Abstract
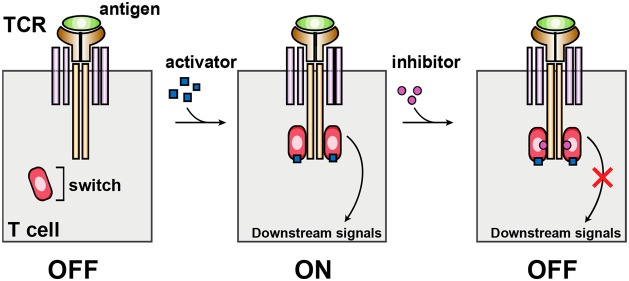
T cells expressing tumor-specific T cell receptors are promising cancer therapeutic agents, but safety control switches are needed to manage potential side effects arising from overactivity. Here, we present the first dual small molecule-gated ZAP70 signaling switch for the regulation of T cell activity. We show that when an analogue-sensitive ZAP70 allele is fused to the engineered ligand binding domain of the estrogen receptor, ERT2, its activity can be upregulated to an extent by a metabolite of an FDA-approved tamoxifen, 4-hydroxy-tamoxifen, and downregulated by an ATP analogue, 3-MB-PP1. The strength of early T cell signaling can also be modulated by varying the concentrations of activator and inhibitor, and the switch exhibits temporal control on the time scale of minutes. Interestingly, the switch has the ability to control CD69 and calcium levels in T cells but has limited capabilities in the regulation of downstream cytokine release, suggesting further investigation is needed before it can be implemented in adoptive T cell therapy.
Cellular immunotherapy has shown promising clinical results in the treatment of cancer. Several clinical trials have demonstrated its efficacy in treating patients with B cell malignancies, and positive responses have been observed in the treatment of other cancers, such as metastatic melanoma, colorectal cancer, and multiple myeloma.1−10 While encouraging, T cell overactivity leading to cytokine release syndrome (CRS) is still a major issue to contend with in clinical practice.11−16 In severe cases of CRS, the uncontrolled immune response can lead to patient deaths.17−20
To improve safety, various genetic switches have been developed for controlling T cell activity, including ON or OFF switches.21−27 While such technologies can be effective, there are still challenges that need to be addressed. Kill switches are an example of such an OFF switch, and are effective at eliminating overactive T cells by inducing apoptosis, but they also destroy the valuable therapeutic agents. This can have drawbacks if the patient requires the use of the engineered cells later during treatment. Furthermore, cells may lose expression of the suicide gene due to silencing, or develop a resistance to the gene by upregulating antiapoptotic genes.28 Additionally, many switches have been designed to be compatible with chimeric antigen receptors (CARs), which are synthetic receptors that use an antibody-derived domain for cell targeting. However, these switches are often incorporated into the CAR design directly and would thus not work for cells employing endogenous or engineered T cell receptors (TCRs). Current switch technologies are also often regulated by a single drug that can only turn ON or OFF T cell activity. To reverse the T cell activity would require the drug inducer to be degraded, which can be time-consuming. In the event of CRS, symptoms can begin 1 h after infusion, indicating how quickly the effect can manifest and highlighting the need for rapid control.29 As such, a dual gated switch that can be regulated by two small molecules, one for ON and one for OFF function, could be more advantageous for tighter temporal control.
Zeta-chain-associated protein kinase 70 (ZAP70) is a critical cytoplasmic protein tyrosine kinase that is involved in the signal transduction of T cell activation.30−34 During T cell activation, the SH2 domains of ZAP70 bind to phosphorylated CD3 immunoreceptor tyrosine-based activation motifs (ITAMs), positioning the kinase to phosphorylate and activate downstream proteins, such as linker of activated T cells (LAT) and lymphocyte cytosolic protein 2 (SLP76).35−39 Studies have shown that ZAP70-deficient T cells display defective TCR-mediated T cell activation.40−43 Its early involvement in the activation pathway also suggests ZAP70 has extensive control over the various signaling cascades that stem from its activation, making it a suitable target for regulating T cell activity.
Despite the essential role that ZAP70 plays in T cell activation, few technologies have been developed for controlling its activity. Previous work on ZAP70 has included regulatable expression of ZAP70 in an effort to control TCR activity, as well as the creation of an analogue-sensitive version of ZAP70 that can be inhibited by a small molecule.44−46 While these methods of control are effective, regulation on a transcriptional or translational level requires time for these processes to occur. Furthermore, tighter control over ZAP70 activity would enable more precise regulation of T cell activity.
Here, we describe a dual-gated ZAP70 protein switch for regulating early T cell signaling. The switch is generated by fusing an ERT2 domain to the above-mentioned analogue-sensitive ZAP70, and shows swift temporal control using two distinct small molecules, 4-hydroxy-tamoxifen and 3-MB-PP1, to turn on and off protein activity, respectively. Dynamics results indicate that the ZAP70 switch introduces tight temporal control over early signaling in the TCR pathway, with activation in less than 2 min and inhibition within 1 min. The ON-OFF switch can also be used to modulate the strength of activation by varying concentrations of activator and inhibitor. While the switch is able to regulate early T cell activation markers, we found that ON switch activity resulted in stunted cytokine release, suggesting that the fusion of ERT2 to ZAP70 is inhibiting its downstream effector function. In order for the switch to meet the need for effective control in T cell immunotherapy, further exploration is needed to understand the cause of this constraint.
