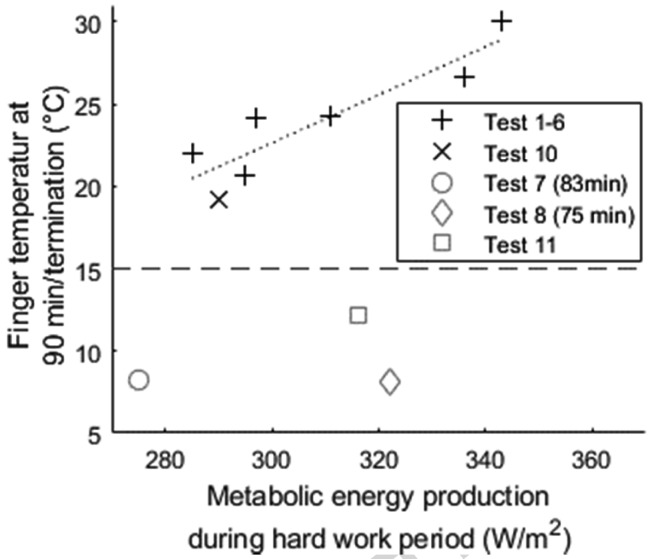
The local cooling as measured by skin temperature varied between the test subjects and with the location on the body. Figure 4 shows the mean temperature of all test subjects at all the sensor locations. Table 5 shows that the finger had the highest inter-subject variability, followed by the hand, the cheek and the backside of the thigh and calf. The neck and front of calf displayed the lowest inter-subject variability. Figure 5 shows the skin temperature for finger, hand, cheek, backside of thigh, neck and upper back for all subjects.Tests 7, 8, 11 and 12 were aborted when the absolute criterion for finger temperature was reached (skin temperature below 8°C), after 83, 75, 100 and 74 min respectively. All the other tests were terminated according to the test protocol, at 90 min for tests 1–6 and 120 min for tests 9 and 10. Figure 6 shows that there was a linear relationship (with correlation coefficient r=0.91) between metabolic energy production during the hard work period (30–60 min) and finger temperature at 90 min (after the 30-min rest period). Subjects whose finger temperatures fell below the critical limit (15°C) do not fit this simple model. They were all in the second group who were instructed not to move their hand or clench their fists.
Fig. 4.
The figure shows the average of the skin temperature at different locations for all test subjects, n=12. The steps in hand and finger temperatures after 70 min are caused by abortion of some of the tests due to reaching abortion criteria. Dashed vertical lines indicate changes in activity level according to the protocol (moderate, hard, rest).
Table 5. Variability in skin temperature between subjects at different locations of the body, given as the mean of the standard deviation values calculated for every minute throughout the test (equation 6 and 7).
| Location | StDevlocation |
|---|---|
| Cheek | 3.2 |
| Finger | 8.0 |
| Hand | 4.3 |
| Forearm | 1.4 |
| Upper Arm | 2.1 |
| Neck | 1.0 |
| Back | 1.6 |
| Front of calf | 1.2 |
| Back of calf | 3.1 |
| Front of thigh | 2.5 |
| Back of thigh | 3.1 |
| Chest | 1.4 |
| Abdomen | 2.9 |
Fig. 5.
Skin temperature measured at finger, hand, cheek, front of thigh, neck and upper back. Black lines shows measurements from test 1–6, grey lines measurements from test 7–12.
Fig. 6.
Finger temperature after 90 min, or at termination, plotted against the metabolic energy production during the hard work period (not available for test 9 and 12). Dashed vertical line shows the critical threshold for finger skin temperature at 15°C. Black markers are subjects in first part of test (allowed to move fingers) grey markers are subjects from second part of test (instructed not to move fingers). The dotted line is the least square fit line for finger temperatures above 15°C. Asterisk mark is test 10, which is the only subject from the second group with temperature above 15°C.
