Abstract
Background:
Hospitalizations of chronic dialysis patients have not been previously studied at a national level in Canada. Understanding the scope and variables associated with hospitalizations will inform measures for improvement.
Objective:
To describe the risk of all-cause and infection-related hospitalizations in patients on dialysis.
Design:
Retrospective cohort study using health care administrative databases.
Setting:
Provinces and territories across Canada (excluding Manitoba and Quebec).
Patients:
Incident chronic dialysis patients with a dialysis start date between January 1, 2005, and March 31, 2014. Patients with a prior history of kidney transplantation were excluded.
Measurements:
Patient characteristics were recorded at baseline. Dialysis modality was treated as a time-varying covariate. The primary outcomes of interest were all-cause and dialysis-specific infection-related hospitalizations.
Methods:
Crude rates for all-cause hospitalization and infection-related hospitalization were determined per patient year (PPY) at 7 and 30 days, and at 3, 6, and 12 months postdialysis initiation. A stratified, gamma-distributed frailty model was used to assess repeat hospital admissions and to determine the inter-recurrence dependence of hospitalizations within individuals, as well as the hazard ratio (HR) attributed to each covariate of interest.
Results:
A total of 38 369 incident chronic dialysis patients were included: 38 088 adults and 281 pediatric patients (age less than 18 years). There were 112 374 hospitalizations, of which 11.5% were infection-related hospitalizations. The all-cause hospitalization rate was similar for all adult age groups (age 65 years and older: 1.40, 1.35, and 1.18 admissions PPY at 7 days, 30 days, and 6 months, respectively). The all-cause hospitalization rate was higher for pediatric patients (1.67, 2.48, and 2.47 admissions PPY at 7 days, 30 days, and 6 months, respectively; adjusted HR: 2.73, 95% confidence interval [CI]: 2.37-3.15, referent age group: 45-64 years). Within the first 7 days after dialysis initiation, patients on peritoneal dialysis had a higher risk of all-cause hospitalization (HR: 1.27, 95% CI: 1.07-1.50) and infection-related hospitalization (HR: 2.05, 95% CI: 1.19-3.55) compared with patients on hemodialysis. Beyond 7 days, the risk did not differ significantly by dialysis modality. Female sex and Indigenous race were significant risk factors for all-cause hospitalization.
Limitations:
The cohort had too few home hemodialysis patients to examine this subgroup. The outcome of infection-related hospitalization was determined using diagnostic codes. Dialysis patients from Manitoba and Quebec were not included.
Conclusions:
In Canada, the rates of hospitalization were not influenced by dialysis modality beyond the initial 7-day period following dialysis initiation; however, the rate of hospitalization in pediatric patients was higher than in adults at every time frame examined.
Keywords: dialysis, administrative data, risk factor, Canadian
Abrégé
Contexte:
Le taux d’hospitalisation des patients dialysés n’avait jamais fait l’objet d’une étude pancanadienne. Une connaissance approfondie de la portée et des variables associées aux hospitalisations orientera les mesures d’amélioration.
Objectif de l’étude:
L’étude visait à mieux évaluer les risques d’hospitalisations des patients dialysés; toutes causes confondues ou liées spécifiquement à une infection.
Type d’étude:
Il s’agit d’une étude de cohorte rétrospective fondée sur des bases de données administratives en santé.
Cadre de l’étude:
L’étude couvrait les provinces et territoires du Canada à l’exception du Québec et du Manitoba.
Patients:
L’étude a porté sur tous les patients dialysés à vie dont le traitement avait commencé entre le 1er janvier 2005 et le 31 mars 2014. Les patients ayant reçu une greffe rénale ont été exclus.
Mesures:
Les caractéristiques initiales des patients ont été consignées, et la modalité de dialyse a été traitée comme une co-variable sujette à changement dans le temps. La principale issue d’intérêt était une hospitalisation due à une infection directement liée à la dialyse, ou une hospitalisation toutes causes confondues.
Méthodologie:
Les taux bruts d’hospitalisations toutes causes confondues (global) et d’hospitalisations liées à une infection ont été calculés en années-patients (HAP) à différents moments suivant le début de la dialyse (7 jours, 30 jours, 3 mois, 6 mois et 12 mois). Un modèle stratifié de fragilité à distribution gamma a été employé pour i) répertorier les hospitalisations répétées; ii) déterminer l’interrécurrence et le lien de dépendance entre les hospitalisations pour chaque patient; et iii) établir le rapport de risque (RR) attribué à chaque covariable d’intérêt.
Résultats:
En tout, 38 369 patients dialysés, soit 38 088 adultes et 281 patients mineurs (moins de 18 ans) ont été inclus dans l’étude. Au cours de la période étudiée, on a répertorié 112 374 hospitalisations, dont 11,5 % étaient dues à une infection en lien direct avec la dialyse. Le taux d’hospitalisations global était similaire pour tous les groupes d’âge chez les patients adultes. Par exemple, chez les patients âgés de 65 ans et plus, ce taux se situait respectivement à 1,40 HAP, à 1,35 HAP et à 1,18 HAP lorsque calculé 7 jours, 30 jours et 6 mois après l’initiation de la dialyse. Lorsque comparé au groupe des 45-64 ans, le taux d’hospitalisations global s’est avéré plus élevé chez les patients pédiatriques (1,67 HAP à 7 jours, 2,48 HAP à 30 jours et 2,47 HAP à 6 mois) post-initiation de la dialyse (RR: 2,73; IC 95 %: 2,37-3,15). Dans les 7 jours suivant l’initiation du traitement, les patients traités par dialyse péritonéale présentaient un risque plus élevé d’hospitalisation toutes causes confondues (RR: 1,27; IC 95 %: 1,07-1,50) ou d’hospitalisation liée à une infection (RR: 2,05; IC 95 %: 1,19-3,55) que les patients hémodialysés. Par contre, cet écart entre les modalités de dialyse n’était plus observable au-delà des sept premiers jours. Enfin, le fait d’être autochtone ou de sexe féminin s’avérait un facteur de risque d’hospitalisation significatif (toutes causes confondues).
