Abstract
Background:
Functional disability is defined as the need for assistance with self-care tasks.
Objective:
To document changes in functional status over time among older prevalent renal transplant recipients.
Design:
Single center, prospective, follow-up study.
Setting:
Single center, tertiary care transplant center.
Patients:
Patients, with a functioning kidney transplant, aged 65 years or older who underwent assessment of functional status approximately 12 months previously.
Measurements:
Validated tools used included Barthel Index, the Lawton-Brody Scale of Instrumental Activities of Daily Living, the Timed Up and Go test, the Veterans Specific Activity Questionnaire, the Mini-Cog, and dynamometer handgrip strength.
Methods:
Outpatient assessment by a trained observer.
Results:
Of the 82 patients previously studied, 64 (78%) patients participated in the follow-up study (mean age 70.5 ± 4.4 years, 58% male, 55% diabetic). Among those completing functional status measures, 32 (50%) had functional disability at baseline. Over the 1-year period, 11 (17%) of these patients experienced progressive functional decline, 6 (9%) exhibited no change, and 15 (23%) had functional recovery. Eleven patients (17%) initially independent, developed new-onset disability. One of the strongest predictors of progressive functional decline was having 1 or more falls in the previous year.
Limitations:
Assessments were performed only on 2 occasions separated by approximately 1 year.
Conclusions:
Fluctuations in disability states are common among older adults living with renal transplants. Episodes of functional disability may place individuals at higher risk of persistent and/or progressive disability.
Keywords: elderly, functional dependence, geriatric, kidney transplant
Abrégé
Contexte:
La déficience fonctionnelle se définit comme le besoin pour une personne d’être assistée dans ses activités et soins quotidiens.
Objectifs de l’étude:
L’étude visait à documenter les variations dans l’état fonctionnel qui se constatent au fil du temps chez les personnes âgées receveuses d’une greffe rénale.
Type et cadre de l’étude:
Il s’agit d’une étude de suivi prospective qui s’est tenue dans un seul centre de soins tertiaires en transplantation.
Participants:
Une cohorte de patients âgés de 65 ans et plus ayant reçu une greffe rénale et dont l’évaluation de l’état fonctionnel avait été faite dans les 12 mois précédant l’intervention.
Mesures:
Les outils validés suivants ont servi à colliger les données : l’indice Barthel, l’échelle d’activités instrumentales de la vie courante de Lawton (IDAL - Lawton-Brody Scale of Instrumental Activities of Daily Living), le test chronométré du lever de chaise (timed up and go test), le Veterans Specific Activity Questionnaire, le test Mini-Cog et le test de force de préhension au dynamomètre.
Méthodologie:
L’évaluation des patients externes a été effectuée par un observateur formé à cet effet.
Résultats:
Des 82 patients étudiés précédemment, 64 (78 %) ont participé à l’étude de suivi; leur âge moyen était de 70,5 ± 4,4 ans, 58 % étaient des hommes et 55 % souffraient de diabète. Parmi les patients qui ont complété les mesures de l’état fonctionnel, 32 (50 %) présentaient des déficiences fonctionnelles au départ. Au cours de l’année, 11 (17 %) patients ont vu leur état fonctionnel décliner progressivement, 6 (9 %) n’ont connu aucun changement de leur état et 15 (23 %) ont vu leur capacité fonctionnelle rétablie. Par ailleurs, au cours de la même période, on a constaté l’apparition d’une nouvelle incapacité pour onze patients (17 %) considérés au départ comme indépendants. On a observé que le fait d’avoir chuté une ou plusieurs fois au cours de l’année précédente s’avérait l’un des meilleurs facteurs prédictifs d’un déclin fonctionnel progressif.
Limites de l’étude:
L’évaluation des patients n’a été réalisée qu’à deux reprises, et celles-ci étaient séparées d’une période d’environ un an.
Conclusion:
Les variations de l’état fonctionnel sont fréquentes chez les personnes âgées ayant subi une transplantation rénale. Les épisodes d’incapacité fonctionnelle sont susceptibles d’exposer le patient à un plus grand risque de déclin fonctionnel persistant ou progressif.
What was known before
Previous studies have shown that more than half of older renal transplant recipients have functional disability and/or accidental falls.
What this adds
We found that more than 30% of those who had disability at baseline, had persistent or worsening disability after one year despite ongoing stable kidney transplant function. Our data suggest that individuals with a history of one or more accidental falls, and those with abnormal physical performance testing at a clinic visit, may be more prone to persistent or progressive functional loss suggesting an opportunity for detection, and possibly intervention.
Introduction
Kidney transplantation offers the best chance of long-term survival and improved quality of life of all treatment modalities offered to patients with end-stage renal disease. In recent years, United States Renal Data System (USRDS) data suggest the number of individuals living with a functioning kidney transplant, who are aged 65 years or more, is increasing both because of improved patient and graft survival and because transplantation continues to be offered as readily to older individuals.1 Thus, health-related problems associated with aging, such as functional loss, are increasingly recognized.
