Abstract
Background/Aim:
Recently, endoscopic ultrasound-guided gallbladder drainage (EUS-GBD) has emerged using a self-expandable metallic stent (SEMS). The aim of the study was to evaluate the long-term outcomes of this procedure. In addition, the efficacy and safety of EUS-GBD with SEMS were assessed.
Patients and Methods:
Thirteen consecutive patients who underwent EUS-GBD for acute cholecystitis between February 2014 and September 2016 were included in this retrospective study. EUS-GBD was performed under the guidance of EUS and fluoroscopy, through puncturing the gallbladder with a needle, inserting a guidewire, dilating the puncture hole, and placing a SEMS.
Results:
The rates of technical success, functional success, and adverse events were 100%, 92.3% and 7.7%, respectively. The median procedure time was 26.9 min (range 19–42 min). The median follow-up time was 240 days (range 14–945 days) and during this follow-up period recurrence of cholecystitis was observed in one patient (7.7%).
Conclusion:
EUS-GBD with a SEMS is a possible alternative treatment for acute cholecystitis in high surgical risk patients. Long-term outcomes after EUS-GBD were promising.
Keywords: Cholecystitis, endoscopic ultrasond-guided biliary drainage, endoscopic ultrasound- guided gallbladder drainage, endoscopic
INTRODUCTION
Laparoscopic cholecystectomy is currently considered the treatment of choice for most patients with acute cholecystitis.[1,2,3] In high surgical risk patients such as having an advanced malignant tumor or other severe organ failures, gallbladder drainage is considered an alternative method. Percutaneous transhepatic gallbladder drainage (PTGBD) is the gold standard method for gallbladder drainage.[4,5] However, PTGBD has also several potential complications, including bleeding, decreasing of patient's quality of life due to external drainage, and it is unsuitable for patients who have massive ascites or dementia, which may lead to the possibility of tube dislodgement.[6]
For these conditions, percutaneous transhepatic gallbladder aspiration and endoscopic transpapillary gallbladder drainage with either nasobiliary drainage tube or stent placement are usually performed as an alternative.[7]
Recently, endoscopic ultrasound-guided gallbladder drainage (EUS-GBD) has emerged for acute cholecystitis.[8,9,10,11,12,13,14,15] However, adverse events can occur after the EUS-GBD procedure such as stent occlusion and stent migration which may be fatal. Moreover, the long-term outcome of EUS-GBD is still unclear.
The aim of this study was to evaluate long-term outcomes of EUS-GBD in high-risk patients with acute cholecystitis who are not candidates for surgical intervention. Also, safety and efficacy of fully covered self-expandable metal stent (FCSEMS) with inside pigtail plastic stent were assessed.
PATIENTS AND METHODS
Patients
In this study, consecutive patients who underwent EUS-GBD for acute cholecystitis between February 2014 and September 2016 were retrospectively included. During this period, PTGBD was done in six patients and cholecystectomy was performed in 62 patients. In our hospital, the indications of EUS-GBD in acute cholecystitis were the following: having an advanced malignant tumor, severe organ failures, or risk of self removal of tube in case of percutaneous drainage.
The patients were continuously followed up by blood tests and imaging modalities (abdominal ultrasonography and computed tomography (CT) for detection of stability of the stent and patency of cystic duct in patients in whom stent was removed) every 2–4 months. Patients provided their written, informed consent for all procedures associated with the study. This study was approved by the Hospital's Institutional Review Board (IRB) for human research.
Technical tips of endoscopic ultrasound-guided gallbladder drainage
All patients were given antibiotics prior to the procedure. Also, all patients performed abdominal CT the day after EUS-GBD to confirm the stable position of the stent as stent migration may be fatal.
First, an echoendoscope (GF-UGT260; Olympus Optical, Tokyo, Japan) was introduced into the stomach or duodenum. The echoendoscope was manipulated until an appropriate puncture route, free from interposing vessels, using color Doppler was identified. The puncture site was selected as the region where the distance between the gastrointestinal tract and the gallbladder was smallest (1 cm or less). When both the stomach and duodenum provided equally good access, the duodenum was preferred because it was easier to maintain the scope position at the duodenum than at the stomach.