Limites de l’étude:
Plusieurs facteurs limitent la portée des résultats: i) la cohorte comptait trop peu de patients hémodialysés à domicile pour permettre une analyse de ce sous-groupe; ii) les hospitalisations relatives à une infection ont été établies à l’aide de codes diagnostiques; et iii) les patients dialysés résidant au Québec et au Manitoba étaient exclus de l’étude.
Conclusion:
Au Canada, au-delà des sept jours suivant l’initiation de la dialyse, la modalité employée n’a plus d’influence sur les taux d’hospitalisations. Cependant, à tous les moments post-initiation mesurés, les taux d’hospitalisations se sont avérés plus élevés chez les patients pédiatriques que chez les adultes.
What was known before
Patients on dialysis have a high risk of hospitalization relative to the general population. Hospitalization rates of dialysis patients in the United States have been tracked for many years. In contrast, there are limited data on hospitalizations of dialysis patients in Canada.
What this adds
This is the first national study to describe the important issue of hospitalizations in Canadian chronic dialysis patients. Pediatric, Indigenous, and female patients are at higher risk for hospitalizations, and the initial weeks postdialysis initiation represent a high-risk transitional period.
Introduction
Patients on dialysis have an extremely high risk of requiring admission to an acute care hospital (hospitalization) relative to the general population.1 Over the past few decades, the dialysis population has shifted demographically to older patients with a higher number of comorbidities.2 This has led to concern that the acute hospitalization rate may rise, which would place further strain on existing health care resources. Hospitalizations denote a critical inflection point for the health of dialysis patients, as they are associated with multiple adverse clinical outcomes.3-5
Hospitalizations in dialysis patients have been tracked in the United States for many years. Data from the 2016 United States Renal Data System (USRDS) annual report showed that patients with end-stage kidney disease (ESKD) are admitted to hospital, on average, nearly twice per year, and inpatient treatment accounts for approximately 40% of all Medicare spending for dialysis patients.6 In contrast, there are limited data on the incidence and patient risk factors associated with hospitalizations in dialysis patients in Canada. It remains unclear whether the risk of hospitalization differs between the United States and Canada. There are key practice differences between the 2 countries, such as a higher prevalence of peritoneal dialysis (PD) use, broader access to predialysis care, and higher use of central venous catheters (CVC) in Canada,7 which may all modify hospitalization risks. To date, hospitalizations of dialysis patients in Canada have not been reported at a national level. Prior Canadian studies have examined only provincial or single-center level data, or have focused solely on infection-related hospitalizations.8-11 Recognizing the negative impact of hospitalizations on dialysis patient quality of life and the enormous cost burden on finite health care budgets, further studies are needed to better understand this important issue. The first step in developing strategies to improve health outcomes and reduce health care utilization in Canadian dialysis patients is a population-based study that considers different factors (demographic, comorbid disease, and dialysis-related) which may be associated with all-cause and infection-related hospitalizations.
Methods
Design and Setting
We conducted a population-based retrospective cohort study that included provinces and territories across Canada using health care databases housed at the Canadian Institute for Health Information (CIHI). Hospitalization data could not be linked for Manitoba and Quebec, so these provinces were excluded. The study was conducted according to a prespecified protocol approved by the Hamilton Integrated Research Ethics Board. The reporting of this study follows the REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) guidelines for observational studies (see Appendix A in Supplementary Material).12
Data Sources
The Canadian Organ Replacement Register (CORR) is a validated registry that includes demographics, comorbidities, dialysis modality and related outcomes, vascular access subtype, transplantation and mortality data on all ESKD patients in Canada.13,14 The ESKD is defined by the requirement for dialysis for at least 90 consecutive days. The CIHI discharge abstract database (DAD) contains diagnostic and procedure information on all hospitalizations. Hospitalization events and the reason for hospitalization were extracted from the CIHI-DAD. For the province of Ontario, hospitalization data were supplemented with the Ontario Mental Health Reporting System (OMHRS). The data sets were linked using unique encoded identifiers and analyzed at CIHI.
Study Cohort
We included all incident chronic dialysis patients with a dialysis start date between January 1, 2005, and March 31, 2014. Dialysis patients with nonlinkable health care numbers, patients residing in Quebec and Manitoba, patients simultaneously on both hemodialysis (HD) and PD, and those with a kidney transplant prior to dialysis initiation were excluded.
Hospitalizations
The primary outcomes of interest were all-cause hospitalizations and dialysis-specific infection-related hospitalizations, ie, related to a vascular access device, septicemia, or peritonitis (diagnostic codes for infection-related hospitalizations are detailed in Appendix B in Supplementary Material). The cause of hospitalization was determined using the most responsible diagnosis recorded in the DAD, which is the single diagnosis or condition described as being most responsible for the patient’s length of stay in hospital. If there were multiple diagnoses or conditions, the one most responsible for the greatest use of resources was recorded.
Statistical Analysis
Crude rates for all-cause hospitalization, infection-related hospitalization, and in-hospital mortality were determined per patient year (PPY) after dialysis initiation at 7 and 30 days, and at 3, 6, and 12 months, and reported by age group (0-17, 18-44, 45-64, ⩾65 years). A stratified, gamma-distributed frailty model was used to assess repeated hospital admissions and to appropriately handle the statistical dependence of hospitalization events within individuals, and estimate the hazard ratio (HR) attributed to each covariate of interest. The frailty model was stratified by 4 regions: Atlantic Canada; Ontario; Saskatchewan, Alberta, the Northwest Territories, and Nunavut; and British Columbia and Yukon. Patients were followed from their date of dialysis initiation until the first of kidney transplantation, withdrawal from dialysis, loss to follow-up, death, or the end of study follow-up (March 31, 2015). Demographics, comorbidities, cause of ESKD, and dialysis care type (in-center vs home) were recorded at the time of registration into CORR (ie, time of registration as a chronic dialysis patient). Dialysis modality (PD vs HD) was determined at registration into CORR and over the duration of follow-up, recognizing that many patients change dialysis modality over time. The number of predialysis hospitalizations was ascertained in the 6 months prior to dialysis initiation. Hospitalizations with an admission date prior to or on the date of dialysis initiation were treated as predialysis hospitalizations. As such, patients admitted to hospital at the time of dialysis initiation would first have to be discharged to be at risk for a hospitalization event.
