Opinion statement
Purpose of review
Parents of infants admitted to the Neonatal Intensive Care Unit (NICU) experience psychological distress, loss of the parenting role, and disruptions to parent-infant bonding. The inclusion of evidence-based practices to address these challenges in the NICU has largely been based upon short-term improvements in parent and infant functioning. However, less is known regarding the extent to which family-based interventions may also be associated with longer-term parenting behaviors and children’s neurobehavioral outcomes.
Recent findings
Comprehensive family-based NICU interventions demonstrate consistent links with later parental mental wellbeing, sensitive parenting behaviors, and children’s cognitive and socioemotional development. Dyadic co-regulation activities implemented inconsistently and/or in isolation to other components of NICU interventions show mixed associations with outcomes, highlighting the need for multifaceted wrap-around care. Further research is needed to delineate associations between NICU interventions and children’s neurological and language development, with follow-up beyond very early childhood in larger samples.
Summary
Long-term associations may reflect the stability of early parental responses to NICU interventions and the extent to which parents continue to implement mental health and sensitive parenting techniques in the home. However, the transition of parental psychiatric care from hospital to community-based services upon NICU discharge remains a pertinent need for high-risk families. Remaining issues also concern the extent to which NICU interventions incorporate sociodemographic differences across families, and whether interventions are generalizable or feasible across hospitals. Despite variation across interventions and NICUs; supporting, educating, and partnering with parents is crucial to strengthen longer-term family functioning and alter the developmental trajectories of high-risk infants.
Keywords: Neonatal intensive care unit, family-centered care, parenting, child development, follow-up
Introduction
The Neonatal Intensive Care Unit (NICU) is a specialized level-III/IV treatment setting for high-risk infants. From 2007 to 2012, American NICU admissions rose from 6.4% to 7.8% of all live births (1). Parents of hospitalized infants experience psychological distress, loss of the parental role, and disrupted parent-infant bonding (2,3). The inclusion of evidence-based practices to address these challenges has largely been based upon improvements in parental functioning reported during the NICU stay. However, less is known regarding longer-term family outcomes post-NICU discharge. This review examines links between family-based NICU interventions and longer-term parenting behaviors and children’s neurobehavioral outcomes.
Mental Health in the NICU
Maternal depression before and during pregnancy increases the likelihood that an infant will be admitted to the NICU and compounds the risk for postpartum depression (4–7). Up to 20% of mothers of hospitalized infants experience depression, with more severe symptoms than mothers of healthy infants (7–9). Anxiety and post-traumatic stress disorder (PTSD) are also common among parents of hospitalized infants (4,8). Approximately 35% of mothers and 24% of fathers experience Acute Stress Disorder days after infant hospitalization, with 15% of these mothers and 8% of these fathers having ongoing PTSD symptoms (6). Importantly, poor parental mental health disrupts parent-infant bonding in the NICU (10).
Having an infant in the NICU is a stressful experience for parents, with sources of psychological distress reported across a number of domains. For example, the health of the hospitalized infant is a key source of distress as parents feel helpless to protect their baby from medical procedures (11,12). Parents also report witnessing near-death and resuscitation events as overwhelming and frightening (13). Findings from multiple cohorts indicate that the perceived loss of the parental role is a prominent NICU-related stressor (11,12,14). A recent study (n=211) found that parents experienced greater levels of stress relating to parent-infant separation, the inability to provide care and disrupted parent-infant bonding relative to stress concerning their infant’s appearance and the NICU environment (12). Wider sources of stress reflect the practical challenges that parents encounter as they attempt to visit their infant in the NICU, spanning difficulties with time management, organizing child care, and family finances (15).
Social Circumstances
Mothers from socially disadvantaged backgrounds are more likely to have a hospitalized infant and longer NICU stays as a result of exposure to poverty, high stress levels, and poor prenatal care coupled with obstetric complications (16–18). Social adversity also places families at increased risk of stress and psychopathology in the NICU (8,14). Key predictors include low education, single parenthood, and prior stressful life events (8,11,14). Worryingly, families facing socio-economic hardships have more limited means to facilitate NICU visitation, which in turn, hinders early parental adjustment and engagement (3,19). Parental engagement, defined as participation in clinical decision making and caregiving in the NICU, improves infant health and family outcomes (3). Enhancing parental engagement, however, is relies upon the development and implementation of interventions that support parents during the NICU stay (20).
Family-Based NICU Interventions
Family-based interventions advocate that optimal family outcomes are achieved when parents are supported, educated, and included in the healthcare team (20–22). Key components of family-based care span the physical NICU environment and addressing the psychosocial needs of parents (Figure 1). Comprehensive interventions include Family-Centered Care (20,21,23), Family Integrative Care (24), Compassionate Family Care (25), Family Support (2,20,21) and Neonatal Integrative Developmental Care (26). These interventions support parents via collaborative partnerships; access to psychosocial care; restoration of the parenting role; and supporting the transition to home (Table 1) (23,27).
Figure 1.
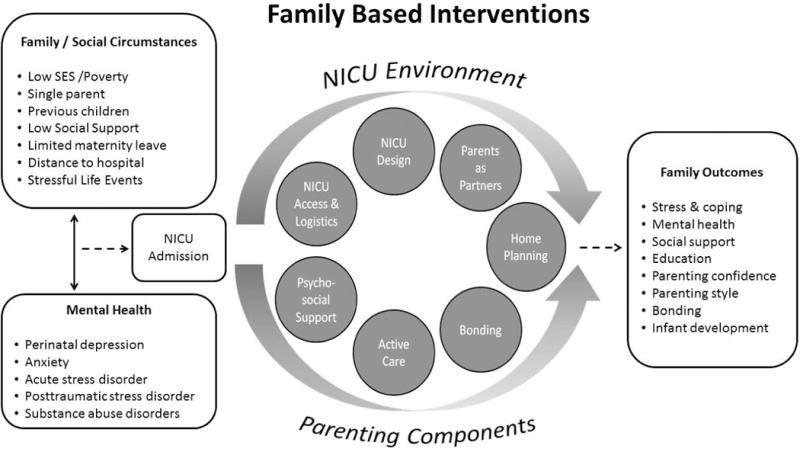
A Conceptual Overview of Family-Based NICU Interventions. This figure provides a conceptual overview of links between family social circumstances leading to NICU admission; core components of family-centered care implemented in the NICU; and targeted longer-term family outcomes.
Table 1.