While approaching the gallbladder from the stomach, body of the gallbladder was the preferred target as it can be easily accessed from the gastric antrum. On the other hand, in approaching the gallbladder from the duodenum, the neck of the gallbladder (which is the part attached to cystic duct) was the ideal target as it can be easily accessed from duodenal bulb. And from the anatomical point of view, for better placement of stent. Puncture directed toward the neck of gallbladder is preferred as this area is less mobile and its movement away from the duodenal wall is less likely.[16] Then, the neck or body of the gallbladder was punctured with a 19 G fine-needle aspiration (FNA) (Sonotip pro control 19 G; Medi-Globe GmbH, Rosenheim, Germany) under EUS guidance.
Bile juice was aspirated and a small amount of contrast medium was injected. Then, 0.025-inch guidewire (VisiGlide; Olympus Medical Systems, Tokyo, Japan) was then inserted into the gallbladder through the FNA needle. Next, fine gauge balloon catheter (4 mm, REN; KANEKA, Osaka, Japan) was inserted, and the gallbladder and the intestinal wall were dilated. After this procedure, FCSEMS placement (BONA stent, Standard Sci Tech Inc., Seoul, Korea) from the gallbladder to the intestine was performed under EUS and fluoroscopic guidance using intrachannel release technique in which we stabilized EUS scope until the stent was deployed up to 1 cm within the scope. Then, the EUS scope was pulled a little bit after stent delivery system was pushed. Finally, the stent release was performed mainly under the endoscopic view guidance. A double pigtail plastic stent (7Fr, 10 cm, Cook Medical, Bloomington, Indiana, USA) was placed within the metallic stent to prevent stent migration.[11] In some patients we used 6 cm FCSEMS with 10 cm inside pigtail plastic stent, while in other patients we used 8 cm FCSEMS with 12 cm pigtail plastic stent.
Definitions
The follow-up period was measured from the day of performance of EUS-GBD to the final observation. Procedure time was also measured from echoendoscope insertion to stent placement. Technical success was defined as successful FCSEMS and plastic stent deployment. Functional success was also defined as complete resolution of clinical symptoms, such as abdominal pain and fever, or decreased inflammation or liver enzymes on blood tests.
Recurrence of acute cholecystitis after EUS-GBD was defined based on the characteristic clinical features such as abdominal pain and fever, laboratory data, and imaging studies. Adverse events of EUS-GBD included early adverse events (<2 weeks) and late adverse events (>2 weeks) and were defined according to the American Society for Gastrointestinal Endoscopy Lexicon's severity grading system.[17]
The patients had severe underlying diseases such as advanced cholangiocarcinoma, advanced pancreatic adenocarcinoma, severe cerebrovascular diseases (e.g., cerebral infarction, carotid aneurysm), and cardiopulmonary diseases (e.g., congestive heart failure, hypertrophic cardiomyopathy) for which surgery and general anesthesia carried high risk. Also, PTGBD was refused by some patients because of poor performance status and risk of inadvertent tube dislodgement. In addition, few patients had dementia for which PTGBD was inconvenient.
The severity of each patient's condition was assessed by American Society of Anesthesiologists physical status (ASA PS) classification.[18]
Statistical analysis
Results are given as medians (range) and means (±standard deviation [SD]). The patients' characteristics were compared by Student's t-test for continuous variables and Fisher's exact test for categorical variables. All statistical analyses were performed using Statistical Package for the Social Sciences version 23 (IBM Corp., Armonk, New York, USA) statistical software.
