Abstract
Physical exercise is beneficial for general health and is an effective treatment for metabolic disorders. Vitamin E is widely used as dietary supplement and is considered to improve non-alcoholic fatty liver disease by reducing inflammation and dyslipidemia. However, increased vitamin E intake may interfere with adaptation to exercise training. Here, we explored how vitamin E alters the acute exercise response of the liver, an organ that plays an essential metabolic role during physical activity. Mice fed a control or an α-tocopherol-enriched diet were subjected to a non-exhaustive treadmill run. We assessed the acute transcriptional response of the liver as well as glucocorticoid signalling and plasma free fatty acids (FFA) and performed indirect calorimetry. Vitamin E interfered with the exercise-induced increase in FFA and upregulation of hepatic metabolic regulators, and it shifted the transcriptional profile of exercised mice towards lipid and cholesterol synthesis while reducing inflammation. Energy utilization, as well as corticosterone levels and signalling were similar, arguing against acute differences in substrate oxidation or glucocorticoid action. Our results show that high-dose vitamin E alters the metabolic and inflammatory response of the liver to physical exercise. The interference with these processes may suggest a cautious use of vitamin E as dietary supplement.
Keywords: liver, exercise, vitamin E, tocopherol, Ppargc1a, inflammation, lipogenesis
1. Introduction
The beneficial effects of exercise make it a powerful means to improve general health and treat conditions such as obesity, non-alcoholic fatty liver disease (NAFLD), insulin resistance, and type 2 diabetes [1,2,3]. Physical exercise is a physiological, yet metabolically demanding, state that involves not only the contracting muscles, but the organism as a whole. The liver, an organ with pleiotropic functions, takes a particularly active role as it provides glucose to compensate for the increased uptake by the muscles [3,4]. This process is supported by a fall in hepatic energy charge as well as increased uptake and oxidation of fatty acids by the liver [3].
Increased mitochondrial substrate oxidation during exercise may result in the production of reactive oxygen species (ROS), a phenomenon that has long been known to occur in skeletal muscle [5]. Concern about the potential negative effects of oxidative stress has contributed to the propagation of antioxidant intake among athletes [5]. However, ROS, while possibly detrimental and even performance-limiting [6], may at the same time be essential signalling molecules which trigger antioxidant defenses and other beneficial long-term effects of exercise [7,8,9]. This hypothesis has been tested in different human and animal studies, frequently employing the vitamin E form α-tocopherol as an antioxidant and predominantly in combination with other antioxidative supplements. In human subjects, these studies have reported an interference with the training-induced improvement in insulin sensitivity [10] and blunted increases in transcriptional regulators of mitochondrial biogenesis and in mitochondrial proteins in skeletal muscle [10,11]. Similar effects of vitamin E have been described in rodents [12].
In addition to its local actions, some of which may be non-antioxidant activities [13], vitamin E could also interact with the endocrine response to physical exercise: It has been shown to reduce plasma corticosterone in stress-exposed rats [14] and to affect glucocorticoid signalling in skeletal muscle [15]. In humans, a combined vitamin E and C supplementation blunted the exercise-induced increase in cortisol [16]. While not all studies have confirmed the negative consequences of vitamin E-containing antioxidant supplements on training adaptation [17,18], a potential negative effect is certainly worth considering in view of the high prevalence of antioxidant supplementation: In a study published in 2005, more than 10% of US adults reported consuming at least 400 IU of vitamin E per day [19].
Similar to skeletal muscle, the liver shows both an acute stress response to physical exercise [20,21] and long-term adaptations to this metabolic challenge. We have previously reported that exercise acutely upregulates genes involved in the immune response and glucose and fatty acid metabolism [20], such as peroxisome proliferative activated receptor gamma coactivator 1 alpha (Ppargc1a), pyruvate dehydrogenase kinase 4 (Pdk4), insulin receptor substrate 2 (Irs2), angiopoietin like 4 (Angptl4) and the carnitine transporter solute carrier family 22 member 5 (Slc22a5), whereas it downregulates fatty acid synthase (Fasn) [22,23]. By increasing mitochondrial fatty acid oxidation and suppressing lipid anabolic processes in the liver, training reduces hepatic fat content and improves NAFLD, even in the absence of weight loss [3,23]. These direct effects on the liver may be a highly relevant mechanism by which physical activity improves general health. In contrast to the important roles of the liver in relation to physical exercise, little attention has been paid to whether its adaptation to exercise is also affected by vitamin E. This is particularly noteworthy as the liver is the main organ involved in the control of vitamin E status [24]. Vitamin E could affect the hepatic response to exercise by exerting local antioxidant or non-antioxidant activities [13], but also by interfering with glucocorticoid signalling [13,14,15], which has been implicated in the upregulation of Ppargc1a [25], Angptl4 [26], Irs2, and Pdk4 [27].