Summary of Family-Based Interventions Used in the Neonatal Intensive Care Unit (NICU)
| Model | Description | Core components | Program Implementation | Duration | Populations | Outcomes | |
|---|---|---|---|---|---|---|---|
| Parent Centered Interventions | Family-Centered Care (20,21,23) | Mutually beneficial partnerships between NICU staff & parents | - Parents as partners - Participation in caregiving - Information sharing - Respect & dignity for families |
- Open NICU access - Care for all family members - Education sessions - Active caregiving - Peer-to-peer support groups - Sibling education - Home transition planning |
NICU admission to transition to home | - Preterm infants - Infants with birth defects |
↑ Psychological wellbeing ↑ Social Support ↑ Confidence ↑ Knowledge transformation ↑ Engagement ↑ Attachment/bonding |
|
| |||||||
| Family Integrated Care (24,51) | Parents are completely integrated into the NICU care team | - Support, educate & empower parents - Restoration of parenta role |
- Education sessions - Peer-to-peer support groups - Bedside parental presence - Attend clinical rounds - Active caregiving - Perform basic charting |
NICU admission | - Preterm infants - Infants with no/low respiratory support |
↑ Parenting efficacy ↑ Attachment/bonding |
|
|
| |||||||
| Compassionate Family Care (25) | Compassionate partnerships between NICU staff & parents | - Parents as partners - Communication - Compassionate relationships |
- Active listening - Addressing parental concerns/needs - Positive communication |
NICU admission to transition to home | - Preterm infants - Critically ill term infants |
↑ Parenting efficacy ↑ Empowerment ↑ Attachment/bonding ↑ Developing identity |
|
|
| |||||||
| Parental Presence at the Bedside (37) | Parental presence as part of family-centered care | - Parents as partners - Communication - Create learning opportunities |
- Attend clinical rounds - Bedside parental presence - Parents encouraged to ask questions |
Variable: During NICU stay, rounds approx. 2 hours long | - Preterm infants admitted for 5 consecutive days | ↑ Psychological wellbeing ↑Confidence in healthcare providers |
|
|
| |||||||
| Neonatal-Family Interventions | Neonatal Integrative Developmental Care (26) | Holistic neuroprotective, family-centered, developmental care | - Healing environment - Parents as partners - Protect infant brain development - Support infant neurobehavioral & neurosensory development |
- Open NICU access - Single family NICU rooms - Education sessions - Interactive workshops - Psychosocial support - Skin-to-skin contact - Active caregiving - Home transition planning |
NICU admission to transition to home | - Preterm infants | ↑ Knowledge transformation ↑ Social Support ↑ Confidence ↑ Engagement ↑ Attachment/bonding ↓Hospital stays |
|
| |||||||
| NIDCAP Individualized Care Program (49) | Individualized, developmentally supportive, family-centered care | - Parents as partners - Attachment/bonding - Co-regulation - Infant development |
- Developmentally sensitive care - Assess infant’s capabilities - Reading infant behavioral cues - Skin-to-skin contact |
NICU admission to transition to home | - Preterm infants - Critically ill term infants |
↑ Self-regulation ↑ Competence ↑ Psychological wellbeing ↑ Parent-infant interaction ↑ Attachment/bonding |
|
| Modified Mother-Infant Transaction Program (58) | Parental sensitively and stimulation activities | - Mother as the interventionist - Recognize and support infant needs - Initiate positive stimulation |
- Education sessions - Verbal instruction - Infant observation - Handling infants - Skin-to-skin contact - Infant massage - Infant bath session |
NICU admission and in-home follow-up visits | - Preterm infants | X Depression ↓ Stress ↑ Sensitive parenting ↑Parent-infant synchrony |
|
|
| |||||||
| Newborn Behavioral Observations System (48) | Assess infant capabilities in the context of parent-infant dyad | - Infant behavior as communication - Caregiver awareness & responsiveness - Quality of parent-infant interaction |
- Structured observations - Education sessions - Active caregiving |
Variable: Delivery to 3 postpartum | - Term infants - Preterm infants |
↑ Knowledge transformation ↑ Competence ↑ Parental role ↑ Attachment/bonding ↑ Parent-infant interaction |
|
|
| |||||||
| Family Nurture Intervention (50) | Dyadic co-regulatory activities | - Attachment/bonding - Infant development - Maternal wellbeing |
- Isolette odor exchange, sustained touch, vocal soothing, eye contact - Active caregiving - Family sessions |
NICU admission to transition to home | - Preterm infants | ↑ Social support ↑ Psychological wellbeing ↑ Parent-infant interaction |
|
|
|
|||||||
| Psychosocial Interventions | Creating Opportunities for Parent Empowerment (42) | Three phase educational-behavioral program | - Parental education - Parental engagement - Restoration of parental role |
- Education sessions - Audiotapes - Written materials - Activity workbook - Active caregiving |
NICU admission to transition to home | - Preterm infants | ↓ Stress ↑ Psychological wellbeing ↑ Competency ↑ Knowledge transformation |
|
| |||||||
| Individualized Support (43) | Five phase individualized intervention | - Strategies for coping - Dealing with grief - Restoration of parental role - Family dynamics |
- Education sessions - Workshops - Guided activities with baby - Home transition planning |
NICU admission to transition to home | - Congenital heart defect - Perinatal HIE - At least 4 weeks in NICU |
↓ Anxiety ↓ Depression X Stress |
|
|
| |||||||
| Counseling Model for Postpartum Women (45) | Counselling intervention | - Expression of feelings - Perceptions of birth trauma - Strategies for coping |
- Brief counselling sessions | Variable: Within 72 hours of delivery to 4 – 6 weeks postpartum | - Traumatic birth - Has not been evaluated in context of preterm birth |
↑ Social support ↑ Psychological wellbeing |
|
|
| |||||||
| Prevention of Traumatic Stress in Mothers with | Intervention for posttraumatic stress, depression & | - Trama focused treatment - Psychoeducation - Cognitive restructuring |
- Highly manualized therapeutic sessions - Once or twice weekly - 44 – 45 minutes per session |
Variable: 3 – 4 weeks during the NICU stay | - Preterm infants | ↑ Psychological wellbeing ↓ PTSD |
|
| Preterm Infants (46) | anxiety | - Redefining negative perceptions | |||||
|
| |||||||
| Peer-to-Peer Support (20) | Connecting current NICU parents with veteran NICU parents | - Parents as partners - Parent education |
- Education sessions - Peer-to-peer support groups - Bedside support - Telephone support |
NICU admission to transition to home | - Not defined | ↑ Knowledge transformation ↑ Social support ↑ Parent-staff communication ↑ Coping |
|
Note. Preterm infants <33 weeks gestational age. ↑ indicates increase in positive outcome; ↓ indicates reduction in adverse outcome; X indicates no effect. NIDCAP: The Newborn Individualized Developmental Care & Assessment Program. HIE: hypoxic-ischemic encephalopathy.
Design of the NICU
The NICU consists of open-bay wards, and more recently, single family rooms (28). Open-bay wards contain multiple infant isolettes and small family areas in close proximity, which some parents find overwhelming (29). Single family rooms were therefore introduced to protect the family unit (28). Infants placed in single family rooms show better clinical progress and experience greater parental caregiving (29,30). Family benefits include increased parental visitation, privacy, and family cohesion (29,31). However, one study found that after accounting for wider social support, mothers in single family rooms reported greater stress compared to mothers in open-bay wards, potentially due to their perceived isolation and/or obligation to provide care (31). This highlights the importance of balancing NICU design features such that parents in open-bay wards have access to private spaces, and parents in single rooms are connected with peer-support groups (20).
Parents as Partners
An important cornerstone of NICU access concerns welcoming families as partners in the healthcare team (32). Unrestricted visiting hours and the ability to bring support persons to the NICU is associated with positive parental perceptions of the NICU (33). There has also been some effort to provide access to supervised hospital playrooms for parents with additional children (2,34). However, as some playrooms do not supervise infant siblings and/or have specific hours, parents still report challenges with childcare (15). Nonetheless, an expanding NICU practice concerns parental presence at the infant’s bedside during clinical rounds (35). Parental presence at the bedside encourages knowledge exchange such that staff can ascertain the needs of each family and discuss infant clinical progress (25) while parents participate in shared decision making (24,34,35). Parental presence increases confidence in the healthcare team, reduces anxiety and stress, and is linked to improved neonatal outcomes (36–38).
Psychosocial Interventions
To promote parental wellbeing during the parent’s earliest experiences with their infant (39), many NICU interventions integrate psychosocial services as part of wrap-around care (22,26,40). Embedding mental health professionals is important to contextualize parent’s negative emotions and screen for current or emerging psychopathology (41). Effective interventions span educational-behavioral programs (42), psychological interventions (43,44), and trauma-focused care (45,46).
Both educational- and cognitive-based interventions reduce depressive symptoms in the perinatal period, with less consistent effects found for anxiety. For example, the Creating Opportunities for Parental Empowerment (COPE) program is an educational-behavioral intervention administered from NICU admission to 1-week post-hospital discharge (42). The COPE provides parents with information and behavioral activities that reinforce topics related to high-risk infants and sensitive parenting. Study findings indicated that COPE mothers (n=138) had reduced NICU-related stress (d=.27) than control mothers (n=109), although effects on depression and anxiety were not evident until 2-months post-NICU discharge (42). The efficacy of the COPE has also been examined as part of a meta-analysis reporting NICU intervention effects on depression and anxiety (44). Compared to educational programs (including the COPE) and dyadic mother-infant interventions, the meta-analysis showed that Cognitive Behavioral Therapy was the most effective type of intervention to treat depression in the NICU (44). While the meta-analysis was not able to detect pooled intervention effects for anxiety, improvements in anxiety have been reported following the completion of an individualized intervention that addressed parental grief and coping, integrating the infant into the family, and hospital discharge planning (43).
Trauma-focused interventions show promise for treating perinatal-specific PTSD. For example, a 6-session PSTD intervention utilized therapeutic activities to address birth trauma through psychoeducation, cognitive restructuring, and muscle relaxation (46). By 1-month postpartum, mothers (n=62) who received trauma-focused NICU care had lower PTSD (d=0.41) and depressive (d=0.59) symptoms compared to control mothers (n=43). Furthermore, mothers with high stress levels pre-intervention demonstrated greater gains in wellbeing post-intervention, highlighting benefits of trauma-focused care in high-risk parents (46).
Peer-to-peer support is a widely utilized psychosocial intervention, connecting current NICU parents with veteran parents through meetings in the NICU or through telecommunication services (20,47). Support provided by peer groups is valuable for NICU parents who do not have or do not use existing support systems, or who do not respond to clinician-led programs. However, the success of peer-support depends upon how well families are matched on sociodemographic and infant characteristics; length of NICU stay; and how willing parents are to leave their infant’s bedside (41,47).