Results and Discussion
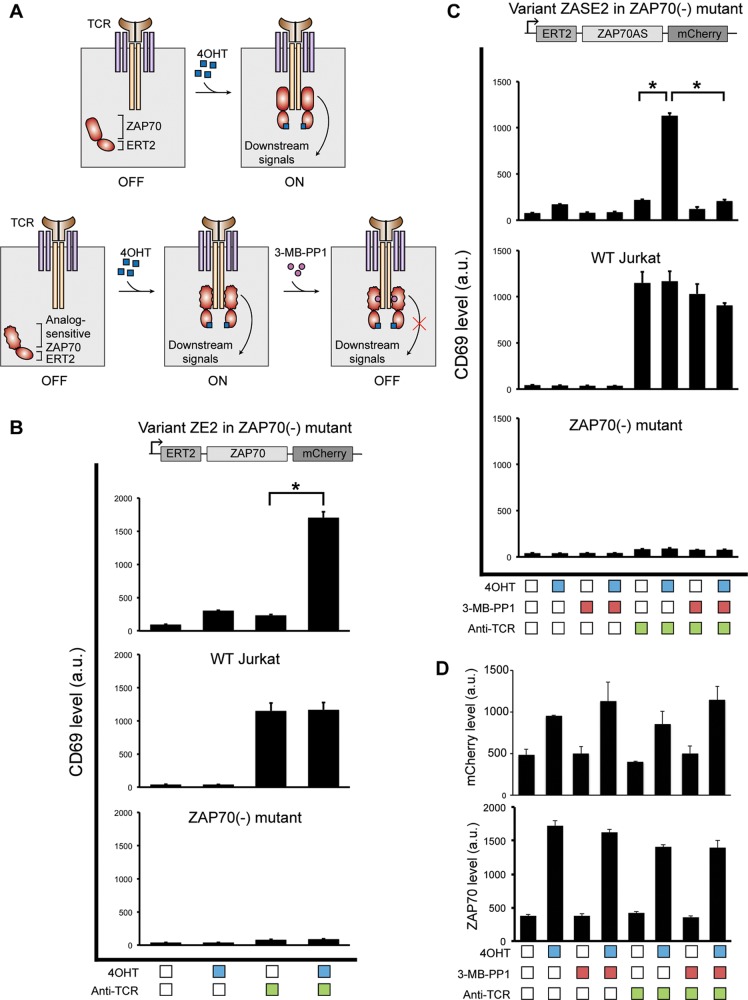
Control over TCR Activity
To develop a dual-gated system for regulating T cell activity, we engineered the ZAP70 to be sensitive to small molecule regulation. We found serendipitously that by fusing an ERT2 domain to the N-terminus of ZAP70, we were able to render ZAP70 inactive. The switch was also linked to an mCherry fluorescent protein to detect expression in cells, and facilitate later downstream sorting of switch-expressing cells. When the ERT2-ZAP70 (ZE) switch was introduced into ZAP70-deficient Jurkat T cells (P116),43 the addition of 4-hydroxy-tamoxifen (4OHT) alleviated the inhibition and allowed ZAP70 to transduce the signal originated from the TCR and subsequently upregulate expression of CD69, a marker of T cell activation (Figure 1a top, 1b). It was also found that certain configurations of the ERT2-ZAP70 fusion protein did not exhibit this ON-activity as strongly as others (Figure S1). The addition of 4OHT to wild-type Jurkat cells or P116 did not impact CD69 expression, suggesting its specificity for ERT2-ZAP70 (Figure 1b).
Figure 1.
Characterization of the ON-OFF switch with TCRs. (A) Schematic illustrating the mechanisms for the ZAP70 ON and ON-OFF switches. (B) Various cell lines were treated with combinations of activator and anti-TCR antibody, and CD69 levels analyzed by flow cytometry (mean ± s.d., n = 3, *P < 0.0001). (C) CD69 levels for cells incubated with combinations of activator, inhibitor, and anti-TCR antibody (mean ± s.d., n = 3, *P < 0.0001). (D) mCherry and ZAP70 levels for ZASE-expressing P116 cells under various small molecule conditions.
Previous work has shown that when the gatekeeper methionine residue of the ZAP70 kinase domain is mutated to alanine, a nonfunctional analogue of adenosine triphosphate (ATP), the small molecule 3-MB-PP1 can bind to the ATP pocket and inhibit kinase activity. 3-MB-PP1 therefore acts as a competitive inhibitor, thus serving as an OFF switch for T cells expressing only this analogue-sensitive (AS) ZAP70 allele.44 We tested whether our ERT2-ZAP70 switch could be combined with the analogue-sensitive allele of ZAP70 into a single protein to generate the first dual small molecule-gated ZAP70 switch (Figure 1a bottom). Similar to the ERT2-ZAP70 switch, variants of the ERT2 domain and analogue-sensitive ZAP70 were tested, and results showed that the effectiveness of the ON activity from the ERT2-ZAP70 constructs carried over to their respective ZAP70-AS-ERT2 (ZASE) constructs (Figure S2). ZASE2 was chosen as the final ZASE construct due to the high CD69 levels resulted in the presence of 4OHT and anti-TCR antibody (C305), while preserving low levels with anti-TCR antibody alone. Indeed, CD69 levels indicate that the activity of the ZAP70-AS-ERT2 protein was induced by 4OHT and potently inhibited by 3-MB-PP1 (Figure 1c). When cells expressing the switch fused to mCherry were treated with 4OHT, an elevation of both mCherry and ZAP70 was also noted (Figure 1d). Interestingly, when IL-2 levels were analyzed for the ZE and ZASE switches, little elevation in IL-2 was observed when the switches were turned on compared to what was observed for the activation of wild-type ZAP70, suggesting that there may be functional limitations to the ON-OFF switch (Figure S3). There is, however, a small IL-2 increase with ON switch conditions in comparison with the other combinations of small molecules, though this is more prominent in the ZE switch than ZASE. Furthermore, 3-MB-PP1 has shown slight nonspecific inhibition of wild-type ZAP70, though its effect is minimal (Figure 1c). The inhibitor showed the same nonspecificity for ERT2-ZAP70 as well, which was expected (Figure S4).
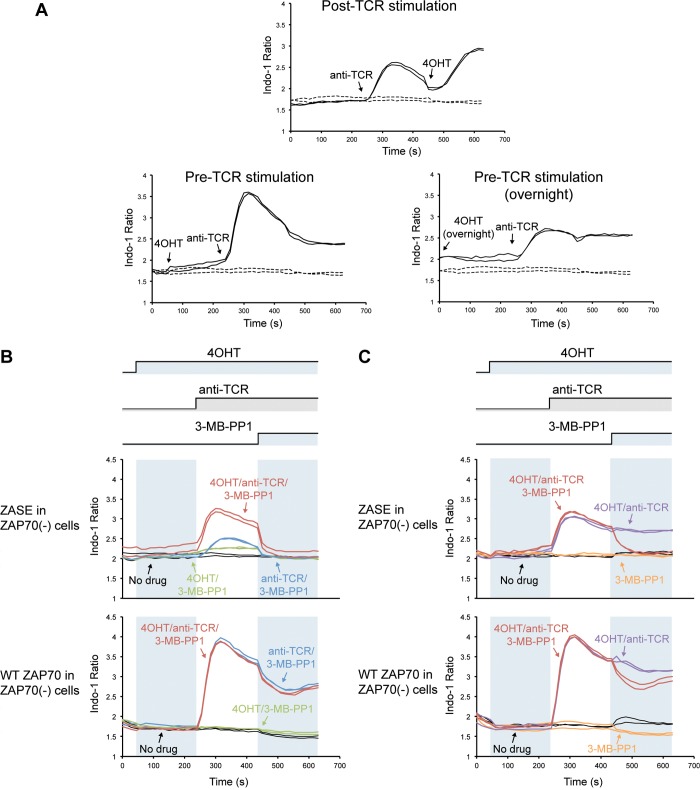
Dynamics of ZAP70 Switch
Upon activation of the TCR, a rise in intracellular calcium is known to occur.47−49 To test the dynamics of ZASE, P116 cells expressing the switch were loaded with the Indo-1 AM dye to measure intracellular calcium flux while treated with various combinations of 4OHT, 3-MB-PP1, and anti-TCR antibody. To study the dynamics of ZASE ON activity, cells expressing the ZAP70 switch were incubated with 4OHT at different time points relative to stimulation of the TCR. When the TCR was stimulated, a transient increase in calcium was observed. Subsequent addition of 4OHT resulted in a further increase in calcium levels. This elevation in intracellular calcium was initiated immediately after 4OHT was added, though peak calcium levels were achieved in just below 2 min (Figure 2a top). Treatment of cells with 4OHT alone resulted in no calcium flux, until the TCR was stimulated. At this point, the increase in calcium was greater than if 4OHT had been added post-C305 (Figure 2a bottom left). Cells preincubated with 4OHT overnight prior to stimulation of the TCR showed an increase in calcium when the TCR was stimulated, which was comparable to stimulation of the TCR alone. However, the peak calcium level was sustained for a longer time (Figure 2a bottom right).
