Abstract
Complete atrioventricular (AV) block in association with Takotsubo syndrome (TS) has been well recognized, but the cause and effect relationship has not been elucidated. We describe a 78-year-old female who presented with complete AV block but one week later developed new-onset, diffuse T-wave inversions, QT prolongation, and acceleration of junctional escape rate. Left ventriculogram revealed features typical of TS. One year after permanent pacemaker implantation, complete AV block persisted despite the reversal of wall motion defects implying that conduction abnormality was the trigger of TS rather than its consequence.
Keywords: Takotsubo syndrome, Atrioventricular block, Complete heart block, Permanent pacemaker, Takotsubo cardiomyopathy
1. Introduction
Takotsubo syndrome (TS) is a reversible form of acute left ventricular systolic dysfunction with characteristic wall motion abnormalities, mimicking myocardial infarction, but in the absence of angiographic evidence of obstructive coronary artery disease or acute plaque rupture. It is triggered by emotional or physical stress and has a predilection for postmenopausal women. Prognosis is considered to be favorable which may be misleading as arrhythmias in the acute phase can lead to increased mortality [1]. Complete atrioventricular (AV) block in association with TS has been well recognized, but the cause and effect relationship has not been elucidated. Unlike left ventricular (LV) function, whether AV block recovers entirely in TS is not well known. As such, need for a permanent pacemaker in these patients is unclear.
2. Case report
A 78-year-old hypertensive woman was evaluated for complaints of dyspnea, presyncope, and fatigue of one-week duration. She was diagnosed with complete AV block one week back at a different hospital where electrocardiogram (ECG) revealed junctional escape rhythm at 38 bpm, normal corrected QT interval (QTc 442 ms), and upright T waves (Fig. 1A). Transthoracic echocardiogram (TTE) at that time had revealed normal LV function with no regional wall motion abnormality and was advised permanent pacemaker implantation (PPI). At admission to our center, her pulse rate was 55 bpm, blood pressure was 148/66 mm Hg, and arterial oxygen saturation was 97%. ECG at admission revealed complete AV block with an acceleration of junctional escape rate to 54bpm, QTc of 630 ms, and new-onset, diffuse T-wave inversions (Fig. 1B). She was not taking any rate-reducing drug, and her metabolic profile including serum electrolytes, renal function, liver function, and thyroid function tests was normal. Transthoracic echocardiogram (TTE) revealed hypokinesia of left ventricular mid and apical segments with a hyperkinetic base. Her LV function was reduced with an ejection fraction of 30%. Serum troponin-T at admission was 1036 ng/L which lead to the suspicion of acute coronary syndrome. A coronary angiogram was performed which revealed normal epicardial coronaries (Fig. 2A and B). Left ventriculogram showed ballooning of apical and mid segments with a hypercontractile base (Fig. 2C and D). A temporary pacemaker was inserted through the right internal jugular vein, and anti-heart failure treatment was initiated after which she improved clinically. But no recovery of conduction abnormality was noted till seven days. A dual chamber permanent pacemaker was implanted, and TTE repeated after five days showed marked improvement in LV function with ejection fraction of 62%. T-wave inversions and QTc also became normal. At one-year follow-up, ECG with pacing-off (OVO mode) revealed the persistence of complete AV block but with upright T-waves, and a normal QTc (Fig. 2E).
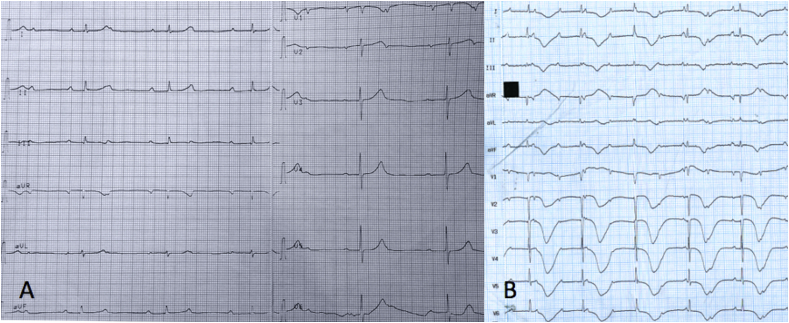
Fig. 1.