Discussion
The aim of this study was to improve decision support for workers in cold climates by taking advantage of the information provided by biomedical data from the rapidly growing market of wearable sensors. Important findings were that for some test persons the subjective evaluation of cold stress was not in line with the physiological measurements and that there were individual differences in metabolic energy production and thermal responses with same exposure. In real life both genders would be present, as well as a greater variation in age and health, thus real-life variation and deviation will probably be significantly greater. Temperature, humidity, activity and heart rate were found to be relevant indicators for cold stress assessment, and the locations of the sensors in the prototype jacket were adequate. The study reveals the need for cold stress assessment and indicate that a generalized approached is not sufficient to assess cold stress on an individual level. This is not taken into account by the international standards, which are based on average values.
The need for a personalized model for cold stress assessment
The measured sensor data showed that there were large individual differences in metabolic energy production and thermal responses under identical exposure conditions. Metabolic energy production while walking at 5m/s at two different inclinations (0 or 5%), varied substantially between individuals, even within this homogeneous group of young males in good physical condition. Heart rate, humidity and air temperature in clothing also displayed wide individual differences. Subjects with high aerobic capacity and thus worked at a relatively low percentage of their maximal aerobic capacity during treadmill walking showed little or no increase in relative humidity due to sweating, and the air temperature inside the clothing microclimate therefore fell more rapidly. Our results showed that the subjective thermal sensation of the hands did not closely correspond to the measured hand and finger skin temperature, indicating large individual differences in cold tolerance. Nielsen and Nielsen21) demonstrated that neither changes in skin temperature nor skin temperature distribution correlated with general thermal sensation. This is similar to our observation that similar ratings of thermal sensation of the hands could well be associated with a 10–15 °C difference in finger skin temperature. Gerret et al.22) demonstrated that sensitivity is greatest at the head, followed by the torso and declines towards the extremities, which is the general consensus of regional sensitivity distribution. The palms of the hands were among the least sensitive areas during cold stimulation, and further suggested that the hands are more sensitive to changes in skin temperature than to absolute temperatures22). Thermal sensation is an important component of a feeling of well-being and comfort during work, but due to wide variations in individual experience and cold tolerance, additional objective measures like skin temperature would be beneficial in a decision-support system.
These results justify the need for a decision system to assess cold stress, as in many cases “feeling” of cold were for several subjects not a good guideline, low temperature may impair the function of hands and fingers and thereby increase the risk for dangerous situations. Since the responses differed with the same exposure, these results show that a model based on average values is not suitable, personalization is necessary to address the cold stress.
Relevant sensors and locations for online cold stress assessment
Our protocol was set up to produce only local rather than general cooling, and based on the subjective evaluation there was no indication that any of the subjects experienced general cooling. However, four of the 12 tests were terminated due to local cooling, i.e. reaching the critical limit for skin temperature. Distributed skin temperature was measured and in the average of all tests, of the locations measured the unprotected cheek was found to be the coldest area, followed by the thigh and the calf. However, finger temperature fell more rapidly when the subjects started to get cold, and all the tests that were terminated after meeting the low skin temperature criteria, were terminated due to reaching critical temperature at the finger. At the same time, an adequate finger temperature is critical to avoid degradation of manual performance4, 5). This indicates that the finger is the most relevant location for measurements of skin temperature. Today no temperature sensors exist that could be integrated unobtrusively into the finger of the glove and provide reliable measurements for extended periods; however sensors of this kind will probably become available in the not too distant future. We believe that the back of the hand is the best choice for the present, since this is the closest area to the fingers. A sensor for measuring skin temperature in unprotected areas such as the cheek may also be desirable. This could be a sensor attached to a headset or similar.
The accelerometer data showed that it was easy to discriminate between rest and activity, but they did not clearly discriminate between moderate and hard work since the subjects were walking on a treadmill and only the incline was changed between the two intensity periods. The activity sensor on the back of the hand varied more by subject than the sensor on the torso. Data from the sensor on the torso were less subject-dependent and more related to movement and metabolic energy production. That means that sensors on the torso will be the most valuable for assessments of activity level, although locating them on the hand or arm may be useful as a means of identifying specific risk-related movements and work tasks. Studies have shown that low temperature in combination with vibration exposure influences the finger blood flow23) and also increases the risk for pathologies17). In earlier work we have shown that the sensor and location used in this study may also be used as an indicator of exposure to vibration24).