Figure 2.
Calcium dynamics under varying small molecule conditions. (A) Intracellular calcium levels of ZASE-expressing P116 cells, with 4OHT added at different time points relative to stimulation of TCR. Control cells with no 4OHT or anti-TCR antibody are repeated in each panel for comparison with basal calcium levels. (B) Activation controls for cells expressing ZASE or wild-type ZAP70. Cells were treated with or without 4OHT, and with or without anti-TCR antibody. All cells were then inhibited with 3-MB-PP1. (C) Inhibition controls for cells expressing ZASE or wild-type ZAP70. Cells were treated with or without activation drugs, and with or without 3-MB-PP1.
ZASE-expressing cells were then tested with various combinations of 4OHT and C305 to ensure that activation required both of these molecules. When 4OHT alone was added to cells, no calcium flux was observed, and addition of C305 alone resulted in a slight increase in calcium levels. The largest increase in calcium was observed when cells were treated with both 4OHT and C305 (Figure 2b top). The same conditions tested in cells expressing wild-type ZAP70 indicated calcium elevation whenever C305 was added, with peak levels slightly higher than what is observed with ZASE. These cells did not seem to be affected by the presence of 4OHT, though a mild dip in calcium was seen when 3-MB-PP1 was introduced, likely due to nonspecific inhibition of wild-type ZAP70 (Figure 2b bottom). Additionally, the dynamics of wild-type ZAP70-expressing cells were recapitulated by wild-type Jurkat cells. P116 cells expressing no ZAP70 displayed a small increment in calcium when C305 was added, and it should be noted that a basal level of signaling is present even in the absence of ZAP70. This slight increase is likely due to ZAP70-independent TCR activation pathways that have been tied to intracellular calcium release, but the cells were otherwise unaffected by the molecules (Figure S5).50
It has been previously shown both in vitro and in vivo that 3-MB-PP1 is able to fully inhibit analogue-sensitive ZAP70 in less than a minute, thus providing a rapid OFF switch.44 To verify quick temporal control using 3-MB-PP1, inhibition conditions were also assessed. Combinations of activation using 4OHT and C305, and inhibition using 3-MB-PP1 were tested. Activated ZASE-expressing cells that were subsequently inhibited with 3-MB-PP1 showed calcium levels brought down to basal within 1 min. When these cells were activated but not inhibited, a sustained calcium level was observed. Treatment with only 3-MB-PP1 indicated no change in calcium levels (Figure 2c top). Simultaneous addition of C305 and 3-MB-PP1 resulted in a diminished calcium increase compared to cells that were not treated with inhibitor (Figure S6). Though complete shutdown was not instantaneous, this demonstrates the immediate inhibitory effect 3-MB-PP1 can have on ZASE. The inhibition conditions tested on wild-type ZAP70 cells also demonstrate more clearly that wild-type ZAP70 is marginally inhibited by 3-MB-PP1, as cells without the inhibitor contrastingly maintain their elevated calcium levels (Figure 2c bottom).
To verify that the ZAP70 switch can still be turned ON following inhibition by 3-MB-PP1, cells expressing the switch were preincubated with 4OHT and 3-MB-PP1, then washed with media containing only 4OHT. These cells were then rested for various intervals of time and activated. CD69 levels were measured as a marker for T cell activation. Within 2 h of washing out the drug and activation of cells, CD69 expression in ZASE-expressing cells increased from basal levels to that comparable to cells that had not been inhibited with 3-MB-PP1 (Figure S7 top). This indicates that the inhibitor does not irreversibly bind the switch, and ZASE is able to reactivate fairly quickly following shutdown by the inhibitor. Preincubation of wild-type Jurkat cells with the inhibitor did not hinder CD69 expression, and ZAP70-deficient cells were unaffected by the inhibitor or C305 (Figure S7 bottom).
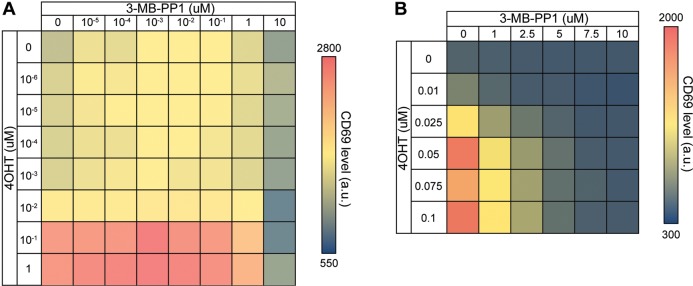
Modulation of TCR Activity
In a clinical setting, patient variability may require treatment conditions to be tailored to the individual. The desired level of T cell activity can also depend on the stage of treatment, and intended immune response. As such, we systematically characterized the dose response profile of ZASE activity with 4OHT and 3-MB-PP1 by measuring CD69 levels, and showed that 10 μM of 3-MB-PP1 can inhibit activity of ZASE at all tested concentrations of 4OHT (Figure 3a). To reduce nonspecific inhibition of wild-type ZAP70, a focused dose response was performed in the range of 0–10 μM and found that 7.5 μM 3-MB-PP1 was sufficient for shutting off ZAP70 activity (Figure 3b). Induction of the switch using 4OHT also occurs as an abrupt change between 0.01 μM to 0.1 μM 4OHT, though the more detailed dose response reveals a gradual increase in T cell activity within this range (Figure 3b). These gradual changes indicate that the intensity of T cell activation can be controlled by altering the concentrations of activator and inhibitor used. The same dose response of small molecules was additionally tested in wild-type Jurkat and P116 cells, and displayed no effect on activation of these cells (Figure S8).