The Parental Role
To mitigate the loss of the parenting role, family-based interventions optimize parental engagement through educational and guided caregiving activities (20,26,34). Parenting interventions include Family Integrated Care (24), the Neonatal Behavioral Observations (NBO) system (48), the Newborn Individualized Developmental Care Program (NIDCAP) (49), and the Family Nurture Intervention (FNI) (50). The core philosophy of Family Integrated Care is to include parents as healthcare team members (51). Parents attend clinical rounds, complete basic charting, and perform caregiving tasks and skin-to-skin care (also known as kangaroo care). Family Integrated Care has been piloted in a sample (n=42) of mothers of very preterm (VPT, <32 weeks gestation) infants (51) and is being evaluated in a large trial spanning 27 NICUs (24). Pilot results suggest that Family Integrated Care is associated with improvements in infant weight gain, parental stress, and incidence of breastfeeding by hospital discharge (51).
Neuro-protective developmental interventions encourage sensitive caregiving in the context of the parent-infant relationship (52,53). In the NBO, the clinician demonstrates handling and caregiving techniques that parents can use in the home (48). Similarly, the NIDCAP invites parents to observe the clinician as they develop an individualized caregiving plan tailored to the infant’s neurobehavioral sensory and regulatory capacities (49,54). A small study found that NBO mothers (n=10) gained knowledge regarding their infant’s capabilities and how to sensitively interact with their infant (55). Gains in parenting confidence and knowledge (d=.25–.54), as well as positive parent-infant interactions in the NICU (d=.26), have also been linked to the COPE program (42).
Dyadic co-regulation interventions target parent-infant bonding in the NICU (21,56–58). The FNI has parents participate in tactile, visual, and vocal activities at the bedside, and skin-to-skin contact during holding and feeding (50). The FNI promotes higher-quality caregiving in the NICU (59) and reduces depression and anxiety from term to 4-months post-intervention (60). Skin-to-skin care encourages bonding because it unites parent and infant, and activates the release of oxytocin and reduction of cortisol during contact (61). However, positive correlations have been reported between hours of skin-to-skin care and parental stress (62), potentially highlighting the need to consider parenting readiness in the NICU.
The Transition to Home
The continuum of parental needs extends beyond the NICU stay (63,64). Discharge planning should begin early and provide incremental education about the discharge process (20). The Train-To-Home program delivers information on neonatal health and key NICU-to-home milestones to increase parental understanding of infant clinical progress and subsequent readiness for discharge (65). Overnight transition rooms also facilitate discharge readiness as parents provide independent care within the monitored environment (66,67). Importantly, systematic discharge planning is associated with reduced outpatient healthcare utilization and fewer re-hospitalizations (68–70).
As part of the transition of care, Family-Centered Care recommends appointing a NICU team member to coordinate follow-up appointments with a primary care provider and/or pediatric specialist to meet the infant’s ongoing medical needs (64,69,71). Parental referral to community-based psychiatric services, however, remains a pertinent need for high-risk families. Mothers with psychiatric disorders perceive themselves as having poor emotional readiness for NICU discharge (72), with ongoing risks for postpartum depression (73). In-home follow-up visits may, to some extent, facilitate continued nursing care and psychosocial support (64).
Longer-Term Parenting Outcomes
Family-based NICU interventions directly restore the parental role and support the foundation of sensitive parenting behaviors (20). Longer-term parenting domains that have been evaluated thus far include parental mental wellbeing, the quality of the home environment, and parenting behaviors in the context of the parent-child relationship.
Parental Mental Wellbeing
Longitudinal findings highlight the role of NICU-based psychiatric treatments and dyadic interventions on parental mental wellbeing within 12-months of discharge (42,46,57,74). For example, after covariate adjustment, mothers who completed COPE had reduced anxiety (d=.24) and depressive (d=.30) symptoms compared to control mothers at 2-months follow-up (42). Similarly, Shaw et al. found that their trauma-focused intervention (46) had increasing benefits for depression, anxiety, and PTSD symptoms from 1- to 6-months post-intervention (75). This might suggest that trauma-focused interventions have delayed effects and/or that responses to trauma-focused interventions continue to emerge as mothers use learned cognitive-behavioral techniques in the home.
In terms of dyadic interventions, Holditch et al. examined whether skin-to-skin contact and a multisensory auditory-tactile-visual-vestibular (ATVV) intervention improved parental psychological wellbeing at 12-months post-intervention (74). Compared to mothers who did not complete any NICU intervention, mothers who performed infant massage (including ATVV) showed improvements in depressive symptoms, whereas skin-to-skin care reduced infant-related worries (74). When taken together, findings suggest that psychiatric interventions have targeted effects on parental wellbeing due to shared underlying mental health constructs, whereas dyadic interventions may have more general effects on parental wellbeing.
The Home Environment
Follow-up studies have examined the quality of the home environment using the Home Observation for Measurement of the Environment (HOME) inventory (57,74,76). Feldman et al. found that preterm infants of mothers who provided consistent skin-to-skin care obtained higher Emotional and Verbal Responsiveness (d=.48), Organization of the Physical Environment (d=.48), and Opportunities for Variety in Daily Life (d=.40) HOME scores than demographically-matched control mothers of preterm infants at the 3-month follow-up (57). Similar associations between dyadic co-regulation interventions and total HOME scores have also been reported at 6-months post-intervention (74). In contrast, the parent training Parent Baby Interaction Program (PBIP) was not associated with stimulation and support provided to the child in home (76). The PBIP was, however, a low-dose intervention administered in a stressed sample of mothers, coupled with low rates of skin-to-skin care. Thus, dyadic interventions that reduce mother-infant separation need to be implemented often and consistently to engender maternal bonding, emotional closeness, and supportive behavior that generalizes beyond the NICU (77).
The Parent-Child Relationship
Surprisingly, mixed outcomes have been reported between dyadic co-regulation interventions and the longer-term quality of the parent-child relationship (57,58,74,76). For example, a modified version of the Mother-Infant Transaction Program (MITP) that included skin-to-skin care, was associated with higher observational ratings of parent-infant reciprocity and synchrony at 3-months follow-up (58). Skin-to-skin care is also linked to longer-term sensitive parenting behaviors characterized by positive affect, timely and appropriate responses, and adapting behavior to suit the changing needs of the infant (57). Findings likely reflect homotypic continuity in terms of parents continuing to implement sensitive parenting techniques in the home (42,55,57,59). Infants who are better regulated as a result of NICU family-based interventions may also be easier to parent, thereby contributing to the reciprocal parent-infant relationship (78,79). On the other hand, Holditch et al. did not report any dyadic co-regulation intervention effects on observational ratings of parental involvement at 2- and 6-months follow-up (74). However, discrepancies between study findings may be explained by differences in sample characteristics, parenting variables examined, and the extent to which mothers participated in other non-assigned NICU interventions. Compared to follow-up studies of dyadic interventions, few studies have examined links between educational or psychiatric interventions and longer term parenting behaviors despite initial evidence linking the COPE with more positive mother-infant interactions in the NICU (42). There is also a paucity of findings beyond 12-months follow-up. However, registered protocols indicate that studies investigating parenting outcomes by 5-years post-intervention are forthcoming (80,81).
Longer-Term Child Outcomes
Family-based NICU interventions support children’s neurobehavioral outcomes through early contributions to neural and neurophysiological organization, and through early and continued parental involvement (49,54,57,79). Reported outcomes include brain development, cognitive ability, language skills, and socioemotional behaviors. Fewer studies have examined neuromotor outcomes (30,54,82). However, as family-based interventions do not typically target infant motor development (83), these findings will not be discussed.
Brain Development
Studies linking family-based interventions with structural and functional brain development have focused on the neonate (54,84–86). Just two studies have examined associations between the NIDCAP and structural and functional connectivity in school-age preterm children (29–33 weeks gestation) born birthweight appropriate for gestational age (87) or intrauterine growth restricted (88). Compared to preterm children who received standard care as infants, the non-growth restricted NIDCAP cohort had more mature frontal and parietal brain connectivity and more mature fiber tracts in the internal capsule and cingulum bundle at age 8-years (87). Similarly, the growth restricted NIDCAP cohort had increased connectivity between frontal, occipital and parietal regions, and larger cerebellums than control preterm children at age 9-years (88). These collective findings advocate for neuroprotective developmental care in the NICU. However, both of studies included small samples (n<25) and thus study replication with larger cohorts is warranted.
