Abstract
Sonography of the male inguinal canal for hernia is a common request. There is debate about the accuracy and even need for sonographic assessment of inguinal hernia. A clear, concise method is presented, with correlated diagrams and sonographic images, which aims to improve the ability of sonographers to easily identify inguinal herniae.
Keywords: Abdomen, herniation, musculo‐skeletal, technique, ultrasound
Introduction
Inguinal herniae in the male are a common complaint,1, 2, 3, 4, 5, 6, 7 and yet sonographic examination of this pathology can be challenging for general sonographers.8, 9, 10 If a hernia is not detected when present, then the patient may not be offered curative surgery, or they may have to undergo further tests. Therefore, it is important for sonographers to use a technique that maximises the diagnostic accuracy of this examination.
The reasons for the challenging nature of this examination for many sonographers are most likely twofold:
there is scant literature on sonographic technique for the evaluation of the inguinal hernia, with many articles focussing on the anatomy, physiology and embryology, and
the current, various techniques, when mentioned, may be inadequately explained and can be technically difficult.
Ultrasound is often considered to be ‘operator‐dependent’.8, 11, 12, 13, 14 This may often be the case as a result of variability in the operator's knowledge, skills and experience. Operator dependency can be limited by good training, and employing rigorous scanning protocols.
This paper provides a clear methodology on how to successfully scan the inguinal canal in the male, and assist uniform accuracy in hernia detection.
Anatomy and Pathology
The inguinal canal in the male begins at the deep ring at its junction with the peritoneal cavity. From there it courses slightly infero‐medially to exit at the superficial ring just supero‐laterally to the symphysis pubis (Fig. 1). It is generally considered to be approximately 4 cm in length.15, 16, 17, 18
Figure 1.
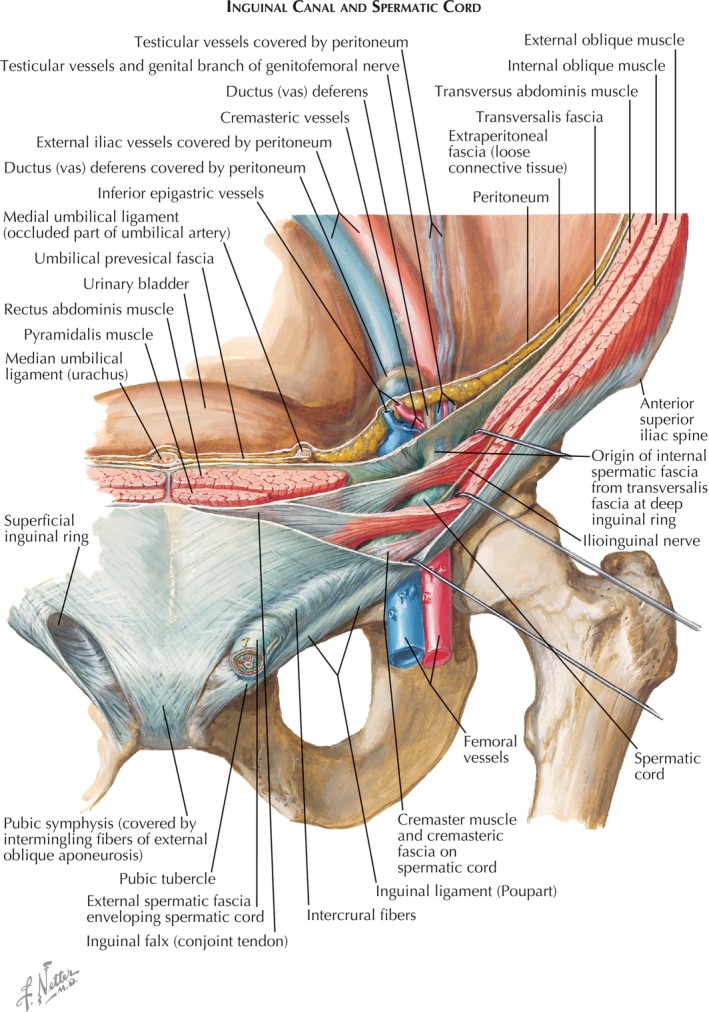
Inguinal Canal – Netters Atlas of Human Anatomy (license to reproduce was obtained).17
The inguinal canal exists as a remnant pathway of the passage of the testis into the scrotum, and normally contains only the spermatic cord, and the genital branch of the genitofemoral nerve.19
There are two types of inguinal hernia:
The terminology of these herniae are somewhat misleading, because they are termed opposite to the method of hernia their name suggests.