To study how vitamin E interacts with the acute hepatic adaptation to exercise, we fed mice an α-tocopherol-enriched antioxidant diet before subjecting them to a non-exhaustive treadmill run. We investigated the metabolic responses and changes in the liver transcriptome immediately after the bout of exercise. Vitamin E supplementation counteracted the increase in circulating free fatty acids (FFA) and the induction of inflammatory transcripts in the liver. At the same time, genes involved in cholesterol and lipid synthesis, processes that are normally suspended during physical exercise and negatively regulated by fatty acids, were upregulated by exercise combined with vitamin E. These effects appeared not to be related to alterations in glucocorticoid signalling or whole-body energy consumption in exercising mice. By altering the acute response to physical exercise, high doses of vitamin E could interfere with the beneficial long-term adaptation of the liver during regular exercise training.
2. Materials and Methods
2.1. Diets and Exercise Protocol
The animal experiment was performed in accordance with the EU Directive 2010/63/EU and approved by the local authorities (Regierungspräsidium Tübingen). Mice were kept under an inverted light–dark cycle (dark period 9:30–21:30 h, light period 21:30–9:30 h). Experiments were performed between 10:00 and 14:00 h. Seven week-old male C57BL/6N mice were purchased from Charles River (Sulzfeld, Germany) and assigned to either a diet supplemented with 100 mg/kg vitamin C and 2000 IU/kg vitamin E (as α-tocopheryl acetate) or to control diet (0 mg/kg vitamin C, 149 IU/kg vitamin E) based on the purified diet C1000 (Altromin, Lage, Germany). In contrast to humans, mice can synthetize vitamin C. However, a small amount of vitamin C was added to the vitamin E-enriched diet since it is required for vitamin E regeneration [28].
After 4 weeks of feeding, at an age of 11–12 weeks, the animals were weighed and n = 12 mice from each dietary group were subjected to 1 h of treadmill running (13 m/min and 14° uphill slope), as described previously [22]. For a subset (n = 6 per diet) of exercising mice, respirometry was performed during the treadmill run using an indirect calorimetric system (Oxylet, Panlab, Cornellà, Spain). Oxygen consumption and the respiratory quotient (CO2produced/O2consumed) were calculated using Metabolism 2.1.04 Software (Panlab, Cornellà, Spain). Immediately after the exercise bout, mice were analgosedated with an intraperitoneal injection of ketamine and xylazine (150 and 10 mg/kg body weight, respectively), and exsanguinated by decapitation. Blood was transferred into EDTA collectors and livers were removed and frozen in liquid nitrogen. Blood and liver collection was carried out within 5 min of completion of the exercise bout. The control mice (n = 10 per diet) remained in their cages, but in close proximity to the treadmill, and were deprived of food for 60 min before they were killed, to align with the feeding state of the exercised animals.
2.2. Metabolites and Glucocorticoid Receptor Activity
Plasma FFA concentrations were determined using an enzyme-based colorimetric kit (HR Series NEFA-HR(2), Wako Chemicals GmbH, Neuss, Germany) on an automated clinical chemistry analyzer (ADVIA 1650, Siemens Healthcare Diagnostics, Fernwald, Germany). Vitamin E was analyzed on a HPLC with UV detection; sample preparation and analysis were performed using a commercial kit (Vitamins A and E in Serum/Plasma, 34000, Chromsystems, München, Germany) according to the manufacturer’s instructions. Plasma corticosterone was measured by radioimmune assay (Double Antibody Corticosterone 125I RIA Kit for Rats and Mice, 07120103, MP Biomedicals, Santa Ana, CA, USA; coefficients of variation according to manufacturer: intra-assay 4–10% for 56–370 ng/mL, inter-assay 6–7% for 119–469 ng/mL).
Quantification of triglycerides was done by homogenizing frozen liver pieces in 0.9% NaCl containing 1% Triton X-100 (10 µL/mg tissue) using a TissueLyser (Qiagen, Hilden, Germany). Debris was removed by centrifugation (10 min, 16,000 g, room temperature), and triglycerides in the supernatant were quantified on an automated clinical chemistry analyzer using an enzyme-based colorimetric kit (ADVIA Chemistry TRIG_2, Siemens Healthcare Diagnostics). Glucocorticoid receptor DNA binding activity was assessed with the TransAM GR DNA-binding ELISA (45496, Active Motif, Carlsbad, CA, USA) using nuclear extracts prepared from frozen liver tissue using the NE-PER™ Nuclear and Cytoplasmic Extraction Kit (78833, ThermoFisher, Waltham, MA, USA), in accordance with the manufacturers’ instructions.