A- Electrocardiogram 1 week before admission revealed complete AV block with a junctional escape at 38 bpm, upright T-waves in precordial leads, and a corrected QT interval of 442 ms. B- Electrocardiogram at admission to our center showed complete AV block with new-onset, diffuse T-wave inversions, and a corrected QT interval of 630 ms. Note the acceleration of junctional escape rate to 54 bpm, presumably due to exaggerated sympathetic activation.
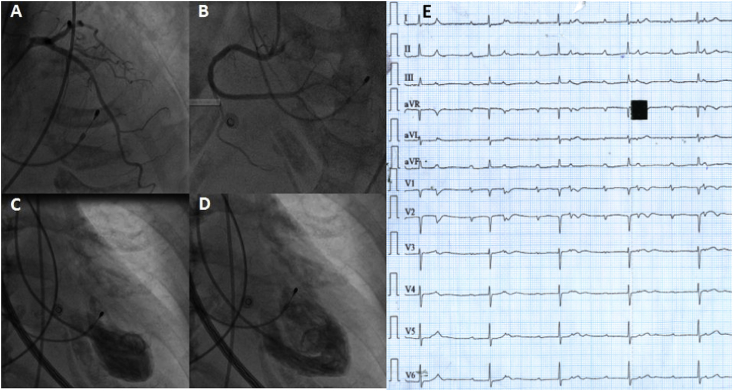
Fig. 2.
Left (A) and right (B) coronary angiograms revealed normal epicardial coronaries. Left ventriculogram in systole (C) and diastole (D) showed apical ballooning with basal hyperkinesis. Electrocardiogram at 1-year follow-up (E) with pacing-off (OVO mode) revealed the persistence of complete AV block with reversal of T-wave changes and normalization of QT interval. Note the slowing of escape rate to 42 bpm, suggesting the regression of sympathetic overactivity.
3. Discussion
Takotsubo syndrome is a reversible form of acute heart failure, initially described in Japan, but subsequently has been reported globally. Up to 10% of cases occur in young individuals [2]. In TS, myocardial stunning commonly occurs at the apex and mid portion of the left ventricle with a hypercontractile base. Exaggerated sympathetic activation secondary to emotional or physical stress is the underlying factor responsible for these typical wall motion abnormalities. However, the pathophysiology of arrhythmias in this condition is unclear. Most cases of complete AV block associated with TS have been described in elderly individuals, an age in which degenerative conduction system disease is also common [3]. Majority of reported cases had both complete AV block and TS at initial presentation, and the chronological sequence was not apparent. Nef et al. first reported complete AV block in a 58-year-old patient which necessitated a PPI [4]. However, after three months, conduction abnormality had partially recovered, and the patient had first degree AV block only. Le et al. reported a 73-year-old woman with complete AV block and TS at presentation which necessitated a permanent pacemaker [3]. At 1-month follow-up, complete AV block persisted despite the recovery of left ventricular function. Benouda et al. reported a 69-year-old lady with 2:1 AV block associated with TS which persisted at two years follow-up and required PPI [5]. In a large series of patients with TS, Stiermaier et al. reported that complete AV block occurred in 3% of patients [6]. Patients who underwent PPI continued to be in complete AV block on long-term follow-up. Patients who had complete AV block or ventricular asystole as initial rhythm at presentation but did not undergo pacemaker implantation had sudden deaths on follow-up. Our case is unique since we could document the temporal relationship between the rhythm disturbance and the subsequent TS. The occurrence of new-onset T-wave inversions, QT prolongation, and acceleration of junctional escape rate concurrent with typical wall motion abnormalities implied the onset of TS which resolved after two weeks. Our case, therefore, supports the hypothesis that the stress of complete AV block was the cause of TS rather than the effect. Implantation of a permanent pacemaker, therefore, is the appropriate strategy in such patients. The choice of pacemaker (dual chamber versus biventricular) in patients with impaired LV function due to TS is not clear. As the LV systolic dysfunction is reversible and spontaneously normalises in most patients with TS, a dual chamber pacemaker may be preferable over a biventricular pacemaker [2]. The precise level of AV block could not be ascertained in our patient since we did not perform an invasive electrophysiological study. However, the narrow QRS escape rhythm, as well as sensitivity of the escape rhythm to fluctuation in sympathetic tone, suggest that the escape rhythm originated above the bifurcation of the His bundle. The occurrence of transient AV block as a consequence of TS is hard to explain as the sympathetic tone is exaggerated in these patients and the affected segment is the LV apex rather than the base. Moreover, the time course of resolution of conduction defects is different from the recovery of LV systolic function suggesting different pathophysiologic mechanisms. Degenerative complete AV block can be intermittent early in its natural history which can explain at least some cases of transient AV block associated with TS. In other patients, a secondary increase in vagal tone or transient microvascular dysfunction has been proposed as the cause of reversible conduction abnormality [6]. Complete AV block triggering TS is probably an under-recognized entity, and the diagnosis of TS should be considered in all patients with complete AV block demonstrating regional wall motion abnormalities.