Cognition
Follow-up studies have examined a wide range of NICU interventions on cognitive outcomes from age 6-months to school-age. Findings from two preterm cohorts suggest that infants cared for in single family rooms obtain higher cognitive scale scores on the Bayley Scales of Infant Development-III (BSID-III) at age 18–24 months than infants cared for in open-bay rooms (89,90). However, the extent to which these findings reflect higher levels of parental caregiving and/or other NICU interventions implemented in single family rooms remains unclear (29).
In terms of links between isolated parenting activities in the NICU and cognitive outcomes, findings are mixed. One prospective study found that preterm infants (25–34 weeks gestation) who received skin-to-skin care in the NICU obtained higher BSID-II cognitive scores at age 6-months compared to infants who received standard care (57). A more recent retrospective study, however, reported non-significant associations between hours of skin-to-skin care in the NICU and cognitive outcomes of extremely preterm infants (<27 weeks gestation) at ages 6- and 12-months (91). Discrepancy in findings may be attributed to differences in infant clinical characteristics, and the fact that one study (91) analyzed hours of skin-to-skin care using a median split which potentially masked linear associations with cognitive scores (92).
In comparison, comprehensive parenting interventions show consistent associations with cognitive outcomes (54,87,93,94). For example, the COPE program was associated with higher cognitive scores in low birthweight preterm infants at ages 3-months (d=.60) and 6-months (d=.72) (94). COPE mothers were likely better prepared to parent a high-risk infant, having gained parenting confidence and knowledge in the NICU (42). While the NIDCAP is not effective in reducing global neurodevelopmental impairment (82), the NIDCAP is associated with improved general cognitive ability at age 9-months (54) and performance on tasks drawing upon planning, decision-making, executive function, and visual-spatial processing at age 8-years (87). Taking findings together, the context in which neuroprotective care, dyadic co-regulation activities, and holistic parenting programs are implemented in the NICU appear to support general cognitive development in very early childhood, and components of executive function at school age.
Language
Follow-up studies are now linking single family NICU rooms with language outcomes in childhood, however, the findings have been mixed (85,89,90,91). For example, one study found that compared to VPT infants placed in an open-bay wards (n=40), VPT infants placed in single family rooms (n=46) obtained lower BSID-III language scores (d=.61) at age 2-years (85). Findings persisted after adjusting for family background, parental visitation, and holding in the NICU; potentially highlighting the role of sensory deprivation among disadvantaged samples with low visitation rates. In contrast, Vohr et al. found that low birthweight infants placed in single family rooms (n=161) had higher total and expressive BSID-III language scores at age 18–24 months (90). While other studies suggest that single family rooms are associated with increased visitation and enhance the effects of parental involvement on language outcomes (28,31,89), Vohr et al. did not adjust findings for NICU visitation rates which may have indirectly contributed to language outcomes.
Socioemotional Development
Few follow-up studies have assessed internalizing and externalizing outcomes. Pineda and colleagues reported that after adjusting for clinical, social, and family factors; VPT infants placed in single parent rooms received higher parent-report ratings on the externalizing problems scale of the Infant Toddler Social Emotional Assessment at age 2-years, than infants in open-bay wards (85). This finding potentially reflects the longer-term sequelae of low parental involvement during a sensitive period of infant brain development, or the heritability of externalizing problems as parents with psychopathology may be less likely to engage in NICU care. Other indirect factors, including the quality of care and mental health support provided in the NICU, predict internalizing problems in early childhood (95).
Comprehensive NICU interventions show reliable associations with both parent-report and observational ratings of socioemotional outcomes (54,58,93). For example, mothers who completed the MITP, which included skin-to-skin care, were more likely to rate their infants as having easier temperament, more approach behaviors, and fewer regulatory problems at age 3-months compared to preterm infants who received standard care (58). The NIDCAP has also been associated with observational ratings of emotion regulation skills (54), whereas the FNI has demonstrated positive associations with parent-report ratings of social-relatedness and attention in very early childhood (93). Dyadic co-regulation activities implemented in isolation to other parenting practices, however, do not appear to be effective (57). Supporting children’s socioemotional development may, therefore, depend upon comprehensive NICU interventions that target ways in which parents can sensitively interact with and support their infants in the NICU and provide the foundation for later positive parenting behaviors (96).
Directions for Future Research
In light of associations between family-based NICU interventions and longer-term parent and child outcomes, a number of research gaps remain. First, most follow-up studies have focused on preterm populations. Less is known about the utility of NICU interventions in parents of infants with specific high-risk medical complications who may need individualized support. Second, as family-centered care is multifaceted, it is difficult to pinpoint independent and/or additive effects attributable to components of an intervention (30,74,76). Thus, the need for large prospective RCTs remains. Third, as recent studies highlight gaps in service provision for mothers with psychopathology (72,97), investigation of NICU discharge planning that incorporates referral to community-based mental health programs is desperately needed for mothers with perinatal mental health disorders.
Remaining Clinical Considerations
A remaining challenge of NICU intervention implementation is to accommodate differences across sociodemographic groups. High-risk mothers are more likely to have an infant admitted to the NICU (7,16) but have low visitation rates due to their sociofamilial circumstances (19). Furthermore, the ability to take extended maternity or family medical leave undeniably impacts the extent to which parents are able to engage in NICU interventions (58,98). Although some social factors may not be modifiable, NICU access and interventions may need to be tailored for parents who are willing to provide care but lack the mobility to do so. Careful consideration should also be given to intervention timing and duration (40,76). Intervening when parents are less traumatized may improve engagement in parenting interventions, and therefore, longer-term parental wellbeing and family functioning (45,62).
In the application of family-based NICU interventions, the extent to which interventions are generalizable or feasible across hospitals remains unclear. Variation in NICU practices may reflect the fact that family-based interventions are heterogeneous; differing in focus, duration, and the resources needed to implement the program. Disparities in service provision may also exist due to NICU differences in administrative organization, staff culture and/or expertise, and NICU design or resources (99). Some NICUs may also be situated in adult hospitals (likely adjacent to an obstetric service) and are attempting to implement family-centered care in a hospital that typically serves adult patient populations. For a small service to implement family-focused care within an adult hospital, it requires overcoming numerous barriers that may not be encountered in pediatric hospitals. Thus, some NICUs implement all components family-care while others offer isolated components or are at varying stages of implementation (21,97,99). In addition, there are no standardized recommendations for providing psychosocial support in the NICU, underscoring the importance of embedding evidence-based guidelines for psychiatric and trauma-focused care (97).
Conclusions
Comprehensive family-based NICU interventions address parental psychological distress, the loss of the parenting role, and disruptions to parent-infant bonding. Extending short-term outcomes, improvements in parental mental wellbeing, sensitive parenting behaviors, and children’s cognitive and socioemotional development are relatively consistent. Long-term associations may reflect the stability of early parental responses to NICU interventions and the extent to which parents continue to implement mental health and sensitive parenting techniques in the home. Remaining issues concern the extent to which NICU interventions incorporate sociodemographic differences across families, and whether effective interventions are generalizable or feasible across hospitals. Despite variation across interventions and NICUs; supporting, educating, and partnering with parents is crucial to strengthen longer-term family functioning and alter the developmental trajectories of high-risk infants.
Acknowledgments
Dr. Rogers is funded by the National Institutes of Health NICHD K23 MH105179 and KL2 TR000450, and The Doris Duke Charitable Foundation.
Footnotes
Compliance with Ethics Guidelines
Conflicts of Interest
The authors have no commercial or financial conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Contributor Information
Rachel E. Lean, Department of Psychiatry, Washington University School of Medicine, 660 South Euclid Avenue, Campus Box 8504, St. Louis, MO 63110, USA.
Cynthia E. Rogers, Department of Pediatrics and Psychiatry, Washington University School of Medicine, 660 South Euclid Avenue, Campus Box 8504, St. Louis, MO 63110, USA. Phone: 314-286-0540.
Rachel A. Paul, Department of Obstetrics and Gynecology, Washington University School of Medicine, 660 South Euclid Avenue, Campus Box 8219, St. Louis, MO 63110, USA. Phone: 314-747-8176.
Emily D. Gerstein, Department of Psychological Sciences, University of Missouri- St. Louis, 1 University Blvd, St. Louis, MO 63118, USA. Phone 314-516-5398.