2.3. RNA Isolation, Quantitative PCR and Transcriptome Analysis
RNA isolation, reverse transcription and quantitative real-time PCR were performed as previously described [22] using QuantiTect Primer Assays (Qiagen, Hilden, Germany). The mRNA content is given in arbitrary units. The non-normalized results shown throughout the manuscript were similar after normalization to β-actin mRNA (not shown).
Transcriptome analysis was done as in [29], with the following differences: we used Mouse Gene 2.1 ST arrays (Affymetrix, Santa Clara, CA, USA) and Expression Console software (v.1.4.1.46, Affymetrix). Array data have been submitted to the GEO database at NCBI (GSE110747).
2.4. Data Analysis
Statistical analysis was performed with JMP 13 (SAS Institute, Cary, NC, USA). Plasma analytes, glucocorticoid activity and weight were compared by Student’s t-tests. mRNA data were compared using the non-parametric Wilcoxon method as they did not fulfill the normality requirement. A p-value < 0.05 was considered significant and p < 0.1 was considered a trend. Data are shown as means ± standard deviation (SD).
Microarray data were analyzed as described [29] with limma t-tests and a p-value < 0.05 as the cut-off. To reduce the background signal, data were filtered for average linear arbitrary expression >4 in at least one group. Transcripts with a limma t-test p-value < 0.05 and median fold change >|1.2| between exercised mice fed the control or the vitamin E diet were subjected to upstream regulator analysis using Ingenuity Pathway Analysis (Qiagen, Redwood City, CA, USA). The upstream regulator types drugs and chemicals were excluded. Open-source MultiExperiment Viewer software [30] was employed for heatmap generation, using autoscaled values.
3. Results
3.1. Vitamin E Interferes with Exercise-Induced Increase in Plasma FFA and Expression of Key Metabolic Regulators in the Liver
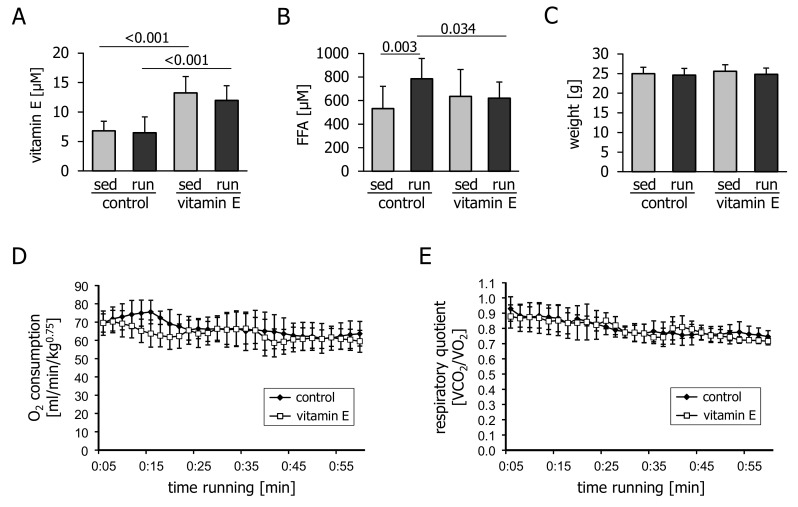
Dietary supplementation of α-tocopherol resulted in an approximately two-fold increase in the concentration of plasma vitamin E that was not changed by the acute treadmill run (Figure 1A). Exercise caused a moderate increase in plasma FFA levels that was blunted by vitamin E supplementation (Figure 1B). Body weight was similar in all groups (Figure 1C). The O2 consumption (Figure 1D) and respiratory quotient (Figure 1E) of running mice were not affected by vitamin E intake, indicating a similar reliance on fatty acids as a metabolic fuel.
Figure 1.
Plasma levels of (A) vitamin E and (B) circulating free fatty acids (FFA) in mice immediately after 1 h of treadmill running (run) or remaining sedentary (sed) and fasting for the same period of time. Prior to the experiment, mice had been fed a control or a vitamin E-enriched diet for four weeks. (C) Body weight, measured before the exercise bout; (D) O2 consumption and (E) respiratory quotient measured during the treadmill run. Values are means ± standard deviation from n = 10 (sedentary groups) or n = 12 (exercised groups) animals (A–C) or from n = 6 mice (D,E).
