Abstract
Background
Attempts to refine toothbrushing (TB) technique, an ingrained habit in adults, can meet with some challenges. Recently, the role of proactive interference as a barrier to improving the learning of proper brushing has been proposed. This pilot feasibility study was designed to investigate TB behavior and to see how it changes after training. Smartphone video “selfies” (SPVSs) are increasingly being used in the medical field to assess, monitor, and determine the progression of diseases.
Materials and Methods
We used SPVS to study TB skills in a small sample of volunteers. Over a period of 14 days, after a one-time group training session, we observed TB behavior of volunteers using self-captured SPVS.
Results
Following the brief intervention, we observed an 8% of improvement in TB skills.
Discussion
To the best of our knowledge, this is the first report using SPVS to study TB behavior. We demonstrated initial feasibility of using SPVS in the dental setting. We observed modest improvements in toothbrushing accuracy and quality, and we generated important experiences about the use of Selfies for TB monitoring and intervention, and some interesting insights about where in the toothbrushing is more or less effective.
Conclusion
Further investigation using a larger sample size is needed to thoroughly assess the effectiveness of this approach to improve TB skills and better understand the role of proactive interference.
Keywords: Behavior change, brushing techniques, selfies, toothbrushing, video
Oral health is an integral part of general well-being.[1] Proper maintenance of oral health may help to avert preventable oral diseases such as dental caries and periodontal diseases. Toothbrushing (TB) is the most widely used method of oral hygiene.[2] Proper TB can drastically reduce the risk for oral diseases although this depends on the effectiveness of the TB technique that is used.[3] At present, consensus has not yet been achieved on the optimal, psychological approach for encouraging proper TB; however, new concepts and models for health theory behavior-based interventions have begun to emerge.[4] The process and mechanisms of TB habit formation have been previously described, and to varying degrees, intervention approaches have been based on these foundations.[2] For example, it has been pointed out that both a neurocognitive approach and an effective psychological approach are needed for complete integration and regular practice of TB.[5] In a recent study examining the adoption of proper TB technique while being video-recorded through a mirror, a significant number of participants did not fully integrate proper TB into their regular routine in spite of having seemingly sufficient motivation, skill, and desire.[5] Recently, we described a coaching approach encouraging proper TB that was informed by the Information-Motivation-Behavioral Skills (IMB) model proposed by Fisher et al., 2009,[6] and other important health theories such as motivational interviewing (MI) by Miller and Rollnick, 2012,[7] and integrative health coaching as described by Simmons and Wolever, 2013.[8] IMB is a recent conceptual framework that helps promote individual level health-related behavior change. In the context of oral health, the IMB model theorizes that participants are more likely to undertake health-promoting behaviors when they are aware of relevant information regarding an existing or potential oral disease state, when they are sufficiently and personally motivated to take corrective action, and when they are fully aware of the precise behavioral skills that are required (as well as strategies to follow if there are barriers to completing the desired behaviors).[6,9] Further, integration of a behavior change approach informed by the IBM model, MI, and integrative health coaching, as described by Vernon and Howard, 2015, stresses the importance of promoting internal motivation and enhancing the participant’s self-efficacy to adopt and maintain proper oral hygiene self-care.[10] Ideally, the resultant change in behavior and motor skills will manifest as proper oral hygiene maintenance, that is, a newly formed TB habit. However, in spite of one’s best efforts, a significant percentage of patient’s may relapse back into their old and improper TB habits.[11,12] Recently, researchers have speculated that proactive interference (when learning a new behavior is impeded by interference of knowledge and habits tied to an old behavior) may have an important influence in reverting to improper, old TB habits.[12] Adopting a more effective TB technique can be challenging; this is especially true when TB has been practiced for a number of years without proper supervision, guidance, and reinforcement. On an individual level, for a proper TB skills to be adopted, there are a number of separate steps or components-for example, the process of memory formation, coding, retrieval, contextual cueing, association, “muscle memory”, addressing interferences besides sufficient motor skill, and one’s desire to change the old TB habit.[13] It is interesting to note however that, currently, there is no single, universally recommended, proper TB technique that has been shown to be successful in all situations; thus, only tailored approaches have been shown to be successful.[13] Smartphones have permeated almost all walks of human life in the 21st century and have been recently used for early diagnosis and prognosis of disorders such as Parkinson disease.[14] This trend, of using mobile technology, has been characterized as a new modality for scientific inquiry and is frequently referred to as mHealth.[15] With advancing mobile phone technology and innovations, experts in participatory medicine and patient-generated health data postulate that with easier interfaces, increasing smartphone use (by more people) and the availability of high-speed internet connectivity (of sufficient quality and with access to high percentage of the population) would allow patients to monitor themselves via photography, video, and other means, either on their own or in conjunction with the clinician.[16] In the dental setting, use of this technology could help shift the focus from treating a condition such as periodontal disease to preventing such oral conditions and promoting more optimal oral health.
The use of self-photography or “selfies” using smartphone-based technology is now widely popular. Further, the specific use of smartphone video “selfies” (SPVSs) is also growing in popularity; in the near future, this practice may provide a venue by which patients can receive timely health care.[17] On-site video recordings of TB have been shown to be an effective method to educate and motivate participants to refine, enhance, and maintain the refined TB habits.[18,19] Currently, to the best of our knowledge, using dental SPVS to promote proper TB behavior has not been previously described. In this pilot feasibility study, we explore the use SPVS to assess TB skill before and after a brief intervention and note any trends that may be consistent with proactive interference.
MATERIALS AND METHODS
This was a small prospective, interventional pilot feasibility study. After baseline measures had been collected (including the on-site, baseline SPVS), there was a brief intervention after which four more SPVSs (for a total of 5) were self-recorded in their own home by participants at 24 h and 48 h on the 7th day and 14th day. Our intention was to explore the extent to which participants would adopt an improved TB technique and to inform an intervention and research design for large-scale studies.