RESULTS
Patients' characteristics
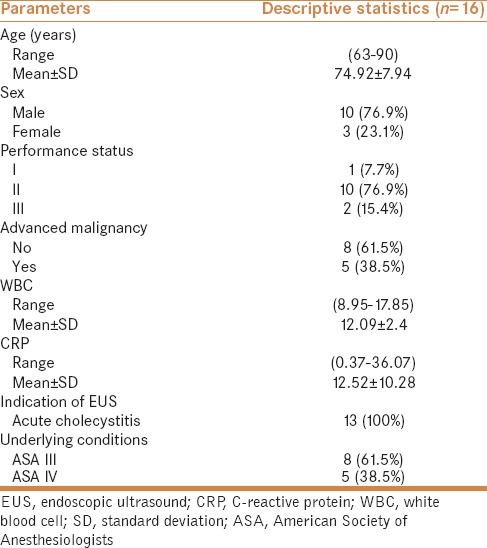
Totally, 13 patients (mean age 74.92 years, range 63–90 years; 10 males, 3 females) were enrolled for the study [Table 1]. Eight patients were ASA class III and five patients were ASA class IV. Also, five patients had advanced malignancy (one patient had renal cell carcinoma with pancreatic metastasis, another patient had pancreatic cancer with liver and lymph node metastasis, another patient had combined pancreatic cancer and cholangiocarcinoma, and two patients had advanced cholangiocarcinoma). On blood examination, the mean white blood cell (WBC) count was 12.09 μl−1, and the mean C-reactive protein (CRP) was 12.52 mg/dl. Indication for EUS-GBD was acute cholecystitis (n = 13).
Table 1.
Patients' characteristics
Results of endoscopic ultrasound-guided gallbladder drainage
Table 2 shows the results of EUS-GBD. EUS-GBD was performed and was technically successful in all patients and functionally successful in 12 patients. The EUS-GBD procedure was performed via the stomach and duodenum in four and nine cases, respectively. The median procedure time was 26.9 min (range 19–42 min). On CT imaging, stent migration was not seen in any patients, and swelling of the gallbladder was resolved. However, pneumoperitoneum was seen in one patient and responded well to conservative treatment.
Table 2.
Results of EUS-GBD
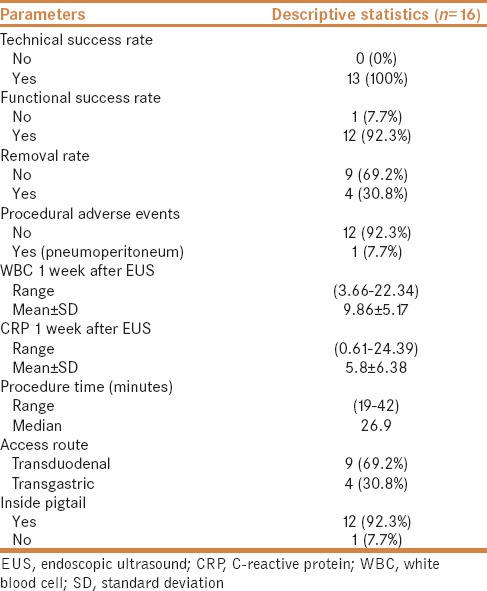
Seven days after EUS-GBD, the mean WBC count was 9860 μl−1 (range 3660–22340 μl−1), and CRP was 5.8 mg/dl (range 0.61–24.39 mg/dl).
Long-term outcomes after endoscopic ultrasound-guided gallbladder drainage
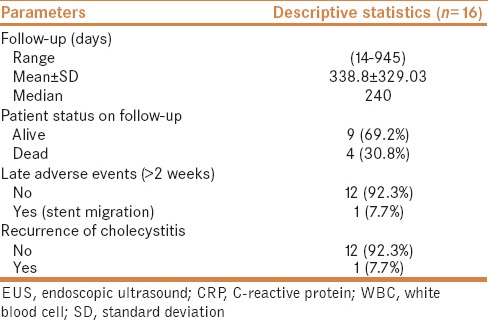
Table 3 shows the long-term outcomes after EUS-GBD. The median follow-up time was 240 days (range 14–945 days). Recurrence of cholecystitis based on clinical symptoms, laboratory markers, and imaging studies was observed in one patient (7.7%). Also, during this period, four patients died due to underlying comorbid diseases (advanced malignancy in two, cardiopulmonary diseases in one, and severe pneumonia in one patient). Of those four patients, two patients lived for 6 months after EUS-GBD and the other two patients lived for 1 month. Moreover, distal stent migration was seen by abdominal CT in one patient 2 weeks after EUS-GBD for whom another EUS was done and the stent was removed and was not replaced as there was no recurrence of cholecystitis.