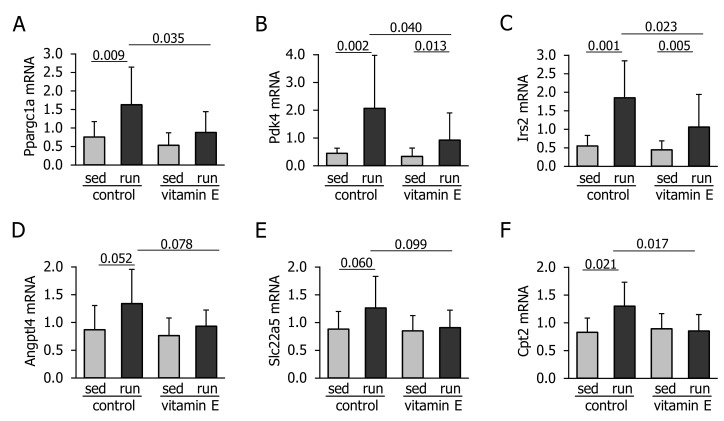
Exercise caused the upregulation of Ppargc1a Pdk4, Irs2, Angptl4, Slc22a5 and carnitine palmitoyltransferase 2 (Cpt2) (Figure 2A–F). Vitamin E significantly reduced the upregulation of Ppargc1a, Pdk4, Irs2 and Cpt2 and tended to lower the mRNA levels of Angptl4 and Slc22a5 (Figure 2A–F).
Figure 2.
Liver mRNA levels of (A) peroxisome proliferative activated receptor gamma coactivator 1 alpha (Ppargc1a), (B) pyruvate dehydrogenase kinase 4 (Pdk4), (C) insulin receptor substrate 2 (Irs2), (D) angiopoietin like 4 (Angptl4), (E) solute carrier family 22 member 5 (Slc22a5), and (F) carnitine palmitoyltransferase 2 (Cpt2) in mice immediately after 1 h of treadmill running (run) or remaining sedentary (sed) and fasting for the same period of time. Prior to the experiment, mice had been fed a control or a vitamin E-enriched diet for four weeks. Values are means ± standard deviation from n = 10 (sedentary groups) or n = 12 (exercised groups) animals in arbitrary units.
3.2. Corticosterone Levels and Glucocorticoid Signalling are not Affected by Vitamin E
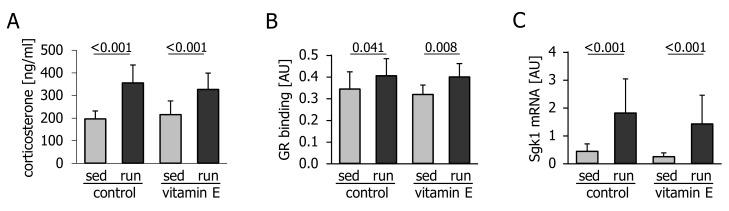
The attenuated upregulation of the exercise-responsive transcripts Ppargc1a, Pdk4, Irs2, and Angptl4 might have been due to the previously reported interference of vitamin E with glucocorticoid levels and signalling. In our study, exercise caused a pronounced increase in circulating corticosterone levels (Figure 3A), a significant increase in glucocorticoid receptor DNA-binding activity (Figure 3B) and upregulation of the glucocorticoid receptor target gene serum/glucocorticoid regulated kinase 1 (Sgk1), in the liver (Figure 3C). However, there was no effect of vitamin E (Figure 3A–C).
Figure 3.
(A) Plasma corticosterone levels, (B) glucocorticoid receptor (GR) DNA-binding activity, and (C) amount of liver serum/glucocorticoid regulated kinase 1 (Sgk1) mRNA in mice immediately after 1 h of treadmill running (run) or remaining sedentary (sed) and fasting for the same period of time. Prior to the experiment, mice had been fed a control or a vitamin E-enriched diet for four weeks. Values are means ± standard deviation from n = 10 (sedentary groups) or n = 12 (exercise groups) animals. AU, arbitrary units.
3.3. Vitamin E Alters the Hepatic Transcriptional Response Related to Lipid and Cholesterol Synthesis and Inflammation
To gain a more detailed insight into how vitamin E alters the regulatory processes that normally take place in the liver in response to exercise, we next performed a global transcriptome analysis. A total of 445 transcripts were significantly different (p < 0.05, median fold change >|1.2|) between exercised vitamin E-supplemented and exercised control mice. Among the 143 upregulated transcripts, only one, the phospholipid transfer protein (Pltp), was also upregulated by vitamin E in the sedentary state (median fold increase 1.58 in sedentary and 1.43 in exercised mice). Among the 302 downregulated transcripts, only two protein-coding genes showed consistent downregulation due to vitamin E supplementation in both sedentary and exercised mice: RNA specific adenosine deaminase (Adar) and the interleukin 21 receptor (Il21r). Next, all 445 transcripts differentially expressed between exercised vitamin E-supplemented and exercised control mice were subjected to an upstream regulator analysis using Ingenuity Pathway Analysis. A total of 11 upstream regulators were predicted to be activated (z-score ≥ 2) and 20 to be inhibited (z-score ≤ −2) with a significant p-value of overlap (p < 0.05) (Table 1).