Figure 3.
Modulation of ZASE-controlled TCR activity as measured by CD69 levels, by modifying small molecule doses. (A) ZASE-expressing P116 cells were treated with various concentrations of activator and inhibitor, and CD69 levels analyzed by flow cytometry. A wide range of concentrations were tested. (B) 2-D dose response for ZASE-expressing P116 cells with a narrowed range of concentrations tested.
The modulation of T cell activation using 4OHT was further verified with calcium flux assays on cells expressing the switch. Levels of calcium reached during activation increased in a direct relationship with the concentration of 4OHT up to 0.1 μM. A concentration of 0.01 μM 4OHT led to no further increase in calcium compared to cells treated with no 4OHT, reinforcing the dose response profile seen with CD69 expression (Figure 4). Dynamics data for analogue-sensitive ZAP70 with varying concentrations of 3-MB-PP1 has previously been established to control the extent of inhibition.44
Figure 4.

Calcium dynamics for ZASE-expressing P116 cells using a range of 4OHT concentrations. Cells were loaded with Indo-1 AM dye and treated with various concentrations of 4OHT. Cells were then activated with anti-TCR antibody, and inhibited by 3-MB-PP1.
ZAP70 Switch and CARs
Though both TCRs and chimeric antigen receptors (CARs) contain the CD3ζ domain that ZAP70 is known to interact with, surprisingly ZASE exhibits compatibility issues with CARs. ERT2-ZAP70 and the ZASE construct were introduced into P116 cells expressing a Her2 third generation H3B1 CAR comprising of the CD28 and 4–1BB costimulatory domains, and CD69 levels analyzed as markers of T cell activation. While 3-MB-PP1 was able to turn off T cell activation initiated by CARs, the addition of 4OHT in the absence of Her2 displayed leaky elevated CD69 levels for both ERT2-ZAP70 and ZASE (Figure S9). These raised CD69 levels were observed for Her2 CARs of varying scFv affinity, and additionally a CAR targeting CD19 (data not shown).
The ZASE switch represents the first dual small molecule gated switch in T cells, with a true ON and OFF function that is regulated by two separate drugs. We have shown that the switch is able to control the early T cell activation pathway, as measured by CD69 and intracellular calcium. While the mechanism for the ON switch remains enigmatic, we postulate that it may be attributed to stabilization of the fusion protein when 4OHT is bound to ERT2. This is supported by an increase in mCherry and ZAP70 levels when cells were treated with 4OHT. The use of a mutant estrogen receptor as a destabilization domain has also previously been seen with the distinct mutated estrogen receptor ligand binding domain (ERLBD), whose stabilization is recovered upon the addition of 4OHT.51 The instability from such degradation domains has previously been shown to result in the degradation of the whole fusion protein, which could explain the ability of 4OHT to control mCherry and ZAP70 protein levels.52,53 It is interesting to note that certain configurations of ERT2 and ZAP70 do not encompass this ON switch activity, but rather behave similarly to wild-type ZAP70 by allowing T cells to activate whenever anti-TCR antibody is present. It is possible that the structural conformations of certain ERT2-ZAP70 configurations preclude control by 4OHT.
While in theory the ZAP70 switch should be able to control any receptor including the CD3ζ chain, its curious incompatibility with CARs suggests there is more to its mechanism, and could use additional study. Upon addition of 4OHT, higher expression of the ZAP70 switch was observed in T cells, possibly raising the basal level of CD69 and resulting in the leaky switch behavior observed in CAR-T cells. It would also be interesting to quantify the amounts of CAR and TCR on the surface of the T cells in order to determine whether an excess of CARs to TCRs may be contributing to this leakiness. Furthermore, minimal IL-2 induction is seen following ZE and ZASE activation. As the ZAP70 protein also functions as an adaptor protein, it is conceivable that the presence of the ERT2 domain obstructs its moderation of proteins known to regulate IL-2 production, such as Lck.54 While early T cell activation markers CD69 and intracellular calcium are regulated by the switch, constraints on downstream effector functions like cytokine release can impede its use in immunotherapy application, and should be noted when assessing the limitations on the functionality of this ZAP70 switch.
Calcium flux assays have indicated that the dual-gated switch can be turned on in just under 2 min, and rapidly turned off within a minute. While ON activity takes slightly longer to reach peak calcium levels, the ZAP70 switch still exhibits tight temporal control by 4OHT and 3-MB-PP1. The small molecules also show little to no effect on wild-type ZAP70, emphasizing the specificity they have to the switch. By varying concentrations of activator and inhibitor, we were also able to modulate early T cell signaling through ZASE. The switch thus enables quick regulation over early steps of the T cell activation pathway, with degrees of activity swiftly controlled by small molecule.
The inclusion of ZASE in T cells is a step toward alleviating overactivity issues that are currently observed in cancer immunotherapy. Ideally, if off-target activities are detected in time, the switch could also be used to shut off T cell activity. However, in order for ZASE to have clinical use, the issue of diminished T cell downstream effector function needs to be addressed. To determine if or how ERT2 may be obstructing ZAP70 activity, the current roles of ZAP70 should be further investigated. For example, early interactions such as ZAP70 binding to ITAMs and phosphorylation of ZAP70 by Lck should be verified. The propagation of this signaling should then be explored to determine if ERT2 affects the ability of the kinase to phosphorylate other proteins like LAT and SLP76. If ERT2 poses a steric hindrance on the function of ZAP70, variants of ZASE could be tested that include linkers of different lengths between the two proteins. Alternatively, if an unavoidable characteristic of ERT2 is impeding ZAP70 function, the ERLBD could theoretically serve as the ON switch aspect of ZASE instead, with the added benefit of control by the same drug. We believe that with the right enhancements to ZASE to ameliorate T cell effector function, it could become a suitable technology for improving the safety of T cell immunotherapy. In order to reach this goal, the mechanism of ZASE in the TCR pathway needs to be further studied.
Methods
Plasmids
ZAP70 switches were introduced into human T cells using pHR lentivectors.55 The expression of ZAP70 switches is driven by an EF-1 alpha promoter followed by a kozak sequence. Switches were tagged with an mCherry fluorescent protein through a GS linker (5′-gggtctggctccggatcaagtggtggcagc-3′) to verify expression of the construct in cells and facilitate downstream cell sorting. Plasmids were packaged into lentiviruses using pDelta, Vsvg and pAdv packaging and envelope plasmids.