Table 3.
Long-term outcomes after EUS-GBD
DISCUSSION
The aim of the current study was to evaluate the feasibility and safety of EUS-GBD in patients with acute cholecystitis who are not candidates for cholecystectomy. In high surgical risk patients with acute cholecystitis, gallbladder drainage is considered an alternative treatment. PTGBD is considered the first-line drainage method. However, this drainage method is not indicated for patients who have massive ascites or are on anticoagulant therapy.[11]
Moreover, PTGBD has several disadvantages such as biliary peritonitis, pneumothorax, and bleeding, which can occur in up to 12% of cases.[4] Also, patients' quality of life may be decreased due to external drainage and postprocedural pain, and inadvertent tube dislodgement or migration has been reported in up to 12% of cases.[19] Furthermore, recurrence of cholecystitis after PTGBD tube removal occurred in 22–47% of cases if surgical treatment was not performed.[20,21]
On the contrary, EUS-GBD can be performed in patients taking anticoagulant therapy because the gastrointestinal tract is less vascular than the liver and it is associated with improved patients' quality of life.[10,22] If EUS-GBD is performed using self-expandable metallic stent (SEMS) or another large diameter metallic stent, compared with a PTGBD tube, a greater drainage effect may be obtained.[11]
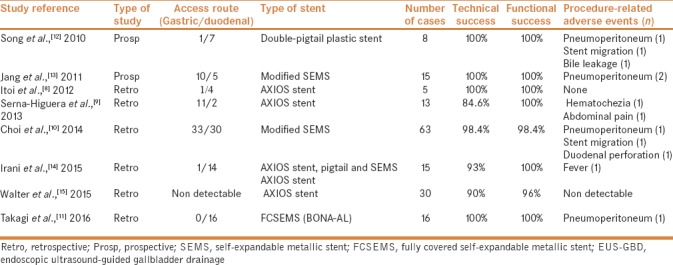
Previous reports about EUS-GBD (including at least five cases and excluding nasobiliary tube only) are summarized in Table 4.[8,9,10,11,12,13,14,15] The reported technical success rate of EUS-GBD ranged from 84.6 to 100%, and the functional success rate ranged from 96 to 100%. The puncture sites were transgastric in 42.2% (57/135) and transduodenal in 57.8% (78/135). The stents used with EUS-GBD were pigtail plastic stents, BONA-AL metallic stents, or AXIOS metallic stents. The most frequent adverse events were pneumoperitoneum (n = 4) and stent migration (n = 3). Also, recurrence of cholecystitis was seen in previous reports.[10,15]
Table 4.
