Abstract
Background/Aims:
Patients with simultaneous upper gastrointestinal bleeding (UGIB) and acute myocardial infarction (AMI) have higher mortality than patients with either GIB or AMI. We aimed to assess the incidence and risk factors of in-hospital mortality in patients with UGIB and AMI.
Patients and Methods:
A total of 243 patients with UGIB and AMI were enrolled during 2012–2017. Clinical and laboratory data were collected and analyzed for clinical characteristics and potential risk factors of in-hospital mortality.
Results:
Among the 243 patients, 60 in-hospital deaths were observed (in-hospital mortality rate of 24.7%). Patients who died were older than the survivors (78.7 ± 6.6 vs. 72.6 ± 10.5 years, P < 0.001). Compared with survivors, patients who died showed increased peak white blood cell (WBC) count (9.74 ± 4.72 vs. 7.60 ± 2.91 × 109/L, P = 0.002), serum creatinine levels [134 (106, 190) vs. 97 (79, 125) mmol/L, P = 0.014], peak blood urine nitrogen levels (16.31 ± 8.48 mmol/L vs. 9.86 ± 6.33 mmol/L, P < 0.001), and peak brain natriuretic peptide (BNP) amounts [13,250 (6071, 30,000) vs. 3598 (728, 12,842) pg/mL, P < 0.001]. Meanwhile, patients who died also displayed lower minimum hemoglobin levels (78.3 ± 21.1 vs. 86.3 ± 22.3 g/L, P = 0.018) and minimum platelet counts (184.3 ± 79.1 vs. 214.6 ± 80.1 × 109/L, P = 0.013). In multivariable logistic analysis, age [OR (95% CI) =1.118 (1.053–1.186), P < 0.001], peak WBC count [OR (95% CI) =1.252 (1.113–1.407), P < 0.001], minimum platelet count [OR (95% CI) = 0.994 (0.989–1.000), P = 0.032], and peak BNP levels [OR (95% CI) =3.880 (1.761–8.550), P = 0.001] were independent predictors of in-hospital mortality.
Conclusions:
Patients with UGIB and AMI had a high in-hospital mortality, which was independently associated with age, peak WBC count, minimum platelet count, and peak BNP levels.
Keywords: Acute myocardial infarction, in-hospital mortality, risk factors, upper gastrointestinal bleeding
INTRODUCTION
Upper gastrointestinal bleeding (UGIB) and acute myocardial infarction (AMI) are common but serious medical emergencies that cause synergistic sequelae.[1,2,3,4,5] Yavorski et al.[6] found a UGIB incidence of 36 per 100,000 people; the overall mortality of UGIB was 7–10%, and increased along with age in both males and females. Wilcox et al.[7] found that the 30-day mortality rates of gastrointestinal bleeding (GIB) and AMI were 2.5% and 4.4% in hospitalized patients, respectively.
According to AMI guidelines,[8,9,10,11,12] reperfusion followed by medical therapy (e.g., aspirin, clopidogrel, and statin) is the gold standard for AMI treatment, but while clopidogrel and aspirin in combination may reduce the risk of cardiovascular events, they increase the risk of hemorrhage.[13,14,15,16,17,18] Myocardial infarction and acute GIB (upper and lower GIB, hereafter referred to as UGIB and LGIB, respectively) occurring simultaneously is well documented. In a multicenter, case-controlled study, 36 patients with combined GIB and AMI were assessed.[19] The study showed that patients with simultaneous UGIB and AMI had significantly greater mortality than either GIB or AMI controls. The incidence of AMI with UGIB has steadily increased following the recommendations for aggressive dual antiplatelet therapy.[20] Puymirat et al. demonstrated that hospitalized elderly AMI patients receiving low molecular weight heparin (LMWH) present decreased bleeding and higher survival compared with those using nonfractioned heparin (UFH).[21] In agreement, bleeding during hospitalization was shown to be correlated with a high 5-year mortality in patients with AMI.[22]
Age, a previous history of GIB (upper or lower) and/or anemia, chronic kidney disease, respiratory failure, severe heart failure, and gastrointestinal cancer are demonstrated risk factors for GIB among patients with AMI after PCI.[23] Nevertheless, no guidelines presently define the causes, risk factors, and treatment principles in UGIB with AMI. Therefore, the aim of this study was to assess the frequency of in-hospital mortality in patients with UGIB and AMI, and determine the potential risk factors for this condition.