Functional status reflects a person’s ability to complete their self-care tasks independently. It declines with age and with chronic ill health.2,3 Moreover, persistent functional disability, in the general population, is strongly associated with a range of important health outcomes such as hospitalization, need for long-term care, and mortality.4-6 We previously performed a cross-sectional study of individuals, aged 65 years or older, who had a functioning kidney transplant, and found a surprisingly high level of functional disability.7 A total of 54% of patients reported functional disability, while 21% reported having had an accidental fall in the previous 12 months. These data, however, were cross-sectional, and the literature in the general population suggests that functional disability at a single time point does not imply inevitable progression.8-11 Often disability can be transient and reversible in nature. We, therefore, sought to identify whether the functional status remained stable or improved in these individuals using a prospective longitudinal study design. Secondary objectives included reassessing the fall risk in this patient population, as well as identification of markers or predictors of subsequent functional decline.
Patients and Methods
Study Population
Over the period June 15, 2012, to August 15, 2012, all patients aged 65 years or more attending a kidney transplant follow-up appointment at the University Health Network (UHN) were approached to participate in a project to evaluate functional status in older transplant recipients. All previous participants were eligible for recruitment into the current follow-up study.
In the initial study published in 2014,7 patients were considered eligible if they had previously undergone kidney transplantation, were living in the community, and were aged 65 years or more at the time of the clinic visit. For the current study, patients who had previously participated, and in whom, at least 12 months had elapsed since their initial assessment were approached. For convenience, most study patients chose to undergo reassessment during the period June 1, 2013, to January 15, 2014, at a time when they were attending an outpatient follow-up clinic at UHN. Individuals who were unable to communicate in English were assisted by a translator.
Study Procedures
The study methodology has been reported previously.7 Eligible patients were approached in clinic and invited to participate in the follow-up study. Informed consent was sought. Additional clinical data were extracted from the clinical charts including the most recent hemoglobin (Hb), serum creatinine (SCr), serum albumin (Alb), current medications, and the cumulative dose of prednisone taken over the previous 6 months. As before, functional assessment tools included the Barthel Index,12 the Lawton-Brody Scale of Instrumental Activities of Daily Living,13 the timed up and go (TUG) test,14 and dynamometer handgrip strength.15,16 In addition to baseline functional assessments, patients were asked to complete the Veterans Specific Activity Questionnaire (VSAQ)17,18 and the Mini-Cog19,20 and to recall whether they had experienced any falls since last assessment.
The VSAQ was added to the assessment protocol to gather further data about physical ability as a substantial proportion of patients, in the initial study, were found to be fully independent in both basic activities of daily living and instrumental activities of daily living. The VSAQ is a 13-item instrument that assesses an individual’s peak level of physical activity. It has been used to estimate exercise capacity, predict peak metabolic equivalents (METS), and measure peak oxygen uptake (VO2).17,18 It is a patient-administered questionnaire that lists a number of physical activities that correspond to different METS. Patients mark the highest level of activity that they would be able to do without symptoms such as fatigue, chest discomfort, or shortness of breath. Results are scored using a standardized system (VSAQmax). Additional testing for cognitive function was also included to assess whether patients with functional disability had concomitant cognitive dysfunction. The Mini-Cog was chosen as it is a validated, sensitive and specific, rapid screening tool used to identify patients with cognitive impairment or dementia across a wide range of abilities.20 It is also applicable across different cultural and educational levels and minimally influenced by English language fluency. The test comprises 3-word recall and clock drawing performed in a standardized fashion. The Mini-Cog assesses attention, executive function, and memory.
All functional assessments were conducted by 1 of 2 trained assessors (K.Y. and J.F.F.) using a standardized protocol.
Definitions Used
Disability was measured as a categorical variable (no disability vs disability) using the principles of the disability staging model.21,22 Patients were defined as having no disability if they were independent in all activities of daily living on both the Barthel Index and Lawton-Brody IADL scales, and as having disability if they were dependent in at least 1 activity of daily living on these scales.
Functional decline was defined as a net loss of independence in ≥1 activity of daily living over the follow-up period, while functional improvement was a net gain of independence in ≥1 activity of daily living. Progressive decline was used to refer to individuals who had disability in at least 1 activity of daily living at baseline and who demonstrated a net loss of ≥1 activity at the follow-up assessment.
Handgrip strength was interpreted against population norms using standardized methods.15 Individuals with handgrip strength readings that were below the 10th percentile compared with age-matched and gender-matched normative data were said to have significant muscle strength impairment. Those at or above the 10th percentile were defined as normal.
TUG test results were categorized into 3 groups: those with optimal functional mobility speed (<10 seconds), those with borderline impairment (10 to 15 seconds), and those who had significant impairment (>15 seconds).
The VSAQmax score was used to predict exercise capacity using the validated equation:
For the purposes of the study, patients were stratified into 3 groups (low, medium, and high exercise capacity) based on their predicted METS (defined as <5 METS, 5 to 8 METS, and >8 METS, respectively).