Cell Culture
Lentiviruses were generated using HEK293FT cells, which were cultured in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% fetal bovine serum (FBS; Thermo Fisher, 10437028), penicillin/streptomycin (Corning, 30001CI), l-glutamine (Corning, 25005CI) and 1 mM sodium pyruvate (Lonza, 13115E). ZAP70-deficient Jurkat T cells, P116, were obtained from the Weiss Lab at UCSF and cultured in RPMI 1640 supplemented with 10% FBS and l-glutamine. Wild-type Jurkat cells were cultured in RPMI 1640 supplemented with 5% FBS, l-glutamine and penicillin/streptomycin. For T cell activation, 2 × 105 cells were added to plate-bound C305 and incubated overnight at 37 °C, 5% CO2. Cells that were not treated with 4OHT (Sigma-Aldrich, H6278–50MG; reconstituted in methanol) or 3-MB-PP1 (Calbiochem, 529582–5MG; reconstituted in dimethyl sulfoxide (DMSO)) were incubated with methanol or DMSO respectively as a control.
Lentivirus Generation and Transduction
HEK293FT cells were grown in 6-well plates and cotransfected with lentivirus packaging/envelope plasmids (described above) and ZAP70 switch-encoding vector using polythylenimine (PEI). Supernatant containing virus was collected after 72 h and spun down to remove remnant cells. P116 cells were infected with virus-containing media for 72 h at 37 °C before washing out the virus.
Surface and Intracellular Staining
For surface staining, cells were stained for CD69 expression using APC-Cy7-conjugated mouse antihuman CD69 antibody (BD Pharmingen, 557756) at a dilution of 1:100. Myc-tagged Her2 CARs were stained using Alexa Fluor 488-conjugated mouse antihuman myc antibody (R&D Systems, IC3696G). 2 × 105 cells were washed twice with FACS buffer (1× phosphate buffered saline (PBS), 0.1% NaN3, 1% BSA, 2 mM EDTA) before incubating with antibody in the dark at room temperature for 40 min. Cells were then washed and resuspended with FACS buffer before analysis on flow cytometer. For intracellular staining, cells were washed with FACS buffer prior to fixation (BD Cytofix, 554655) at room temperature for 10 min, then washed again. The cell membrane was permeabilized by adding 90% cold methanol to cells on ice and cold incubation for 30 min, followed by washing and incubation with antibody. Intracellular staining of ZAP70 protein was performed using Alexa Fluor 488-conjugated mouse anti-ZAP70 antibody (Life Technologies, MHZAP7020) at a dilution of 1:50.
Flow Cytometry
Transduced cells were sorted for mCherry-positive cells at the Boston University Imaging Core using a Sony SH800 Cell Sorter. Cells were treated with 0.1 μM 4OHT prior to sorting. Myc-tagged CAR and CD69 expression levels from T cell activation experiments were measured poststaining using an Attune NxT flow cytometer.
IL-2 ELISA
Supernatant from cells incubated with various combinations of C305, 4OHT, and 3-MB-PP1 was saved and tested in an enzyme-linked immunosorbent assay (ELISA) to measure IL-2 levels. The BD OptEIA human IL-2 ELISA kit (BD Biosciences, 555190) was used according to manufacturer’s instructions with a 0.05% Tween-20 in PBS (Thermo Scientific, 28352) wash buffer, and remaining reagents from BD OptEIA Reagent Set B (BD Biosciences, 550534). ELISAs were performed with 96-well MaxiSorp plates (Thermo Scientific, 442404).
Calcium Dynamics
Intracellular calcium levels were measured by loading 1.5 × 106 cells with 8 μM Indo-1 acetoxymethyl dye (Invitrogen, I1203) diluted in media (RPMI 1640 supplemented with 10% FBS and l-glutamine). Loading specifications of 45 min at 37 °C were used. Cells were then washed in media and incubated in the dark at room temperature for 10 min. Prior to analysis, cells were equilibrated to 37 °C, then read on a SpectraMax M5 (Molecular Devices) at 37 °C. The 400/500 nm emission ratio was taken as a measurement of intracellular calcium.
Reactivation of ZAP70 Switch
Cells were incubated with 0.1 μM 4OHT and 7.5 μM 3-MB-PP1 for 16 h, followed by washing out of 3-MB-PP1 and incubating cells in media containing 4OHT for various durations (2, 4, 8, 16 h). Cells were then added to plate-bound C305 to activate for 16 h, stained for CD69 and measured by flow cytometry. For the 0 h time point, 3-MB-PP1 was not washed out and cells were directly stimulated with C305. Control samples were either incubated with no 3-MB-PP1 and then activated with C305 (positive control), or incubated with 3-MB-PP1 and not activated with C305 (negative control).
Statistics
Data between two groups was compared using an unpaired two-tailed t test. A P-value < 0.05 was considered to be statistically significant.
Acknowledgments
W.W. acknowledges funding from the Boston University Ignition Award, NIH Director’s New Innovator Award (1DP2CA186574), NSF Expedition in Computing (1522074), NSF CAREER (162457), NSF EAGER (1645169), and NSF BBSRC (1614642). We thank Matthew Brenner for suggestions on the manuscript, and Todd Blute from the Boston University imaging core facility for cell sorting assistance.
Supporting Information Available
The Supporting Information is available free of charge on the ACS Publications website at DOI: 10.1021/acssynbio.7b00394.
Supporting Figures (PDF)
Author Contributions
N.W. designed and generated genetic constructs, performed experiments, and generated figures. N.W. and W.W. analyzed data. W.W. conceived the project. N.W. and W.W. wrote the paper. All authors commented on and approved the paper.
The authors declare no competing financial interest.