The study was composed of four volunteers who were dental residents completing their internship period (final 5th year of supervised clinical training prior to degree certification after successful completion of 4 years of dental course work). The study was approved by the Ragas Dental College and Hospital’s Institutional Review Board and written informed consent was obtained from all participants. Study participation was voluntary and there were no financial or other or incentives except that a mobile phone stand worth INR 100 (about US $1.50) was given to each participant. This mobile phone stand was intended to help standardize SPVS data collection and to keep the phone safe during the video-acquiring process. The study participants were chosen based on a brief, informal interview involving assessment of their willingness to cooperate with a study regarding their TB behavior. The inclusion criteria were high level of motivation (≥8 on the motivational scale of 0 to 10),[20] low oral hygiene index-simplified (OHI-S) score (<0.6),[21] and willingness to comply with the study protocol as well as owning or having access to a mobile smartphone with a reasonable field of vision and memory space, with a front camera of minimum 3 MP resolution. The exclusion criteria were those with poor motivation (≤7),[20] a subjective assessment by the interviewer as having of a potential for noncompliance to study protocol/procedures including poor ability to handle smartphone videography correctly, high OHI-S score (>0.6),[21] those under current orthodontic appliance therapy, the presence of overhanging fillings, and those who had periodontal interventions or had undergone oral hygiene instructions within the past 6 months. Further, persons with poor oral hygiene were also excluded from the study so that they could receive timely and proper oral health care.
The study protocol was as follows. At baseline and prior to the brief intervention, the OHI-S score was assessed as a combined score of the coronal extent of soft debris index-simplified (DI-S) and the calculus index-simplified (CI-S) was performed on 6 index teeth surfaces.[21] We collected scores of two submeasures (DI-S and CI-S) (which could range between 0 and 3, thus, an overall score of 0–6 was possible)[21] and the participant’s level of motivation to improve TB skills (assessed using a Likert scale of 0–10, with “0” indicating no motivation and 10 referring to the highest level of motivation). The participants were uniformly trained to demonstrate competence video recording themselves while brushing their teeth using their own cell phones to record an SPVS. During video-capture training, emphasis was on placed using front-facing camera view to correctly record the mouth with the hand, brush, and bristles in the field of view. Volunteers were asked to use their regular toothbrush and toothpaste. Training was provided to video shoot the “dental-selfie” (or SPVS) of brushing without divulging the entire face or eyes or any personally identifying marker. Therefore, the resultant SPVS recorded the process of TB while focusing on the mouth with maximum attention to the participant’s hand and TB angulations. Thus, participants were asked to record their regular and entire TB behavior prior to the brief TB intervention, which served as the baseline SPVS recording.
For this study, the widely recommended modified Bass technique[22] was used in the brief intervention training as the standard for “proper” TB technique. Each baseline SPVS, taken prior to the brief TB intervention, was reviewed by an experienced oral health-care giver (PDMK) and individually, the participant’s procedural errors were pointed out and the correct procedure was demonstrated. Next, individually, each participant was asked to repeat the TB procedure. Then, errors in the modified Bass technique were specifically pointed out and iterative corrections were made until volunteers were able to demonstrate the proper TB technique.
No further reminders, instructions, or feedbacks were given to the participants. All participants were asked by the research team not to deliver oral hygiene instructions to any of their patients during the 14-day study period. The participants were asked not to view any of their SPVSs after they were recorded. After recording an on-site, baseline SPVS of TB, participants recorded (at their own home) their brushing at the end of 24 h, 48 h, day 7, and day 14. For each participant, 5 (1 baseline and 4 subsequent recordings) SPVSs were analyzed. At the end of the day 14, participants’ level of motivation and OHI-S scores were collected again as previously described (given above). The participant’s brushing method was not checked or reviewed during the study period. At the end of the study, on-site authors (PDMK, TR) reviewed each video separately. TB skills were assessed for quality and accuracy as described below. Prior to the start of the study, the authors had agreed upon the assessment criteria (given below). Accordingly, data were collected from each SPVS. Authors (PDMK, TR) performed their assessment separately; any discordance between raters triggered a review of the video by both raters and was discussed until consensus was reached. The mean score of both raters was taken as the final value. We present separate assessments of changes across time in TB quality and accuracy informed by earlier works of Poche et al., 1982, and Rachel, 2012.[23,24] Finally, for each video, the length of time spent on TB was measured and recorded in seconds.
Assessment of toothbrushing quality
We assessed six sextants of teeth (three per maxillary and mandibular arch) consisting of right posterior teeth [premolars and molars–universal tooth number 1–5; 28–32], anterior teeth [incisors and canines–universal tooth number 6–11, 22–27], left posterior teeth [premolars and molars, tooth 12–16; 17–21] each with the buccal and lingual sides considered separately, for a total of 12 sections of teeth. The total of each complete TB stroke (to and fro motion) in each of the 12 sections was counted and recorded. If the participant performed the majority of strokes in a correct, prescribed rhythmic manner, they were given a score of “1” in each section. If not, a score of “0” was given in each section. Similarly, the maintenance of the proper 45° angle of the toothbrush bristles to the surface of the teeth at the cervical margin of teeth at the start of the stroke-if done correctly, a score of “1” was given in each of the 12 sections, whereas incorrect angulation was given a score of “0” in each of 12 sections. If there was uncertainty with a given rating, the video was paused and re-reviewed. Single screenshots were obtained and saved as a JPEG image and were then checked by drawing a line to calculate the exact angle between toothbrush bristle and surface of teeth as captured on serial digital images using Microsoft paint program (Microsoft Windows 7.0 office Edition, 2012) (digital assessments were performed by TR). A final decision was arrived upon by consensus of the two raters. Similarly, the correct brush handling position-i.e., hand position, wrist position, and delivery of the brushing movement-if it was as per the recommended technique, a score of “1” was given and if not, a score of “0” was given-again, in each of 12 sections. Hence, in all 12 sections of teeth, each of three parameters (correct stroke/TB angulation/positioning of brush) totaled a maximum score of 36 (i.e., 12 × 3 = 36) points. The cumulative score converted to an overall average score by dividing by 12 (i.e. 6 sextants involving two surfaces-buccal and lingual = 12) to yield an overall score that could range from 0 to 3. Hence, the score “3” implies that the participant has performed the brushing correctly as per the criteria in all sextants and surfaces in terms of the three parameters (correct stroke/ angulations/positioning of brush) while a score of “0” implies that participant has not correctly brushed in all sextants and surfaces as per the three parameters.