Cognition was scored using previously validated methods.19,20 Patients were determined to have normal cognition if able to recall of all 3 words on the Mini-Cog. Patients were determined to have abnormal cognition if unable to recall any of the 3 words on the Mini-Cog. For those who had intermediate word recall (1 to 2 words), the clock-drawing test was used to categorize results. The clock-drawing test was scored as either normal or abnormal, depending on the accuracy and placement of the numbers and hands of the clock. If the participant was unable to complete the clock after 2 minutes, the result was categorized as abnormal.19,20
Sample Size and Data Analysis
The sample size was contingent on the number of patients previously studied and willing to be reapproached.
Demographic and descriptive data were analyzed and reported using percentages for categorical variables, and using mean (± standard deviation) or median (with interquartile range) as appropriate for continuous variables. Changes between baseline and follow-up were compared using a paired t test or Wilcoxon signed rank test for continuous variables, and McNemar test for categorical variables. Exploratory associations between the reported change in disability and objective measures of function (TUG, handgrip strength) were assessed graphically and analyzed using correlation statistics (Pearson’s correlation coefficient). Comparisons between individuals completing follow-up compared with those who did not were tested using chi-squared and Fisher exact tests for categorical variables (gender, cause of end-stage renal disease), and Student t test or Wilcoxon signed rank test for continuous variables (age, cumulative prednisone dose, years since transplantation). A 2-sided P value of <.05 was considered statistically significant. The study was approved by the local hospital Research Ethics Committee.
Results
Of the 82 patients who participated in the first study, 65 (79%) agreed to participate. Reasons for nonparticipation included no opportunity to recruit (n = 11), death (n = 1), and unwillingness to consent or complete the follow-up assessment (n = 5). No significant differences in patient characteristics were found between the 65 recruited patients and the 17 patients from the initial study who were not followed. One patient was acutely hospitalized on the day of recruitment and, thus, all results pertain to the remaining 64 patients. The hospitalized patient not followed was female, with a previously low baseline function (dependent in 5 out of 18 activities of daily living). The overall study patient characteristics were similar when this patient was excluded from Table 1 (data not shown). The mean time between baseline and follow-up assessment of the study sample was 394 ± 53 days. Participants were on average aged 70.5 ± 4.4 years at the time of follow-up; 18 had previously undergone living donor transplantation, while the remaining had deceased donor organs. The racial mix was similar to the catchment population served (52 White; 3 South-Asian; 4 Asian; and 5 black). Participant characteristics are summarized in Table 1. Within the cohort, 10 individuals had been hospitalized at least once during the follow-up period (median: 1, range: 1-4 hospitalizations) for a median of 4 days (range: 1-27).
Table 1.
Baseline and Follow-up Characteristics of Eligible Patients Who Participated in the Study Compared With Patients in the Original Cohort.
| Original cohort (n = 82) |
Current study (n = 64) |
||||
|---|---|---|---|---|---|
| Baseline | P valuea | Baseline | Follow-up | P valueb | |
| Demographics | |||||
| Age | 69.4 ± 4.2 | .91 | 69.4 ± 4.4 | 70.5 ± 4.4 | <.001 |
| Male gender | 45 (49%) | .72 | 37 (58%) | 37 (58%) | <.001 |
| Time with current transplant, years (median, IQR) | 4.7 (1.5, 10.7) | .98 | 5.0 (1.5, 9.1) | 6.2 (2.6, 10.3) | <.001 |
| Medications | |||||
| Number of hypertensive drugs | (n = 81) 1.94 ± 1.03 |
.95 | 1.95 ± 1.08 | — | — |
| Prednisone use | 63 (77%) | .97 | 54 (84%) | 56 (88%) | .50 |
| Prednisone dose/6 months (mg) | (n = 81) 841 ± 550 |
.99 | 840 ± 578 | 904 ± 503 | .44 |
| Laboratory data | |||||
| Hemoglobin (g/L) | 123.5 ± 19 | .68 | 122.2 ± 19 | 126.4 ± 19 | .03 |
| Serum albumin (g/L) | (n = 81) 39.1 ± 3.5 |
.78 | 39.5 ± 3.6 | 39.9 ± 2.6 | .33 |
| Serum creatinine (µmol/L) | 134.6 ± 61 | .74 | 131.4 ± 58 | 140.6 ± 72 | .03 |
| Residence | |||||
| House | 45 (55%) | .98 | 35 (55%) | 31 (48%) | .42 |
| Apartment | 34 (42%) | .92 | 26 (41%) | 31 (48%) | .30 |
| Retirement residence | 3 (4%) | 1.00 | 3 (5%) | 2 (3%) | 1.00 |
| Lives alone | 11 (13%) | .91 | 9 (14%) | 13 (20%) | .22 |
| Employed | 15 (18%) | .76 | 13 (20%) | 10 (16%) | .38 |
| Comorbidities | |||||
| Number (median, IQR) | 3 (3, 5) | .87 | 3 (2, 5) | — | — |
| Diabetes | 41 (50%) | .71 | 35 (55%) | — | — |
| Ischemic heart disease | 21 (26%) | .90 | 17 (26 %) | — | — |
| Other cardiovascular diseasec | 76 (92%) | .65 | 58 (89%) | — | — |
| Neurological disease | 7 (9%) | .63 | 7 (11%) | — | — |
| Anticoagulation | 26 (32%) | .79 | 19 (30%) | — | — |
| Functional status | |||||
| TUG (seconds) | (n = 79) 12.7 ± 6.7 |
.89 | (n = 62) 12.9 ± 6.7 |
(n = 63) 12.3 ± 6.5 |
.31 |
| Number of disabled ADLs | 1.7 ± 2.3 | .79 | 1.7 ± 2.4 | 1.9 ± 2.8 | .42 |
| Median number disabilities (range) | 1.00 (0-12) | — | 0.50 (0-12) | 0.50 (0-11) | — |
| TUG >10 seconds or not attempted | 51 (62%) | .97 | 40 (63%) | 33 (52%) | .04 |
| ≥1 ADL disability | 44 (54 %) | .95 | 32 (50%) | 32 (50%) | 1.00 |
| ≥1 reported fall in past year | 17 (21%) | .77 | 12 (19%) | 18 (28%) | .24 |
| Dominant handgrip <10th percentile | 24 (29%) | .96 | 25 (39%) | 29 (45%) | .42 |
Note. Plus-minus values are means ± SD. ADL = Activities of daily living; IQR = interquartile range; TUG = Timed Up and Go Test.