Table 1.
Ingenuity upstream regulator analysis of the 445 transcripts that were significantly different between exercised mice fed a control or a vitamin E-enriched diet (limma t-test p < 0.05 and median fold change >|1.2|). All regulators with z-score ≥|2.0| (i.e., predicted to be activated or inhibited) and with a p-value of overlap <0.05 are shown (drugs and chemical upstream regulators were excluded).
| Upstream Regulator | Molecule Type | Activation z-Score | p-Value of Overlap | Predicted State |
|---|---|---|---|---|
| SCAP | Other | 3.58 | <0.001 | Activated |
| SREBF2 | Transcription regulator | 3.27 | <0.001 | Activated |
| SREBF1 | Transcription regulator | 2.71 | <0.001 | Activated |
| TSC2 | Other | 2.45 | 0.004 | Activated |
| Nr1h (LXR) | Group | 2.40 | 0.016 | Activated |
| PPARD | Ligand-dependent nuclear receptor | 2.23 | 0.006 | Activated |
| MLXIPL (ChREBP) | Transcription regulator | 2.22 | <0.001 | Activated |
| miR-145-5p 1 | Mature microRNA | 2.20 | <0.001 | Activated |
| FAS | Transmembrane receptor | 2.18 | 0.004 | Activated |
| INHA | Growth factor | 2.00 | 0.049 | Activated |
| ATP7B | Transporter | 2.00 | 0.002 | Activated |
| TLR7 | Transmembrane receptor | −2.62 | 0.004 | Inhibited |
| Interferon alpha | Group | −2.61 | 0.031 | Inhibited |
| TGFB1 | Growth factor | −2.59 | 0.002 | Inhibited |
| TICAM1 | Other | −2.43 | 0.011 | Inhibited |
| SP1 | Transcription regulator | −2.43 | 0.033 | Inhibited |
| APP | Other | −2.40 | 0.024 | Inhibited |
| IFNB1 | Cytokine | −2.40 | 0.013 | Inhibited |
| INSIG1 | Other | −2.39 | <0.001 | Inhibited |
| SRF | Transcription regulator | −2.37 | 0.002 | Inhibited |
| Vegf | Group | −2.36 | 0.035 | Inhibited |
| POR | Enzyme | −2.35 | <0.001 | Inhibited |
| MAP4K4 | Kinase | −2.24 | 0.005 | Inhibited |
| Ifn | Group | −2.20 | 0.021 | Inhibited |
| CREB1 | Transcription regulator | −2.17 | 0.008 | Inhibited |
| TGM2 | Enzyme | −2.16 | <0.001 | Inhibited |
| IFNG | Cytokine | −2.15 | <0.001 | Inhibited |
| MGEA5 | Enzyme | −2.11 | 0.025 | Inhibited |
| CSF2 (GM-CSF) | Cytokine | −2.07 | 0.018 | Inhibited |
| OSM | Cytokine | −2.04 | 0.025 | Inhibited |
| SAMSN1 | Other | −2.00 | 0.032 | Inhibited |
Common alternative symbols are given in brackets. 1 And other miRNAs with the seed UCCAGUU.