References and Recommended Reading
Papers of particular interest, recently published, have been highlighted as:
* Of importance
** Of major importance
- 1.Harrison W, Goodman D. Epidemiologic trends in neonatal intensive care, 2007–2012. JAMA Pediatr. 2015;169:855–62. doi: 10.1001/jamapediatrics.2015.1305. [DOI] [PubMed] [Google Scholar]
- 2.Hall SL, Phillips R, Hynan MT. Transforming NICU care to provide comprehensive family support. Newborn Infant Nurs Rev. 2016;16:69–73. [Google Scholar]
- 3.Samra HA, McGrath JM, Fischer S, Schumacher B, Dutcher J, Hansen J. The NICU Parent Risk Evaluation and Engagement Model and Instrument (PREEMI) for neonates in intensive care units. J Obstet Gynecol Neonatal Nurs. 2015;44:114–26. doi: 10.1111/1552-6909.12535. [DOI] [PubMed] [Google Scholar]
- 4*.Greene MM, Rossman B, Patra K, Kratovil AL, Janes JE, Meier PP. Depressive, anxious and perinatal post-traumatic distress in mothers of very low birth weight Infants in the NICU. J Dev Behav Pediatr. 2015;36:362–70. doi: 10.1097/DBP.0000000000000174. This study highlights the importance of embedding psychological screening and trauma-focused care in the NICU. Maternal PTSD symptoms remained relatively stable throughout the NICU stay, and were predicted by maternal psychological and obstetric history and the clinical characteristics of the hospitalized infant. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Latendresse G, Wong B, Dyer J, Wilson B, Baksh L, Houge C. Duration of maternal stress and depression: Predictors of newborn admission to neonatal intensive care unit and postpartum depression. Nurs Res. 2015;64:331–41. doi: 10.1097/NNR.0000000000000117. [DOI] [PubMed] [Google Scholar]
- 6.Lefkowitz DS, Baxt C, Evans JR. Prevalence and correlates of posttraumatic stress and postpartum depression in parents of infants in the Neonatal Intensive Care Unit (NICU) J Clin Psychol Med Settings. 2010;17:230–7. doi: 10.1007/s10880-010-9202-7. [DOI] [PubMed] [Google Scholar]
- 7*.Vasa R, Eldeirawi K, Kuriakose VG, G JN, Newsom C, Bates J. Postpartum depression in mothers of infants in neonatal intensive care unit: Risk factors and management strategies. Am J Perinatol. 2014;31:425–34. doi: 10.1055/s-0033-1352482. This study assessed incidence, predictors, and management strategies of postpartum depression in the NICU. Approximately 20% of mothers reported elevated postpartum depressive symptoms, reiterating the need for psychiatric screening upon infant admission to the NICU. Key predictors of postpartum depression included prenatal depression, delivery complications, and infant hospitalization longer than 2-weeks. [DOI] [PubMed] [Google Scholar]
- 8.Rogers CE, Kidokoro H, Wallendorf M, Inder TE. Identifying mothers of very preterm infants at-risk for postpartum depression and anxiety before discharge. J Perinatol. 2013;33:171–6. doi: 10.1038/jp.2012.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tahirkheli NN, Cherry AS, Tackett AP, McCaffree MA, Gillaspy SR. Postpartum depression on the neonatal intensive care unit: Current perspectives. Int J Womens Health. 2014;6:975–87. doi: 10.2147/IJWH.S54666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dubber S, Reck C, Müller M, Gawlik S. Postpartum bonding: The role of perinatal depression, anxiety and maternal–fetal bonding during pregnancy. Arch Womens Ment Health. 2015;18:187–95. doi: 10.1007/s00737-014-0445-4. [DOI] [PubMed] [Google Scholar]
- 11.Woodward LJ, Bora S, Clark CAC, Montgomery-Hönger A, Pritchard VE, Spencer C, et al. Vey preterm birth: Maternal experiences of the neonatal intensive care environment. J Perinatol. 2014;34:555–61. doi: 10.1038/jp.2014.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baía I, Amorim M, Silva S, Kelly-Irving M, de Freitas C, Alves E. Parenting very preterm infants and stress in Neonatal Intensive Care Units. Early Hum Dev. 2016;101:3–9. doi: 10.1016/j.earlhumdev.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 13.Sawyer A, Ayers S, Bertullies S, Thomas M, Weeks AD, Yoxall CW, et al. Providing immediate neonatal care and resuscitation at birth beside the mother: Parents’ views, a qualitative study. BMJ Open. 2015;5:e008495. doi: 10.1136/bmjopen-2015-008495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alkozei A, McMahon E, Lahav A. Stress levels and depressive symptoms in NICU mothers in the early postpartum period. J Matern Fetal Neonatal Med. 2014;27:1738–43. doi: 10.3109/14767058.2014.942626. [DOI] [PubMed] [Google Scholar]
- 15.Pritchard VE, Montgomery-Hönger A. A comparison of parent and staff perceptions of setting-specific and everyday stressors encountered by parents with very preterm infants experiencing neonatal intensive care. Early Hum Dev. 2014;90:549–55. doi: 10.1016/j.earlhumdev.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 16*.Miller GE, Culhane J, Grobman W, Simhan H, Williamson DE, Adam EK, et al. Mothers’ childhood hardship forecasts adverse pregnancy outcomes: Role of inflammatory, lifestyle, and psychosocial pathways. Brain Behav Immun. 2017;65:11–9. doi: 10.1016/j.bbi.2017.04.018. This study suggests that mothers exposed to lifetime socioeconomic hardships are predisposed to deliver prematurely and have an infant admitted to a special care unit. Links between lifetime socioeconomic hardship and adverse birth outcomes were mediated by low education, inflammation during pregnancy, and obstetric complications. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lindquist A, Kurinczuk JJ, Redshaw M, Knight M. Experiences, utilisation and outcomes of maternity care in England among women from different socio-economic groups: Findings from the 2010 National Maternity Survey. BJOG. 2015;122:1610–7. doi: 10.1111/1471-0528.13059. [DOI] [PubMed] [Google Scholar]
- 18.Brumberg HL, Shah SI. Born early and born poor: An eco-bio-developmental model for poverty and preterm birth. J Neonatal-Perinat Med. 2015;8:179–87. doi: 10.3233/NPM-15814098. [DOI] [PubMed] [Google Scholar]
- 19.Greene MM, Rossman B, Patra K, Kratovil A, Khan S, Meier PP. Maternal psychological distress and visitation to the neonatal intensive care unit. Acta Paediatr. 2015;104:e306–13. doi: 10.1111/apa.12975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gooding JS, Cooper LG, Blaine AI, Franck LS, Howse JL, Berns SD. Family Support and Family-Centered Care in the neonatal intensive care unit: Origins, advances, impact. Semin Perinatol. 2011;35:20–8. doi: 10.1053/j.semperi.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 21.Cooper LG, Gooding JS, Gallagher J, Sternesky L, Ledsky R, Berns SD. Impact of a family-centered care initiative on NICU care, staff and families. J Perinatol. 2007;27:S32–7. doi: 10.1038/sj.jp.7211840. [DOI] [PubMed] [Google Scholar]
- 22.Roué J-M, Kuhn P, Lopez Maestro M, Maastrup RA, Mitanchez D, Westrup B, et al. Eight principles for patient-centered and family-centered care for newborns in the neonatal intensive care unit. Arch Dis Child - Fetal Neonatal Ed. 2017;102:F364–8. doi: 10.1136/archdischild-2016-312180. [DOI] [PubMed] [Google Scholar]
- 23.Ramezani T, Shirazi ZH, Sarvestani RS, Moattari M. Family-centered care in neonatal intensive care unit: A concept analysis. Int J Community Based Nurs Midwifery. 2014;2:268. [PMC free article] [PubMed] [Google Scholar]
- 24.O’Brien K, Bracht M, Robson K, Ye XY, Mirea L, Cruz M, et al. Evaluation of the Family Integrated Care model of neonatal intensive care: A cluster randomized controlled trial in Canada and Australia. BMC Pediatr. 2015;15:210. doi: 10.1186/s12887-015-0527-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Altimier L. Compassionate Family Care Framework: A new collaborative compassionate care model for NICU families and caregivers. Newborn Infant Nurs Rev. 2015;15:33–41. [Google Scholar]
- 26.Altimier L, Phillips R. The Neonatal Integrative Developmental Care Model: Advanced clinical applications of the seven core measures for neuroprotective family-centered developmental care. Newborn Infant Nurs Rev. 2016;16:230–44. [Google Scholar]
- 27.Heydarpour S, Keshavarz Z, Bakhtiari M. Factors affecting adaptation to the role of motherhood in mothers of preterm infants admitted to the neonatal intensive care unit: A qualitative study. J Adv Nurs. 2017;73:138–48. doi: 10.1111/jan.13099. [DOI] [PubMed] [Google Scholar]