4. Conclusions
AV conduction defects can rarely be associated with TS. Complete AV block preceding the onset of TS supports the hypothesis that stress of AV block is the trigger rather than the consequence of TS in the majority of cases. Persistence of conduction abnormality on long-term follow-up despite the reversal of wall motion defects, T-wave inversions, and QT prolongation further reinforces this inference. Permanent pacemaker implantation, therefore, is an appropriate decision in such patients.
Funding sources
None.
Conflicts of interest
None.
Footnotes
Peer review under responsibility of Indian Heart Rhythm Society.
References
- 1.Syed F.F., Asirvatham S.J., Francis J. Arrhythmia occurrence with takotsubo cardiomyopathy: a literature review. Europace. 2010;13:780–788. doi: 10.1093/europace/euq435. https://doi.org/10.1093/europace/euq435 [DOI] [PubMed] [Google Scholar]
- 2.Sharkey S.W., Windenburg D.C., Lesser J.R., Maron M.S., Hauser R.G., Lesser J.N. Natural history and expansive clinical profile of stress (tako-tsubo) cardiomyopathy. J Am Coll Cardiol. 2010;55:333–341. doi: 10.1016/j.jacc.2009.08.057. https://doi.org/10.1016/j.jacc.2009.08.057 [DOI] [PubMed] [Google Scholar]
- 3.Le M.T., Grimard C., Varenne O., Jakamy R., Rosencher J. Tako-Tsubo cardiomyopathy and high-degree atrio-ventricular block: do we need to wait left ventricular function recovery to implant a pacemaker ? Int J Cardiol. 2014;176:e56–e59. doi: 10.1016/j.ijcard.2014.07.037. https://doi.org/10.1016/j.ijcard.2014.07.037 [DOI] [PubMed] [Google Scholar]
- 4.Nef H.M., Möllmann H., Sperzel J., Weber M., Brück H., Hamm C.W. Temporary third-degree atrioventricular block in a case of apical ballooning syndrome. Int J Cardiol. 2006;113:E33–E35. doi: 10.1016/j.ijcard.2006.04.007. https://doi.org/10.1016/j.ijcard.2006.04.007 [DOI] [PubMed] [Google Scholar]
- 5.Benouda L., Roule V., Foucault A., Dahdouh Z., Lebon A., Milliez P. Conduction disturbances in Tako Tsubo cardiomyopathy: a cause or a consequence? Int J Cardiol. 2012;159:61–62. doi: 10.1016/j.ijcard.2012.03.164. https://doi.org/10.1016/j.ijcard.2012.03.164 [DOI] [PubMed] [Google Scholar]
- 6.Stiermaier T., Rommel K.P., Eitel C., Möller C., Graf T., Desch S. Management of arrhythmias in patients with Takotsubo cardiomyopathy: is the implantation of permanent devices necessary? Heart Rhythm. 2016;13:1979–1986. doi: 10.1016/j.hrthm.2016.06.013. https://doi.org/10.1016/j.hrthm.2016.06.013 [DOI] [PubMed] [Google Scholar]