The association of the following a priori covariates with all-cause hospitalization and infection-related hospitalization was determined: age (0-17, 18-44, 45-64, 65-74, ⩾75 years), sex, race (Asian, Indian subcontinent, Indigenous, black, Caucasian, other or unknown), neighborhood income quintile (derived from postal code), dialysis care type (home vs in center), cause of ESKD (glomerulonephritis, diabetes, renal vascular disease, congenital/hereditary, other, uncertain), comorbidities (cardiovascular disease, congestive heart failure, peripheral vascular disease, diabetes, malignancy, chronic obstructive pulmonary disease, hypertension defined by the need for antihypertensive therapy), time in hospital during the 6 months prior to dialysis initiation (treated as a continuous variable per week of cumulative hospital time), and dialysis modality (PD vs HD). Dialysis modality over follow-up was analyzed as a time-varying covariate.
Results
Baseline Characteristics
The final study cohort included 38 369 incident chronic dialysis patients (Supplementary Figure 1). Baseline characteristics are detailed in Table 1. Most patients were age 45 to 64 years (33.4%), male (61.0%), Caucasian (70.3%), and from the lowest income quintile (25.0%). The majority of patients were on HD (80.2%) and performed dialysis in-center (80.4%). The most common cause of ESKD was diabetes (36.1%). There was a high prevalence of hypertension (76.5%), cardiovascular disease (29.6%), and congestive heart failure (22.8%). Most patients had 1 or more hospitalizations in the 6 months prior to dialysis initiation (66.4%).
Table 1.
Patient Characteristics.
| Characteristic | Number of patients (%) |
|---|---|
| Age group | |
| 0-17 | 281 (0.7) |
| 18-44 | 4097 (10.7) |
| 45-64 | 12 798 (33.4) |
| 65-74 | 9811 (25.6) |
| ⩾75 | 11 382 (29.7) |
| Female sex | 14 979 (39) |
| Race | |
| Caucasian | 26 988 (70.3) |
| Asian | 2554 (6.7) |
| Indian subcontinent | 2044 (5.3) |
| Indigenous | 1777 (4.6) |
| Black | 1430 (3.7) |
| Other or unknown | 3576 (9.3) |
| Income quintilea | |
| 5 (high) | 5588 (14.6) |
| 4 | 6764 (17.6) |
| 3 | 7325 (19.1) |
| 2 | 8386 (21.9) |
| 1 (low) | 9587 (25.0) |
| Missing | 719 (1.9) |
| Province/territoryb | |
| British Columbia | 6696 (17.5) |
| Alberta | 4483 (11.7) |
| Saskatchewan | 1729 (4.5) |
| Ontario | 21 743 (56.7) |
| New Brunswick | 1032 (2.7) |
| Nova Scotia | 1437 (3.7) |
| Prince Edward Island | 193 (0.5) |
| Newfoundland and Labrador | 1008 (2.6) |
| Territories | 48 (0.1) |
| Modalityc | |
| HD | 30 777 (80.2) |
| PD | 7592 (19.8) |
| Care locationc | |
| In center | 30 860 (80.4) |
| Home | 7509 (19.6) |
| Cause of ESKD | |
| Diabetes | 13 863 (36.1) |
| Renal vascular disease | 7104 (18.5) |
| Glomerulonephritis | 4924 (12.8) |
| Uncertain | 3035 (7.9) |
| Congenital/hereditary | 2190 (5.7) |
| Other | 4963 (12.9) |
| Missing | 2290 (6.0) |
| Comorbidities | |
| Cardiovascular disease | 11 339 (29.6) |
| Congestive heart failure | 8757 (22.8) |
| Cerebrovascular disease | 4982 (13.0) |
| Peripheral vascular disease | 6065 (15.8) |
| Diabetesd | 4982 (13.0) |
| Malignancy | 5061 (13.2) |
| COPD | 4281 (11.2) |
| Hypertension | 29 336 (76.5) |
| Predialysis hospitalizationse | |
| 0 | 12 910 (33.6) |
| 1 | 16 070 (41.9) |
| 2 | 5931 (15.5) |
| 3 | 2150 (5.6) |
| 4 | 817 (2.1) |
| 5 | 313 (0.8) |
| 6 | 98 (0.3) |
| ⩾7 | 80 (0.2) |
Note. All variables are captured at the start of dialysis. HD = hemodialysis; PD = peritoneal dialysis; ESKD = end-stage kidney disease; COPD = chronic obstructive pulmonary disease.
Patient level household income is an estimate using neighborhood income levels.
Province/territory is determined by issuance of health card.
Dialysis modality and care location were determined at baseline. In-center care location was assigned to patients on HD or PD receiving total in-center care at the time of dialysis initiation.
The diabetes comorbidity variable excludes patients with a primary ESKD diagnosis of diabetes.
Denotes the number of hospital admissions within 6 months before the first dialysis treatment.