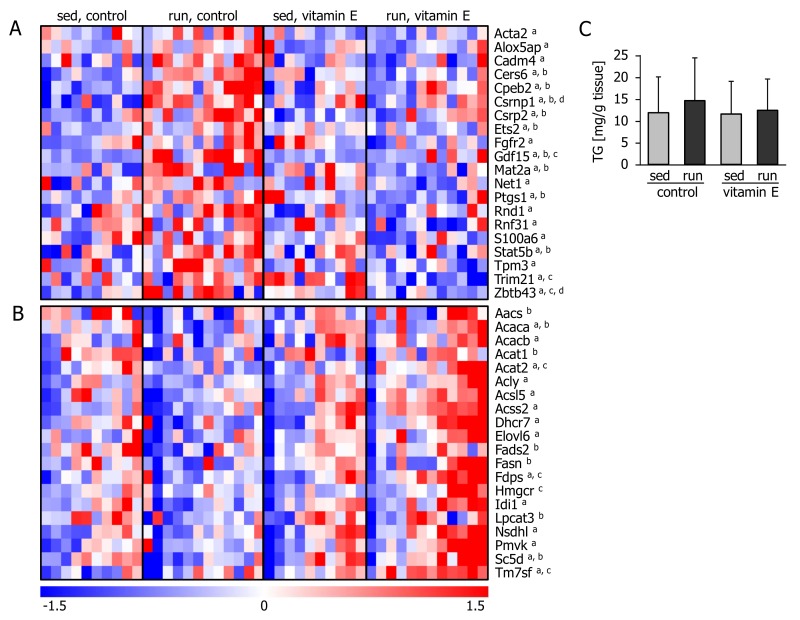
The upstream regulators predicted to be inhibited by vitamin E after the exercise bout comprised a number of well-known inflammatory players: toll like receptor 7 (TLR7) and the TLR adaptor protein, TICAM1; alpha, beta, and gamma interferons; transforming growth factor beta 1 (TGFB1) and the cytokines colony stimulating factor 2 (CSF2) and oncostatin (OSM), as well as the transcription factor cAMP responsive element binding protein 1 (CREB1) which may also be involved in immune function [31]. Next, we took a closer look at the individual transcripts predicted to be regulated by these inflammatory players according to Ingenuity Pathway Analysis. Several of these transcripts, such as growth differentiation factor 15 (Gdf15), prostaglandin synthase 1 (Ptgs1), and signal transducer and activator of transcription 5B (Stat5b), were increased in the livers of exercising control-fed mice, and this inflammatory response was attenuated by vitamin E supplementation (Figure 4A).
Figure 4.
Liver transcripts associated with upstream regulators of (A) inflammation and (B) lipid and cholesterol synthesis. Each column represents one animal. Superscript letters denote significant differences (p < 0.05) between a exercised mice fed the control or the vitamin E-enriched diet, b sedentary and exercised control mice, c sedentary and exercised vitamin E-supplemented mice, and d sedentary mice fed a control or vitamin E-enriched diet. (C) Liver triglycerides (TG) of mice immediately after 1 h of treadmill running (run) or remaining sedentary (sed) and fasting for the same period of time. Prior to the experiment, mice had been fed a control or a vitamin E-enriched diet for four weeks. Values are means ± standard deviation from n = 10 (sedentary groups) or n = 12 (exercise groups) animals.
Among the 11 transcriptional regulators predicted to be activated in the vitamin E group, we identified six as being involved in lipid synthesis and cholesterol metabolism: the nuclear receptor subfamily 1 receptors (Nr1h, also known as LXR), peroxisome proliferator activated receptor delta (PPARD), MLX interacting protein like (MLXIPL, also known as ChREBP), the sterol regulatory element binding transcription factors (SREBF) 1 and 2, and SCAP, a protein with a sterol sensing domain that activates SREBFs in the absence of cholesterol. Complementing these activated factors, INSIG, which acts antagonistically to SREBF1/2 and SCAP, was predicted to be inhibited (Table 1).
The transcript levels of key enzymes involved in lipogenesis and cholesterol synthesis, such as Fasn, acetyl-CoA carboxylases alpha (Acaca) and beta (Acacb),ATP citrate lyase (Acly), 3-hydroxy-3-methylglutaryl-CoA reductase (Hmgcr) and farnesyl diphosphate synthase (Fdps), were expressed at similar or even lower levels in the livers of sedentary and of exercised control-fed mice (Figure 4B). In contrast, in the livers of exercised, vitamin E-supplemented mice, the amount of these transcripts was generally increased. None of these transcripts showed a significant difference between the sedentary groups. This apparent exercise-induced activation of lipogenic pathways in vitamin E-supplemented mice was not reflected by a different hepatic triglyceride content at the investigated timepoint—immediately after the exercise bout (Figure 4C).
4. Discussion
The results of our study show that vitamin E (α-tocopherol) supplementation can impair the acute adaptation of the liver to physical exercise. The hepatic exercise response is characterized by an increase in glucose production and fatty acid oxidation [3] and by an activation of inflammatory and stress signalling pathways [19,20]. We have previously reported that the liver responds to exercise with an increased transcription of key regulators of mitochondrial biogenesis and glucose and lipid metabolism [21]. In the long run, these acute responses are supposed to translate into decreased lipogenesis and increased lipid oxidation, which both contribute to the reduction of hepatic fat content [3]. The results of our global transcriptome analysis and targeted mRNA quantification indicate that vitamin E supplementation interferes with the acute metabolic and inflammatory responses of the liver. At the same time, vitamin E counteracted the moderate increase in circulating FFA that is normally seen shortly after an endurance activity of this type in mice [21] and humans [32].