An indirect inguinal hernia occurs when the peritoneal sac, and its content, pushes directly down into the inguinal canal through the now expanded opening of the deep ring.
A direct inguinal hernia occurs when the peritoneal sac, and its content, pushes indirectly down into the inguinal canal through a weakening or hole in the pelvic floor, which would otherwise normally not be there.15, 16, 17
Preparation:
Equipment recommendations
High‐resolution transducer (minimum 7–12 MHz)
Modern, high‐end ultrasound machine
Cine‐loop capability
Patient preparation
No fasting needed
Informed consent required
Clear access to groin required – all clothing should be removed from the waist down, and a hand towel applied to cover the genitalia centrally, allowing clear access to the groin crease and lower pelvis
-
Explain method of straining (to induce hernia response) – it is recommended that patients are asked to
-
○
push their stomach out hard/valsalva
-
○
make themselves fat
-
○
strain down
-
○
place their hands behind their head, and raise their head and chest off the bed (partial sit‐up).
-
○
Asking patients to cough certainly increases the intra‐abdominal pressure, however makes a hernia hard to see/track.
Technique
Historical
Most methods for identification of the inguinal canal suggest searching in the lower lateral quadrant for the external iliac vessels, then using a transverse transducer approach, identify the inferior epigastric artery and vein.12, 13, 14, 15, 16 Crossing over these vessels, near their origin with the external iliac vessels, the deep ring is said to be identified. Maintaining this transverse approach the patient is asked to strain and movement of material from deep to superficial is said to constitute a hernia.15, 17, 20 As an example Ryan16 similarly suggests ‘Scan the femoral vessels transversely, and find the level of the epigastric vessels. The inguinal canal lies anterior and medial to these vessels.’
This technique, used by many sonographers, can be problematic, viz:
it can be difficult to identify the origin of the inferior epigastric vessels, and thus the deep ring;
this method does not allow interrogation of the hernia into and along the length of the canal
mistakes are made confusing direct inguinal herniae and Spigelian herniae with indirect inguinal herniae
normal movement of the spermatic cord could be mistaken for an indirect hernia
Suggested method
The following method is suggested, which involves finding the spermatic cord at the pubis, and tracing it superiorly to the deep ring. This is effectively the reverse of the conventional, most commonly used technique. In our opinion following over 15 years of experience in performing and teaching this method, it is simpler, easier to perform and enables accurate evaluation of the entire length of the inguinal canal consistently.
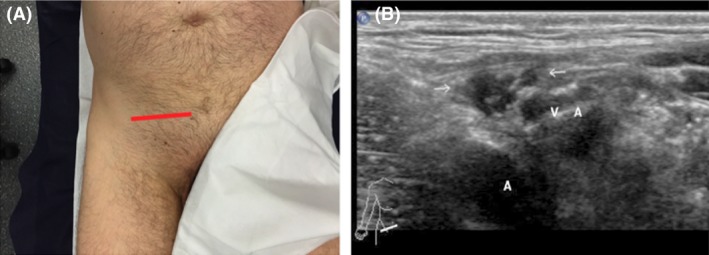
The sonographer should commence with the transducer in transverse orientation just lateral to the symphysis pubis (Fig. 2A), and identify the spermatic cord. The cord is easily visible in the transverse plane at this level as a series of hypo‐echoic rounded fascicles representing the blood vessels in cross‐section (Fig. 2B). As the cord runs superficially over the superior ramus of the pelvic bone, a shallow depth of field of around 3–4 cm is typically all that is required.
Figure 2.

(A) Transducer position transverse superficial ring (B) Associated image with arrows showing spermatic cord complex. Patient permission was obtained to publish the photograph.
If the femoral vessels can be identified then the transducer is too lateral and should be moved medially.
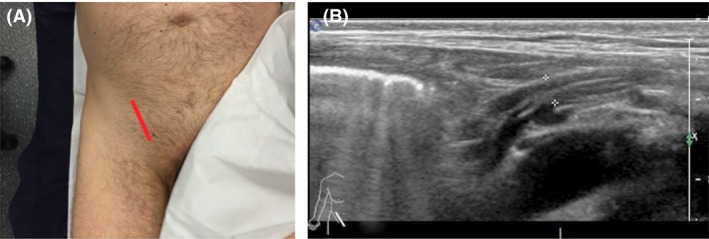
Once the cord is identified trace it supero‐laterally in the transverse plane as it travels proximally toward the deep ring (Fig. 3A). Typically it has a fairly straight path with no curve to it. At the deep ring (Fig. 3B) the cord will ‘disappear’ down into the peritoneal cavity, and typically it is lost to view. The canal should be repeatedly panned in the transverse plane from superficial to deep ring, and back again. Straining is not required at this stage. With increasing practice and experience the sonographer will correctly identify any ‘extra material’ in the canal.