- 28.Meredith JL, Jnah A, Newberry D. The NICU Environment: Infusing single-family room benefits into the open-bay setting. Neonatal Netw. 2017;36:69–76. doi: 10.1891/0730-0832.36.2.69. [DOI] [PubMed] [Google Scholar]
- 29.Shahheidari M, Homer C. Impact of the design of neonatal intensive care units on neonates, staff, and families: A systematic literature review. J Perinat Neonatal Nurs. 2012;26:260–266. doi: 10.1097/JPN.0b013e318261ca1d. [DOI] [PubMed] [Google Scholar]
- 30*.Lester BM, Hawes K, Abar B, Sullivan M, Miller R, Bigsby R, et al. Single-family room care and neurobehavioral and medical outcomes in preterm infants. PEDIATRICS. 2014;134:754–60. doi: 10.1542/peds.2013-4252. Findings from this study suggest that infants cared for in single family rooms have improved infant clinical and neurobehavioral outcomes by hospital discharge. Links between NICU room type and infant outcomes were mediated by greater maternal involvement and developmental support for infants, highlighting single parent rooms as a setting that fosters active parental caregiving in the NICU. [DOI] [PubMed] [Google Scholar]
- 31.Pineda RG, Stransky KE, Rogers C, Duncan MH, Smith GC, Neil J, et al. The single-patient room in the NICU: Maternal and family effects. J Perinatol. 2012;32:545–51. doi: 10.1038/jp.2011.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Griffin T. A family-centered “visitation” policy in the neonatal intensive care unit that welcomes parents as partners. J Perinatol Neonatal Nurs. 2013;27:160–5. doi: 10.1097/JPN.0b013e3182907f26. [DOI] [PubMed] [Google Scholar]
- 33.Lee LA, Carter M, Stevenson SB, Harrison HA. Improving family-centered care practices in the NICU. Neonatal Netw. 2014;33:125–32. doi: 10.1891/0730-0832.33.3.125. [DOI] [PubMed] [Google Scholar]
- 34.Craig JW, Glick C, Phillips R, Hall SL, Smith J, Browne J. Recommendations for involving the family in developmental care of the NICU baby. J Perinatol. 2015;35:S5–8. doi: 10.1038/jp.2015.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harris GM. Family-Centered Rounds in the Neonatal Intensive Care Unit. Nurs Womens Health. 2014;18:18–27. doi: 10.1111/1751-486X.12090. [DOI] [PubMed] [Google Scholar]
- 36.Enke C, Oliva y Hausmann A, Miedaner F, Roth B, Woopen C. Communicating with parents in neonatal intensive care units: The impact on parental stress. Patient Educ Couns. 2017;100:710–9. doi: 10.1016/j.pec.2016.11.017. [DOI] [PubMed] [Google Scholar]
- 37**.Grzyb MJ, Coo H, Rühland L, Dow K. Views of parents and health-care providers regarding parental presence at bedside rounds in a neonatal intensive care unit. J Perinatol. 2014;34:143–8. doi: 10.1038/jp.2013.144. This study suggests that parental presence at the infant’s bedside during clinical rounds is an effective strategy that can be used to partner with parents in the NICU. Parents who attended clinical rounds reported reduced anxiety and increased confidence in the healthcare team. [DOI] [PubMed] [Google Scholar]
- 38.Howard MB, Schiff DM, Penwill N, Si W, Rai A, Wolfgang T, et al. Impact of parental presence at infants’ bedside on Neonatal Abstinence Syndrome. Hosp Pediatr. 2017;7:63–9. doi: 10.1542/hpeds.2016-0147. [DOI] [PubMed] [Google Scholar]
- 39.Friedman SH, Kessler A, Yang SN, Parsons S, Friedman H, Martin RJ. Delivering perinatal psychiatric services in the neonatal intensive care unit. Acta Paediatr. 2013;102:e392–7. doi: 10.1111/apa.12323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kantrowitz-Gordon I. Expanded care for women and families after preterm birth. J Midwifery Womens Health. 2013;58:158–66. doi: 10.1111/j.1542-2011.2012.00242.x. [DOI] [PubMed] [Google Scholar]
- 41.Hynan MT, Steinberg Z, Baker L, Cicco R, Geller PA, Lassen S, et al. Recommendations for mental health professionals in the NICU. J Perinatol. 2015;35:S14–8. doi: 10.1038/jp.2015.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Melnyk BM, Feinstein NF, Alpert-Gillis L, Fairbanks E, Crean HF, Sinkin RA, et al. Reducing premature infants’ length of stay and improving parents’ mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: A randomized, controlled trial. PEDIATRICS. 2006;118:e1414–1427. doi: 10.1542/peds.2005-2580. [DOI] [PubMed] [Google Scholar]
- 43.Cano Giménez E, Sánchez-Luna M. Providing parents with individualised support in a neonatal intensive care unit reduced stress, anxiety and depression. Acta Paediatr. 2015;104:e300–5. doi: 10.1111/apa.12984. [DOI] [PubMed] [Google Scholar]
- 44.Mendelson T, Cluxton-Keller F, Vullo GC, Tandon SD, Noazin S. NICU-based interventions to reduce maternal depressive and anxiety symptoms: A meta-analysis. PEDIATRICS. 2017;139:e20161870. doi: 10.1542/peds.2016-1870. [DOI] [PubMed] [Google Scholar]
- 45.Gamble J, Creedy DK. A counselling model for postpartum women after distressing birth experiences. Midwifery. 2009;25:e21–30. doi: 10.1016/j.midw.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 46**.Shaw RJ, John NS, Lilo EA, Jo B, Benitz W, Stevenson DK, et al. Prevention of traumatic stress in mothers With preterm infants: A randomized controlled trial. PEDIATRICS. 2013;132:e886–94. doi: 10.1542/peds.2013-1331. This study indicates that providing trauma-focused care in the NICU important to reduce maternal PTSD and depressive symptoms following birth trauma and infant hospitalization. This intervention had high maternal satisfaction ratings and was particularly effective among mothers with high NICU stress levels pre-intervention. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hall SL, Ryan DJ, Beatty J, Grubbs L. Recommendations for peer-to-peer support for NICU parents. J Perinatol. 2015;35:S9–13. doi: 10.1038/jp.2015.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nugent KJ. The Newborn Behavioural Observation (NBO) System as a form of intervention and support for new parents. ZERO TO THREE Journal. 2015;36:2–10. [Google Scholar]
- 49.Als H, McAnulty GB. The Newborn Individualized Developmental Care and Assessment Program (NIDCAP) with Kangaroo Mother Care (KMC): Comprehensive care for preterm infants. Curr Womens Health Rev. 2011;7:288–301. doi: 10.2174/157340411796355216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Welch MG, Hofer MA, Brunelli SA, Stark RI, Andrews HF, Austin J, et al. Family Nurture Intervention (FNI): Methods and treatment protocol of a randomized controlled trial in the NICU. BMC Pediatr. 2012;12:14–30. doi: 10.1186/1471-2431-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.O’Brien K, Bracht M, Macdonell K, McBride T, Robson K, O’Leary L, et al. A pilot cohort analytic study of Family Integrated Care in a Canadian neonatal intensive care unit. BMC Pregnancy Childbirth. 2013;13:S12–19. doi: 10.1186/1471-2393-13-S1-S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lean RE, Smyser CD, Rogers CE. Assessment: The newborn. Child Adolesc Psychiatr Clin N Am. 2017;26:427–40. doi: 10.1016/j.chc.2017.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Macho P. Individualized developmental care in the NICU: A concept analysis. Adv Neonatal Care. 2017;17:162–74. doi: 10.1097/ANC.0000000000000374. [DOI] [PubMed] [Google Scholar]
- 54.Als H, Duffy FH, McAnulty GB, Rivkin MJ, Vajapeyam S, Mulkern RV, et al. Early experience alters brain function and structure. PEDIATRICS. 2004;113:846–57. doi: 10.1542/peds.113.4.846. [DOI] [PubMed] [Google Scholar]
- 55.Sanders LW, Buckner EB. The Newborn Behavioral Observations System as a nursing intervention to enhance engagement in first-time mothers: Feasibility and desirability. Pediatr Nurs. 2006;32:455–9. [PubMed] [Google Scholar]
- 56*.Cho E-S, Kim S-J, Kwon MS, Cho H, Kim EH, Jun EM, et al. The effects of Kangaroo Care in the neonatal intensive care unit on the physiological functions of preterm infants, maternal-infant attachment, and maternal stress. J Pediatr Nurs. 2016;31:430–8. doi: 10.1016/j.pedn.2016.02.007. The findings of this quasi-experimental study suggest that skin-to-skin care has positive effects on infant physiological functions, mother-infant bonding, and maternal stress levels. Thus, skin-to-skin care should be implemented often and consistently in the NICU to support parental and infant wellbeing and the development of the parent-infant relationship. [DOI] [PubMed] [Google Scholar]