An Ingenuity Pathway Analysis comparing exercised mice with and without vitamin E supplementation predicted the activation of 11 upstream regulators, while 20 were inhibited. Out of the 11 activated factors, six were transcriptional regulators of lipid and cholesterol synthesis, such as SREBP, SCAP, and ChREBP. In contrast, INSIG, a negative regulator of SREBP and SCAP, was predicted to be inhibited. When looking at individual transcripts that are under the control of these regulators, we found the rate-limiting enzymes in fatty acid synthesis to be significantly higher in exercised, vitamin E-fed mice than in exercised control mice, for example, the levels of Fdps and of Acaca and Acacb. Acacb and the fatty acid synthase, Fasn, were downregulated by exercise under control diet conditions, and this downregulation was abrogated with vitamin E. In contrast, vitamin E supplementation caused transcripts such as Fdps and Hmgcr, which are key enzymes in cholesterol biosynthesis, to be upregulated by exercise. Thus, vitamin E supplementation shifted the overall lipid and cholesterol synthesis-related transcriptional response towards an activation that is normally not seen after physical activity.
Since the upstream regulators SREBP, LXR and ChREBP are normally inhibited in catabolic conditions by fatty acids [33], the different transcriptional profiles could, at least in part, be related to the attenuated exercise-induced increase in FFA levels in vitamin E-fed mice. These lower FFA concentrations could be caused by a reduced rate of lipolysis or by an increased uptake and utilization. We did not detect differences in whole-body oxygen consumption, a measure of energy expenditure, or in the respiratory quotient, which reflects the percentage of fat oxidized. Therefore, the lower plasma FFA concentrations were likely not caused by major differences in the utilization of energy sources. FFA taken up by the liver could also be re-esterified into triglycerides. While we did not find liver triglyceride levels to be different, the increased abundance of Pltp mRNA in sedentary and exercised vitamin-E fed mice may be of interest in this context; Pltp is a vitamin E transfer protein and is also important for the lipidation and hepatic secretion of VLDL [34]. Thus, the vitamin E-supplemented mice may not have accumulated hepatic triglycerides due to increased VLDL release.
Alternatively, vitamin E could have reduced adipose tissue lipolysis through its previously reported interference with the glucocorticoid response [13,14,15], as glucocorticoids stimulate lipolysis [35]. Glucocorticoid receptor signal transduction has also been implicated in the gene expression of Irs2 and Pdk4 [27], Angptl4 [26], and Ppargc1a [25]. However, we could not find evidence for an altered glucocorticoid response as corticosterone levels and signalling increased to a similar extent in both groups of exercised mice. Catecholamine-triggered cAMP-dependent pathways are important activators of lipolysis as well as regulators of Irs2 [36] and Ppargc1a [37] transcription. A potential suppressive effect of vitamin E on cAMP signalling was suggested by the predicted inhibition of the upstream regulator CREB. We did not, however, attempt to quantify catecholamines, which increase rapidly in mice during procedures such as immobilization and anaesthesia.
The list of inhibited regulators further encompassed several inflammatory players, namely, TLR7, TGFB1, and the cytokines IFNB1, IFNG, CSF2 and OSM. Transcripts that were upregulated by exercise only in the absence of vitamin E included the TGFB family member and pleiotropic cytokine Gdf15, the cytokine signal transducer Stat5b, and enzymes involved in the synthesis of inflammation-related molecules, such as prostaglandin synthase (Ptgs1), arachidonate 5-lipoxygenase activating protein (Alox5ap) and ceramide synthase 6 (Cers6).
The detailed mechanism by which vitamin E altered the inflammatory response to exercise is unclear. Vitamin E is known to decrease pro-inflammatory cytokines such as interleukin 6 (IL-6) [38], which is known to acutely increase during physical exercise [39]. We did not assess IL-6 levels in this study, but we have previously found mice lacking IL-6 to respond to physical activity with similar increases in circulating FFA and in hepatic Ppargc1a and Irs2 transcription [40], which argues against a major role for circulating IL-6 in mediating the vitamin E effects of exercise. However, cytokines other than IL-6 may also play a role and be confined to a local response, and as vitamin E also interferes with monocyte adhesion, it could affect the inflammatory response independent of differences in cytokine levels [38].