Overview of outcomes of EUS-GBD
The methods and devices used for EUS-GBD have not yet been standardized. Technical tips for the present technique are divided into two important points: (1) to puncture the gallbladder neck and (2) to use relatively long SEMS and pigtail stents. EUS-GBD has two puncture sites. One is transgastric and the other is transduodenal. If EUS-GBD is performed via transgastric approach, the gallbladder body is normally punctured and this may be associated with increased risk of bile leakage and distal stent migration which may be attributed to the relatively long distance between the gallbladder and the stomach. On the contrary, if it is performed via transduodenal approach, the neck of the gallbladder is punctured. Puncturing of the gallbladder neck is preferred because it is less mobile, making stent migration less likely to occur, and the top of the stent is directed toward gallbladder fundus making it difficult for food or sludge to flow into the common bile duct through the cystic duct.[23] In addition, the inflamed gallbladder becomes adherent to the duodenal wall, making bile leakage through puncture site less likely to occur.[16] Most studies did not mention the reason of transduodenal approach vs. transgastric approach. However, Walter et al. hypothesized that transduodenal access may result in less tissue reaction after longer stent dwell time, so it was considered the access of choice.[15] In our study, transduodenal approach with puncturing gallbladder neck was performed in nine patients, while transgastric approach with puncturing gallbladder body was performed in four patients in whom puncturing gallbladder neck was technically difficult. Also, we usually obstruct the cystic duct using a relatively long FCSEMS. Then, a pigtail plastic stent is inserted inside the FCSEMS. This pigtail plastic stent has two important roles: One is to prevent stent migration, and the other is to prevent food flowing into the gallbladder.[11]
Recently, a novel metallic stent with anchor flanges and flares is available for EUS-GBD, and it may be much better than straight FCSEMS in preventing stent migration.[24,25,26] However, if this flanged metallic stent is not used, a pigtail plastic stent should be added into the straight metallic stent.[27] In a systematic review of EUS-GBD, lumen apposing metal stent seemed to have higher efficacy and safety; however, its technical success was lower compared to conventional biliary SEMS (91.5% vs. 98.6%, respectively).[28]
In the present study, patients were followed after EUS-GBD to assess if clinical symptoms or stent-related adverse events occurred or not to avoid unnecessary interventions. Our findings were comparable with a study done by Choi et al., who followed patients after EUS-GBD (median 275 days; range 40–1185 days), and during that follow-up period, 54 patients (96.4%) had no recurrence of cholecystitis.[10]
Even when stent migration occurs, patients are less likely to have a recurrence of cholecystitis, presumably due to the maturation of cholecystoenteric fistula.[10] Also, our findings were compared with a study done by Kamata et al., who followed patients after EUS-GBD (median 304 days; range 78–1492 days), and during that follow-up period, 11 patients (91.7%) had no recurrence of cholecystitis.[29]
The study is limited by its single-center retrospective design, small sample size, and the lack of a control group.
CONCLUSION
In conclusion, EUS-GBD with a FCSEMS and inside pigtail plastic stent performed by an experienced endosonographer has good long-term outcomes and can be an effective and safe alternative treatment for patients with acute cholecystitis who are unsuitable for surgical interference. However, a prospective, randomized, adequately powered head-to-head comparison of PTGBD and EUS-GBD is required.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Spira RM, Nissan A, Zamir O, Cohen T, Fields SI, Freund HR. Percutaneous transhepatic cholecystostomy and delayed laparoscopic cholecystectomy in critically ill patients with acute calculus cholecystitis. Am J Surg. 2002;183:62–6. doi: 10.1016/s0002-9610(01)00849-2. [DOI] [PubMed] [Google Scholar]