P value for differences at baseline between patients enrolled in the original cohort and those completing both baseline and follow-up study.
P value for differences between baseline and follow-up tests in those completing both baseline and follow-up assessments.
Other cardiovascular disease includes congestive heart failure, arrhythmias, hypertension, peripheral vascular disease, or other heart disease.
Functional Status
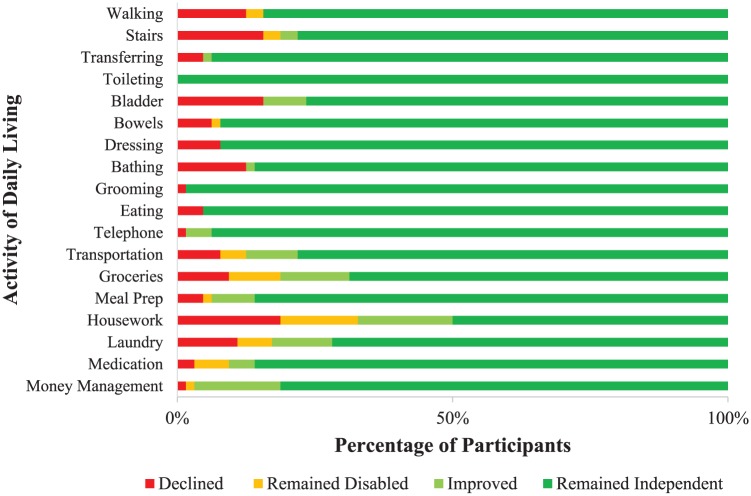
Thirty-two of 64 (50%) patients had functional disability at baseline, and the same proportion (50%) had disability at follow-up. When compared with the baseline assessment, 37 (58%) of the 64 patients were found to have experienced a change in functional status. The direction of change seen was both improvement (n = 15, 41%) and deterioration (n = 22, 59%). Functional deterioration was seen in approximately one-third of patients. This appeared consistent across the cohort, regardless of whether disability was noted at the initial assessment or not (Figure 1). Of those with previous disability (Table 2), 11 patients had progressive decline.
Figure 1.
Stacked bar graph showing direction of functional change according to level of baseline disability.
Table 2.
Characteristics Showing Differences Within the Subgroup of Participants With Baseline Disability (n = 32) Comparing Those Who Demonstrated Further Functional Decline Over the Follow-up Period Versus Those Who Remained Stable or Improved.
| Progressive functional decline (n = 11) | Functional stability or improvement (n = 21) | |
|---|---|---|
| Age at follow-up (mean ± SD) |
72.0 ± 5.8 | 71.2 ± 4.6 |
| Male (%) | 8/11 (73%) | 13/21 (62%) |
| Time since transplant (years) (median, IQR) | 6.9 (2.5, 8.9) | 3.8 (2.0, 7.7) |
| No. of comorbidities at baseline (median, IQR) | 4.7 (3, 6) | 3.0 (2, 5) |
| TUG >15 seconds at baseline (%) | 6/10 (60%) | 5/20 (25%) |
| Dominant handgrip <10th percentile at baseline (%) | 6/11 (55%) | 9/21 (43%) |
| Median disabled ADLs at baseline (IQR) | 3 (1, 5) | 2 (1, 4) |
| Independent in instrumental ADLs at baseline (%) | 8/11 (73%) | 16/21 (76%) |
| Fall during year of follow-up (%) | 6/11 (55%) | 3/21 (14%) |
| Hospitalized during year of follow-up (%) | 2/11 (18%) | 9/21 (43%) |
Note. ADL = Activities of daily living; IQR = interquartile range; TUG = Timed Up and Go Test.