Assessment of toothbrushing accuracy
In this assessment, the total number of strokes in each of 12 sections of teeth was counted. The numbers of correct application strokes, the number of times the toothbrush bristles that were held in the prescribed 45° angulation against the tooth and correct positioning of the arm (parallel to the floor) were also counted. These values were expressed as percent of the number of correct strokes for that section of teeth using the below formula:
The overall accuracy of TB skills for the particular section of teeth was the mean of the percent of correct strokes, percent of correct angulations of the brush, and percent of correct brush positions. The overall accuracy of the participant was; the mean of the 12 sections.
In this calculation, if, in a sections of teeth (per sextant within the buccal and lingual surfaces), only one stroke is performed and is as per our training recommendations, then the value would be computed as 100% correct; thus, a potential limitation of this method is that can introduce an artificial bias into the results. In anticipation of this limitation and to mitigate it, the assessment measures of TB quality and total length of time spent on TB were also incorporated into the study. Hence, the results are best interpreted by considering both the assessment of TB quality and TB accuracy rather than either measure in isolation.
Analytical approach
All the data were entered and analyzed in Statistical Package for Social Services (SPSS, IBM, IL, USA), version 20.0 or R Statistical Software, version 3.2.4 (Open source software, www.r-project.org, The R Foundation). Descriptive statistics are presented and discussed. A one-way ANOVA for ranks (nonparametric Kruskal–Wallis test) was employed to assess the difference between the above-described outcome parameters during the study intervals employing a P ≤ 0.05 for evaluation of significant difference.
RESULTS
Patient characteristics
A total of six volunteers were interviewed, of which four volunteers (dental student interns) entered and completed the study. Each of four volunteers completed all five SPVSs; a total of twenty SPVSs were included in the analyses. Participants’ mean age was 21.25 ± 0.5 years. There were three males and one female in this pilot, feasibility study. The mean OHI-S was calculated as 0.475 ± 0.15. The CI-S was “0” in all the dental interns and accumulated dental plaque/debris contributed to the score. At the end of the study, the mean OHI-S was 0.425 ± 0.2. At baseline, the self-declared mean motivational score was 8.5 ± 0.58 while at the end of the study, it was 9 ± 0.57.
The investigator’s descriptive summary of the training phase
All participants were right-handed and used the right hand for brushing. At baseline (prior to training), several surfaces within sextants within were not being brushed - notably the lingual surface of maxillary and mandibular anterior segment and the palatal aspect of the right maxillary posterior segment. After our brief training, this lack of attention was rectified at all study time points even at the 24 h period. However, the number and direction of brushing strokes (as recommended by the modified Bass technique for that particular sextant), the angulation at which the brush should be held against the tooth surface (as recommended when using the modified Bass technique), and brush position were not in compliance with the prescribe technique and were not adequate to be rated as a full score. This lack of adopting the prescribed technique persisted till the end of the study. Again, after the intervention, all four participants had TB strokes that covered all their tooth surfaces. However, much of the variability in TB was limited to buccal/facial surfaces as compared to the lingual/palatal surfaces and more coverage was given to cervical areas of the posterior tooth. Hence, remnants of “hot spots”[19] (i.e., areas where TB was not adequately performed) persisted. Further, in spite of requesting that participants should brush for a full 2 min, the length of time spent on TB at baseline appeared to persist relatively unchanged from baseline to the end of the study (mean time at baseline was 70 ± 19.4 s and at the end of the 14th day was 54.3 ± 11.6 s). Thus, even after our brief intervention, participants still continued brushing their teeth the same (habitual) length of time during the study.
Toothbrushing quality and accuracy results
The quality and accuracy scores regarding the effectiveness of TB over the time period of the study are depicted in Tables 1–3 and Figure 1. Evaluation of mean differences over longitudinal time points of the outcome scores yielded no statistically significant differences despite the appearance of episodic decreases and increases. Note that the baseline TB accuracy was 46.5 ± 26.7%, which at the end of the 14-day trial period marginally increased to 50.3 ± 25.9% (P is Not Significant). This delta (change over time) of + 3.8 in effectiveness should be interpreted with caution due to the low sample size and high standard deviation. Interestingly, an increase of 8.06% in the accuracy of TB quality (3.8/46.5 × 100) from baseline is observed although this is likely due to a disproportionate contribution of one participant, as can often happen often in small samples, and hence the need for a larger trial. The time spent on TB (duration measured in seconds) at different time points across the study is shown in Table 3.
Table 1.
Summary of the toothbrushing quality of four participants across five time points
| Toothbrushing quality (%)
|
|||||
|---|---|---|---|---|---|
| Baseline | 24 h | 48 h | 7 days | 14 days | |
| Participant-1 | 83.3 | 63.9 | 88.9 | 75 | 100 |
| Participant-2 | 83.3 | 66.7 | 63.9 | 77.8 | 77.8 |
| Participant-3 | 69.4 | 72.2 | 83.3 | 77.8 | 80.6 |
| Participant-4 | 50 | 58.3 | 58.3 | 50 | 55.6 |
Table 3.