Figure 3.
(A) Transducer position transverse deep ring (B) Associated image with arrows showing spermatic cord complex and vasculature at deep ring. Patient permission was obtained to publish the photograph.
Once the deep ring is again located the transducer is rotated through 90 degrees to obtain an elongated view of the deep ring and proximal inguinal canal (Fig. 4A and B). The spermatic cord should be easily identified arising superficially from within the peritoneal cavity to begin its journey through the deep ring, along the inguinal canal, and down into the scrotal sac.
Figure 4.
(A) Transducer position long deep ring (B) Associated image with calipers showing height of proximal inguinal canal at the deep ring. Patient permission was obtained to publish the photograph.
At the level of the deep ring in the longitudinal plane, the patient should be encouraged to strain while observing the presence or absence of any material entering the canal. Note that in many patients there is some considerable movement of the spermatic cord itself, which is normal. Material may enter and then leave the canal, or enter and remain within the canal. In the latter case transducer pressure is used to attempt to reduce the hernia.
Often an irreducible hernia is identified without need of straining techniques, which only serve to enhance the hernia size or document distal extension of the hernia sac. Panning with the transducer across the deep ring in the longitudinal plane will ensure herniae are not missed, as often herniae occur in the plane just laterally or medially to the deep ring.
If the deep ring is intact and normal, the task is now to examine the remainder of the canal in the longitudinal plane looking for a direct hernia entering the canal through the canal floor distal to the deep ring. The transducer is simply slid distally to the mid to distal canal (Fig. 5A and B), and with the application of patient straining observe for direct hernia. It is important when searching for a direct hernia to also pan laterally and medially just off the canal.
Figure 5.

(A) Transducer position long mid to distal canal (B) Associated image with calipers showing height of distal inguinal canal. Patient permission was obtained to publish the photograph.
Observation of a ‘step’ at the distal canal is the exiting of the spermatic cord at the superficial ring, just prior to it passing over the superior bony ramus. This ‘step’ is the anterior displacement of the spermatic cord as it exits the rigidity of the inguinal canal (Fig. 6). This ‘step’ is a normal finding. The cord then tracks antero‐medially over the bony ramus before descending into the scrotum.
Figure 6.
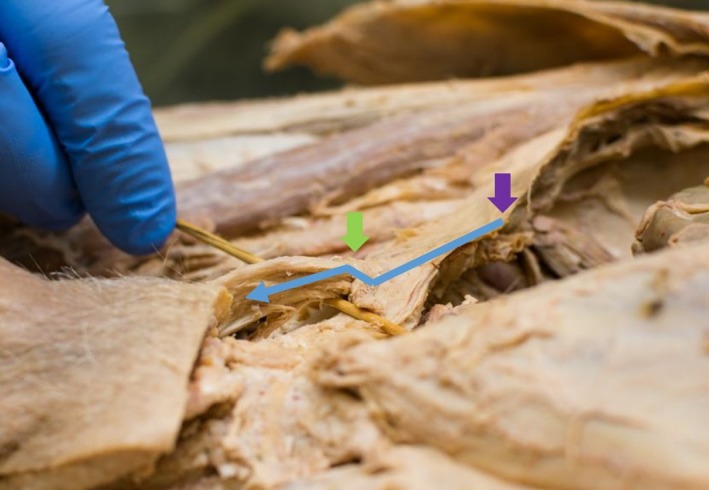
Cadaveric specimen showing ‘step’ (blue arrow) of spermatic cord complex exiting superficial ring (green arrow). Deep ring (purple arrow). Permission was obtained from the School of Medicine, Deakin University to publish this photo.
Image and report the findings. Include a cineloop of the hernia as proof of the reducibility, or lack thereof, and extent of the hernia. Recommended still images are longitudinal views of the deep ring pre‐ and post‐strain with antero‐posterior measurements of the proximal canal at the deep ring, along with a longitudinal view at strain of the mid to distal canal to include/exclude direct herniae.
Conclusion
A sound sonographic technique for the evaluation of inguinal herniae in the male is imperative for the diagnostic accuracy of the examination.13, 16
This suggested method is an easy to follow, simple technique for evaluation of the inguinal canal to assess for herniae.
With repeated practice to master this technique, it should provide a reliable, repeatable examination for evaluation of the male inguinal canal, with sonographers eventually becoming familiar with the variations, and variants, encountered during this examination.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgements
Nil. No financial grants were received to produce this manuscript.