PATIENTS AND METHODS
Patients
This was a retrospective analysis of hospitalized patients with UGIB and AMI during the January 2012 to January 2017 period at the emergency department of a local Chinese hospital. The inclusion criterion was confirmed admission diagnosis of non-ST segment elevation AMI[24] with subsequent UGIB,[5,25] treated with conservative treatments only and without percutaneous coronary intervention. Patients with a positive fecal occult blood test but no visible melena or without any other clinical evidence of UGIB were excluded. The patients did not undergo gastroscopy after UGIB, but they discontinued antiplatelet therapy and were given proton pump inhibitors (PPIs). This study was approved by the ethics committee of our institution.
Data collection
Clinical history, medication, and laboratory data were collected. Laboratory data were recorded at admission and after 12, 24, and 48 h, and included peak values of white blood cell (WBC) count, alanine aminotransferase (ALT), aspartate aminotransferase (AST), glucose, serum creatinine (SCr), blood urea nitrogen (BUN), brain natriuretic peptide (BNP), creatine kinase (CK), and creatine kinase muscle B (CK-MB), and minimum values of red blood cell (RBC) count, hemoglobin, and platelets for all patients.[19]
Study endpoint
The main study endpoint was in-hospital mortality from all causes, including cardiac death, sudden death, stroke, and multiple organ failure. The various risk factors for mortality were assessed as well.
Statistical analysis
Categorical data were presented as frequencies (percentages) and compared using the Chi-square test or Fisher's exact test, as appropriate. Normally distributed continuous data were presented as mean ± standard deviation, and non-normally distributed parameters as median and interquartile range (IQR). The unpaired t-test and Mann–Whitney U-test were used for assessing normally and non-normally distributed parameters, respectively. Variables significantly associated with mortality in univariate analysis were entered into a multivariate logistical regression model to identify risk factors of in-hospital mortality. Data were analyzed using the SPSS 17.0 statistical software (IBM, Armonk, NY, USA), and P < 0.05 was considered statistically significant.
RESULTS
Patient characteristics
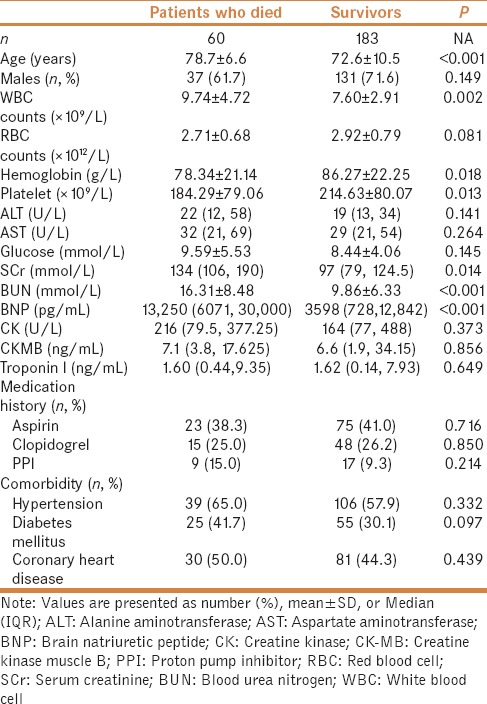
Based on both inclusion and exclusion criteria, 243 UGIB patients with AMI were included in the current study. Among them, 60 died (in-hospital mortality rate of 24.7%). As shown in Table 1, the Patients who died were older than the survivors (78.7 ± 6.6 vs. 72.6 ± 10.5 years, P < 0.001). Compared with survivors, the Patients who died showed increased peak white blood cell (WBC) count (9.74 ± 4.72 vs. 7.60 ± 2.91 × 109/L, P = 0.002), serum creatinine levels [134 (106, 190) vs. 97 (79, 125) mmol/L, P = 0.014], peak blood urine nitrogen levels (16.31 ± 8.48 mmol/L vs. 9.86 ± 6.33 mmol/L, P < 0.001), and peak brain natriuretic peptide (BNP) amounts 13250 (6071, 30,000) vs. 3598 (728, 12,842) pg/mL, P < 0.001]. Meanwhile, Patients who died also displayed lower minimum hemoglobin levels (78.3 ± 21.1 vs. 86.3 ± 22.3 g/L, P = 0.018) and minimum platelet counts (184.3 ± 79.1 vs. 214.6 ± 80.1 × 109/L, P = 0.013). The remaining parameters, including sex, red blood cell levels, transaminase levels, blood glucose amounts, history of medication, hypertension, diabetes mellitus, coronary heart disease, and blood transfusion treatment had similar values in both groups.