Hospitalizations
During the study period, there were 112 374 hospitalizations, and 12 931 (11.5%) of these hospitalizations were dialysis-specific infection-related hospitalizations. Among pediatric patients (age 0-17 years), kidney disease was listed as the most responsible diagnosis for 290 (25.7%) hospitalizations and dialysis-specific infections were listed for 132 (11.7%) hospitalizations. Among patients age 18 to 64 years, kidney disease was the most responsible diagnosis for 3399 (6.2%) hospitalizations, and dialysis-specific infections were listed for 5413 (9.9%) hospitalizations. Other common most responsible diagnoses in patients age 18 to 64 years were diabetes (7908; 14.5% of hospitalizations) and cardiovascular disease (angina and myocardial infarction: 1809; 3.3% of hospitalizations). Among patients age 65 years and older, dialysis-specific infections (5140; 9.1%), diabetes (4311; 7.6%), cardiovascular disease (2975; 5.3%), and kidney disease (1823; 3.2%) were the most common most responsible diagnoses for hospitalizations.
Crude all-cause and infection-related hospitalization rates and all-cause in-hospital mortality rates by age group are presented in Figure 1 and Supplementary Tables 1 to 3. The all-cause hospitalization rate was similar for the 3 adult age groups and declined slightly over time (age 65 years and older: 1.40, 1.35, and 1.18 admissions PPY at 7 days, 30 days, and 6 months postdialysis initiation). Compared with all adult age groups, the all-cause hospitalization rate for pediatric patients was slightly higher at 7 days postdialysis initiation (1.67 admissions PPY), increased thereafter, and remained much higher over time (2.48 and 2.47 admissions PPY at 30 days and 6 months postdialysis initiation, respectively). Within the first 30 days of dialysis initiation, the infection-related hospitalization rate in pediatric patients consistently increased, surpassing the rate in all adult age groups at >30 days postdialysis initiation (ages 0-17 years: 0.00 PPY at 7 days, 0.13 PPY at 30 days, 0.21 PPY at 6 months; ages 45-64 years: 0.12 PPY at 7 days, 0.13 PPY at 30 days, 0.12 PPY at 6 months). The infection-related hospitalization rate was similar across all adult age groups and remained stable over time. The all-cause in-hospital mortality rate was highest in elderly (age ⩾65) dialysis patients and lowest in pediatric patients over the entire follow-up (at 1 year; ages 0-17 years: 0.01 PPY, age 65 years and older: 0.13 PPY).
Figure 1.
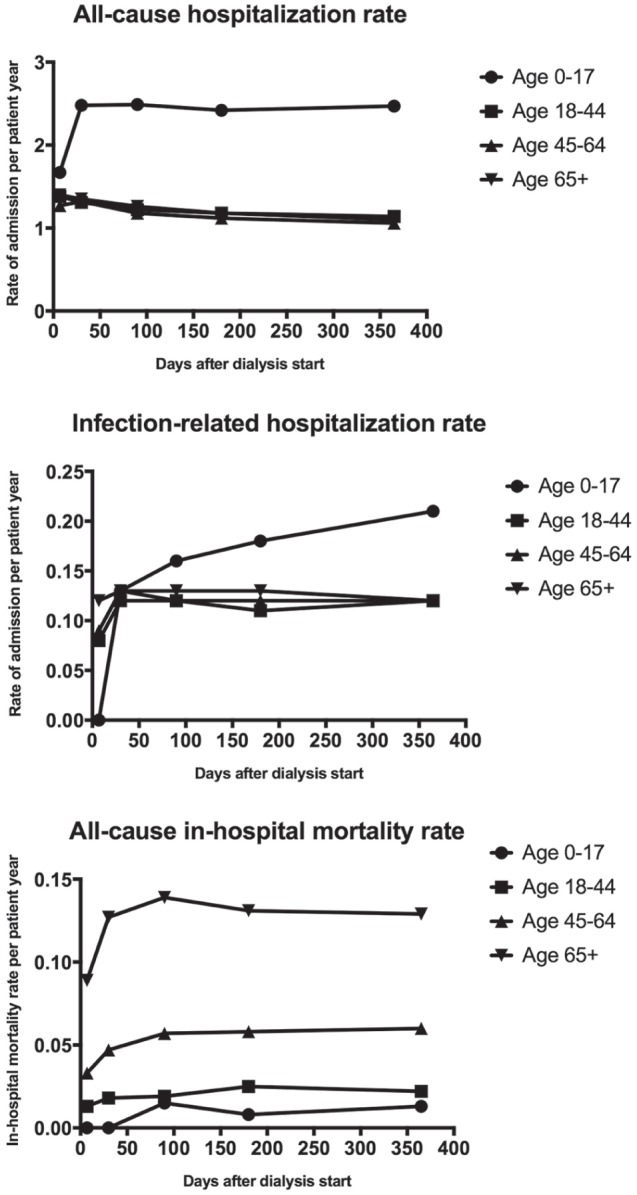
Crude hospitalization and in-hospital mortality rates over time by age group.
Risk Factors for Hospitalization
The adjusted HRs for all-cause and infection-related hospitalizations for each covariate of interest are presented in Table 2. The HRs for dialysis modality as a time-varying covariate are presented separately in Figure 2 and Supplementary Table 4. Compared with dialysis patients age 45 to 64 years (referent), pediatric patients (HR: 2.73, 95% confidence interval [CI]: 2.37-3.15) and 18- to 44-year-old patients (HR: 1.21, 95% CI: 1.15-1.27) had a higher risk of all-cause hospitalization. Patients age 65 to 74 years had a lower risk (HR: 0.95, 95% CI: 0.91-0.98). When limited to infection-related hospitalization, the trends were similar, though not statistically significant. Female dialysis patients had a higher risk of all-cause hospitalization (HR: 1.08, 95% CI: 1.05-1.11) but not infection-related hospitalization. Compared with Caucasians, Indigenous patients had a higher risk of all-cause hospitalization (HR: 1.20, 95% CI: 1.12-1.28), while other races had a lower risk. The risk of infection-related hospitalization was significantly higher in Indigenous patients (HR: 1.30, 95% CI: 1.11-1.53) and lower in Asian patients (HR: 0.76, 95% CI: 0.65-0.89) compared with Caucasians. Patients with ESKD secondary to diabetes were at increased risk, and patients with congenital or hereditary kidney disease were at lower risk for all-cause and infection-related hospitalizations compared with patients with glomerulonephritis. Patients who had dialysis treatments at home were at lower risk for all-cause hospitalization (HR: 0.84, 95% CI: 0.79-0.88) and infection-related hospitalization. Every week spent in hospital in the 6 months prior to dialysis initiation increased the risk of all-cause hospitalization following dialysis initiation by 2% and infection-related hospitalization by 5%. Patients on HD and PD had a decline in the risk of all-cause hospitalization over time (HD: HRs 0.76 and 0.53 at 8-30 days and 6-12 months respectively; PD: HRs 0.73 and 0.56 at 8-30 days and 6-12 months respectively; referent group: HD at ⩽7 days). Within the first 7 days after dialysis initiation, patients on PD had a higher risk of all-cause hospitalization (HR: 1.27, 95% CI: 1.07-1.50) and infection-related hospitalization (HR: 2.05, 95% CI: 1.19-3.55).
