Clinical presentation
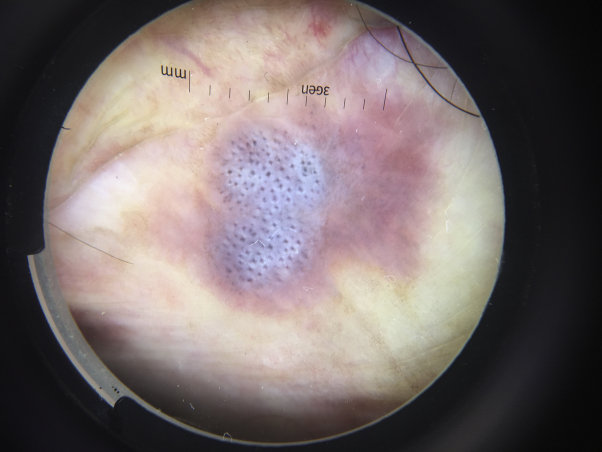
We report the case of a 66-year-old white man with a 6-month history of a blue-gray plaque of the glans. The patient was heterosexual, with 2 sexual partners in the last 6 months, and denied condom use. There was no personal or family history of melanoma. Physical examination of the uncircumcised penis found a round, well-demarcated, smooth, blue-gray plaque measuring 8 × 10 mm, arising within an erythematous background plaque of the glans (Fig 1). The remaining physical examination was unremarkable, including the oral cavity.
Fig 1.
Round, well-demarcated, smooth, blue-gray plaque measuring 8 × 10 mm, arising within an erythematous background plaque of the glans.
Dermoscopic appearance
Within the plaque we observed regularly arranged gray dots surrounded by a white halo over a blue-white structureless background (Fig 2).
Fig 2.
Regularly arranged gray dots surrounded by a white halo over a blue-white structureless background.
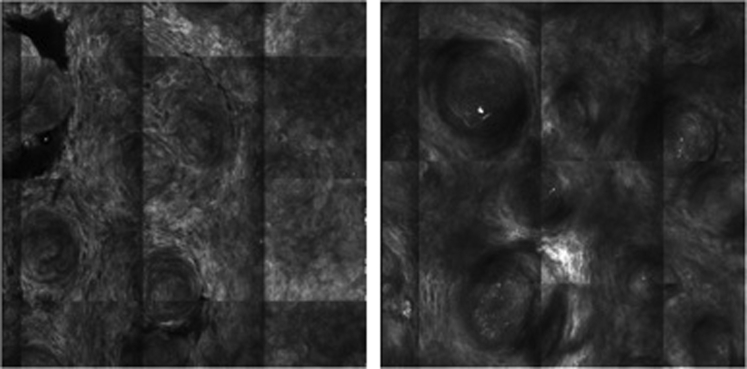
Confocal microscopy appearance
We observed a cordlike pattern with refractile round cellular structures in the stratum corneum, suggesting parakeratosis.1 We also observed a typical honeycomb pattern (Fig 3).
Fig 3.
Cordlike pattern with refractile round cellular structures in the stratum corneum, suggesting parakeratosis. Typical honeycomb pattern.
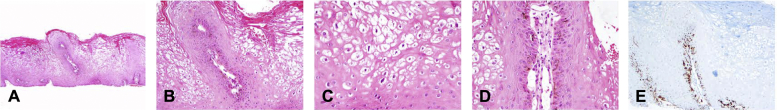
Histologic diagnosis
A shave biopsy found the presence of parakeratosis, acanthosis, and papillomatosis of the epidermis. We also observed within the keratinocytes, abundant cytoplasm and irregularly hyperchromatic nuclei (koilocytosis) (Fig 4). Polymerase chain reaction of the biopsy was positive for human papillomavirus type 6.
Key message.
Genital warts are the most common sexually transmitted disease, and they are caused by the human papillomavirus.2 This case highlights the difficulties encountered in the differential diagnosis of darkly pigmented planar lesions of the penis. Dermoscopic patterns in genital warts have been described by several investigators (fingerlike, knoblike, mosaiclike, and pattern combinations).3, 4, 5, 6, 7, 8 We present a case of genital wart that falls into none of the aforementioned patterns. The honeycomb pattern observed on confocal microscopy is normally observed in seborrheic keratoses. This case illustrates the complementarity of dermoscopy and confocal microscopy in the diagnosis of clinically atypical lesions of the genital mucosa.
Fig 4.
A, Parakeratosis with acanthosis, mild papillomatosis, and diffuse koilocytosis. B, Abundant basal melanic pigment and papilla with prominent ectatic vascular core. C, Detail of the koilocytes with conspicuous perinuclear vacuolization and elongated and irregular hyperchromatic nuclei. D, Detail of a markedly dilated capillary in a papilla and the abundant melanic pigment at the basal layer cells. E, HMB-45 marker highlighting melanocytes and their cytoplasmic processes. (A-D, Hematoxylin-eosin stain; E, HMB-45 stain; original magnifications: A, ×40; B and E, ×100; C and D, ×200.)
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Gonzalez S. [Clinical applications of reflectance confocal microscopy in the management of cutaneous tumors] Actas Dermosifiliogr. 2008;99(7):528–531. [PubMed] [Google Scholar]
- 2.Partridge J.M., Koutsky L.A. Genital human papillomavirus infection in men. Lancet Infect Dis. 2006;6(1):21–31. doi: 10.1016/S1473-3099(05)70323-6. [DOI] [PubMed] [Google Scholar]
- 3.Dong H., Shu D., Campbell T.M., Fruhauf J., Soyer H.P., Hofmann-Wellenhof R. Dermatoscopy of genital warts. J Am Acad Dermatol. 2011;64(5):859–864. doi: 10.1016/j.jaad.2010.03.028. [DOI] [PubMed] [Google Scholar]
- 4.Ozdemir F., Kilinc-Karaarslan I., Akalin T. A pigmented, hemorrhagic genital wart: clinical, dermoscopic, and histopathologic features. Arch Dermatol. 2008;144(8):1072–1073. doi: 10.1001/archderm.144.8.1072. [DOI] [PubMed] [Google Scholar]
- 5.Ozkur E., Falay T., Turgut Erdemir A.V., Gurel M.S., Leblebici C. Vestibular papillomatosis: an important differential diagnosis of vulvar papillomas. Dermatol Online J. 2016;22(3) [PubMed] [Google Scholar]
- 6.Pastar Z., Lipozencic J. Significance of dermatoscopy in genital dermatoses. Clin Dermatol. 2014;32(2):315–318. doi: 10.1016/j.clindermatol.2013.08.016. [DOI] [PubMed] [Google Scholar]
- 7.Veasey J.V., Framil V.M., Nadal S.R., Marta A.C., Lellis R.F. Genital warts: comparing clinical findings to dermatoscopic aspects, in vivo reflectance confocal features and histopathologic exam. An Bras Dermatol. 2014;89(1):137–140. doi: 10.1590/abd1806-4841.20141917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zalaudek I., Giacomel J., Cabo H. Entodermoscopy: a new tool for diagnosing skin infections and infestations. Dermatology. 2008;216(1):14–23. doi: 10.1159/000109353. [DOI] [PubMed] [Google Scholar]