Sweating may be an important measure, because during sweating heat loss immediately increases, as does the sensation of cold. The accumulation of humidity inside the clothing may over time also reduce clothing insulation25). Mainly due to variations in aerobic capacity, there were large differences in sweating response and further humidity in the clothing layers. Several subjects experienced a sudden decrease in the humidity close to the skin when hard work was stopped, indicating that humidity was transported out to the outer layers of clothing. In other subjects, there was little or no decrease in humidity during the rest period. The three subjects who answered that they were thermally comfortable after 90 min were all in the group with a sudden decrease in measured humidity, which is in line with the results of Bakkevig et al26). However, additional factors like heat acclimation, and individual differences in onset of sweat and absolute sweat rate, can lead to profound individual differences in sweat responses.
Heart rate increased as a function of intensity and varied in the same way for all subjects during the protocol, but the magnitude of the changes differed between the test subjects, due to differences in fitness level and physiology. Heart rate is usually obtained from electrical measurements on the chest using electrodes in a pulse belt (as in this study), or through optical measurements of the blood flow at e.g. the wrist. The chest electrode is more reliable and provides more accurate measurements than the optical blood flow measurements at the wrist, but for this application, where beat to beat variation may not be relevant, the accuracy of a wrist band with an optical sensor may be sufficient27).
Metabolic energy production was estimated from measurements of VO2, and differed between the subjects due to fitness and physiological differences. In a wearable system where measurements of VO2 is not an option, HR is widely used to estimate metabolic energy production, based on a linear relationship between heart rate and VO228). Even though considerable inter-individual differences in the HR-VO2 relationship exist due to differences in movement efficiency, age and fitness, the HR-VO2 relationship is found to be consistent for an individual across a range of submaximal tasks29, 30). It is most usual to establish a person’s HR-VO2 relationship during walking or bicycling at submaximal intensities. However, since the HR-VO2 relationship differs between upper-and lower-body activities31), walking or cycling would not provide accurate measures during typical industrial work that often involves heavy upper-body loads. Even though HR is a well-established proxy measurement for metabolic energy production, since heart rate is known to be influenced by both physiological and psychological factors in addition to the fact that the HR-VO2 relationship is dependent on the specific activity, such estimates can be improved if used in conjunction with other sensors such as accelerometers that provide valuable information about the specific task and actual work load28, 32). Moreover, a neural network-, and heart rate variability-based method has recently been developed to estimate metabolic energy production from HR and R-to-R interval recordings variability without the need for individual calibration between HR and VO233,34,35). This method has been utilised and is frequently used in commercial sport watches such as Garmin, Polar or Suunto, and might be valuable for use in occupational health studies36).
Our approach was to use physiological sensors integrated into a jacket, in addition to measuring heart rate and activity with a chest belt. All sensors used in the prototype jacket were suitable for assessment of cold stress. Heart rate can be used to assess the workload and estimate metabolic energy production. Humidity and activity sensors will have useful context information to correct the model in order to take different activity periods into account, and skin temperature is necessary to reveal local cooling. This would make it possible to design a truly wearable system for decision support for workers in cold climate. The advantage of integrating sensors into standard work clothing compared to add-on sensors is that no extra work is needed to deploy the sensors. In addition, this would ensure that the workers always would wear the sensors. The disadvantages are possible wear on the system, and handling, e.g. when washing the clothing, and charging the battery.
Towards a wearable sensor system for continuous occupational cold stress assessment
Our approach was to provide online decision support in occupational settings. The indexes for cold stress described in both the literature and industrial standards, e.g. IREQ and WCI, are based on averages and do not take into account the huge individual variations that we and others have shown. However, an IREQ model with real time personal input data has the potential to assess general cooling on an individual level by using continuous real-time sensor data as input instead of average estimates.