Table 2.
Risk Factors for Hospitalization.
| All-cause
hospitalization Adjusted HR (95% CI) |
Infection-related
hospitalization Adjusted HR (95% CI) |
|
|---|---|---|
| Age group | ||
| 0-17 | 2.73 (2.37-3.15) | 1.30 (0.90-1.88) |
| 18-44 | 1.21 (1.15-1.27) | 1.03 (0.90-1.16) |
| 45-64 | Referent | Referent |
| 65-74 | 0.95 (0.91-0.98) | 0.96 (0.88-1.06) |
| ⩾75 | 1.01 (0.97-1.05) | 1.02 (0.92-1.12) |
| Sex | ||
| Female | 1.08 (1.05-1.11) | 1.03 (0.96-1.11) |
| Race | ||
| Asian | 0.72 (0.68-0.77) | 0.76 (0.65-0.89) |
| Indian subcontinent | 0.78 (0.73-0.84) | 0.86 (0.73-1.02) |
| Indigenous | 1.20 (1.12-1.28) | 1.30 (1.11-1.53) |
| Black | 0.86 (0.80-0.93) | 0.98 (0.81-1.18) |
| Caucasian | Referent | Referent |
| Income quintilea | ||
| 5 (high) | 1.02 (0.97-1.06) | 1.07 (0.95-1.20) |
| 4 | 0.96 (0.92-1.01) | 0.98 (0.87-1.09) |
| 3 | 0.97 (0.93-1.01) | 1.00 (0.90-1.12) |
| 2 | 0.98 (0.94-1.02) | 1.05 (0.95-1.17) |
| 1 (low) | Referent | Referent |
| Dialysis care location | ||
| Home | 0.84 (0.79-0.88) | 0.85 (0.75-0.97) |
| Cause of ESKD | ||
| Glomerulonephritis | Referent | Referent |
| Diabetes | 1.17 (1.11-1.22) | 1.17 (1.03-1.33) |
| Renal vascular disease | 1.00 (0.95-1.06) | 0.95 (0.82-1.09) |
| Congenital/hereditary | 0.92 (0.85-0.99) | 0.78 (0.64-0.95) |
| Comorbidities | ||
| Cardiovascular disease | 1.14 (1.10-1.18) | 1.05 (0.96-1.14) |
| Congestive heart failure | 1.13 (1.09-1.17) | 1.04 (0.95-1.14) |
| Cerebrovascular disease | 1.06 (1.01-1.10) | 1.07 (0.96-1.19) |
| Peripheral vascular disease | 1.16 (1.12-1.21) | 1.17 (1.06-1.29) |
| Diabetesb | 1.10 (1.05-1.15) | 1.27 (1.13-1.42) |
| Malignancy | 1.21 (1.16-1.26) | 1.19 (1.07-1.33) |
| COPD | 1.15 (1.10-1.21) | 1.21 (1.08-1.36) |
| Hypertension | 0.90 (0.87-0.94) | 0.84 (0.76-0.93) |
| Predialysis hospitalization | ||
| Every week in hospital prior to dialysis start | 1.02 (1.02-1.03) | 1.05 (1.04-1.06) |
Note. HR = hazard ratio; CI = confidence interval; ESKD = end-stage kidney disease; COPD = chronic obstructive pulmonary disease.
Patient level household income is an estimate using neighborhood income levels.
The diabetes comorbidity covariate excludes patients with a primary ESKD diagnosis of diabetes.
Figure 2.
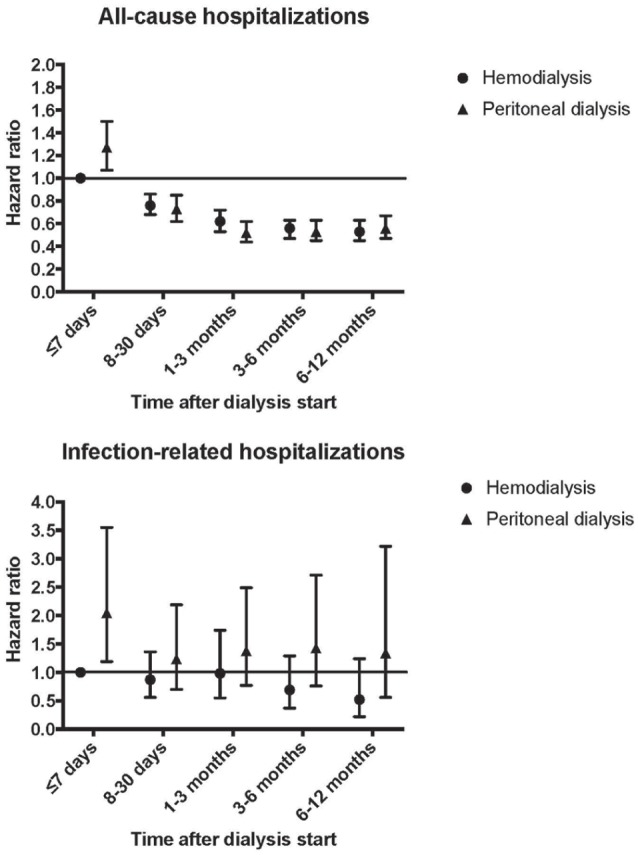
Comparative risk of hospitalization over time by modality type.