Analysis of outcome parameters with Kruskal- Wallis nonparametric test
| Time point | Mean±SD | P | |
|---|---|---|---|
| Quality score (maximum 3) | Baseline | 2.2±1.2 | 0.35 |
| 24 h | 2±1.0 | ||
| 48 h | 2.2±0.9 | ||
| 7 days | 2.1±1.0 | ||
| 14 days | 2.4±0.9 | ||
| Percent of correct strokes | Baseline | 63.2±40.3 | 0.86 |
| 24 h | 56.8±40.1 | ||
| 48 h | 66.1±38.3 | ||
| 7 days | 61.8±41.8 | ||
| 14 days | 62.7±40.1 | ||
| Percent of correct angulations of toothbrush | Baseline | 38.2±26.4 | 0.69 |
| 24 h | 42±32.2 | ||
| 48 h | 47.2±27.6 | ||
| 7 days | 44±28.9 | ||
| 14 days | 41.6±29.0 | ||
| Percent of correct brush positions | Baseline | 38.2±33.0 | 0.72 |
| 24 h | 43.8±37.2 | ||
| 48 h | 48.8±35.2 | ||
| 7 days | 45.2±34.4 | ||
| 14 days | 46.5±36.7 | ||
| Overall accuracy (%) | Baseline | 46.5±26.7 | 0.64 |
| 24 h | 47.5±30.0 | ||
| 48 h | 54.0±25.3 | ||
| 7 days | 50.3±27.6 | ||
| 14 days | 50.3±25.9 | ||
| Time (s) | Baseline | 70±19.4 | 0.80 |
| 24 h | 63±8.4 | ||
| 48 h | 58.8±11.1 | ||
| 7 days | 61.5±14.6 | ||
| 14 days | 54.3±11.6 |
SD=Standard deviation. P=Not significant
Figure 1.

(a) Change in toothbrushing quality of four participants across five time points (b) Change in toothbrushing accuracy of four participants across five time points
Exploratory analyses
It was observed that there was an increase in the number of strokes performed till the 7th day and then this value began to decrease. Table 4 depicts the changes in the mean ± standard deviation, median, number of strokes for each of the surfaces in all sextants in the study. However, the difference between the number of strokes over longitudinal time points was statistically significant neither under the Kruskal–Wallis test (df = 4.0, P = 0.79) nor the Friedman χ2 = 75.8 df = 59, P = 0.07 (the tests satisfy different assumptions for small repeated measures data). Although we did not measure stroke length, it was qualitatively observed that the strokes were relatively shorter and the speed of strokes was increased.
Table 4.
Number of toothbrushing strokes by four participants at five time points in 12 sections of teeth
| Sections and surface | Baseline | 24 h | 48 h | 7 days | 14 days |
|---|---|---|---|---|---|
| Right maxillary posterior - buccal | |||||
| Mean±SD | 10.5±7.9 | 12.0±11.2 | 9.0±6.4 | 14.8±13.9 | 9.8±9.9 |
| Median | 9.5 | 10.0 | 7.0 | 13.5 | 6.0 |
| Minimum, maximum | 3, 20 | 2, 26 | 4, 18 | 2, 30 | 3, 24 |
| Right maxillary posterior - lingual | |||||
| Mean±SD | 0.5±1 | 2.3±3.9 | 3.0±4.7 | 1.8±2.9 | 2.8±3.1 |
| Median | 0.0 | 0.5 | 1.0 | 0.5 | 2.0 |
| Minimum, maximum | 0, 2 | 0, 8 | 0, 10 | 0, 6 | 0, 7 |
| Maxillary anterior - labial | |||||
| Mean±SD | 9.5±9.0 | 9.0±6.2 | 8.8±5.5 | 7.8±5.6 | 6.0±4.1 |
| Median | 7.0 | 7.0 | 7.5 | 8.0 | 4.5 |
| Minimum, maximum | 2, 22 | 4, 18 | 4, 16 | 2, 13 | 3, 12 |
| Maxillary anterior - palatal | |||||
| Mean±SD | 1.8±1.3 | 1.5±1.9 | 3.0±3.5 | 2.0±1.6 | 2.3±1.5 |
| Median | 2.0 | 1.0 | 2.0 | 2.0 | 3.0 |
| Minimum, maximum | 0, 3 | 0, 4 | 0, 8 | 0, 4 | 0, 3 |
| Right maxillary posterior - buccal | |||||
| Mean±SD | 14.0±12.4 | 9.5±7 | 7.3±7.3 | 9.3±10.4 | 10.0±8.8 |
| Median | 13.5 | 9.5 | 4.5 | 5.5 | 8.0 |
| Minimum, maximum | 2, 27 | 3, 16 | 2, 18 | 2, 24 | 2, 22 |
| Right maxillary posterior - palatal | |||||
| Mean±SD | 1.3±1.9 | 3.8±2.2 | 3.8±4.4 | 2.5±2.7 | 3.0±2.9 |
| Median | 0.5 | 4.0 | 2.5 | 2.0 | 3.0 |
| Minimum, maximum | 0, 4 | 1, 6 | 0, 10 | 0, 6 | 0, 6 |
| Left mandibular posterior - buccal | |||||
| Mean±SD | 8.5±6.0 | 8.3±4.7 | 8.5±7.9 | 7.5±7.9 | 7.3±5.4 |
| Median | 7.0 | 7.0 | 5.5 | 5.0 | 5.5 |
| Minimum, maximum | 3, 17 | 4, 15 | 3, 20 | 1, 19 | 3, 15 |
| Left mandibular posterior - lingual | |||||
| Mean±SD | 7.8±8.1 | 7.5±4.2 | 6.3±5.1 | 6.5±4.1 | 4.3±3.0 |
| Median | 5.5 | 7.5 | 5.5 | 6.0 | 4.0 |
| Minimum, maximum | 1, 19 | 3, 12 | 2, 12 | 3, 11 | 1, 8 |
| Mandibular anterior - buccal | |||||
| Mean±SD | 7.5±4.4 | 7.0±5.0 | 8.0±6.6 | 7.8±6.9 | 8.0±6.7 |
| Median | 6.5 | 6.5 | 6.0 | 5.0 | 5.0 |
| Minimum, maximum | 4, 13 | 2, 13 | 3, 17 | 3, 18 | 4, 18 |
| Mandibular anterior - lingual | |||||
| Mean±SD | 4.3±3.4 | 5.3±4.1 | 4.0±3.4 | 2.3±1.7 | 2.8±2.1 |
| Median | 3.5 | 6.0 | 2.5 | 2.5 | 3.0 |
| Minimum, maximum | 1, 9 | 0, 9 | 2, 9 | 0, 4 | 0, 5 |
| Right mandibular posterior - buccal | |||||
| Mean±SD | 10.5±8.3 | 9.0±7.0 | 9.3±6.9 | 12.0±10.5 | 8.5±10.3 |
| Median | 9.0 | 9.0 | 8.5 | 11.0 | 3.5 |
| Minimum, maximum | 3, 21 | 2, 16 | 2, 18 | 3, 23 | 3, 24 |
| Right mandibular posterior - lingual | |||||
| Mean±SD | 3.8±1 | 6.0±1.6 | 5.3±2.9 | 5.3±3.2 | 5.0±2.5 |
| Median | 3.5 | 6.0 | 4.5 | 5.5 | 4.5 |
| Minimum, maximum | 3, 5 | 4, 8 | 3, 9 | 2, 8 | 3, 8 |
SD=Standard deviation