Supplementary Material
References
- Davila M. L.; Riviere I.; Wang X.; Bartido S.; Park J.; Curran K.; Chung S. S.; Stefanski J.; Borquez-Ojeda O.; Olszewska M.; Qu J.; Wasielewska T.; He Q.; Fink M.; Shinglot H.; Youssif M.; Satter M.; Wang Y.; Hosey J.; Quintanilla H.; Halton E.; Bernal Y.; Bouhassira D. C.; Arcila M. E.; Gonen M.; Roboz G. J.; Maslak P.; Douer D.; Frattini M. G.; Giralt S.; Sadelain M.; Brentjens R. (2014) Efficacy and toxicity management of 19–28z CAR T cell therapy in B cell acute lymphoblastic leukemia. Sci. Transl. Med. 6, 224ra225. 10.1126/scitranslmed.3008226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochenderfer J. N.; Dudley M. E.; Kassim S. H.; Somerville R. P.; Carpenter R. O.; Stetler-Stevenson M.; Yang J. C.; Phan G. Q.; Hughes M. S.; Sherry R. M.; Raffeld M.; Feldman S.; Lu L.; Li Y. F.; Ngo L. T.; Goy A.; Feldman T.; Spaner D. E.; Wang M. L.; Chen C. C.; Kranick S. M.; Nath A.; Nathan D. A.; Morton K. E.; Toomey M. A.; Rosenberg S. A. (2015) Chemotherapy-refractory diffuse large B-cell lymphoma and indolent B-cell malignancies can be effectively treated with autologous T cells expressing an anti-CD19 chimeric antigen receptor. J. Clin. Oncol. 33, 540–549. 10.1200/JCO.2014.56.2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochenderfer J. N.; Wilson W. H.; Janik J. E.; Dudley M. E.; Stetler-Stevenson M.; Feldman S. A.; Maric I.; Raffeld M.; Nathan D. A.; Lanier B. J.; Morgan R. A.; Rosenberg S. A. (2010) Eradication of B-lineage cells and regression of lymphoma in a patient treated with autologous T cells genetically engineered to recognize CD19. Blood 116, 4099–4102. 10.1182/blood-2010-04-281931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee D. W.; Kochenderfer J. N.; Stetler-Stevenson M.; Cui Y. K.; Delbrook C.; Feldman S. A.; Fry T. J.; Orentas R.; Sabatino M.; Shah N. N.; Steinberg S. M.; Stroncek D.; Tschernia N.; Yuan C.; Zhang H.; Zhang L.; Rosenberg S. A.; Wayne A. S.; Mackall C. L. (2015) T cells expressing CD19 chimeric antigen receptors for acute lymphoblastic leukaemia in children and young adults: a phase 1 dose-escalation trial. Lancet 385, 517–528. 10.1016/S0140-6736(14)61403-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maude S. L.; Frey N.; Shaw P. A.; Aplenc R.; Barrett D. M.; Bunin N. J.; Chew A.; Gonzalez V. E.; Zheng Z.; Lacey S. F.; Mahnke Y. D.; Melenhorst J. J.; Rheingold S. R.; Shen A.; Teachey D. T.; Levine B. L.; June C. H.; Porter D. L.; Grupp S. A. (2014) Chimeric antigen receptor T cells for sustained remissions in leukemia. N. Engl. J. Med. 371, 1507–1517. 10.1056/NEJMoa1407222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan R. A.; Dudley M. E.; Wunderlich J. R.; Hughes M. S.; Yang J. C.; Sherry R. M.; Royal R. E.; Topalian S. L.; Kammula U. S.; Restifo N. P.; Zheng Z.; Nahvi A.; de Vries C. R.; Rogers-Freezer L. J.; Mavroukakis S. A.; Rosenberg S. A. (2006) Cancer regression in patients after transfer of genetically engineered lymphocytes. Science 314, 126–129. 10.1126/science.1129003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkhurst M. R.; Yang J. C.; Langan R. C.; Dudley M. E.; Nathan D. A.; Feldman S. A.; Davis J. L.; Morgan R. A.; Merino M. J.; Sherry R. M.; Hughes M. S.; Kammula U. S.; Phan G. Q.; Lim R. M.; Wank S. A.; Restifo N. P.; Robbins P. F.; Laurencot C. M.; Rosenberg S. A. (2011) T cells targeting carcinoembryonic antigen can mediate regression of metastatic colorectal cancer but induce severe transient colitis. Mol. Ther. 19, 620–626. 10.1038/mt.2010.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapoport A. P.; Stadtmauer E. A.; Binder-Scholl G. K.; Goloubeva O.; Vogl D. T.; Lacey S. F.; Badros A. Z.; Garfall A.; Weiss B.; Finklestein J.; Kulikovskaya I.; Sinha S. K.; Kronsberg S.; Gupta M.; Bond S.; Melchiori L.; Brewer J. E.; Bennett A. D.; Gerry A. B.; Pumphrey N. J.; Williams D.; Tayton-Martin H. K.; Ribeiro L.; Holdich T.; Yanovich S.; Hardy N.; Yared J.; Kerr N.; Philip S.; Westphal S.; Siegel D. L.; Levine B. L.; Jakobsen B. K.; Kalos M.; June C. H. (2015) NY-ESO-1-specific TCR-engineered T cells mediate sustained antigen-specific antitumor effects in myeloma. Nat. Med. 21, 914–921. 10.1038/nm.3910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Till B. G.; Jensen M. C.; Wang J.; Chen E. Y.; Wood B. L.; Greisman H. A.; Qian X.; James S. E.; Raubitschek A.; Forman S. J.; Gopal A. K.; Pagel J. M.; Lindgren C. G.; Greenberg P. D.; Riddell S. R.; Press O. W. (2008) Adoptive immunotherapy for indolent non-Hodgkin lymphoma and mantle cell lymphoma using genetically modified autologous CD20-specific T cells. Blood 112, 2261–2271. 10.1182/blood-2007-12-128843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turtle C. J.; Hanafi L. A.; Berger C.; Gooley T. A.; Cherian S.; Hudecek M.; Sommermeyer D.; Melville K.; Pender B.; Budiarto T. M.; Robinson E.; Steevens N. N.; Chaney C.; Soma L.; Chen X.; Yeung C.; Wood B.; Li D.; Cao J.; Heimfeld S.; Jensen M. C.; Riddell S. R.; Maloney D. G. (2016) CD19 CAR-T cells of defined CD4+:CD8+ composition in adult B cell ALL patients. J. Clin. Invest. 126, 2123–2138. 10.1172/JCI85309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonifant C. L.; Jackson H. J.; Brentjens R. J.; Curran K. J. (2016) Toxicity and management in CAR T-cell therapy. Mol. Ther Oncolytics 3, 16011. 10.1038/mto.2016.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brudno J. N.; Kochenderfer J. N. (2016) Toxicities of chimeric antigen receptor T cells: recognition and management. Blood 127, 3321–3330. 10.1182/blood-2016-04-703751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maude S. L.; Barrett D.; Teachey D. T.; Grupp S. A. (2014) Managing cytokine release syndrome associated with novel T cell-engaging therapies. Cancer J. 20, 119–122. 10.1097/PPO.0000000000000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suntharalingam G.; Perry M. R.; Ward S.; Brett S. J.; Castello-Cortes A.; Brunner M. D.; Panoskaltsis N. (2006) Cytokine storm in a phase 1 trial of the anti-CD28 monoclonal antibody TGN1412. N. Engl. J. Med. 355, 1018–1028. 10.1056/NEJMoa063842. [DOI] [PubMed] [Google Scholar]