Table 1.
Patient demographic and clinical characteristics
Risk factors of in-hospital mortality in patients with upper gastrointestinal bleeding and acute myocardial infarction
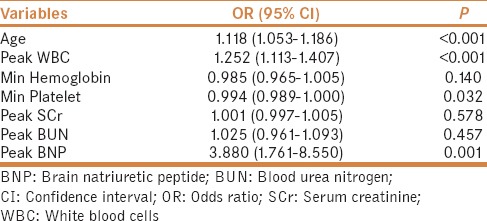
Multivariable logistic regression analysis was used to determine the independent risk factors for in-hospital mortality. The variables showing statistically significant differences between the death and survivor groups were selected for analysis [Table 2]. The included variables were age, peak WBC, minimum hemoglobin, minimum platelet, peak Cr, peak BUN, and peak BNP (BNP levels were log-transformed before data analysis). Interestingly, age [OR (95% CI) =1.118 (1.053–1.186), P < 0.001], peak WBC count [OR (95% CI) =1.252 (1.113–1.407), P < 0.001], minimum platelet count [OR (95% CI) = 0.994 (0.989–1.000), P = 0.032], and peak BNP levels [OR (95% CI) =3.880 (1.761–8.550), P = 0.001] were significantly associated with in-hospital mortality.
Table 2.
Logistic regression analysis of risk factors for mortality
DISCUSSION
This study strongly suggests that UGIB with AMI leads to high in-hospital mortality, with age, peak WBC count, minimum platelet count, and peak BNP amounts representing significant risk factors of mortality. These findings provide a basis for improving the clinical management of such patients.
In this retrospective study, the mortality of patients with UGIB and AMI was 24.7%. The ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) trial demonstrated that GIB is strongly associated with 30-day all-cause mortality (hazard ratio [HR]: 4.87 [IQR 2.61 to 9.08], P < 0.0001), cardiac mortality (HR: 5.35 [IQR 2.71 to 10.59], P < 0.0001), and composite ischemia (HR: 1.94 [IQR 1.14 to 3.30], P = 0.014).[26] Shalev et al. demonstrated that UGIB in patients with ACS is associated with markedly increased overall mortality, with a 30-day mortality rate of 33%. Moreover, previous peptic disease and use of combined anti-platelet therapy, especially in conjunction with heparin, are strong risk factors for mortality.[2] In UGIB and MI, bleeding represents the main symptom, and hypotension, tachycardia, and hematemesis are commonly found; independent of other epidemiological parameters, the mortality rate of combined GIB and MI is higher than that of each individual condition.[19] Lee et al. showed that mortality of patients with AMI and nonvariceal UGIB was only 8.7%, much lower than in the present study,[27] but no gastroscopy was performed in the present study and we could not distinguish patients with nonvariceal UGIB from those with variceal UGIB.