- 2.Yi NJ, Han HS, Min SK. The safety of a laparoscopic cholecystectomy in acute cholecystitis in high-risk patients older than sixty with stratification based on ASA score. Minim Invasive Ther Allied Technol. 2006;15:159–64. doi: 10.1080/13645700600760044. [DOI] [PubMed] [Google Scholar]
- 3.Lo CM, Liu CL, Fan ST, Fan ST, Lai EC, Wong J. Prospective randomized study of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Ann Surg. 1998;227:461–7. doi: 10.1097/00000658-199804000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McGahan JP, Lindfors KK. Percutaneous cholecystostomy: An alternative to surgical cholecystostomy for acute cholecystitis? Radiology. 1989;173:481–5. doi: 10.1148/radiology.173.2.2678261. [DOI] [PubMed] [Google Scholar]
- 5.Kiviniemi H, Makela JT, Autio R, Tikkakoski T, Leinonen S, Siniluoto T, et al. Percutaneous cholecystostomy in acute cholecystitis in high-risk patients: An analysis of 69 patients. Int Surg. 1999;83:299–302. [PubMed] [Google Scholar]
- 6.Itoi T, Coelho-Prabhu N, Baron TH. Endoscopic gallbladder drainage for management of acute cholecystitis. Gastrointest Endosc. 2010;71:1038–45. doi: 10.1016/j.gie.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 7.Peñas-Herrero I, de la Serna-Higuera C, Perez-Miranda M. Endoscopic ultrasound-guided gallbladder drainage for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 2015;22:35–43. doi: 10.1002/jhbp.182. [DOI] [PubMed] [Google Scholar]
- 8.Itoi T, Binmoeller KF, Shah J, Sofuni A, Itokawa F, Kurihara T, et al. Clinical evaluation of a novel lumen-apposing metal stent for endosonography-guided pancreatic pseudocyst and gallbladder drainage (with video) Gastrointest Endosc. 2012;75:870–6. doi: 10.1016/j.gie.2011.10.020. [DOI] [PubMed] [Google Scholar]
- 9.De la Serna-Higuera C, Perez-Miranda M, Gil-Simon P, Ruiz-Zorrilla R, Diez-Redondo P, Alcaide N, et al. EUS-guided transenteric gallbladder drainage with a new fistula forming, lumen apposing stent. Gastrointest Endosc. 2013;61:601–6. doi: 10.1016/j.gie.2012.09.021. [DOI] [PubMed] [Google Scholar]
- 10.Choi JH, Lee SS, Choi JH, Park DH, Seo DW, Lee SK, et al. Long-term outcomes after endoscopic ultrasonography-guided gallbladder drainage for acute cholecystitis. Endoscopy. 2014;46:656–61. doi: 10.1055/s-0034-1365720. [DOI] [PubMed] [Google Scholar]
- 11.Takagi W, Ogura T, Sano T, Saori O, Atsushi O, Daisuke M, et al. EUS-guided cholecystoduodenostomy for acute cholecystitis with an anti-stent migration and anti-food impaction system; a pilot study. Ther Adv Gastroenterol. 2016;9:19–25. doi: 10.1177/1756283X15609285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Song TJ, Park Do H, Eum JB, Moon SH, Lee SS, Seo DW, et al. EUS-guided cholecystoenterostomy with single-step placement of a 7F double-pigtail plastic stent in patients who are unsuitable for cholecystectomy: A pilot study (with video) Gastrointest Endosc. 2010;71:634–40. doi: 10.1016/j.gie.2009.11.024. [DOI] [PubMed] [Google Scholar]
- 13.Jang JW, Lee SS, Park do H, Seo DW, Lee SK, Kim MH, et al. Feasibility and safety of EUS-guided transgastric/transduodenal gallbladder drainage with single-step placement of a modified covered self-expandable metal stent in patients unsuitable for cholecystectomy. Gastrointest Endosc. 2011;74:176–81. doi: 10.1016/j.gie.2011.03.1120. [DOI] [PubMed] [Google Scholar]
- 14.Shayan I, Todd HB, Ian SG, Mouen AK. EUS-guided gallbladder drainage with a lumen-apposing metal stent. Gastrointest Endosc. 2015;82:1110–5. doi: 10.1016/j.gie.2015.05.045. [DOI] [PubMed] [Google Scholar]
- 15.Walter D, Teoh A, Itoi T, Miranda M, Larghi A, Yague A, et al. EUS-guided gall bladder drainage with alumen-apposing metal stent: A prospective long-term evaluation. Gut. 2016;65:6–8. doi: 10.1136/gutjnl-2015-309925. [DOI] [PubMed] [Google Scholar]
