Abstract
Persistent left superior vena cava (PLSVC) is an uncommon congenital anomaly. We report a case of implantation of cardiac resynchronization therapy - pacemaker (CRT-P) device in a 38-year-old lady with idiopathic dilated cardiomyopathy. After left axillary vein puncture, we faced an unexpected entry of left subclavian to PLSVC draining into the coronary sinus (CS). The target posterolateral vein which had been identified before, seemed to have an acute angle at its entry into the CS. Hence, at this stage we were in a dilemma, whether to switch to the right side or to continue from the same side. We continued the procedure from the left side and completed it successfully after some manipulation and improvisation.
1. Introduction
Persistent left superior vena cava (PLSVC) is seen in 0.3–2% of the general population [1]. Its prevalence is much higher (2.8–4.6%) in patients with congenital cardiac anomalies [2]. The two variants are a double SVC (right and left SVC,with or without an innominate vein connecting the two) or a single left SVC (without a right SVC). Unless associated with other significant congenital anomalies, it is usually asymptomatic and unrecognized until a left cephalic or subclavian approach is used as a diagnostic or therapeutic modality. When this entity is encountered during implantation of cardiac resynchronization therapy (CRT) device, placement of leads especially the right ventricular (RV) and the coronary sinus (CS) lead pose technical challenges. Although at times it necessitates switch to the opposite side, often the procedure can be completed from the left side itself with some improvisation of technique.
2. Case report
A 38-year-old woman, known to be suffering from idiopathic dilated cardiomyopathy, presented with recurrent heart failure symptoms. She was in NYHA class III despite optimal medical management with carvedilol, ramipril and diuretics. The ECG showed left bundle branch block (LBBB) with QRS width of 168 ms. The echocardiogram revealed severe left ventricular global hypokinesia with gross left ventricular dyssynchrony. There was no history of any ventricular arrhythmias and a 24-h Holter was also unremarkable. She was electively planned for CRT-pacemaker (CRT-P) implantation.
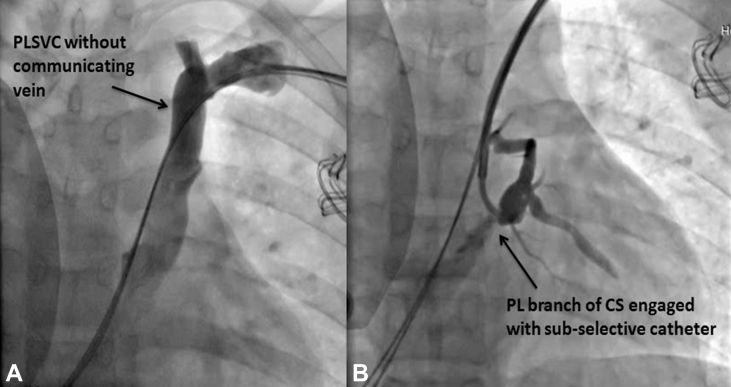
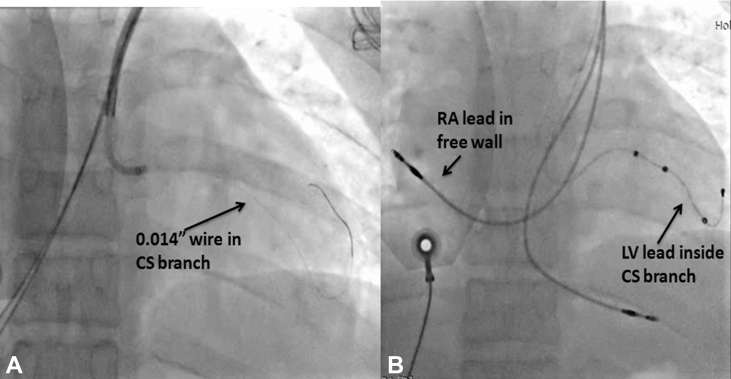
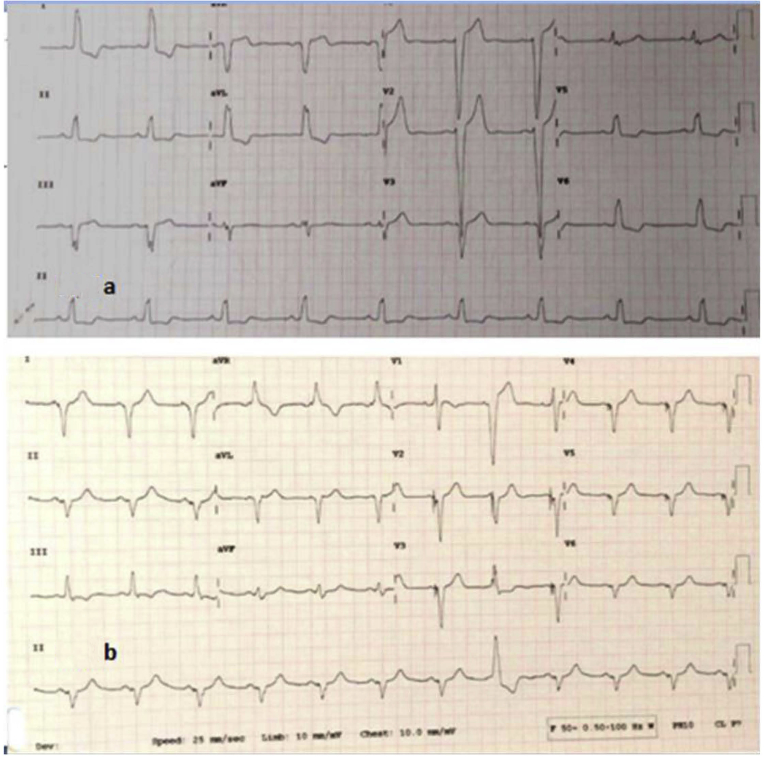
A left coronary angiogram was performed at the beginning of the procedure, the levophase of which showed a large CS with a prominent posterolateral (PL) vein. This vein made a loop before joining the CS at an acute angle of 45°. As per our usual practice, the CRT implantation procedure was started from the left side. A venogram performed from the left arm to visualize the axillary vein for puncture faintly opacified the subclavian vein. A left deltopectoral incision was made and