As shown above, age, peak WBC count, minimum platelet count, and peak BNP were independent risk factors for in-hospital mortality in patients with UGIB and AMI. To our knowledge, this is the first study revealing the associations of peak WBC count, minimum platelet count, and peak BNP with in-hospital mortality in UGIB with AMI. Previous studies showed that MI occurs frequently in patients with GI hemorrhage and admitted to an ICU. Age above 65 years and two or more risk factors for coronary artery disease have been shown to identify the patients at greatest risk of MI.[28] Al-Mallah et al. showed that 3% (80/3045) of patients with ACS develop clinically significant GIB. In the latter study, the risk factors of GIB were found to be older age, female gender, smoking status, peak troponin I amounts, and a history of heart failure, diabetes, and/or hypertension; in-hospital mortality was significantly higher in ACS patients with GIB versus those without (36% vs. 5%, P < 0.001).[29] Wu et al. also found that women and patients below 65 show fewer comorbidities compared with older individuals or men.[30]
Several studies have indicated that proton pump inhibitors significantly reduce major bleeding incidence in patients treated with dual antiplatelet therapy, especially among those with additional risk factor(s) for bleeding.[17,31,32] Nevertheless, Gaspar et al. and Kim et al. found that PPI in addition to aspirin and clopidogrel after ACS is not associated with a better prognosis.[33,34] In agreement, we found that the mortality rate in patients treated with aspirin, clopidogrel, and PPIs after ACS was not significantly different from that of patients without PPIs. Interestingly, a large Chinese trial demonstrated that AMI risk in patients with coronary artery disease increases by two-fold after UGIB.[30]
As shown above, multiple factors were associated with high mortality in patients with UGIB and AMI. It should be noted that UGIB and AMI are both clinical conditions and each has high mortality. In addition, treatment methods for UGIB and AMI are partially contradictory. Previous studies demonstrated that endoscopy is relatively safe for the diagnosis and management of UGIB in patients with AMI.[35,36] Yachimski et al. also supported endoscopy prior to cardiac catheterization in patients with AMI and overt UGIB; this strategy resulted in fewer deaths and reduced complications.[37] Lin et al. concluded that, in patients with concomitant UGIB and AMI, urgent endoscopy is most beneficial in patients with UGIB as the initial event, as well as in those presenting with hematemesis and hemodynamic instability.[38] Nevertheless, to avoid medical tangles, doctors often choose a relatively conservative therapy. Finally, there are no definitive guidelines for the management of patients with such unique scenarios and most practitioners rely on empiric treatment.
A few limitations should be mentioned for this study. First, this was a retrospective analysis, with inherent shortcomings. Some risk factors of UGIB and AMI mortality could not be assessed; indeed, albumin[39,40] and alcohol[41,42] could not be analyzed in the present study. Moreover, the treatment and disease severity was not consistent in the study population, but the treatment principles were consistent. In addition, relatively few patients with AMI and UGIB were included, and very small amounts of data were available on endoscopy efficacy. Finally, these patients were usually treated with conservative therapy, so there were few coronary angiography and coronary computed tomography angiography (CTA) data in the record. Bedside echocardiography generally could not be used as the clinical evaluation basis due to many factors such as availability and economical reasons. Hence, the heart conditions could only be estimated based on the levels of blood myocardial enzymes and BNP. Therefore, the present findings should be interpreted with caution.