- 57.Feldman R, Eidelman AI, Sirota L, Weller A. Comparison of skin-to-skin (kangaroo) and traditional care: Parenting outcomes and preterm infant development. PEDIATRICS. 2002;110:16–26. doi: 10.1542/peds.110.1.16. [DOI] [PubMed] [Google Scholar]
- 58.Newnham CA, Milgrom J, Skouteris H. Effectiveness of a Modified Mother–Infant Transaction Program on outcomes for preterm infants from 3 to 24 months of age. Infant Behav Dev. 2009;32:17–26. doi: 10.1016/j.infbeh.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 59*.Hane AA, Myers MM, Hofer MA, Ludwig RJ, Halperin MS, Austin J, et al. Family Nurture Intervention improves the quality of maternal caregiving in the neonatal intensive care unit: Evidence from a randomized controlled trial. J Dev Behav Pediatr. 2015;36:188–96. doi: 10.1097/DBP.0000000000000148. This RCT suggests that nurture-based interventions should be included in NICU care to foster bonding and emotional closeness between mothers and their infants. After covariate adjustment for infant and maternal factors; the Family Nurture Intervention was associated with higher quality maternal caregiving in the NICU. [DOI] [PubMed] [Google Scholar]
- 60**.Welch MG, Halperin MS, Austin J, Stark RI, Hofer MA, Hane AA, et al. Depression and anxiety symptoms of mothers of preterm infants are decreased at 4 months corrected age with Family Nurture Intervention in the NICU. Arch Womens Ment Health. 2016;19:51–61. doi: 10.1007/s00737-015-0502-7. Dyadic co-regulation interventions support maternal mental wellbeing after NICU discharge. Study findings showed that mothers who completed the Family Nurture Intervention had reduced depression and anxiety at 4-months post-intervention compared to mothers who received standard care. [DOI] [PubMed] [Google Scholar]
- 61*.Vittner D, McGrath J, Robinson J, Lawhon G, Cusson R, Eisenfeld L, et al. Increase in oxytocin from skin-to-skin contact enhances development of parent-infant relationship. Biol Res Nurs. 2017 doi: 10.1177/1099800417735633. E-Pub ahead of print. This study provides a biological mechanism associating skin-to-skin care with parental mental wellbeing and the parent-infant relationship. Results showed that skin-to-skin care activated salivary oxytocin release in mothers, fathers and infants; and decreased salivary cortisol levels in infants. Parents with higher salivary oxytocin release reported lower anxiety scores, and exhibited higher levels of parent-infant synchrony and responsiveness during interactions. [DOI] [PubMed] [Google Scholar]
- 62**.Samra HA, Dutcher J, McGrath JM, Foster M, Klein L, Djira G, et al. Effect of skin-to-skin holding on stress in mothers of late-preterm infants: A randomized trial. Adv Neonatal Care. 2015;15:354–64. doi: 10.1097/ANC.0000000000000223. This study linked greater hours of skin-to-skin/kangaroo care performed in the NICU with higher maternal stress levels. Findings emphasize the need to consider parental mental health and parenting readiness prior to the initiation of parenting interventions. [DOI] [PubMed] [Google Scholar]
- 63.Hobbs JE, Tschudy MM, Hussey-Gardner B, Jennings JM, Boss RD. “I don’t know what I was expecting”: Home visits by neonatology fellows for infants discharged from the NICU. Birth Issues Perinat Care. 2017 doi: 10.1111/birt.12301. E-Pub ahead of print. [DOI] [PubMed] [Google Scholar]
- 64.Purdy IB, Craig JW, Zeanah P. NICU discharge planning and beyond: Recommendations for parent psychosocial support. J Perinatol. 2015;35:S24–28. doi: 10.1038/jp.2015.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ingram J, Blair PS, Powell JE, Manns S, Burden H, Pontin D, et al. Preparing for Home: A before-and-after study to investigate the effects of a neonatal discharge package aimed at increasing parental knowledge, understanding and confidence in caring for their preterm infant before and after discharge from hospital. Southhampton: NIHR Journals Library; 2016. [PubMed] [Google Scholar]
- 66.Aagaard H, Uhrenfeldt L, Spliid M, Fegran L. Parents’ experiences of transition when their infants are discharged from the Neonatal Intensive Care Unit: A systematic review protocol. JBI Database Syst Rev Implement Rep. 2015;13:123–32. doi: 10.11124/jbisrir-2015-2287. [DOI] [PubMed] [Google Scholar]
- 67.Broedsgaard A, Wagner L. How to facilitate parents and their premature infant for the transition home. Int Nurs Rev. 2005;52:196–203. doi: 10.1111/j.1466-7657.2005.00414.x. [DOI] [PubMed] [Google Scholar]
- 68.Ingram JC, Powell JE, Blair PS, Pontin D, Redshaw M, Manns S, et al. Does family-centered neonatal discharge planning reduce healthcare usage? A before and after study in South West England. BMJ Open. 2016;6:e010752. doi: 10.1136/bmjopen-2015-010752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Smith VC, Hwang SS, Dukhovny D, Young S, Pursley DM. Neonatal intensive care unit discharge preparation, family readiness and infant outcomes: Connecting the dots. J Perinatol. 2013;33:415–21. doi: 10.1038/jp.2013.23. [DOI] [PubMed] [Google Scholar]
- 70.Vohr B, McGowan E, Keszler L, O’Donnell M, Hawes K, Tucker R. Effects of a transition home program on preterm infant emergency room visits within 90 days of discharge. J Perinatol. 2017 doi: 10.1038/jp.2017.136. E-pub ahead of print. [DOI] [PubMed] [Google Scholar]
- 71.Raffray M, Semenic S, Osorio Galeano S, Ochoa Marín SC. Barriers and facilitators to preparing families with premature infants for discharge home from the neonatal unit: Perceptions of health care providers. Invest Educ Enferm. 2014;32:379–92. doi: 10.17533/udea.iee.v32n3a03. [DOI] [PubMed] [Google Scholar]
- 72**.McGowan EC, Du N, Hawes K, Tucker R, O’Donnell M, Vohr B. Maternal mental health and neonatal intensive care unit discharge readiness in mothers of preterm infants. J Pediatr. 2017;184:68–74. doi: 10.1016/j.jpeds.2017.01.052. Mothers with perinatal mental health disorders may need additional and/or targeted support in the NICU. Specifically, mothers with mental health disorders perceived themselves as having poor emotional readiness and reduced support for NICU discharge. In addition, these mothers did not view their infant as being ready to leave the NICU environment, suggesting that they were unprepared to independently parent a high-risk infant. [DOI] [PubMed] [Google Scholar]
- 73**.Hawes K, McGowan E, O’Donnell M, Tucker R, Vohr B. Social emotional factors increase risk of postpartum depression in mothers of preterm infants. J Pediatr. 2016;179:61–7. doi: 10.1016/j.jpeds.2016.07.008. Perinatal mental health assessment is essential to identify women at risk of postpartum depression and to provide timely referrals to community-based services prior to NICU discharge. Mothers who had a history of poor mental health and who reported negative perceptions of herself and her infant prior during the NICU stay were more likely to have elevated depressive symptoms by 1-month postpartum. [DOI] [PubMed] [Google Scholar]
- 74.Holditch-Davis D, White-Traut RC, Levy JA, O’Shea TM, Geraldo V, David RJ. Maternally administered interventions for preterm infants in the NICU: Effects on maternal psychological distress and mother-infant relationship. Infant Behav Dev. 2014;37:695–710. doi: 10.1016/j.infbeh.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75**.Shaw RJ, St John N, Lilo E, Jo B, Benitz W, Stevenson DK, et al. Prevention of traumatic stress in mothers of preterms: 6-month outcomes. PEDIATRICS. 2014;134:e481–488. doi: 10.1542/peds.2014-0529. Findings of this study demonstrate the efficacy of a trauma-focused cognitive behavioral therapy intervention on PTSD, anxiety, and depressive symptoms. Significant intervention effects were reported for PTSD, anxiety, and depression outcomes at both the 1-month and 6-month follow-up assessments, with effect sizes becoming more prominent at 6-months post-intervention. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Glazebrook C, Marlow N, Israel C, Croudace T, Johnson S, White IR, et al. Randomised trial of a parenting intervention during neonatal intensive care. Arch Dis Child Fetal Neonatal Ed. 2007;92:F438–443. doi: 10.1136/adc.2006.103135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tessier R, Cristo M, Velez S, Giron M, de Calume ZF, Ruiz-Palaez JG, et al. Kangaroo mother care and the bonding hypothesis. PEDIATRICS. 1998;102:e17. doi: 10.1542/peds.102.2.e17. [DOI] [PubMed] [Google Scholar]