We further considered the potential influence of sextant and aspect (buccal or lingual) on the mean levels of TB accuracy over study time points. Using a mixed model designed for ordinal outcomes,[25,26] appropriate for our averaged percentages over the three outcomes, we assessed that whether TB location (sextant and surface) on these two parameters accounted for significant differences in intercepts over time. The overall model fit was sufficient in comparison to a null model without estimates for section of teeth (by sextant and surface). Although differences in mean levels among participants for sextant were apparent, they were not significant in our model. There was a significant time × tooth surface interaction, however (γ = 0.37, P < 0.01), suggesting that intercept level differences over time points varied significantly between buccal and lingual brushing. The boxplot in Figure 2 displays these means and variances. Although we did not think that with such a small sample that these differences warranted further investigation, we do think that this could be an important feature to explore in the future and to mention in our discussion (see below); for this reason, we have included boxplots by mean level differences with their variability in TB accuracy for all participants combined and for each participant individually [Figures 2 and 3]. Figure 2 shows the striking stability of lower variances for all participants on the buccal aspect versus stable but much greater variances for the lingual aspect. We reviewed boxplots [Figure 3] of individual participants and also saw this greater variability and less consistency in lingual brushing versus buccal.
Figure 2.

Box plot and whisker plot of toothbrushing accuracy of four participants over five time points. The center dot inside the box represents the mean, the first and third quartiles are at the ends of the box, maximum and minimum are at the ends of the whiskers
Figure 3.
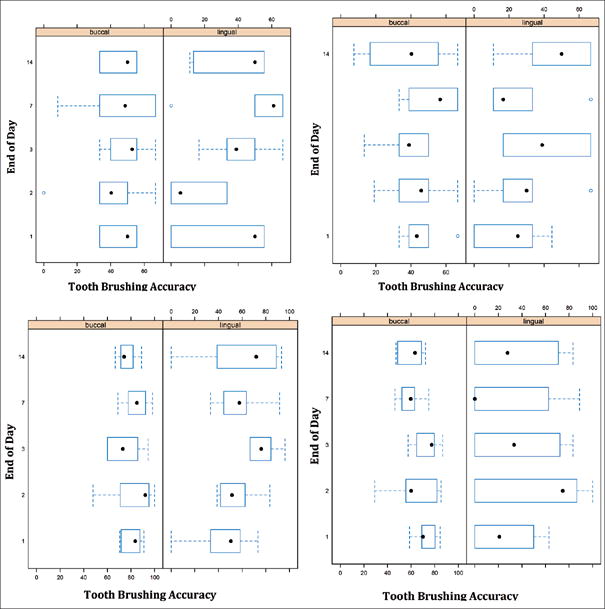
Box plot and whisker plots of toothbrushing accuracy of each of 4 participants over five time points. The center dot inside the box represents the mean, the first and third quartiles are at the ends of the box, maximum and minimum are at the ends of the whiskers
DISCUSSION
In this small but novel study, we determined initial feasibility using SPSV to record TB behavior and as a method to evaluate, in essence, directly observed TB skills and how they changed over 14 days. Investigators rated TB skills of research participants using two methods of direct observation; these methods were based on previous work.[23,24] Similar to other studies,[27] we determined that the length of time a person brushed their teeth did not change measurably after our brief intervention; however, we did observe a modest increase in accuracy and an increase in number of strokes per observed sextant in the initial phases of the study [Table 4]. The IMB model informed the structure and design of our study. Selected participants (dental interns) had background knowledge (information) on the science of teeth and oral health, the importance of TB, and some familiarity with optimal TB skills. A high level of motivation was an inclusion criterion for participants. Our brief training and use of SPVS across time offered some initial exposure to tooth brush behavioral skills training. In future studies, these IMB-related health theory constructs could be defined in detail a priori and measured more precisely. Our main addition to the literature is that similar to areas in medicine,[28–30] dental SPVSs were able to be used easily and efficiently to record, monitor, and evaluate change over time in TB skills after a brief intervention. Importantly, our measure of TB behavior was directly observed and not based on plaque accumulation, gingival or periodontal health;[31–33] such direct observation is critical component to implement and evaluate future IMB-based or informed interventions.
Previously, the effectiveness of TB has been measured either by participant’s self-reported behavior (which is prone to “reactivity”); biological measures (biomarkers/pH etc.); indirect measures (toothbrush changes, tooth wear); direct outcomes (involving biofeedback devices); and clinical outcomes.[15,31] There have been few reports using direct observation methodology to assess and quantify the effectiveness of TB; instead, indirect methods, such as the presence of plaque, calculus, or debris, have been used to measure TB effectiveness—and such indirect approaches have strengths and limitations.[32,33] On the other hand, “biofeedback” devices, a direct method of evaluation, are now available; however, they are bulky, not cost-effective, can be technique sensitive, and often require an “in-office” procedure that can limit access to this technology.[31] As well, sensor-based toothbrushes, another direct method of evaluation, are available and increasingly provide intricate details of TB. Notably, the newly emerging smart toothbrushes[34–38] such as those by Oral-B™ (http://oralb.com/en-us/product-collections/bluetooth) which uses sensors and the Prophix toothbrush (https://www.getprophix.com) which uses cameras and a view screen are compatible with and could enable new advantages for our approach.