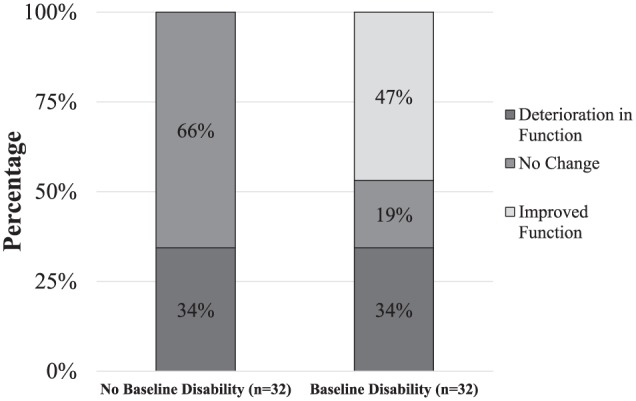
Twenty-eight percent of patients (n = 18) experienced a change in independence (in either direction) in only 1 activity, while 11% (n = 7) changed in 2 activities, and 6% (n = 4) changed in 3 or more activities. Of the 22 individuals with functional decline occurring in the 1-year follow-up period, 50% (n = 11) and 18% (n = 4) had a decline in 1 and 2 activities, respectively, while 32% (n = 7) had a decline in 3 or more activities. Mobility, bladder control, and housework were the domains found to decline most over time (Figure 2).
Figure 2.
Changes in functional status in individual BADL and IADL activities.
Note. BADL = basic activities of daily living; IADL = instrumental activities of daily living.
Physical Function
Sixty-three of 64 patients completed the TUG test. Thirty-one patients (49%) had optimal functional mobility speed, while 18 patients (29%) had borderline impairment and 14 patients (22%) had significant impairment. The TUG score correlated moderately with the number of Activities of daily living (ADL) activities that were not done by the patient (r = 0.65; P < .001). Thirty-six patients (56%) had high exercise capacity on the VSAQ with a predicted METS >8, while 3 (5%) had medium exercise capacity (predicted METS 5-8) and 25 patients (39%) had low exercise capacity (predicted METS <5). Timing on the TUG test correlated with predicted METS (r = −0.60, P < .01). Twenty-nine of 64 (45%) patients who performed the handgrip strength assessment had a dominant handgrip strength that fell below the 10th percentile compared with age-matched and gender-matched norms from the general population.15 No correlation with ADL disability was found (r = −0.18; P = .14).
Accidental Falls
Eighteen of 64 patients (28%) experienced a total of 25 falls in the year between the 2 study evaluations. Of 4 individuals with multiple falls, 1 person had 4 falls. Collectively, 24 (38%) patients in this cohort experienced at least 1 fall during the 2-year period assessed, with 41 total falls and an incidence rate, over 2 years, of 0.32 falls per patient-year. Among those with falls in the follow-up period, 6 (33%) had also reported having had 1 or more falls in the year prior to the baseline assessment.
The relationship between falls and functional decline was explored post hoc. Patients who had progressive decline had a 3.8 times greater risk of falling in the time between study assessments (P = .035, 95% confidence interval [CI] = 1.2-12.4, Table 2). Individuals who reported 1 or more falls in the year between assessments were at 5-fold greater risk of progressive disability (7/8, 88% of fallers, compared with 4/24 nonfallers; P = .001, relative risk reduction (RRR) = 5.3, 95% CI = 2.1-13.3).
Cognitive Function
Cognitive impairment, as measured using the Mini-Cog, was seen in 18 patients (28%). 33% (n = 21) of patients failed the clock-drawing test, while 20% (n = 13) of patients were unable to recall 2 or more words from a 3-item recall. Two patients were unable to recall any words.
Discussion
The data presented in this paper confirm our previous observation of a high burden of functional disability in older patients living with a functioning kidney transplant7 and extend our understanding of the nature of changes in function over time. The data presented confirm that disability is a fluid state, with fluctuation in 2 directions leading to both functional recovery and decline.8,23 The data also suggest that individuals with a history of 1 or more accidental falls, and those with abnormal physical performance testing, may be more prone to persistent or progressive functional loss suggesting an opportunity for detection and possibly intervention.
The finding that our patients experienced functional change over time is somewhat consistent with that from the general population.24,25 What is unexpected, however, is the observation that more than 30% of those who had disability at baseline had persistent or worsening disability at the follow-up assessment despite ongoing stable kidney transplant function. In a large prospective study of 754 community-dwelling patients aged 70 years or more, followed monthly over a 3-year period, 46% of those at high risk due to frailty and medical morbidity experienced at least 1 episode of basic ADL disability. Of those, one-third occurred insidiously (defined as disability occurring in the absence of a clear precipitating event), and in around 15% lasted more than a month.25 Although most individuals subsequently regained independence, those individuals with persistent disability had episodes of disability that lasted on average 6 months, with more frequent disability episodes (and transitions) in those with underlying baseline frailty.26 We postulate that the increased risk of persistent disability (typically defined as disability lasting more than 6 months) seen in our study patients may be related to their high burden of multimorbidity, acute illness associated with hospitalization, or possibly due to more frequent fluctuations associated with infections or other intercurrent illnesses.24,27-32 Regardless, the observation that our patients have a high risk of persistent disability places them at a higher overall risk of poor outcomes such as a future need for nursing home care, death, and/or recurrent or prolonged hospitalization.33
We also confirmed our previous finding that kidney transplant patients have a high rate of accidental falls (almost 2-fold more common than that reported in the general community-dwelling elderly population).34 This is an important finding, as falls are associated with a range of poor outcomes, including an increased risk of future hospitalization, institutionalization, and mortality in both renal and nonrenal elderly populations.34-36 On reflection, this observation should not be unexpected particularly as accidental falls are common among dialysis patients,37,38 and a previous fall is highly predictive of subsequent falls.39 However, we had expected that patients who fall while undergoing maintenance dialysis would be less likely to be waitlisted for or undergo kidney transplantation. In those with progressive decline, it is possible that falls may have caused or exacerbated their functional decline, although the severity or consequences of the falls observed in this study were not captured.