- 78.Feldman R. Mutual influences between child emotion regulation and parent–child reciprocity support development across the first 10 years of life: Implications for developmental psychopathology. Dev Psychopathol. 2015;27:1007–23. doi: 10.1017/S0954579415000656. [DOI] [PubMed] [Google Scholar]
- 79.Feldman R, Eidelman AI. Skin-to-skin contact (Kangaroo Care) accelerates autonomic and neurobehavioural maturation in preterm infants. Dev Med Child Neurol. 2003;45:274–81. doi: 10.1017/s0012162203000525. [DOI] [PubMed] [Google Scholar]
- 80.Ahlqvist-Björkroth S, Boukydis Z, Axelin AM, Lehtonen L. Close Collaboration with Parents™ intervention to improve parents’ psychological well-being and child development: Description of the intervention and study protocol. Behav Brain Res. 2017;15:303–10. doi: 10.1016/j.bbr.2016.10.020. [DOI] [PubMed] [Google Scholar]
- 81.Stefana A, Lavelli M. Parental engagement and early interactions with preterm infants during the stay in the neonatal intensive care unit: Protocol of a mixed-method and longitudinal study. BMJ Open. 2017;7:e013824. doi: 10.1136/bmjopen-2016-013824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ohlsson A, Jacobs SE. NIDCAP: A systematic review and meta-analyses of randomized controlled trials. PEDIATRICS. 2013;131:e881–93. doi: 10.1542/peds.2012-2121. [DOI] [PubMed] [Google Scholar]
- 83.Hughes AJ, Redsell SA, Glazebrook C. Motor development interventions for preterm infants: A systematic review and meta-analysis. PEDIATRICS. 2016;138:e20160147. doi: 10.1542/peds.2016-0147. [DOI] [PubMed] [Google Scholar]
- 84.Myers MM, Grieve PG, Stark RI, Isler JR, Hofer MA, Yang J, et al. Family Nurture Intervention in preterm infants alters frontal cortical functional connectivity assessed by EEG coherence. Acta Paediatr. 2015;104:670–7. doi: 10.1111/apa.13007. [DOI] [PubMed] [Google Scholar]
- 85*.Pineda RG, Neil J, Dierker D, Smyser CD, Wallendorf M, Kidokoro H, et al. Alterations in brain structure and neurodevelopmental outcome in preterm infants hospitalized in different neonatal intensive care unit environments. J Pediatr. 2014;164:52–60. doi: 10.1016/j.jpeds.2013.08.047. This study raises concerns for the potential adverse effects of infant sensory deprivation in single family NICU rooms among urban samples with low visitation rates. At age 2 years, infants placed in single family rooms obtained lower language and motor scores than infants in open-bay rooms at follow-up. Findings persisted after covariate adjustment for clinical, social, and family factors. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Milgrom J, Newnham C, Anderson PJ, Doyle LW, Gemmill AW, Lee K, et al. Early sensitivity training for parents of preterm infants: Impact on the developing brain. Pediatr Res. 2010;67:330–5. doi: 10.1203/PDR.0b013e3181cb8e2f. [DOI] [PubMed] [Google Scholar]
- 87.McAnulty G, Duffy FH, Kosta S, Weisenfeld NI, Warfield SK, Butler SC, et al. School age effects of the Newborn Individualized Developmental Care and Assessment Program for medically low-risk preterm infants: Preliminary findings. J Clin Neonatol. 2012;1:184. doi: 10.4103/2249-4847.105982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88*.McAnulty G, Duffy FH, Kosta S, Weisenfeld NI, Warfield SK, Butler SC, et al. School age effects of the newborn individualized developmental care and assessment program for preterm infants with intrauterine growth restriction: Preliminary findings. BMC Pediatr. 2013;13:25. doi: 10.1186/1471-2431-13-25. This study provides evidence for long-term associations between the NIDCAP intervention and cerebral structural and functional outcomes at age 9 years. While NIDCAP and control subjects did not differ on measures of cognition or academic achievement, evidence was found for group-differences in executive function. However, replication of results with larger samples is needed to support these findings. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89**.Lester BM, Salisbury AL, Hawes K, Dansereau LM, Bigsby R, Laptook A, et al. 18-Month follow-up of infants cared for in a single-family room neonatal intensive care unit. J Pediatr. 2016;177:84–9. doi: 10.1016/j.jpeds.2016.06.069. Findings from this study suggest that infants cared for in single family rooms had improved cognitive and language outcomes in early childhood compared to infants cared for in an open-bay NICU. Links between single family rooms and neurobehavioral outcome were attributable to enhanced maternal involvement and caregiving in single family room settings. [DOI] [PubMed] [Google Scholar]
- 90.Vohr B, McGowan E, McKinley L, Tucker R, Keszler L, Alksninis B. Differential effects of the single-family room neonatal intensive care unit on 18- to 24-month Bayley scores of preterm infants. J Pediatr. 2017;185:42–48. doi: 10.1016/j.jpeds.2017.01.056. [DOI] [PubMed] [Google Scholar]
- 91.Gonya J, Ray WC, Rumpf RW, Brock G. Investigating skin-to-skin care patterns with extremely preterm infants in the NICU and their effect on early cognitive and communication performance: a retrospective cohort study. BMJ Open. 2017;7:e012985. doi: 10.1136/bmjopen-2016-012985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Royston P, Altman DG, Sauerbrei W. Dichotomizing continuous predictors in multiple regression: A bad idea. Stat Med. 2006;25:127–41. doi: 10.1002/sim.2331. [DOI] [PubMed] [Google Scholar]
- 93**.Welch MG, Firestein MR, Austin J, Hane AA, Stark RI, Hofer MA, et al. Family Nurture Intervention in the neonatal intensive care unit improves social-relatedness, attention, and neurodevelopment of preterm infants at 18 months in a randomized controlled trial. J Child Psychol Psychiatry. 2015;56:1202–11. doi: 10.1111/jcpp.12405. Findings showed that preterm infants who were exposed to the Family Nurture Intervention in the NICU demonstrated improved cognitive, language, social-relatedness, and attention outcomes at follow-up. Thus, the Family Nurture intervention supports infant socio-emotional development through its effects on maternal bonding and emotional closeness in the NICU. [DOI] [PubMed] [Google Scholar]
- 94.Melnyk BM, Alpert-Gillis L, Feinstein NF, Fairbanks E, Schultz-Czarniak J, Hust D, et al. Improving cognitive development of low-birth-weight premature infants with the COPE program: A pilot study of the benefit of early NICU intervention with mothers. Res Nurs Health. 2001;24:373–89. doi: 10.1002/nur.1038. [DOI] [PubMed] [Google Scholar]
- 95.Montirosso R, Giusti L, De Carli P, Tronick E, Borgatti R. Developmental care, neonatal behavior and postnatal maternal depressive symptomatology predict internalizing problems at 18 months for very preterm children. J Perinatol. 2017;00:1–5. doi: 10.1038/jp.2017.148. [DOI] [PubMed] [Google Scholar]
- 96.Gerstein ED, Poehlmann-Tynan J, Clark R. Mother-child interactions in the NICU: Relevance and implications for later parenting. J Pediatr Psychol. 2015;40:33–44. doi: 10.1093/jpepsy/jsu064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hall S, Hynan M, Phillips R, Press J, Kenner C, Ryan DJ. Development of program standards for psychosocial support of parents of infants admitted to a neonatal intensive care unit: A national interdisciplinary consensus model. Newborn Infant Nurs Rev. 2015;15:24–7. [Google Scholar]
- 98.Greenfield JC, Klawetter S. Parental leave policy as a strategy to improve outcomes among premature infants. Health Soc Work. 2016;41:17–23. doi: 10.1093/hsw/hlv079. [DOI] [PubMed] [Google Scholar]
- 99.Dykes F, Thomson G, Gardner C, Hall Moran V, Flacking R. Perceptions of European medical staff on the facilitators and barriers to physical closeness between parents and infants in neonatal units. Acta Paediatr. 2016;105:1039–46. doi: 10.1111/apa.13417. [DOI] [PMC free article] [PubMed] [Google Scholar]