- Tey S. K. (2014) Adoptive T-cell therapy: adverse events and safety switches. Clin. Transl. Immunol. 3, e17. 10.1038/cti.2014.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X. J.; Tang Y. M. (2014) Cytokine release syndrome in cancer immunotherapy with chimeric antigen receptor engineered T cells. Cancer Lett. 343, 172–178. 10.1016/j.canlet.2013.10.004. [DOI] [PubMed] [Google Scholar]
- Brentjens R.; Yeh R.; Bernal Y.; Riviere I.; Sadelain M. (2010) Treatment of chronic lymphocytic leukemia with genetically targeted autologous T cells: case report of an unforeseen adverse event in a phase I clinical trial. Mol. Ther. 18, 666–668. 10.1038/mt.2010.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hay K. A.; Hanafi L. A.; Li D.; Gust J.; Liles W. C.; Wurfel M. M.; Lopez J. A.; Chen J.; Chung D.; Harju-Baker S.; Cherian S.; Chen X.; Riddell S. R.; Maloney D. G.; Turtle C. J. (2017) Kinetics and Biomarkers of Severe Cytokine Release Syndrome after CD19 Chimeric Antigen Receptor-modified T Cell Therapy. Blood 130, 2295. 10.1182/blood-2017-06-793141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan R. A.; Yang J. C.; Kitano M.; Dudley M. E.; Laurencot C. M.; Rosenberg S. A. (2010) Case report of a serious adverse event following the administration of T cells transduced with a chimeric antigen receptor recognizing ERBB2. Mol. Ther. 18, 843–851. 10.1038/mt.2010.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Berg J. H.; Gomez-Eerland R.; van de Wiel B.; Hulshoff L.; van den Broek D.; Bins A.; Tan H. L.; Harper J. V.; Hassan N. J.; Jakobsen B. K.; Jorritsma A.; Blank C. U.; Schumacher T. N.; Haanen J. B. (2015) Case Report of a Fatal Serious Adverse Event Upon Administration of T Cells Transduced With a MART-1-specific T-cell Receptor. Mol. Ther. 23, 1541–1550. 10.1038/mt.2015.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cartellieri M.; Feldmann A.; Koristka S.; Arndt C.; Loff S.; Ehninger A.; von Bonin M.; Bejestani E. P.; Ehninger G.; Bachmann M. P. (2016) Switching CAR T cells on and off: a novel modular platform for retargeting of T cells to AML blasts. Blood Cancer J. 6, e458. 10.1038/bcj.2016.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Stasi A.; Tey S. K.; Dotti G.; Fujita Y.; Kennedy-Nasser A.; Martinez C.; Straathof K.; Liu E.; Durett A. G.; Grilley B.; Liu H.; Cruz C. R.; Savoldo B.; Gee A. P.; Schindler J.; Krance R. A.; Heslop H. E.; Spencer D. M.; Rooney C. M.; Brenner M. K. (2011) Inducible apoptosis as a safety switch for adoptive cell therapy. N. Engl. J. Med. 365, 1673–1683. 10.1056/NEJMoa1106152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fedorov V. D.; Themeli M.; Sadelain M. (2013) PD-1- and CTLA-4-based inhibitory chimeric antigen receptors (iCARs) divert off-target immunotherapy responses. Sci. Transl. Med. 5, 215ra172. 10.1126/scitranslmed.3006597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juillerat A.; Marechal A.; Filhol J. M.; Valton J.; Duclert A.; Poirot L.; Duchateau P. (2016) Design of chimeric antigen receptors with integrated controllable transient functions. Sci. Rep. 6, 18950. 10.1038/srep18950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers D. T.; Mazagova M.; Hampton E. N.; Cao Y.; Ramadoss N. S.; Hardy I. R.; Schulman A.; Du J.; Wang F.; Singer O.; Ma J.; Nunez V.; Shen J.; Woods A. K.; Wright T. M.; Schultz P. G.; Kim C. H.; Young T. S. (2016) Switch-mediated activation and retargeting of CAR-T cells for B-cell malignancies. Proc. Natl. Acad. Sci. U. S. A. 113, E459–468. 10.1073/pnas.1524155113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei P.; Wong W. W.; Park J. S.; Corcoran E. E.; Peisajovich S. G.; Onuffer J. J.; Weiss A.; Lim W. A. (2012) Bacterial virulence proteins as tools to rewire kinase pathways in yeast and immune cells. Nature 488, 384–388. 10.1038/nature11259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu C. Y.; Roybal K. T.; Puchner E. M.; Onuffer J.; Lim W. A. (2015) Remote control of therapeutic T cells through a small molecule-gated chimeric receptor. Science 350, aab4077. 10.1126/science.aab4077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos C. A.; Asgari Z.; Liu E.; Yvon E.; Heslop H. E.; Rooney C. M.; Brenner M. K.; Dotti G. (2010) An inducible caspase 9 suicide gene to improve the safety of mesenchymal stromal cell therapies. Stem Cells 28, 1107–1115. 10.1002/stem.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee D. W.; Gardner R.; Porter D. L.; Louis C. U.; Ahmed N.; Jensen M.; Grupp S. A.; Mackall C. L. (2014) Current concepts in the diagnosis and management of cytokine release syndrome. Blood 124, 188–195. 10.1182/blood-2014-05-552729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Au-Yeung B. B.; Deindl S.; Hsu L. Y.; Palacios E. H.; Levin S. E.; Kuriyan J.; Weiss A. (2009) The structure, regulation, and function of ZAP-70. Immunol. Rev. 228, 41–57. 10.1111/j.1600-065X.2008.00753.x. [DOI] [PubMed] [Google Scholar]
- Au-Yeung B. B.; Levin S. E.; Zhang C.; Hsu L. Y.; Cheng D. A.; Killeen N.; Shokat K. M.; Weiss A. (2010) A genetically selective inhibitor demonstrates a function for the kinase Zap70 in regulatory T cells independent of its catalytic activity. Nat. Immunol. 11, 1085–1092. 10.1038/ni.1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan A. C.; Irving B. A.; Fraser J. D.; Weiss A. (1991) The zeta chain is associated with a tyrosine kinase and upon T-cell antigen receptor stimulation associates with ZAP-70, a 70-kDa tyrosine phosphoprotein. Proc. Natl. Acad. Sci. U. S. A. 88, 9166–9170. 10.1073/pnas.88.20.9166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan A. C.; Iwashima M.; Turck C. W.; Weiss A. (1992) ZAP-70: a 70 kd protein-tyrosine kinase that associates with the TCR zeta chain. Cell 71, 649–662. 10.1016/0092-8674(92)90598-7. [DOI] [PubMed] [Google Scholar]