The high prevalence of cognitive impairment in the sample is also notable. We were particularly concerned about the relatively high rate of executive dysfunction on the clock-drawing test, as this is often used to better understand executive function tasks such as those often required with managing transplant medications. Cognitive impairment is common among patients of all ages on dialysis.40 Previous research not only suggests that cognition improves after transplantation but also shows that it remains poorer than that of the general population overall.41-43
Several study strengths are noted. First, the paired study design and relatively high rate of re-recruitment of the initial sample studied (79%) minimized the potential for bias. Second, our choice of widely used and validated measures of disability administered by trained professionals likely improved the reliability of our results. The VSAQ was added to the battery of tests used in response to the results of our initial study where we experienced ceiling effects on the Lawton-Brody IADL score. The data confirm that this is suitable for any subsequent tests in this population. Third, the use of physical and cognitive performance measures applicable across a wide range of patient abilities has helped to gain further insight into the functional status of the patients. Finally, the patients were recruited from a large kidney transplant program that serves a demographically and clinically diverse population.
There are, however, several limitations of the study, including its single-center design and lack of comparator group. Falls were based solely on patient recall and, therefore, subject to a high rate of recall bias that may underestimate fall events.44 There is a potential for survival bias inherent to prevalent studies that may lead to underestimation of the burden of functional disability in an incident kidney transplant population. The relatively small sample size limited our ability to examine factors associated with functional decline or falls. We are also unable to characterize the nature or frequency of the transitions between health states due to the long interval between assessments and absence of baseline VSAQ data. Finally, the study was conducted at a single, large, kidney transplant center so generalizing the results to other settings must be done with caution. Despite these limitations, we believe that these data are foundational for subsequent study into the trajectory of change in functional disability among elderly patients from the time of kidney transplant assessment to death and the implications of functional decline on long-term outcomes. We believe these data are of value to clinicians who may wish to introduce routine monitoring of functional status and falls in older kidney transplant recipients with renal disease and to those wishing to explore the value of rehabilitation programs.
In conclusion, elderly patients living with kidney transplants are vulnerable to functional disability, with some demonstrating a concerning pattern of progressive decline over time. Accidental falls are common, as is reduced physical functioning and cognitive impairment. The data suggest that a geriatric-informed approach to care in this patient group is warranted, with more deliberate clinical monitoring and follow-up addressing these important outcomes.
Supplemental Material
Supplemental material, 2017_Suppl_1yr_transplant_yau_r1_Table_2 for A Longitudinal Study Examining the Change in Functional Independence Over Time in Elderly Individuals With a Functioning Kidney Transplant by Kevin Yau, Janine F. Farragher, S. Joseph Kim, Olusegun Famure and Sarbjit V. Jassal in Canadian Journal of Kidney Health and Disease
Supplemental Material
Supplemental material, 2017_Suppl_2_Assessment_Tools for A Longitudinal Study Examining the Change in Functional Independence Over Time in Elderly Individuals With a Functioning Kidney Transplant by Kevin Yau, Janine F. Farragher, S. Joseph Kim, Olusegun Famure and Sarbjit V. Jassal in Canadian Journal of Kidney Health and Disease
Footnotes
List of Abbreviations: ADLtotal, Total ADL score (derived from sum of Barthel and Lawton-Brody scales); Alb, serum albumin; BADL, basic activities of daily living; Hb, hemoglobin; IADL, instrumental activities of daily living; METS, peak metabolic equivalents; SCr, serum creatinine; TUG, Timed Up and Go Test; VO2max, measured peak oxygen uptake; VSAQ, Veterans Specific Activity Questionnaire score.
Ethics Approval and Consent to Participate: The study protocol was approved by the local hospital research ethics board (REB # 13-6276).
Consent for Publication: All authors have read and approved the final version of this manuscript.
Availability of Data and Materials: Original data are not publicly available. During the consent process, required for hospital research ethics approval, patients enrolled in this study were advised that data collected were confidentially stored and would not be available publicly.
Authors’ Note: The results presented in this paper have not been published previously in whole or part, except in abstract format.