Metabolic energy production is the dominant parameter for estimating DLE in the IREQ model and our data show that the prediction of DLE is very sensitive to this input parameter and is therefore likely to display large subject variations. We calculated DLE values based on VO2 data for metabolic energy production during all three work-intensity periods. In the moderate work intensity period, in which our subjects started in a thermally neutral state, DLEneu ranged from two to more than eight hours. This shows that using actual measurements, or individualised estimates, for metabolic energy production instead of average numbers, will provide a more reliable prediction of DLE.
Limitations of the IREQ model have been reported in previous studies2, 37, 38). Furthermore, our data indicate that previous activity and physiological state are important and reliable predictors of cold stress. In the rest period, the use of actual measurements for metabolic energy production produced DLE values of about 20 min for all subjects. If this was correct, all the subjects should have experienced general/whole-body cooling during the rest period, which lasted for more than 20 min (from 30–60 min). However, all the subjects underwent a period of hard work before the rest period. They were thus not in a thermally neutral state at the start of the rest period, and therefore experienced general cooling. While the DLE calculations based on the IREQ model assume a thermally neutral starting point, a continuous model needs to take into account recent metabolic energy production and a non-neutral thermal state. Metabolic energy production estimates based on HR, HR variability, and humidity and activity sensors may be useful for correcting the DLE for a non-neutral thermal state at start of a rest or low-activity period. A model that estimates the length of the remaining work period that does not pose a risk of general cooling, based on a modified IREQ index with continuous sensor data as input and a correction for a non-neutral thermal state at start, is promising and should be further evaluated.
Correlations between different relevant parameters should be utilised to develop models for cold stress. There was no consistent correlation between finger temperature and hand temperature or any other skin temperature. A generalized model that predicts finger temperature from any other skin temperature is therefore not possible. However, the measurements on the single subject who was tested twice (tests 3 and 9) indicate that there is a consistent correlation on an individual level that might be explored using machine learning techniques.
A simple correlation study between metabolic energy production and finger temperature gave interesting results. We found that for finger skin temperatures above the critical limit of around 15°C, there was a linear relationship between metabolic energy production in the hard-working period and the finger temperature 30 min after the end of that period. This observation might be useful and suggested further work to determine whether local cooling (i.e. finger temperature) can be estimated and/or predicted from parameters related to energy production and movements, e.g. using machine-learning techniques. In addition, Rintamäki et al.39) demonstrated that a core temperature of 37.6°C is needed to start finger warming. The known association between physical activity and core temperature40) further suggests that physical activity should exceed 42% of an individual’s maximal aerobic capacity to warm up the fingers39), which can explain some of the variations in finger skin temperature observed in our study.
Other models or strategies based on heart rate measurements, humidity and activity also ought to be investigated. The growing field of machine learning algorithms is promising and should be utilized in occupation settings. This could clear the way for adaptation and learning on both individual and population levels.
Conclusion
This study demonstrated large individual differences in both subjective and physiological responses combined with short-term variations due to changing tasks and work intensities during severe cold exposure. Wearable sensors provided relevant real-time information for cold stress assessment, and our results support the need for a decision-support system based on individual data rather than a generalized system based on averaged that is used today.
Funding
This study was part of the Safera project SmartPro (Grant no 251907) which was supported by the SAF€RA programme and the Research Council of Norway.
Acknowledgments
The authors wish to thank the subjects for their participation in this study. We also would like to thank Hannu Rintamäki, Sirkka Rissanen and Kirsi Jussila at the Finnish Institute of Occupational Health for valuable discussions and excellent partnership in the SmartPro project.
References
- 1.Holmér I. (2009) Evaluation of cold workplaces: an overview of standards for assessment of cold stress. Ind Health 47, 228–34. [DOI] [PubMed] [Google Scholar]
- 2.Gao C, Lin LY, Halder A, Kuklane K, Holmér I. (2015) Validation of standard ASTM F2732 and comparison with ISO 11079 with respect to comfort temperature ratings for cold protective clothing. Appl Ergon 46 Pt A, 44–53. [DOI] [PubMed] [Google Scholar]
- 3.Enander A. (1987) Effects of moderate cold on performance of psychomotor and cognitive tasks. Ergonomics 30, 1431–45. [DOI] [PubMed] [Google Scholar]
- 4.Wiggen ON, Heen S, Færevik H, Reinertsen RE. (2011) Effect of cold conditions on manual performance while wearing petroleum industry protective clothing. Ind Health 49, 443–51. [DOI] [PubMed] [Google Scholar]
- 5.Heus R, Daanen HA, Havenith G. (1995) Physiological criteria for functioning of hands in the cold: a review. Appl Ergon 26, 5–13. [DOI] [PubMed] [Google Scholar]
- 6.Auerbach PS .(2007) Wilderness Medicine, 5th Ed., Mosby Elsevier. [Google Scholar]
- 7.International Organization for Standardization (2004) Ergonomics —Evaluation of thermal strain by physiological measurements, ISO 9886.