CONCLUSION
The in-hospital mortality rate of patients with UGIB and AMI was very high. Age, peak WBC count, minimum platelet count, and peak BNP levels were shown to be independent risk factors of in-hospital mortality.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Albeldawi M, Qadeer MA, Vargo JJ. Managing acute upper GI bleeding, preventing recurrences. Cleve Clin J Med. 2010;77:131–42. doi: 10.3949/ccjm.77a.09035. [DOI] [PubMed] [Google Scholar]
- 2.Shalev A, Zahger D, Novack V, Etzion O, Shimony A, Gilutz H, et al. Incidence, predictors and outcome of upper gastrointestinal bleeding in patients with acute coronary syndromes. Int J Cardiol. 2012;157:386–90. doi: 10.1016/j.ijcard.2010.12.081. [DOI] [PubMed] [Google Scholar]
- 3.van Leerdam ME. Epidemiology of acute upper gastrointestinal bleeding. Best Pract Res Clin Gastroenterol. 2008;22:209–24. doi: 10.1016/j.bpg.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 4.Crooks C, Card T, West J. Reductions in 28-day mortality following hospital admission for upper gastrointestinal hemorrhage. Gastroenterology. 2011;141:62–70. doi: 10.1053/j.gastro.2011.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hearnshaw SA, Logan RF, Lowe D, Travis SP, Murphy MF, Palmer KR. Acute upper gastrointestinal bleeding in the UK: Patient characteristics, diagnoses and outcomes in the 2007 UK audit. Gut. 2011;60:1327–35. doi: 10.1136/gut.2010.228437. [DOI] [PubMed] [Google Scholar]
- 6.Yavorski RT, Wong RK, Maydonovitch C, Battin LS, Furnia A, Amundson DE. Analysis of 3,294 cases of upper gastrointestinal bleeding in military medical facilities. Am J Gastroenterol. 1995;90:568–73. [PubMed] [Google Scholar]
- 7.Wilcox CM, Cryer BL, Henk HJ, Zarotsky V, Zlateva G. Mortality associated with gastrointestinal bleeding events: Comparing short-term clinical outcomes of patients hospitalized for upper GI bleeding and acute myocardial infarction in a US managed care setting. Clin Exp Gastroenterol. 2009;2:21–30. doi: 10.2147/ceg.s4936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Myocardial Infarction (Updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (Updatingaemorrhage in England: Analysis of hospital admissions 1999 to 2005. Gut. 2009;558:A93. [Google Scholar]
- 9.Kushner FG, Hand M, Smith SC, Jr, King SB, 3rd, Anderson JL, Antman EM, et al. 2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;120:2271–306. doi: 10.1161/CIRCULATIONAHA.109.192663. [DOI] [PubMed] [Google Scholar]
- 10.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Jr, et al. 2011 ACCF/AHA Focused Update Incorporated Into the ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;123:e426–579. doi: 10.1161/CIR.0b013e318212bb8b. [DOI] [PubMed] [Google Scholar]
- 11.Chinese Society of Cardiology, Cardiology EBoCJo. Guidelines for the Management of Unstable Angina/Non-ST-Elevation Myocardial Infarction. Chin J Cardiol. 2007;35:295–304. [Google Scholar]
- 12.Chinese Society of Cardiology, Cardiology EBoCJo. Guidelines for the Management of Patients with ST-Elevation Myocardial Infarction. Chin J Cardiol. 2010;38:675–90. [Google Scholar]
- 13.Peters RJ, Mehta SR, Fox KA, Zhao F, Lewis BS, Kopecky SL, et al. Effects of aspirin dose when used alone or in combination with clopidogrel in patients with acute coronary syndromes: Observations from the Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) study. Circulation. 2003;108:1682–7. doi: 10.1161/01.CIR.0000091201.39590.CB. [DOI] [PubMed] [Google Scholar]
- 14.Sugano K. How do we manage serious gastrointestinal adverse events associated with anti-thrombotic therapy? Expert Rev Gastroenterol Hepatol. 2015;9:5–8. doi: 10.1586/17474124.2014.945913. [DOI] [PubMed] [Google Scholar]
- 15.Manson JE, Bassuk SS. When is the use of aspirin for CVD prevention in women appropriate? Menopause. 2014;21:103–5. doi: 10.1097/GME.0b013e318298d74e. [DOI] [PubMed] [Google Scholar]