- Palacios E. H.; Weiss A. (2007) Distinct roles for Syk and ZAP-70 during early thymocyte development. J. Exp. Med. 204, 1703–1715. 10.1084/jem.20070405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bubeck Wardenburg J.; Fu C.; Jackman J. K.; Flotow H.; Wilkinson S. E.; Williams D. H.; Johnson R.; Kong G.; Chan A. C.; Findell P. R. (1996) Phosphorylation of SLP-76 by the ZAP-70 protein-tyrosine kinase is required for T-cell receptor function. J. Biol. Chem. 271, 19641–19644. 10.1074/jbc.271.33.19641. [DOI] [PubMed] [Google Scholar]
- Horejsi V.; Zhang W.; Schraven B. (2004) Transmembrane adaptor proteins: organizers of immunoreceptor signalling. Nat. Rev. Immunol. 4, 603–616. 10.1038/nri1414. [DOI] [PubMed] [Google Scholar]
- Koretzky G. A.; Abtahian F.; Silverman M. A. (2006) SLP76 and SLP65: complex regulation of signalling in lymphocytes and beyond. Nat. Rev. Immunol. 6, 67–78. 10.1038/nri1750. [DOI] [PubMed] [Google Scholar]
- Wang H.; Kadlecek T. A.; Au-Yeung B. B.; Goodfellow H. E.; Hsu L. Y.; Freedman T. S.; Weiss A. (2010) ZAP-70: an essential kinase in T-cell signaling. Cold Spring Harbor Perspect. Biol. 2, a002279. 10.1101/cshperspect.a002279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W.; Sloan-Lancaster J.; Kitchen J.; Trible R. P.; Samelson L. E. (1998) LAT: the ZAP-70 tyrosine kinase substrate that links T cell receptor to cellular activation. Cell 92, 83–92. 10.1016/S0092-8674(00)80901-0. [DOI] [PubMed] [Google Scholar]
- Chan A. C.; Kadlecek T. A.; Elder M. E.; Filipovich A. H.; Kuo W. L.; Iwashima M.; Parslow T. G.; Weiss A. (1994) ZAP-70 deficiency in an autosomal recessive form of severe combined immunodeficiency. Science 264, 1599–1601. 10.1126/science.8202713. [DOI] [PubMed] [Google Scholar]
- Elder M. E. (1998) ZAP-70 and defects of T-cell receptor signaling. Semin. Hematol. 35, 310–320. [PubMed] [Google Scholar]
- Elder M. E.; Lin D.; Clever J.; Chan A. C.; Hope T. J.; Weiss A.; Parslow T. G. (1994) Human severe combined immunodeficiency due to a defect in ZAP-70, a T cell tyrosine kinase. Science 264, 1596–1599. 10.1126/science.8202712. [DOI] [PubMed] [Google Scholar]
- Williams B. L.; Schreiber K. L.; Zhang W.; Wange R. L.; Samelson L. E.; Leibson P. J.; Abraham R. T. (1998) Genetic evidence for differential coupling of Syk family kinases to the T-cell receptor: reconstitution studies in a ZAP-70-deficient Jurkat T-cell line. Mol. Cell. Biol. 18, 1388–1399. 10.1128/MCB.18.3.1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin S. E.; Zhang C.; Kadlecek T. A.; Shokat K. M.; Weiss A. (2008) Inhibition of ZAP-70 kinase activity via an analog-sensitive allele blocks T cell receptor and CD28 superagonist signaling. J. Biol. Chem. 283, 15419–15430. 10.1074/jbc.M709000200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X.; Adams A.; Wildt K. F.; Aronow B.; Feigenbaum L.; Bosselut R. (2003) Restricting Zap70 expression to CD4+CD8+ thymocytes reveals a T cell receptor-dependent proofreading mechanism controlling the completion of positive selection. J. Exp. Med. 197, 363–373. 10.1084/jem.20021698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saini M.; Sinclair C.; Marshall D.; Tolaini M.; Sakaguchi S.; Seddon B. (2010) Regulation of Zap70 expression during thymocyte development enables temporal separation of CD4 and CD8 repertoire selection at different signaling thresholds. Sci. Signaling 3, ra23. 10.1126/scisignal.2000702. [DOI] [PubMed] [Google Scholar]
- Feske S. (2007) Calcium signalling in lymphocyte activation and disease. Nat. Rev. Immunol. 7, 690–702. 10.1038/nri2152. [DOI] [PubMed] [Google Scholar]
- Joseph N.; Reicher B.; Barda-Saad M. (2014) The calcium feedback loop and T cell activation: how cytoskeleton networks control intracellular calcium flux. Biochim. Biophys. Acta, Biomembr. 1838, 557–568. 10.1016/j.bbamem.2013.07.009. [DOI] [PubMed] [Google Scholar]
- Lewis R. S. (2001) Calcium signaling mechanisms in T lymphocytes. Annu. Rev. Immunol. 19, 497–521. 10.1146/annurev.immunol.19.1.497. [DOI] [PubMed] [Google Scholar]
- Shan X.; Balakir R.; Criado G.; Wood J. S.; Seminario M. C.; Madrenas J.; Wange R. L. (2001) Zap-70-independent Ca(2+) mobilization and Erk activation in Jurkat T cells in response to T-cell antigen receptor ligation. Mol. Cell. Biol. 21, 7137–7149. 10.1128/MCB.21.21.7137-7149.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyazaki Y.; Imoto H.; Chen L. C.; Wandless T. J. (2012) Destabilizing domains derived from the human estrogen receptor. J. Am. Chem. Soc. 134, 3942–3945. 10.1021/ja209933r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banaszynski L. A.; Chen L. C.; Maynard-Smith L. A.; Ooi A. G.; Wandless T. J. (2006) A rapid, reversible, and tunable method to regulate protein function in living cells using synthetic small molecules. Cell 126, 995–1004. 10.1016/j.cell.2006.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwamoto M.; Bjorklund T.; Lundberg C.; Kirik D.; Wandless T. J. (2010) A general chemical method to regulate protein stability in the mammalian central nervous system. Chem. Biol. 17, 981–988. 10.1016/j.chembiol.2010.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo K.; Sefton B. M. (1992) Activated lck tyrosine protein kinase stimulates antigen-independent interleukin-2 production in T cells. Mol. Cell. Biol. 12, 4724–4732. 10.1128/MCB.12.10.4724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zufferey R.; Dull T.; Mandel R. J.; Bukovsky A.; Quiroz D.; Naldini L.; Trono D. (1998) Self-inactivating lentivirus vector for safe and efficient in vivo gene delivery. J. Virol. 72, 9873–9880. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.