- 8.International Organization for Standardization (2004) Ergonomics of the thermal environment —Determination of metabolic rate, ISO 8996.
- 9.ASTM International (2016) Standard practice for determining the temperature ratings for cold weather protective clothing, ASTM F2732-16.
- 10.International Organization for Standardization (2008) Ergonomics of the thermal environment —Cold workplaces: Risk assessment and management, ISO 15743.
- 11.International Organization for Standardization (2007) Ergonomics of the thermal environment —Determination and interpretation of cold stress when using requiered clothing insulation (IREQ) and local cooling effects, ISO 11079.
- 12.International Organization for Standardization (2009) Ergonmics of the thermal environment —Estimation of thermal insulation and water vapour resistance of a clothing ensemble, ISO 9920.
- 13.Holmér I. (1993) Work in the cold. Review of methods for assessment of cold exposure. Int Arch Occup Environ Health 65, 147–55. [DOI] [PubMed] [Google Scholar]
- 14.Osczevski R, Bluestein M. (2005) The new wind chill equivalent temperature chart. Bull Am Meteorol Soc 86, 1453–8. [Google Scholar]
- 15.Holmér I. (1988) Assessment of cold environments in terms of required insulation. Arctic Med Res 47 >Suppl 1, 239–42. [PubMed] [Google Scholar]
- 16.Seeberg TM, Vardoy AS, Austad HO, Wiggen O, Stenersen HS, Liverud AE, Storholmen TC, Faerevik H. (2013) Protective jacket enabling decision support for workers in cold climate. Conf Proc IEEE Eng Med Biol Soc 2013, 6498–501. [DOI] [PubMed] [Google Scholar]
- 17.Burström L, Järvholm B, Nilsson T, Wahlström J. (2010) White fingers, cold environment, and vibration—exposure among Swedish construction workers. Scand J Work Environ Health 36, 509–13. [DOI] [PubMed] [Google Scholar]
- 18.Liverud AE, Vedum J, Fleurey F, Seeberg TM. (2012) Wearable wireless multi-parameter sensor module for physiological monitoring. Stud Health Technol Inform 177, 210–5. [PubMed] [Google Scholar]
- 19.Seeberg TM, Vedum J, Sandsund M, Austad HO, Liverud AE, Vardoy AS, SvagÅrd IS., Strisland F (2014) Development of a wearable multisensor device enabling continuous monitoring of vital signs and activity. Biomedical and Health Informatics. 213–18. [Google Scholar]
- 20.Nielsen B, Hales JR, Strange S, Christensen NJ, Warberg J, Saltin B. (1993) Human circulatory and thermoregulatory adaptations with heat acclimation and exercise in a hot, dry environment. J Physiol 460, 467–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nielsen R, Nielsen B. (1984) Influence of skin temperature distribution on thermal sensation in a cool environment. Eur J Appl Physiol Occup Physiol 53, 225–30. [DOI] [PubMed] [Google Scholar]
- 22.Gerrett N, Ouzzahra Y, Redortier B, Voelcker T, Havenith G. (2015) Female thermal sensitivity to hot and cold during rest and exercise. Physiol Behav 152Pt A, 11–9. [DOI] [PubMed] [Google Scholar]
- 23.Ye Y, Griffin MJ. (2011) Effects of temperature on reductions in finger blood flow induced by vibration. Int Arch Occup Environ Health 84, 315–23. [DOI] [PubMed] [Google Scholar]
- 24.Austad HO, Røed MH, Liverud AE, Dalgard S, Seeberg TM .(2013) Hand-arm vibration exposure monitoring with wearable sensor module, in 10th International Conference on Wearable Micro and Nano Technologies for Personalized Health. PHealth. [PubMed]