- 16.Berger JS, Brown DL, Burke GL, Oberman A, Kostis JB, Langer RD, et al. Aspirin use, dose, and clinical outcomes in postmenopausal women with stable cardiovascular disease: The Women's Health Initiative Observational Study. Circ Cardiovasc Qual Outcomes. 2009;2:78–87. doi: 10.1161/CIRCOUTCOMES.108.791269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ng FH, Wong SY, Lam KF, Chang CM, Lau YK, Chu WM, et al. Gastrointestinal bleeding in patients receiving a combination of aspirin, clopidogrel, and enoxaparin in acute coronary syndrome. Am J Gastroenterol. 2008;103:865–71. doi: 10.1111/j.1572-0241.2007.01715.x. [DOI] [PubMed] [Google Scholar]
- 18.Heer T, Juenger C, Gitt AK, Bauer T, Towae F, Zahn R, et al. Efficacy and safety of optimized antithrombotic therapy with aspirin, clopidogrel and enoxaparin in patients with non-ST segment elevation acute coronary syndromes in clinical practice. J Thromb Thrombolysis. 2009;28:325–32. doi: 10.1007/s11239-008-0294-y. [DOI] [PubMed] [Google Scholar]
- 19.Cappell MS. A study of the syndrome of simultaneous acute upper gastrointestinal bleeding and myocardial infarction in 36 patients. Am J Gastroenterol. 1995;90:1444–9. [PubMed] [Google Scholar]
- 20.Jensen BE, Hansen JM, Junker AB, Lassen JF, Jensen SE, Schaffalitzky de Muckadell OB. High prevalence of ulcer bleeding risk factors in dual antiplatelet-treated patients after percutaneous coronary intervention. Dan Med J. 2015:62. [PubMed] [Google Scholar]
- 21.Puymirat E, Aissaoui N, Collet JP, Chaib A, Bonnet JL, Bataille V, et al. Comparison of bleeding complications and one-year survival of low molecular weight heparin versus unfractioned heparin for acute myocardial infarction in elderly patients. The FAST-MI registry. Int J Cardiol. 2013;166:106–10. doi: 10.1016/j.ijcard.2011.10.008. [DOI] [PubMed] [Google Scholar]
- 22.Ducrocq G, Puymirat E, Steg PG, Henry P, Martelet M, Karam C, et al. Blood transfusion, bleeding, anemia, and survival in patients with acute myocardial infarction: FAST-MI registry. Am Heart J. 2015;170:726–34 e2. doi: 10.1016/j.ahj.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 23.Kikkert WJ, Hassell ME, Delewi R, van der Laan MH, Baan J, Jr, Vis MM, et al. Predictors and prognostic consequence of gastrointestinal bleeding in patients with ST-segment elevation myocardial infarction. Int J Cardiol. 2015;184:128–34. doi: 10.1016/j.ijcard.2015.01.041. [DOI] [PubMed] [Google Scholar]
- 24.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. Circulation. 2012;126:2020–35. doi: 10.1016/j.gheart.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 25.Rafeey M, Shoaran M, Majidy H. Diagnostic endoscopy and clinical characteristics of gastrointestinal bleeding in children: A 10-year retrospective study. Iran Red Crescent Med J. 2013;15:794–7. doi: 10.5812/ircmj.7075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nikolsky E, Stone GW, Kirtane AJ, Dangas GD, Lansky AJ, McLaurin B, et al. Gastrointestinal bleeding in patients with acute coronary syndromes: Incidence, predictors, and clinical implications: Analysis from the ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) trial. J Am Coll Cardiol. 2009;54:1293–302. doi: 10.1016/j.jacc.2009.07.019. [DOI] [PubMed] [Google Scholar]
- 27.Lee YJ, Min BR, Kim ES, Park KS, Cho KB, Jang BK, et al. Predictive factors of mortality within 30 days in patients with nonvariceal upper gastrointestinal bleeding. Korean J Intern Med. 2016;31:54–64. doi: 10.3904/kjim.2016.31.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Emenike E, Srivastava S, Amoateng-Adjepong Y, al-Kharrat T, Zarich S, Manthous CA. Myocardial infarction complicating gastrointestinal hemorrhage. Mayo Clin Proc. 1999;74:235–41. doi: 10.4065/74.3.235. [DOI] [PubMed] [Google Scholar]