the tissue dissected down to the pre-pectoral fascia. Using the modified Seldinger technique, the axillary vein was accessed; the J tip guide wire entered the left subclavian vein and then immediately passed inferiorly to the left of the spine, suggesting a PLSVC draining into the CS. Two more axillary veinpunctures also showed the guide wires to follow the same course. A left subclavian venogram confirmed PLSVC and did not reveal any communicating innominate vein (Fig. 1A). A multipurpose sheath (St. Jude Medical) was advanced over the guide wire into the CS. As anticipated, it was not possible to pass a 0.014-inch guide wire into the PL vein due to the acute angulation. Through the sheath, a sub-selective catheter with 130° curve (St. Jude Medical) was passed into the entry of the posterolateral vein. A selective venogram showed the expected upward course of the PL vein; additionally, it showed that a large anterior vein was also joining this vein (Fig. 1B). A Sion Blue guide wire (Asahi Corporation, Japan) was negotiated deep into the PL vein (Fig. 2A). A 5F quadripolar (60 mm distal to proximal electrode spacing) left ventricular lead (St. Jude Medical) was passed over the guidewire but due to the acute bend, it could not proceed beyond the loop. The Sion Blue wire was then replaced with a Grand Slam extra support guidewire (Asahi Corporation, Japan) and the lead could then be positioned deep in the PL vein. Adequate lead parameters and stability were achieved, without phrenic nerve capture at high outputs. The CS sheath was kept in situ. The right ventricular and right atrial leads were then positioned fairly easily (Fig. 2B). There was rise in systolic blood pressure by 10 mm Hg along with QRS narrowing by 46 ms (with good R wave in V1, and QS in lead 1, avL) with institution of biventricular pacing (Fig. 3A and B). The rest of the procedure was straightforward and completed without any difficulty.
Fig. 1.
1A.Subclavian venogram showing PLSVC with no communicating innominate vein.
1B. Sub-selective venogram showing the PL vein (PLV).
Fig. 2.
2A. Sion blue wire across the PL vein.
2B. Final positions of all three leads. (PA view).
Fig. 3.
3A. Pre-CRT-ECG showing sinus rhythm and complete LBBB with QRS width of 168 ms.
3B. Post CRT-ECGshowing narrowing of QRS (122 ms) with a sharp RS in V1.
3. Discussion
Most of the patients with PLSVC also have a right SVC, but a bridging innominate vein is absent in the majority [1,2]. Lead implantation in patients with PLSVC is often difficult and technically challenging due to i) abnormal venous anatomy and access to heart, ii) associated other congenital anomalies, iii) absence of bridging innominate vein between PLSVC and right SVC, iv) dilated CS and relatively rapid blood flow and v) difficulties in reaching a convenient pacing site and stable lead position [[3], [4], [5]].