- 25.Chen YS, Fan J, Zhang W. (2003) Clothing thermal insulation during sweating. Text Res J 73, 152–7. [Google Scholar]
- 26.Bakkevig MK, Nielsen R. (1994) Impact of wet underwear on thermoregulatory responses and thermal comfort in the cold. Ergonomics 37, 1375–89. [DOI] [PubMed] [Google Scholar]
- 27.Pietilä J, Mehrang S, Tolonen J, Helander E, Jimison H, Pavel M, Korhonen I .(2017) Evaluation of the accuracy and reliability for photoplethysmography based heart rate and beat-to-beat detection during daily activities, in EMBEC & NBC. Springer, Singapore. [Google Scholar]
- 28.Hills AP, Mokhtar N, Byrne NM. (2014) Assessment of physical activity and energy expenditure: an overview of objective measures. Front Nutr 1, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Freedson PS, Miller K. (2000) Objective monitoring of physical activity using motion sensors and heart rate. Res Q Exerc Sport 71Suppl, S21–9. [PubMed] [Google Scholar]
- 30.Livingstone MB. (1997) Heart-rate monitoring: the answer for assessing energy expenditure and physical activity in population studies? Br J Nutr 78, 869–71. [DOI] [PubMed] [Google Scholar]
- 31.Li R, Deurenberg P, Hautvast JG. (1993) A critical evaluation of heart rate monitoring to assess energy expenditure in individuals. Am J Clin Nutr 58, 602–7. [DOI] [PubMed] [Google Scholar]
- 32.Ainslie P, Reilly T, Westerterp K. (2003) Estimating human energy expenditure: a review of techniques with particular reference to doubly labelled water. Sports Med 33, 683–98. [DOI] [PubMed] [Google Scholar]
- 33.Pulkkinen A, Kettunen J, Martinmäki K, Saalasti S, Rusko H. (2004) On- and off-dynamics and respiration rate enhance the accuracy of heart rate based VO2 estimation. Med Sci Sports Exerc 36, 253.14767248 [Google Scholar]
- 34.Pulkkinen A, Saalasti S, Rusko H. (2005) Energy expenditure can be accurately estimated from HR without individual calibration. Med Sci Sports Exerc 37, 113. [Google Scholar]
- 35.VO2 estimation method based on heart rate measurement. Firstbeat Technologies 2005. http://www.firstbeat.fi/files/VO2_Estimation.pdf. Accessed March 28, 2006.
- 36.Smolander J, Juuti T, Kinnunen ML, Laine K, Louhevaara V, Männikkö K, Rusko H. (2008) A new heart rate variability-based method for the estimation of oxygen consumption without individual laboratory calibration: application example on postal workers. Appl Ergon 39, 325–31. [DOI] [PubMed] [Google Scholar]
- 37.Alfano FR, Palella BI, Riccio G. (2013) Notes on the implementation of the IREQ model for the assessment of extreme cold environments. Ergonomics 56, 707–24. [DOI] [PubMed] [Google Scholar]
- 38.Kuklane K, Gao C, Holmér I, Giedraityte L, Bröde P, Candas V, den Hartog E, Meinander H, Richards M, Havenith G. (2007) Calculation of clothing insulation by serial and parallel methods: effects on clothing choice by IREQ and thermal responses in the cold. Int J Occup Saf Ergon 13, 103–16. [DOI] [PubMed] [Google Scholar]
- 39. Rintamäki H, Rissanen S, Makinen T, Peitso A.)(2004) Finger temperatures during military field training at 0 to −29°C. J Therm Biol 29, 857–60. [Google Scholar]
- 40.Åstrand PO, Rodahl K, Dahl HA, Strømme SB .(2003) Textbook of Work Physiology, physiological bases of exercise, 4th Ed., Human Kinetics, Champaign. [Google Scholar]