Author Contributions: Kevin Yau: performance of research, writing of paper, data analysis; Janine F. Farragher: performance of research, writing of paper, data analysis; S. Joseph Kim: writing of paper; Olusegun Famure: writing of paper; Sarbjit V. Jassal: research design, data analysis, writing of paper.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material:Supplementary material is available for this article online.
References
- 1. USRDS 2017 Annual Data Report. Chapter 6: Transplantation www.usrds.org/2017/view (accessed 10 May 2018)
- 2. Dunlop DD, Manheim LM, Sohn MW, Liu X, Chang RW. Incidence of functional limitation in older adults: the impact of gender, race, and chronic conditions. Arch Phys Med Rehabil. 2002;83:964-971. [DOI] [PubMed] [Google Scholar]
- 3. Stuck AE, Walthert JM, Nikolaus T, Bula CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. 1999;48:445-469. [DOI] [PubMed] [Google Scholar]
- 4. Sood MM, Rigatto C, Bueti J, et al. Functional status, discharge to a long-term care facility and in-hospital death among dialysis patients. Am J Kid Dis. 2011;58:804-812. [DOI] [PubMed] [Google Scholar]
- 5. Fortinsky RH, Covinsky KE, Palmer RM, Landefeld CS. Effects of functional status changes before and during hospitalization on nursing home admission of older adults. J Gerontol A Biol Sci Med Sci. 1999;54:M521-M156. [DOI] [PubMed] [Google Scholar]
- 6. Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure.” JAMA. 2011;306:1782-1793. [DOI] [PubMed] [Google Scholar]
- 7. Kasbia GS, Farragher J, Kim SJ, Famure O, Jassal SV. A cross-sectional study examining the functional independence of elderly individuals with a functioning kidney transplant. Transplantation. 2014;98:864-870. [DOI] [PubMed] [Google Scholar]
- 8. Gill TM, Gahbauer EA, Allore HG, Han L. Transitions between frailty states among community-living older persons. Arch Intern Med. 2006;166:418-423. [DOI] [PubMed] [Google Scholar]
- 9. Gill TM, Kurland B. The burden and patterns of disability in activities of daily living among community-living older persons. J Gerontol A Biol Sci Med Sci. 2003;58:70-75. [DOI] [PubMed] [Google Scholar]
- 10. Hardy SE, Gill TM. Recovery from disability among community-dwelling older persons. JAMA. 2004;291:1596-1602. [DOI] [PubMed] [Google Scholar]
- 11. Ciol MA, Rasch EK, Hoffman JM, Huynh M, Chan L. Transitions in mobility, ADLs, and IADLs among working-age Medicare beneficiaries. Disabil Health J. 2014;7:206-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J. 1965;14:61-65. [PubMed] [Google Scholar]
- 13. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179-186. [PubMed] [Google Scholar]
- 14. Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Physical Therapy. 2002;82:128-137. [DOI] [PubMed] [Google Scholar]
- 15. Massy-Westropp NM, Gill TK, Taylor AW, Bohannon RW, Hill CL. Hand grip strength: age and gender stratified normative data in a population-based study. BMC Res Notes. 2011;4:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Silva LF, Matos CM, Lopes GB, et al. Handgrip strength as a simple indicator of possible malnutrition and inflammation in men and women on maintenance hemodialysis. J Ren Nutr. 2011;21:235-245. [DOI] [PubMed] [Google Scholar]
- 17. de Oliveira Brito LV, Maranhao Neto GA, Moraes H, Emerick RF, Deslandes AC. Relationship between level of independence in activities of daily living and estimated cardiovascular capacity in elderly women. Arch Gerontol Geriatr. 2014;59:367-371. [DOI] [PubMed] [Google Scholar]
- 18. Myers J, Bader D, Madhavan R, Froelicher V. Validation of a specific activity questionnaire to estimate exercise tolerance in patients referred for exercise testing. Am Heart J. 2001;142:1041-1046. [DOI] [PubMed] [Google Scholar]
- 19. Borson S, Scanlan JM, Chen P, Ganguli M. The Mini-Cog as a screen for dementia: validation in a population-based sample. J Am Geriatr Soc. 2003;51:1451-1454. [DOI] [PubMed] [Google Scholar]
- 20. Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The mini-cog: a cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry. 2000;15:1021-1027. [DOI] [PubMed] [Google Scholar]
- 21. Na L, Pan Q, Xie D, et al. Activity limitation stages are associated with risk of hospitalization among Medicare beneficiaries. PM R. 2017;9:433-443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hennessy S, Kurichi JE, Pan Q, et al. Disability stage is an independent risk factor for mortality in Medicare beneficiaries aged 65 years and older. PM R. 2015;7:1215-1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gill TM, Allore HG, Hardy SE, Guo Z. The dynamic nature of mobility disability in older persons. JAGS. 2006;54:248-254. [DOI] [PubMed] [Google Scholar]