- 29.Al-Mallah M, Bazari RN, Jankowski M, Hudson MP. Predictors and outcomes associated with gastrointestinal bleeding in patients with acute coronary syndromes. J Thromb Thrombolysis. 2007;23:51–5. doi: 10.1007/s11239-006-9005-8. [DOI] [PubMed] [Google Scholar]
- 30.Wu CJ, Lin HJ, Weng SF, Hsu CC, Wang JJ, Su SB, et al. Acute Myocardial Infarction Risk in Patients with Coronary Artery Disease Doubled after Upper Gastrointestinal Tract Bleeding: A Nationwide Nested Case-Control Study. PLoS One. 2015;10:e0142000. doi: 10.1371/journal.pone.0142000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hsiao FY, Tsai YW, Huang WF, Wen YW, Chen PF, Chang PY, et al. A comparison of aspirin and clopidogrel with or without proton pump inhibitors for the secondary prevention of cardiovascular events in patients at high risk for gastrointestinal bleeding. Clin Ther. 2009;31:2038–47. doi: 10.1016/j.clinthera.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 32.Luinstra M, Naunton M, Peterson GM, Bereznicki L. PPI use in patients commenced on clopidogrel: A retrospective cross-sectional evaluation. J Clin Pharm Ther. 2010;35:213–7. doi: 10.1111/j.1365-2710.2009.01089.x. [DOI] [PubMed] [Google Scholar]
- 33.Gaspar A, Ribeiro S, Nabais S, Rocha S, Azevedo P, Pereira MA, et al. Proton pump inhibitors in patients treated with aspirin and clopidogrel after acute coronary syndrome. Rev Port Cardiol. 2010;29:1511–20. [PubMed] [Google Scholar]
- 34.Kim KR, Jun CH, Cho KM, Wi JW, Park SY, Cho SB, et al. Can proton pump inhibitors reduce rebleeding following Histoacryl sclerotherapy for gastric variceal hemorrhage? Korean J Intern Med. 2015;30:593–601. doi: 10.3904/kjim.2015.30.5.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lim RG, Cobell WJ, Theivanayagam S, Kilgore TW, Matteson ML, Puli SR, et al. Endoscopy after acute myocardial infarction: An evaluation of safety. South Med J. 2013;106:545–9. doi: 10.1097/SMJ.0000000000000001. [DOI] [PubMed] [Google Scholar]
- 36.Cena M, Gomez J, Alyousef T, Trohman RG, Pierko K, Agarwal R. Safety of endoscopic procedures after acute myocardial infarction: A systematic review. Cardiol J. 2012;19:447–52. doi: 10.5603/cj.2012.0083. [DOI] [PubMed] [Google Scholar]
- 37.Yachimski P, Hur C. Upper endoscopy in patients with acute myocardial infarction and upper gastrointestinal bleeding: Results of a decision analysis. Dig Dis Sci. 2009;54:701–11. doi: 10.1007/s10620-008-0403-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lin S, Konstance R, Jollis J, Fisher DA. The utility of upper endoscopy in patients with concomitant upper gastrointestinal bleeding and acute myocardial infarction. Dig Dis Sci. 2006;51:2377–83. doi: 10.1007/s10620-006-9326-7. [DOI] [PubMed] [Google Scholar]
- 39.Gonzalez-Gonzalez JA, Vazquez-Elizondo G, Garcia-Compean D, Gaytan-Torres JO, Flores-Rendon AR, Jaquez-Quintana JO, et al. Predictors of in-hospital mortality in patients with non-variceal upper gastrointestinal bleeding. Rev Esp Enferm Dig. 2011;103:196–203. doi: 10.4321/s1130-01082011000400005. [DOI] [PubMed] [Google Scholar]
- 40.Plakht Y, Gilutz H, Shiyovich A. Decreased admission serum albumin level is an independent predictor of long-term mortality in hospital survivors of acute myocardial infarction. Soroka Acute Myocardial Infarction II (SAMI-II) project. Int J Cardiol. 2016;219:20–4. doi: 10.1016/j.ijcard.2016.05.067. [DOI] [PubMed] [Google Scholar]
- 41.Yedlapati SH, Mendu A, Stewart SH. Alcohol-related diagnoses and increased mortality in acute myocardial infarction patients: An analysis of the nationwide inpatient sample. J Hosp Med. 2016;11:563–7. doi: 10.1002/jhm.2584. [DOI] [PubMed] [Google Scholar]
- 42.Karkkainen JM, Miilunpohja S, Rantanen T, Koskela JM, Jyrkka J, Hartikainen J, et al. Alcohol Abuse Increases Rebleeding Risk and Mortality in Patients with Non-variceal Upper Gastrointestinal Bleeding. Dig Dis Sci. 2015;60:3707–15. doi: 10.1007/s10620-015-3806-6. [DOI] [PubMed] [Google Scholar]