Given the current limitations in the dental literature, this study attempted to quantify the quality and accuracy of TB using a novel approach. The current study based its technique on previously described parameters that were used to measure the outcome of teaching TB to preschool children[25] and children with special needs.[26] This subset of the population lacked sufficient motor skill and required constant motivation to help them perform a complex motor skill such as TB.[25,26] For the present study, although the TB accuracy estimation was time-consuming and resource-demanding, the technique we used provided more opportunities for (actual or potential) patient–provider interactions, a more dynamic evaluation and allowed participation from the privacy and comfort of the participant’s own home. For the oral health provider in this study, there was a plethora of TB information and data to review and consider, such as the as the speed and width of the TB stroke, TB bristle angulation, and the targeting of “hot spots”[19] – observations that may prove useful to continue to refine the training process to develop a proper long-term TB habit. In addition, from the patient’s perspective, easily acquiring dental video selfies made the patient an active and contributing participant in the endeavor—rather than a more passive observer, i.e., one who just carries out the instructions of the oral health-care provider. Thus, such active involvement (while not measured in this study) may bolster motivation and increase the likelihood of a patient “sticking with” the process of re-learning and refining their TB skills. Further, the use of dental SPVS may render the patient more conscious while performing the TB behavior and could allow the participant a chance to correct his/her technique by viewing videos again by themselves, engaging in self-evaluation, and then taking corrective action. Thus, engaging in dental SPVS could itself could serve as an agent to reinforce continued TB monitoring and improvement.
The authors intentionally included highly motivated dental interns for this pilot trial since such participants were assumed to be aware of the brushing technique and more likely to understand the nuances of the modified Bass technique. The results from this study may be difficult to generalize in a general population but serve as an indication of feasibility. It is to be noted that the accuracy of participant’s TB skills at baseline and at the end of the study was less than ideal as defined by the modified Bass technique. Other studies have indicated that TB behavior among Indian dental interns does not meet adequate standards[38–40] when compared to students from other countries.
In a very recent study, people’s adaptation to smartphone-based applications (apps) for TB reminders has shown very promising results.[41] Probably, a video-based monitoring app could be useful to a dentist or dental hygienist who could monitor the participant’s TB behavior, which could be recorded in the luxury of one’s own home and later reviewed by an oral health-care provider remotely. The cost of this app on a smartphone could be a minor while there could, potentially, be major long-term benefits to the user’s oral health and quality of life.
To affect motivation and alter skills will, in most instances, require ongoing supervision. Personal hygiene measures such as hand washing[42] or proper TB or other oral hygiene measures (such as flossing) may take a longer period of time than one may anticipate to be integrated into one’s regular routine. Mobile-based applications, however, have been reported to be successful in making surgeons and theater staffs comply with recommended guidelines for hand washing.[42]
The strengths of the present study are in its novel use of SPVS technology, the direct observation methodology (i.e., assessing TB quality and accuracy), and the in-home data collection by study participants. Certainly, given that this was a pilot project, our sample size is very small and we did not quantify IMB constructs. Despite these limitations, we were able to demonstrate important characteristics of the participant experience, both through descriptive and exploratory data analysis techniques.
For example, in this brief study, participants changed their TB behavior only modestly, did not attain proper TB technique and the time they spent brushing remained close to their baseline level. This may imply that “old habits die hard” (i.e., past behaviors strongly influence current behaviors and habits can be challenging to alter). Clearly, greater attention is needed to lengthen the time spent on brushing and a simple intervention such as brushing for the length of a 2 min song (of the participant’s choice) or similar cueing may be helpful. Regarding achieving proper TB technique, perhaps a more gradual and incremental training approach may be encouraged ongoing improvement. Here, ongoing feedback using SPVS technology and a remote “oral health coach”[10] may improve outcomes. Alternatively, having a participant view a dental selfie in which they have (or another person has) executed the TB technique correctly (for a full 2 minutes and with proper attention to each of 12 sections in the mouth) and which the participant can then imitate, may also help improve outcomes over time. By extension, effective interventions that use both SPVS technology and “smart toothbrushes” could have major public health impact.
Although we were unable with this small sample to demonstrate statistically significant mean differences in the interaction of sextant and aspect, it should be noted that on closer examination of boxplots [Figure 3] reflecting the mean in this interaction, there appears to be greater variability across participants and across time points in the sections on the lingual/palatal surfaces as opposed to the facial/buccal surfaces. It was noted by our trainers that the lingual surfaces had been relatively ignored prior the brief intervention; thus, participants were likely making conscious effort to brush these surfaces although overall attention to brushing the lingual surfaces was not consistent. It may also be that success in some areas has to do with handedness and/or the arc of the arm and wrist. These fluctuations over time, after a one-time, brief intervention, may be consistent with proactive interference[12] and may imply that greater and ongoing feedback and/or cueing is necessary in future studies to focus participant’s attention to routinely and properly brush the lingual surfaces of teeth (or other “hot spots”).[19]
CONCLUSION
Herein, we presented innovative use of “video selfies” for monitoring, implementing change, and evaluating the effectiveness of TB behavior. We established initial feasibility by demonstrating a marginal increase in TB effectiveness. Large-scale studies could be conducted pending implementation of reliable and valid automated technology that can determine TB skills in real time. Advances in the field of biomedical instrumentation may currently or soon be able to provide such an option.[35–37] With emerging evidence and insights in the field of health behavior change and brain circuitry,[43] use of innovative practices—such as the video selfie—may be effectively employed to assist long-term change in TB behaviors.[43] Until sufficient evidence-based guidelines emerge, use of dental video selfies could be implemented by clinicians (with the caveat that privacy and confidentiality concerns are addressed) to better serve the oral health needs of their patients.
Table 2.