Discussion
In this analysis of 38 369 incident chronic dialysis patients in Canada with 112 374 hospitalizations, we found that many hospitalizations (11.5%) were attributable to dialysis-specific infections. We were able to characterize risk factors for hospitalization, including Indigenous race, female sex, and younger age. Patients on PD had a significantly higher risk of all-cause and infection-related hospitalizations within the first 7 days of dialysis initiation. Beyond 7 days, the risk of hospitalization did not differ significantly by dialysis modality, but there was a trend toward an increased risk of infection-related hospitalization in patients on PD. The all-cause hospitalization rate was time-dependent and noted to be highest shortly after starting dialysis.
The hospitalization rates in our study of Canadian dialysis patients are comparable but slightly lower than those described in the most recent reports from the USRDS.6,15 In our study, adult patients had a hospitalization rate ranging from 1.1 to 1.4 PPY. Comparatively, the USRDS reported a rate for patients on HD and PD of 1.7 and 1.6 hospitalizations PPY, respectively.6 European countries participating in the Dialysis Outcomes and Practice Patterns Study (DOPPS) reported a lower hospitalization rate for patients on HD of 0.99 PPY. However, this is a point prevalent rate, which may explain why the DOPPS rate is lower.16 Similar to our study, the USRDS reported a higher hospitalization rate in pediatric dialysis patients (2.0 PPY).6 Our hospitalization rate for elderly dialysis patients (⩾65 years) is similar to a prior American study that reported a rate of 1.5 PPY.17 We report an infection-related hospitalization rate in adult patients of 0.08 to 0.13 PPY, which is slightly higher than a prior study that examined dialysis patients in Quebec, Canada, and reported a rate of 0.05 PPY for dialysis-specific infectious hospitalizations.8 The decline in hospitalization risk seen with increasing age is likely at least partly explained by the competing risk of death.
We found a higher risk of all-cause hospitalization in patients on PD compared with patients on HD during the first 7 days on dialysis. The risk for infection-related hospitalization in patients on PD was particularly high during this initial time period on dialysis. This increased risk in patients on PD is consistent with a prior study demonstrating that most hospitalizations and episodes of peritonitis in patients on PD occur within the first 6 months on dialysis.18 Our finding of a higher risk of infection-related hospitalization in patients on PD is consistent with prior studies by Lafrance et al9 and van Diepen et al,19 but not consistent with a study by Williams et al11 that showed no difference between patients on HD and PD, and a study by Quinn et al10 that showed an increased risk in patients on HD. Discrepant results between studies could be due to a number of reasons. Risk may vary across jurisdictions due to differing practice patterns. Failure to examine risk by time on dialysis could alter results; our results show that the risk of infection-related hospitalization in patients on PD lowers once on dialysis for greater than a week. This initial higher risk may be a true association but may also be explained by the fact that more patients initiate HD (rather than PD) during a hospitalization. If a patient were already hospitalized at the time of dialysis initiation (admission date prior to or on dialysis start date), this would be captured as a predialysis hospitalization, and the patient would not be at risk for a hospitalization event until after discharge. Failure to treat dialysis modality as a time dependent covariate could affect results, as patients often change dialysis modality over time. The definition of infection-related hospitalization is also important. Some studies included nondialysis related infections in the definition of infection-related hospitalization. Patients on PD may be at decreased risk for pneumonia but increased risk for dialysis-related infections,9,19 highlighting the importance of reporting dialysis and nondialysis infection-related hospitalizations separately. Rates could also differ across studies depending on how study populations are defined (ie, incident vs prevalent dialysis patients).
We found that Indigenous dialysis patients were at increased risk for hospitalizations. Potential reasons for this could include socioeconomic factors, geographic isolation limiting access to medical care, and comorbidity burden. A study in the United States found that Indigenous patients were more likely to miss or shorten HD treatments and that doing so had an escalating effect on hospitalization rates.20,21 Contrary to our findings, the 2017 USRDS report did not find that Indigenous dialysis patients were at increased risk for hospitalizations; however; the USRDS analysis by race did not include patients on PD, which could potentially explain the discrepant results.15 A study from the Australia and New Zealand Dialysis and Transplant Registry (ANZDATA) found that Indigenous patients on PD living in remote areas had a higher risk of PD-related complications.22 We did not specifically examine this subgroup, but a high hospitalization rate in this group of patients could be one of the factors driving the increased hospitalization risk in Canadian Indigenous patients. We also found that female patients were at higher risk. The reasons for this requires further study, but this finding was also highlighted in the 2017 USRDS report, where a 17.5% higher hospitalization rate was reported for female compared with male HD patients.15
Reporting on hospitalizations in dialysis patients is important to inform strategies to reduce preventable hospitalizations and readmissions. The United States has long been tracking hospitalizations in dialysis patients and has reported a 19% decline from 2005 to 2014.6 This is the first national study of hospitalizations in dialysis patients in Canada and highlights the need for further studies to determine strategies that may reduce hospitalizations for incident dialysis patients. Proposed strategies may include enhanced monitoring by health care professionals, ensuring patients on home dialysis are properly trained, and appropriately following guidelines for the prevention of dialysis access–related infections.4,23-28 Among patients on HD, strategies aimed at increasing arteriovenous fistula (AVF) use may help to reduce infection-related hospitalizations. An international study using DOPPS data from 20 countries found that Canada had the lowest AVF use at 49% and the highest central venous catheter use at 45%.29 Our study also highlights the important issue of hospitalizations in pediatric dialysis patients, with a large proportion of hospitalizations primarily due to kidney-related or dialysis-related problems. This is clearly a unique patient population with its own set of challenges compared with the adult ESKD population. In addition to enhanced monitoring, education, and infection prevention measures, strategies such as increased uptake of frequent home HD for improved volume control may help to reduce admissions.30 Aggressively minimizing time spent on dialysis by optimizing access to kidney transplantation should also be a key objective in pediatric patients. Overall, there is a paucity of data on hospitalizations in pediatric patients; further study is needed to understand this important issue.