- 24. Laan W, Bleijenberg N, Drubbel I, Numans ME, de Wit NJ, Schuurmans MJ. Factors associated with increasing functional decline in multimorbid independently living older people. Maturitas. 2013;75:276-281. [DOI] [PubMed] [Google Scholar]
- 25. Gill T, Allore H, Holford T, Guo Z. The development of insidious disability in activities of daily living among community-living older persons. Am J Med. 2004;117:484-491. [DOI] [PubMed] [Google Scholar]
- 26. Hardy SE, Allore HG, Guo Z, Dubin JA, Gill TM. The effect of prior disability history on subsequent functional transitions. J Gerontol A Biol Sci Med Sci. 2006;61:272-277. [DOI] [PubMed] [Google Scholar]
- 27. Raiche M, Hebert R, Dubois MF, Gueye NR, Dubuc N. Yearly transitions of disability profiles in older people living at home. Arch Gerontol Geriatr. 2012;55:399-405. [DOI] [PubMed] [Google Scholar]
- 28. Ferrante LE, Pisani MA, Murphy TE, Gahbauer EA, Leo-Summers LS, Gill TM. Functional trajectories among older persons before and after critical illness. JAMA Intern Med. 2015;175:523-529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Provencher V, Sirois MJ, Ouellet MC, et al. Decline in activities of daily living after a visit to a Canadian emergency department for minor injuries in independent older adults: are frail older adults with cognitive impairment at greater risk? J Am Geriatr Soc. 2015;63:860-868. [DOI] [PubMed] [Google Scholar]
- 30. Wojtusiak J, Levy CR, Williams AE, Alemi F. Predicting functional decline and recovery for residents in veterans affairs nursing homes. Gerontologist. 2016;56:42-51. [DOI] [PubMed] [Google Scholar]
- 31. Ryan A, Wallace E, O’Hara P, Smith SM. Multimorbidity and functional decline in community-dwelling adults: a systematic review. Health Qual Life Outcomes. 2015;13:168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Buurman BM, Han L, Murphy TE, et al. Trajectories of disability among older persons before and after a hospitalization leading to a skilled nursing facility admission. J Am Med Dir Assoc. 2016;17:225-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292:2115-2124. [DOI] [PubMed] [Google Scholar]
- 34. Shumway-Cook A, Ciol MA, Hoffman J, Dudgeon BJ, Yorkston K, Chan L. Falls in the Medicare population: incidence, associated factors, and impact on health care. Phys Ther. 2009;89:324-332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337:1279-1284. [DOI] [PubMed] [Google Scholar]
- 36. Iglesias CP, Manca A, Torgerson DJ. The health-related quality of life and cost implications of falls in elderly women. Osteoporos Int. 2009;20:869-878. [DOI] [PubMed] [Google Scholar]
- 37. Cook WL, Tomlinson G, Donaldson M, et al. Falls and fall-related injuries in older dialysis patients. Clin J Am Soc Nephrol. 2006;1:1197-1204. [DOI] [PubMed] [Google Scholar]
- 38. Farragher J, Rajan T, Chiu E, et al. Equivalent fall risk in elderly patients on hemodialysis and peritoneal dialysis. Perit Dial Int. 2016;36:67-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Cook WL, Jassal SV. Prevalence of falls among seniors maintained on hemodialysis. Int Urol Nephrol. 2005;37:649-652. [DOI] [PubMed] [Google Scholar]
- 40. Kurella Tamura M, Yaffe K. Dementia and cognitive impairment in ESRD: diagnostic and therapeutic strategies. Kidney Int. 2011;79:14-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Griva K, Thompson D, Jayasena D, Davenport A, Harrison M, Newman SP. Cognitive functioning pre- to post-kidney transplantation—a prospective study. Nephrol Dial Transplant. 2006;21:3275-3282. [DOI] [PubMed] [Google Scholar]
- 42. Harciarek M, Biedunkiewicz B, Lichodziejewska-Niemierko M, Debska-Slizien A, Rutkowski B. Continuous cognitive improvement 1 year following successful kidney transplant. Kidney Int. 2011;79:1353-1360. [DOI] [PubMed] [Google Scholar]
- 43. Radic J, Ljutic D, Radic M, Kovacic V, Dodig-Curkovic K, Sain M. Kidney transplantation improves cognitive and psychomotor functions in adult hemodialysis patients. Am J Nephrol. 2011;34:399-406. [DOI] [PubMed] [Google Scholar]
- 44. Ganz DA, Higashi T, Rubenstein LZ. Monitoring falls in cohort studies of community-dwelling older people: effect of the recall interval. J Am Geriatr Soc. 2005;53:2190-2194. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, 2017_Suppl_1yr_transplant_yau_r1_Table_2 for A Longitudinal Study Examining the Change in Functional Independence Over Time in Elderly Individuals With a Functioning Kidney Transplant by Kevin Yau, Janine F. Farragher, S. Joseph Kim, Olusegun Famure and Sarbjit V. Jassal in Canadian Journal of Kidney Health and Disease
Supplemental material, 2017_Suppl_2_Assessment_Tools for A Longitudinal Study Examining the Change in Functional Independence Over Time in Elderly Individuals With a Functioning Kidney Transplant by Kevin Yau, Janine F. Farragher, S. Joseph Kim, Olusegun Famure and Sarbjit V. Jassal in Canadian Journal of Kidney Health and Disease