Summary of the toothbrushing accuracy of four participants across five time points
| Toothbrushing accuracy (%)
|
|||||
|---|---|---|---|---|---|
| Baseline | 24 h | 48 h | 7 days | 14 days | |
| Participant-1 | 40.7 | 25.7 | 45.5 | 48.2 | 42.8 |
| Participant-2 | 44.2 | 36.5 | 39.1 | 39.5 | 42.1 |
| Participant-3 | 62.8 | 68.9 | 76.1 | 71.3 | 68.5 |
| Participant-4 | 49 | 59 | 55.5 | 42.3 | 47.8 |
Acknowledgments
We thank the study participants and the funders of the 7th World Workshop on Oral Health and Disease in AIDS (WW7; that took place in Hyderabad, India, November 6–9, 2014) which allowed the opportunity for Drs. Thavarajah and Vernon to meet and thus collaborate on this manuscript. This work was, in part, funded by an NIH/NIDCR grant R21 DE023740.
Financial support and sponsorship
Nil.
Footnotes
Conflicts of interest
There are no conflicts of interest.
References
- 1.US Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General-Executive Summary. Rockville, MD: US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institute of Health; 2000. [Google Scholar]
- 2.Aunger R. Tooth brushing as routine behavior. Int Dent J. 2007;57:364–76. [Google Scholar]
- 3.Wainwright J, Sheiham A. An analysis of methods of toothbrushing recommended by dental associations, toothpaste and toothbrush companies and in dental texts. Br Dent J. 2014;217:E5. doi: 10.1038/sj.bdj.2014.651. [DOI] [PubMed] [Google Scholar]
- 4.Niederman R. Psychological approaches may improve oral hygiene behaviour. What interventions improve adherence to oral hygiene instruction in adults who have periodontal disease? Evid Based Dent. 2007;8:5–6. doi: 10.1038/sj.ebd.6400487. (Summary Review) [DOI] [PubMed] [Google Scholar]
- 5.Schlueter N, Klimek J, Saleschke G, Ganss C. Adoption of a toothbrushing technique: A controlled, randomised clinical trial. Clin Oral Investig. 2010;14:99–106. doi: 10.1007/s00784-009-0269-1. [DOI] [PubMed] [Google Scholar]
- 6.Fisher JD. The information-motivation-behavioural skills model of HIV preventative behavior. In: Crosby RA, Diclemente RJ, Kegler M, editors. Emerging Theories in Health Promotion Practice and Research. 2nd. San Francisco, CA: Jossey-Bass; 2009. pp. 22–63. a Wiley Imprint. [Google Scholar]
- 7.Miller WL, Rollnick S. Motivational Interviewing, Helping People Change. Vol. 3. New York: Guilford Press; 2012. [Google Scholar]
- 8.Simmons LA, Wolever RQ. Integrative health coaching and motivational interviewing: Synergistic approaches to behavior change in healthcare. Glob Adv Health Med. 2013;2:28–35. doi: 10.7453/gahmj.2013.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fisher JD. The information-motivation-behavioral skills model of HIV preventive behavior. In: Crosby RA, Diclemente RJ, Kegler M, editors. Emerging Theories in Health Promotion Practice and Research. 2nd. San Francisco, CA: Jossey-Bass; 2009. pp. 22–63. a Wiley Imprint. [Google Scholar]
- 10.Vernon LT, Howard AR. Advancing health promotion in dentistry: Articulating an integrative approach to coaching oral health behavior change in the dental setting. Curr Oral Health Rep. 2015;2:111–22. doi: 10.1007/s40496-015-0056-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vernon LT, Demko CA, Webel AR, Mizumoto RM. The feasibility, acceptance, and key features of a prevention-focused oral health education program for HIV+ adults. AIDS Care. 2014;26:763–8. doi: 10.1080/09540121.2013.845291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thavarajah R, Kumar M, Mohandoss AA, Vernon LT. Drilling Deeper into tooth brushing skills: Is proactive interference an under-recognized factor in oral hygiene behavior change? Curr Oral Health Rep. 2015;2:123–8. doi: 10.1007/s40496-015-0053-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Claessen J, Bates S, Sherlock K, Seeparsand F, Wright R. Designing interventions to improve tooth brushing. Int Dent J. 2008;58:307–20. [Google Scholar]
- 14.Arora S, Venkataraman V, Zhan A, Donohue S, Biglan KM, Dorsey ER, et al. Detecting and monitoring the symptoms of Parkinson’s disease using smartphones: A pilot study. Parkinsonism Relat Disord. 2015;21:650–3. doi: 10.1016/j.parkreldis.2015.02.026. [DOI] [PubMed] [Google Scholar]
- 15.Smith D, Walls T. mHealth analytics. In: Marsch L, Lord S, Dallery J, editors. Behavioral Healthcare and Technology. 1st. New York: Oxford; 2015. [Google Scholar]
- 16.Shapiro M, Johnston D, Wald J, Mon D. Patient-Generated Health Data: A White Paper. NC, USA: Office of Policy and Planning Office of the National Coordinator for Health Information Technology; 2012. Available from: http://www.healthit.gov/sites/default/files/rti_pghd_hitepaper_april_2012.pdf. [Last accessed on 2015 May 20]. [Google Scholar]
- 17.Burns K. Digital photography and the medical selfie. J Particip Med. 2015;7:e3. [Google Scholar]
- 18.Schlueter N, Klimek J, Ganss C. Relationship between plaque score and video monitored bushing performance after repeated instruction – A controlled randomized clinical trial. Clin Oral Investig. 2013;17:659–67. doi: 10.1007/s00784-012-0744-y. [DOI] [PubMed] [Google Scholar]
- 19.Winterfeld T, Schlueter N, Harnacke D, Illig J, Margraf-Stiksrud J, Deinzer R, et al. Toothbrushing and flossing behaviour in young adults – A video observation. Clin Oral Investig. 2015;19:851–8. doi: 10.1007/s00784-014-1306-2. [DOI] [PubMed] [Google Scholar]
- 20.Erickson SJ, Gerstle M, Feldstein SW. Brief interventions and motivational interviewing with children, adolescents, and their parents in pediatric health care settings: A review. Arch Pediatr Adolesc Med. 2005;159:1173–80. doi: 10.1001/archpedi.159.12.1173. [DOI] [PubMed] [Google Scholar]
- 21.Greene JC, Vermillion JR. The simplified oral hygiene index. J Am Dent Assoc. 1964;68:7–13. doi: 10.14219/jada.archive.1964.0034. [DOI] [PubMed] [Google Scholar]
- 22.Poyato-Ferrera M, Segura-Egea JJ, Bullón-Fernández P. Comparison of modified Bass technique with normal toothbrushing practices for efficacy in supragingival plaque removal. Int J Dent Hyg. 2003;1:110–4. doi: 10.1034/j.1601-5037.2003.00018.x. [DOI] [PubMed] [Google Scholar]
- 23.Poche C, McCubbrey H, Munn T. The development of correct toothbrushing technique in preschool children. J Appl Behav Anal. 1982;15:315–20. doi: 10.1901/jaba.1982.15-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rachel AB. Graduate Theses Submitted for Master of Arts in Applied Behavior Analysis. Department of Child and Family Studies College of Behavioral and Community Sciences, University of South Florida; 2012. Training and Assessment of Toothbrushing Skills among Children with Special Needs; pp. 19–23. [Google Scholar]
- 25.R Software. R Version 3.2.4 (2016-03-10) – “Very very secure Dishes”. The R Foundation for Statistical Computing Platform: x86_64-apple-darwin13.4.0 (64-bit) 2016 Available at: https://www.r-project.org‖ at the end of the citation. [Last Accessed 2016 May 10].