Echocardiography prior to the procedure should specifically look for a PLSVC if the CS is very prominent. However, the CS is often prominent even without a PLSVC due to high venous pressures in patients with heart failure. A left arm agitated saline injection would help in echocardiographic clarification. It is a learning point that routine subclavian venogram taken properly and interpreted carefully might allow us to anticipate this anomaly and be prepared adequately.
While the difficulty of CS cannulation is eliminated by approach via the PLSVC, the selective vein cannulation can be very difficult due to the modified acute angulation, as was seen in our index patient. The AL2 diagnostic catheter is sometimes useful to engage CS branches in this situation, when the CS sub-selection catheter is not helpful. The atrial lead is often needed to be placed at the free wall instead of the right atrial appendage. Negotiation across the tricuspid valve for the right ventricular lead also needs careful manipulation after giving an acute bend to a stiff stylet. There have been a few reports of CRT implantation via a PLSVC [[5], [6], [7], [8], [9], [10]] in the literature, which, like our case, suggest that it is usually possible to complete the procedure from the left side itself, although with a few technical challenges.
Footnotes
Peer review under responsibility of Indian Heart Rhythm Society.
References
- 1.Cha E.M., Khoury G.H. Persistent left superior vena cava. Radiologic and clinical significance. Radiology. 1972;103:375–381. doi: 10.1148/103.2.375. [DOI] [PubMed] [Google Scholar]
- 2.Biffi M., Boriani G., Frabetti L., Bronzetti G., Branzi A. Left superior vena cava persistence in patients undergoing pacemaker or cardioverter-defibrillator implantation: a 10-year experience. Chest. 2001;120:139–144. doi: 10.1378/chest.120.1.139. [DOI] [PubMed] [Google Scholar]
- 3.Konstantino Y., Kusniec J., Shohat-Zabarski R., Battler A., Strasberg B. Cardiac defibrillator implantation via persistent left superior vena cava facilitated by a coronary sinus delivery system. Europace. 2009;11:119–120. doi: 10.1093/europace/eun304. [DOI] [PubMed] [Google Scholar]
- 4.Worley S.J., Gohn D.C., Pulliam R.W. Interventional approach to CRT in a patient with drainage of the superior vena cava into the coronary sinus. Pacing Clin Electrophysiol. 2008;31:506–508. doi: 10.1111/j.1540-8159.2008.01023.x. [DOI] [PubMed] [Google Scholar]
- 5.Sankhla V., Vajifdar B., Shah M., Lokhandwala Y. Left-sided biventricular pacemaker implantation in the presence of persistent left superior vena cava. Indian Heart J. 2010;62:344–345. [PubMed] [Google Scholar]
- 6.Guenther M., Kolschmann S., Rauwolf T.P., Christoph M., Sandfort V., Strasser R.H., Wunderlich C. Implantablecardioverter defibrillator lead implantation in patients with a persistent left superior vena cava—feasibility, chances, and limitations: representative cases in adults. Europace. 2013;15:273–277. doi: 10.1093/europace/eus287. [DOI] [PubMed] [Google Scholar]
- 7.Alemzadeh-Ansari M.J., Shafiee A., Yaminisharif A. Implantation of transvenous permanent pacemaker in a patient with persistent left superior vena cava and absent right superiorvena cava. Int Cardiovasc Res J. 2013;7:152–154. [PMC free article] [PubMed] [Google Scholar]
- 8.Atar İ., Karaçağlar E., Özçalık E., Özin B., Müderrisoğlu H. Implantation of a cardiac resynchronization therapy-defibrillator device in a patient with persistent left superior vena cava. Turk Kardiyol Dern Ars. 2015;43:368–371. doi: 10.5543/tkda.2015.31614. [DOI] [PubMed] [Google Scholar]
- 9.Worley S.J., Gohn D.C., Pulliam R.W. Interventional approach to CRT in a patient with drainage of the superior vena cava into the coronary sinus. Pacing Clin Electrophysiol. 2008;31:506–508. doi: 10.1111/j.1540-8159.2008.01023.x. [DOI] [PubMed] [Google Scholar]
- 10.Elmouchi D., Clyne J. Use of an active fixation coronary sinus pacing lead in a patient with a persistent left superior vena cava. EP Lab digest. 2009;9(5):32–34. [Google Scholar]