Our study has important limitations. The cohort had too few home HD patients to examine this subgroup. Patients on home HD have been previously found to have a lower risk of hospitalizations compared with patients on PD, and a lower risk of cardiovascular hospitalizations but higher risk of infection-related hospitalizations.30-32 Characteristics previously found to be associated with hospitalizations, such as frailty, serum ferritin, and serum sodium, were not examined.33-36 Data on patient adherence with prescribed treatments and individual dialysis prescriptions were also not available. The outcome of infection-related hospitalization was determined using diagnostic codes with uncertain validity. We did not have access to culture results or clinical data to confirm the diagnosis of a dialysis-related infection.
Conclusions
This national study highlights the important issue of hospitalizations in chronic dialysis patients. The rates of hospitalization were not influenced by dialysis modality beyond the initial 7 days following dialysis initiation. Pediatric, Indigenous, and female patients are at higher risk for hospitalizations, and the initial weeks postdialysis initiation represent a high-risk transitional period.
Supplemental Material
Supplemental material, Appendices_(1) for Hospitalizations in Dialysis Patients in Canada: A National Cohort Study by Amber O. Molnar, Louise Moist, Scott Klarenbach, Jean-Philippe Lafrance, S. Joseph Kim, Karthik Tennankore, Jeffrey Perl, Joanne Kappel, Michael Terner, Jagbir Gill, and Manish M. Sood in Canadian Journal of Kidney Health and Disease
Acknowledgments
We would like to acknowledge Naisu Zhu along with the entire Expert Advisory Group for its invaluable advice on the report from the Canadian Institute for Health Information titled High Risk and High Cost: Focus on Opportunities to Reduce Hospitalizations of Dialysis Patients in Canada, 2016. We also acknowledge Frank Ivis, Kelvin Lam, Noura Redding, Greg Webster, Juliana Wu, and Susan Samuel for their important contributions.
Footnotes
Ethics Approval and Consent to Participate: The conduct of this study was approved by the Hamilton Integrated Research Ethics Board. There was no direct patient contact; therefore, individual patient consent was not required.
Consent for Publication: All authors consent to the publication of this study.
Availability of Data and Materials: Privacy regulations of the Canadian Institute for Health Information do not allow for the release of the original data.
Author Contributions: AOM and MMS drafted the initial version of the manuscript. LM, SK, JPL, SJK, KT, JP, JK, MT, JG, and MMS were involved with the study design, analysis, and interpretation of the data. All authors reviewed the final version of the manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Amber O. Molnar is supported by the KRESCENT Foundation. Manish M. Sood is supported by the Jindal Research Chair for the Prevention of Kidney Disease. All funders had no role in the study design, analysis, interpretation, or writing of the manuscript.
References
- 1. Daratha KB, Short RA, Corbett CF, et al. Risks of subsequent hospitalization and death in patients with kidney disease. Clin J Am Soc Nephrol. 2012;7:409-416. [DOI] [PubMed] [Google Scholar]
- 2. van Walraven C, Manuel DG, Knoll G. Survival trends in ESRD patients compared with the general population in the United States. Am J Kidney Dis. 2014;63:491-499. [DOI] [PubMed] [Google Scholar]
- 3. Laurin LP, Harrak H, Elftouh N, Ouimet D, Vallée M, Lafrance JP. Outcomes of infection-related hospitalization according to dialysis modality. Clin J Am Soc Nephrol. 2015;10:817-824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Plantinga LC, Jaar BG. Preventing repeat hospitalizations in dialysis patients: a call for action. Kidney Int. 2009;76:249-251. [DOI] [PubMed] [Google Scholar]
- 5. Plantinga LC, King L, Patzer RE, et al. Early hospital readmission among hemodialysis patients in the United States is associated with subsequent mortality. Kidney Int. 2017;92:934-941. [DOI] [PubMed] [Google Scholar]
- 6. United States Renal Data System. 2016 USRDS annual data report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2016. [Google Scholar]
- 7. Robinson BM, Akizawa T, Jager KJ, Kerr PG, Saran R, Pisoni RL. Factors affecting outcomes in patients reaching end-stage kidney disease worldwide: differences in access to renal replacement therapy, modality use, and haemodialysis practices. Lancet (London, England). 2016;388:294-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lafrance JP, Rahme E, Iqbal S, Elftouh N, Laurin L-P, Vallée M. Trends in infection-related hospital admissions and impact of length of time on dialysis among patients on long-term dialysis: a retrospective cohort study. CMAJ Open. 2014;2:E109-E114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lafrance JP, Rahme E, Iqbal S, et al. Association of dialysis modality with risk for infection-related hospitalization: a propensity score-matched cohort analysis. Clin J Am Soc Nephrol. 2012;7:1598-1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Quinn RR, Ravani P, Zhang X, et al. Impact of modality choice on rates of hospitalization in patients eligible for both peritoneal dialysis and hemodialysis. Perit Dial Int. 2014;34:41-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Williams VR, Quinn R, Callery S, Kiss A, Oliver MJ. The impact of treatment modality on infection-related hospitalization rates in peritoneal dialysis and hemodialysis patients. Perit Dial Int. 2011;31:440-449. [DOI] [PubMed] [Google Scholar]