J Med Radiat Sci 65 (2018) 163–168
References
- 1. Depasquale R, Landes C, Doyle G. Audit of ultrasound and decision to operate in groin pain of unknown aetiology with ultrasound technique explained. Clin Radiol 2009; 64: 608–14. [DOI] [PubMed] [Google Scholar]
- 2. Garvey JF, Hazard H. Sports hernia or groin disruption injury? Chronic athletic groin pain: A retrospective study of 100 patients with long‐term follow‐up. Hernia 2014; 18: 815–23. [DOI] [PubMed] [Google Scholar]
- 3. O'Rourke MGE, O'Rourke TR. Inguinal hernia: Aetiology, diagnosis, post‐repair pain and compensation. ANZ J Surg 2012; 82: 201–6. [DOI] [PubMed] [Google Scholar]
- 4. Pawlak M, Niebuhr H, Bury K. Dynamic inguinal ultrasound: A diagnostic tool for hernia surgeons. Hernia (Letter to the editor) 2015; 19: 1033–4. [DOI] [PubMed] [Google Scholar]
- 5. Saclarides TJ, Myers JA, Millikan KW (eds). Common Surgical Diseases, 3rd edn Springer‐Verlag, New York, 2015; pp. 229–31. [Google Scholar]
- 6. Robinson A, Light D, Kasim A, Nice C. A systematic review and meta‐analysis of the role of radiology in the diagnosis of occult inguinal hernia. Surg Endosc 2013; 27: 11–8. [DOI] [PubMed] [Google Scholar]
- 7. Robinson A, Light D, Nice C. Meta‐analysis of sonography in the diagnosis of inguinal hernias. J Ultrasound Med 2013; 32: 339–46. [DOI] [PubMed] [Google Scholar]
- 8. Alam A, Nice C, Uberoi R. The accuracy of ultrasound in the diagnosis of clinically occult groin hernias in adults. Eur Radiol 2005; 15: 2457–61. [DOI] [PubMed] [Google Scholar]
- 9. Brandi C. Dear colleague, please, do not ask for ultrasound studies for inguinal hernia diagnosis. Hernia (Letter to the editor) 2015; 19: 1031. [DOI] [PubMed] [Google Scholar]
- 10. Miller J, Cho J, Michael M, Saouaf R, Towfigh S. Role of imaging in the diagnosis of occult hernias. JAMA Surg 2014; 149: 1077–80. [DOI] [PubMed] [Google Scholar]
- 11. Alabraba E, Psarelli E, Meakin K, et al. The role of ultrasound in the management of patients with occult groin hernias. Int J Surg 2014; 12: 918–22. [DOI] [PubMed] [Google Scholar]
- 12. Brown AK, O'Connor PJ, Wakefield RJ, Roberts TE, Karim Z, Emery P. Practice, training, and assessment among experts performing musculoskeletal sonography: Toward the development of an international consensus of educational standards for ultrasonography for rheumatologists. Arthritis Rheum 2004; 51: 1018–22. [DOI] [PubMed] [Google Scholar]
- 13. Light D, Ratnasingham K, Banerjee A, Cadwallader R, Uzzaman MM, Gopinath B. The role of ultrasound scan in the diagnosis of occult inguinal hernias. Int J Surg 2011; 9: 169–72. [DOI] [PubMed] [Google Scholar]
- 14. Ohrndorf S, Naumann L, Grundey J, et al. Is musculoskeletal sonography an operator‐dependent method or a fast and reliably teachable diagnostic tool? Interreader agreements of three ultrasonographers with different training levels. Int J Rheumatol 2010;. https://doi.org/10.1155/2010/164518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jamadar DA, Jacobson JA, Morag Y, et al. Sonography of inguinal region hernias. AJR 2006; 187: 185–90. [DOI] [PubMed] [Google Scholar]
- 16. Ryan F. Groin hernias: Mechanical anatomy and ultrasound evaluation. Soundeffects 2003; 3: 24–8. [Google Scholar]
- 17. Netter F. Atlas of Human Anatomy, 6th edn Saunders, Philadelphia, 2014. [Google Scholar]
- 18. Moore KL, Dalley AF, Agur AM. Clinically Oriented Anatomy, 6th edn Wolters Kluwer, Baltimore, 2010. [Google Scholar]
- 19. Ryan F. Embryology and anatomy of inguinal canal. Soundeffects 2003; 2: 30–6. [Google Scholar]
- 20. Bradley M, Morgan D, Pentlow B, Roe A. The groin hernia –an ultrasound diagnosis? Ann R Coll Surg Engl 2003; 85: 178–80. [DOI] [PMC free article] [PubMed] [Google Scholar]