- 26.Bates D, Machler M, Bolker B, Walker S. Fitting Linear Mixed-Effects Models Using lme4. Available from: http://www.arxiv.org/abs/1406.5823. [Last accessed on 2016 May 20].
- 27.Emling RC, Flickinger KC, Cohen DW, Yankell SL. A comparison of estimated versus actual brushing time. Pharmacol Ther Dent. 1981;6:93–8. [PubMed] [Google Scholar]
- 28.Li X, Xu ZR, Tang N, Ye C, Zhu XL, Zhou T, et al. Effect of intervention using a messaging app on compliance and duration of treatment in orthodontic patients. Clin Oral Investig. 2015 doi: 10.1007/s00784-015-1662-6. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 29.Osborn CY, Egede LE. Validation of an information-motivation-behavioral skills model of diabetes self-care (IMB-DSC) Patient Educ Couns. 2010;79:49–54. doi: 10.1016/j.pec.2009.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gao J, Wang J, Zhu Y, Yu J. Validation of an information-motivation-behavioral skills model of self-care among Chinese adults with type 2 diabetes. BMC Public Health. 2013;13:100. doi: 10.1186/1471-2458-13-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chapple IL, Hill K. Getting the message across to periodontitis patients: The role of personalized biofeedback. Int Dent J. 2008;58:294–306. [Google Scholar]
- 32.McCracken G, Janssen J, Heasman L, Stacey F, Steen N, deJager M, et al. Assessing adherence with toothbrushing instructions using a data logger toothbrush. Br Dent J. 2005;198:29–32. doi: 10.1038/sj.bdj.4811954. [DOI] [PubMed] [Google Scholar]
- 33.Hugoson A, Lundgren D, Asklöw B, Borgklint G. Effect of three different dental health preventive programs on young adult individuals: A randomized, blinded, parallel group, controlled evaluation of oral hygiene behaviour on plaque and gingivitis. J Clin Periodontol. 2007;34:407–15. doi: 10.1111/j.1600-051X.2007.001069.x. [DOI] [PubMed] [Google Scholar]
- 34.Harnacke D, Mitter S, Lehner M, Munzert J, Deinzer R. Improving oral hygiene skills by computer-based training: A randomized controlled comparison of the modified Bass and the Fones techniques. PLoS One. 2012;7:e37072. doi: 10.1371/journal.pone.0037072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Flagg A, Boger J, Mihailidis A. An Intelligent Toothbrush: Machines for Smart Brushing. Abstract Presented at the RESNA/ICTA Meeting: Advancing Rehabilitation Technologies for an aging Society; Toronto, Canada. 2011. [Google Scholar]
- 36.Lee JW, Lee KH, Kim KS, Kim DJ, Kim K. Development of smart toothbrush monitoring system for ubiquitous healthcare. Conf Proc IEEE Eng Med Biol Soc. 2006;1:6422–5. doi: 10.1109/IEMBS.2006.259232. [DOI] [PubMed] [Google Scholar]
- 37.Kim KS, Yoon TH, Lee JW, Kim DJ. Interactive toothbrushing education by a smart toothbrush system via 3D visualization. Comput Methods Programs Biomed. 2009;96:125–32. doi: 10.1016/j.cmpb.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 38.Kripal K, Sirajuddin S, Biswas S, Prabhu SS, Chungkham S, Chandrashekar BM, et al. Oral health knowledge, attitude and behaviour in relation to use of manual toothbrush among dental students in Bangalore, India: A Questionnaire Study. Int J Sci Stud. 2015;2:26–38. [Google Scholar]
- 39.Singh MS, Tuli AK. A comparative evaluation of oral hygiene practices, oral health status, and behavior between graduate and post-graduate dentists of North India: An epidemiological survey. J Int Soc Prev Community Dent. 2013;3:19–24. doi: 10.4103/2231-0762.115713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Folayan MO, Khami MR, Folaranmi N, Popoola BO, Sofola OO, Ligali TO, et al. Determinants of preventive oral health behaviour among senior dental students in Nigeria. BMC Oral Health. 2013;13:28. doi: 10.1186/1472-6831-13-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Underwood B, Birdsall J, Kay E. The use of a mobile app to motivate evidence-based oral hygiene behaviour. Br Dent J. 2015;219:E2. doi: 10.1038/sj.bdj.2015.660. [DOI] [PubMed] [Google Scholar]
- 42.Hlady CS, Severson MA, Segre AM, Polgreen PM. A mobile handheld computing application for recording hand hygiene observations. Infect Control Hosp Epidemiol. 2010;31:975–7. doi: 10.1086/655834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O’Hare JK, Ade KK, Sukharnikova T, Van Hooser SD, Palmeri ML, Yin HH, et al. Pathway-specific striatal substrates for habitual behavior. Neuron. 2016;89:472–9. doi: 10.1016/j.neuron.2015.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]