- 12. Reis Filho JR, Cardoso JN, Cardoso CM, dos Reis Cardoso CM, Pereira-Barretto AC. Reverse cardiac remodeling: a marker of better prognosis in heart failure. Arq Bras Cardiol. 2015;104:502-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moist LM, Richards HA, Miskulin D, et al. A validation study of the Canadian Organ Replacement Register. Clin J Am Soc Nephrol. 2011;6:813-818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Canadian Institute for Health Information. Canadian Organ Replacement Register Annual Report: Treatment of End-Stage Organ Failure in Canada, 2005 to 2014. Ottawa, ON: CIHI, 2016. [Google Scholar]
- 15. United States Renal Data System. 2017 USRDS annual data report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2017. [Google Scholar]
- 16. Rayner HC, Pisoni RL, Bommer J, et al. Mortality and hospitalization in haemodialysis patients in five European countries: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant. 2004;19:108-120. [DOI] [PubMed] [Google Scholar]
- 17. Schoonover KL, Hickson LJ, Norby SM, et al. Risk factors for hospitalization among older, incident haemodialysis patients. Nephrology (Carlton, Vic). 2013;18:712-717. [DOI] [PubMed] [Google Scholar]
- 18. Pulliam J, Li NC, Maddux F, Hakim R, Finkelstein FO, Lacson E., Jr. First-year outcomes of incident peritoneal dialysis patients in the United States. Am J Kidney Dis. 2014;64:761-769. [DOI] [PubMed] [Google Scholar]
- 19. van Diepen AT, Hoekstra T, Rotmans JI, et al. The association between dialysis modality and the risk for dialysis technique and non-dialysis technique-related infections. Nephrol Dial Transplant. 2014;29:2244-2250. [DOI] [PubMed] [Google Scholar]
- 20. Obialo C, Zager PG, Myers OB, Hunt WC. Relationships of clinic size, geographic region, and race/ethnicity to the frequency of missed/shortened dialysis treatments. J Nephrol. 2014;27:425-430. [DOI] [PubMed] [Google Scholar]
- 21. Obialo CI, Hunt WC, Bashir K, Zager PG. Relationship of missed and shortened hemodialysis treatments to hospitalization and mortality: observations from a US dialysis network. Clin Kidney J. 2012;5:315-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lim WH, Boudville N, McDonald SP, Gorham G, Johnson DW, Jose M. Remote indigenous peritoneal dialysis patients have higher risk of peritonitis, technique failure, all-cause and peritonitis-related mortality. Nephrol Dial Transplant. 2011;26:3366-3372. [DOI] [PubMed] [Google Scholar]
- 23. Collier S, Davenport A. Reducing the risk of infection in end-stage kidney failure patients treated by dialysis. Nephrol Dial Transplant. 2014;29:2158-2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Erickson KF, Winkelmayer WC, Chertow GM, Bhattacharya J. Hemodialysis hospitalizations and readmissions: the effects of payment reform. Am J Kidney Dis. 2017;69:237-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Piraino B, Bernardini J, Brown E, et al. ISPD position statement on reducing the risks of peritoneal dialysis-related infections. Perit Dial Int. 2011;31:614-630. [DOI] [PubMed] [Google Scholar]
- 26. Lata C, Girard L, Parkins M, James MT. Catheter-related bloodstream infection in end-stage kidney disease: a Canadian narrative review. Can J Kidney Health Dis. 2016;3:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wong B, Muneer M, Wiebe N, et al. Buttonhole versus rope-ladder cannulation of arteriovenous fistulas for hemodialysis: a systematic review. Am J Kidney Dis. 2014;64:918-936. [DOI] [PubMed] [Google Scholar]
- 28. Yon CK, Low CL. Sodium citrate 4% versus heparin as a lock solution in hemodialysis patients with central venous catheters. Am J Health Syst Pharm. 2013;70:131-136. [DOI] [PubMed] [Google Scholar]
- 29. Pisoni RL, Zepel L, Port FK, Robinson BM. Trends in US vascular access use, patient preferences, and related practices: an update from the US DOPPS practice monitor with international comparisons. Am J Kidney Dis. 2015;65:905-915. [DOI] [PubMed] [Google Scholar]
- 30. Suri RS, Li L, Nesrallah GE. The risk of hospitalization and modality failure with home dialysis. Kidney Int. 2015;88:360-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Weinhandl ED, Gilbertson DT, Collins AJ. Mortality, hospitalization, and technique failure in daily home hemodialysis and matched peritoneal dialysis patients: a matched cohort study. Am J Kidney Dis. 2016;67:98-110. [DOI] [PubMed] [Google Scholar]
- 32. Weinhandl ED, Nieman KM, Gilbertson DT, Collins AJ. Hospitalization in daily home hemodialysis and matched thrice-weekly in-center hemodialysis patients. Am J Kidney Dis. 2015;65:98-108. [DOI] [PubMed] [Google Scholar]
- 33. Kato S, Lindholm B, Yuzawa Y, et al. High ferritin level and malnutrition predict high risk of infection-related hospitalization in incident dialysis patients: a Japanese prospective cohort study. Blood Purif. 2016;42:56-63. [DOI] [PubMed] [Google Scholar]
- 34. Kuragano T, Matsumura O, Matsuda A, et al. Association between hemoglobin variability, serum ferritin levels, and adverse events/mortality in maintenance hemodialysis patients. Kidney Int. 2014;86:845-854. [DOI] [PubMed] [Google Scholar]
- 35. Mandai S, Kuwahara M, Kasagi Y, et al. Lower serum sodium level predicts higher risk of infection-related hospitalization in maintenance hemodialysis patients: an observational cohort study. BMC Nephrol. 2013;14:276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. McAdams-DeMarco MA, Law A, Salter ML, et al. Frailty as a novel predictor of mortality and hospitalization in individuals of all ages undergoing hemodialysis. J Am Geriatr Soc. 2013;61:896-901. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Appendices_(1) for Hospitalizations in Dialysis Patients in Canada: A National Cohort Study by Amber O. Molnar, Louise Moist, Scott Klarenbach, Jean-Philippe Lafrance, S. Joseph Kim, Karthik Tennankore, Jeffrey Perl, Joanne Kappel, Michael Terner, Jagbir Gill, and Manish M. Sood in Canadian Journal of Kidney Health and Disease