- 16.Choi J, Lee S. Endoscopic ultrasonography-guided gallbladder drainage for acute cholecystitis: From evidence to practice. Dig Endosc. 2015;27:1–7. doi: 10.1111/den.12386. [DOI] [PubMed] [Google Scholar]
- 17.Cotton PB, Eisen GM, Aabakken L, Hutter MM, Jacobson BC, Mergener K, et al. A lexicon for endoscopic adverse event: Report of an ASGE workshop. Gastrointest Endosc. 2010;71:446–54. doi: 10.1016/j.gie.2009.10.027. [DOI] [PubMed] [Google Scholar]
- 18.Fitz-Henry J. The ASA classification and perioperative risk. Ann R Coll Surg Engl. 2011;93:185–7. doi: 10.1308/147870811X565070a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ito K, Fujita N, Noda Y, Kobayashi G, Kimura K, Sugawara T, et al. Percutaneous cholecystostomy versus gallbladder aspiration for acute cholecystitis: A prospective randomized controlled trial. AJR Am J Gastroenterol. 2004;183:193–9. doi: 10.2214/ajr.183.1.1830193. [DOI] [PubMed] [Google Scholar]
- 20.Mckay A, Abulfaraj M, Lipschitz J. Short- and long-term outcomes following percutaneous cholecystostomy for acute cholecystitis in high-risk patients. Surg Endosc. 2012;26:1343–51. doi: 10.1007/s00464-011-2035-0. [DOI] [PubMed] [Google Scholar]
- 21.Kimura Y, Takada T, Strasberg SM, Pitt HA, Gouma DJ, Garden OJ, et al. TG13 current terminology, etiology, and epidemiology of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2013;20:8–23. doi: 10.1007/s00534-012-0564-0. [DOI] [PubMed] [Google Scholar]
- 22.Jang JW, Lee SS, Song TJ, Hyun YS, Park DY, Seo DW, et al. Endoscopic ultrasound-guided transmural and percutaneous transhepatic drainage are comparable for acute cholecystitis. Gastroenterology. 2012;142:805–11. doi: 10.1053/j.gastro.2011.12.051. [DOI] [PubMed] [Google Scholar]
- 23.Itoi T, Itokawa F, Kurihara T. Endoscopic ultrasound-guided gallbladder drainage: Actual technical presentations and review of the literature (with video) J Hepatobiliary Pancreat Sci. 2011;18:282–6. doi: 10.1007/s00534-010-0310-4. [DOI] [PubMed] [Google Scholar]
- 24.Turner BG, Rotam S, Paddu NU Trost D, Jamal-Kabani A, Gaidhane M, et al. Cholecystoduodenal drainage and gallstone removal in a patient with cholecystitis and unresectable cholangiocarcinoma. Endoscopy. 2013;45:E114–5. doi: 10.1055/s-0032-1325968. [DOI] [PubMed] [Google Scholar]
- 25.Mönkemüller K, Zabielski M, Didowacz-Grollmann A, von Gruchalla C, Neumann H, Vormbrock K. Endoluminal transgastric endoscopic anastomosis of the gallbladder using an anchoring self-expanding metal stent. Endoscopy. 2013;45:E164–6. doi: 10.1055/s-0032-1325776. [DOI] [PubMed] [Google Scholar]
- 26.Dollhopf M, Larghi A, Will U, Rimbaş M, Anderloni A, Sanchez-Yague A, et al. EUS-guided gallbladder drainage in patients with acute cholecystitis and high surgical risk using an electrocautery-enhanced lumen-apposing metal stent device. Gastrointest Endosc. 2017;86:636–43. doi: 10.1016/j.gie.2017.02.027. [DOI] [PubMed] [Google Scholar]
- 27.Ogura T, Masuda D, Imoto A, Umegaki E, Higuchi K. EUS-guided gallbladder drainage and hepaticogastrostomy for acute cholecystitis and obstructive jaundice (with video) Endoscopy. 2014;46(suppl 1):E75–6. doi: 10.1055/s-0033-1359135. [DOI] [PubMed] [Google Scholar]
- 28.Anderloni A, Buda A, Vieceli F, Khashab MA, Hassan C, Repici A. Endoscopic ultrasound-guided transmural stenting for gallbladder drainage in high-risk patients with acute cholecystitis: A systematic review and pooled analysis. Surg Endosc. 2016;30:5200–8. doi: 10.1007/s00464-016-4894-x. [DOI] [PubMed] [Google Scholar]
- 29.Kamata K, Takenaka M, Kitano M, Omoto S, Miyata T, Minaga K, et al. Endoscopic ultrasound-guided gallbladder drainage for acute cholecystitis: Long-term outcomes after removal of a self-expandable metal stent. World J Gastroenterol. 2017;23:661–7. doi: 10.3748/wjg.v23.i4.661. [DOI] [PMC free article] [PubMed] [Google Scholar]