An interesting question is whether the acute effects observed in this study translate to altered or impaired adaptation of the liver when physical exercise training is accompanied by high vitamin E intake, in particular as a means to improve insulin sensitivity and NAFLD. We are only aware of one study that has investigated the effects of training combined with a vitamin E-only supplementation on the liver. This study, performed in rats, found that vitamin E counteracted swim training-induced increases in Ppargc1a protein and mitochondrial content [41], indicating that at least some of the acute effects reported here can culminate in long-term impairments of the hepatic adaptation to exercise.
Vitamin E appeared to affect glucose and lipid metabolism-related transcription in a concerted fashion. Firstly, it counteracted the induction of factors involved in mitochondrial biogenesis (Ppargc1a), insulin signalling (Irs2), fatty acid oxidation (Cpt2), and metabolite fuel selection (Pdk4). Secondly, transcripts involved in lipid and cholesterol synthesis were increased in the condition involving exercise plus vitamin E, which is in contrast to the reduction in lipogenic enzymes in the liver observed in the exercised control mice and in previously published studies [22,42]. Thus, vitamin E could interfere with both mechanisms that mediate the reduction of liver fat following regular physical activity, with the downregulation of lipogenic enzymes and with the upregulation of enzymes involved in fatty acid oxidation.
According to the hormesis theory [7], acute, tolerable stress can be viewed as adjuvant stimulus that triggers beneficial long-term effects. The predominant part of exercise-related research published so far has dealt with skeletal muscle. Here, it is already known that besides redox signalling, a proper local inflammatory response is required for functional adaptation to exercise [43]. In this context, it is worth looking at how physical exercise modulates immune function on the systemic level: Acutely, exercise elicits an intensity-dependent cytokine response [39]. Regular training, in contrast, reduces systemic low-grade inflammation [44,45] and hepatic inflammation associated with NAFLD and obesity [46] and alters the immune state of the liver, making it less susceptible to acute TNF-mediated injury [47]. If, in analogy to the muscle, the acute inflammatory response of the liver contributes to a beneficial adaptation process, one might speculate that the interference of vitamin E with this response is not desirable.
Studies testing vitamin E supplementation for the treatment of NAFLD have not reached a clear conclusion regarding its efficacy and safety, and there is even debate over whether it may increase all-cause mortality at high doses [48]. One reason for the equivocal results of in vivo vitamin E studies might be the fact that it has different modes of action that are still not completely understood [49]. Our data suggest that some effects of vitamin E might only come into play during physical exercise or similar metabolic challenges.
5. Conclusions
Vitamin E affected the acute response of the liver to physical exercise in a concerted fashion that was potentially related to lower levels of circulating FFA. The differences in FFA concentrations and in hepatic transcription were not caused by the previously-reported inhibition of glucocorticoid signalling by vitamin E. By dampening the inflammatory and altering the metabolic response, increased vitamin E intake could interfere with the beneficial adaptations that normally occur in the liver as a result of physical exercise training.
Acknowledgments
This work was supported in part by grants from the German Federal Ministry of Education and Research (BMBF) to the German Center for Diabetes Research (DZD e.V.; No. 01GI0925) and by the Helmholtz Alliance ‘Aging and Metabolic Programming, AMPro’ (J.B.). We thank H.R., A.K.H. and E.M. for excellent technical assistance. We acknowledge support by Deutsche Forschungsgemeinschaft (DFG) and Open Access Publishing Fund of the University of Tübingen.
Author Contributions
M.H. and C.W. conceived and designed the experiments; M.H. and M.I. performed the experiments; M.H., M.I. and C.W. analyzed the data; M.H. and C.W. wrote the paper; M.I., J.B., M.H.d.A. and H.-U.H. contributed to discussion and reviewed the manuscript. All authors have read and approved the final version submitted for publication.
Conflicts of Interest
The authors declare no conflict of interest. The founding sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish the results.
References
- 1.Jakicic J.M., Rogers R.J., Davis K.K., Collins K.A. Role of Physical Activity and Exercise in Treating Patients with Overweight and Obesity. Clin. Chem. 2018;64:99–107. doi: 10.1373/clinchem.2017.272443. [DOI] [PubMed] [Google Scholar]
- 2.Orci L.A., Gariani K., Oldani G., Delaune V., Morel P., Toso C. Exercise-based Interventions for Nonalcoholic Fatty Liver Disease: A Meta-analysis and Meta-regression. Clin. Gastroenterol. Hepatol. 2016;14:1398–1411. doi: 10.1016/j.cgh.2016.04.036. [DOI] [PubMed] [Google Scholar]
- 3.Trefts E., Williams A.S., Wasserman D.H. Exercise and the Regulation of Hepatic Metabolism. Prog. Mol. Biol. Transl. Sci. 2015;135:203–225. doi: 10.1016/bs.pmbts.2015.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shephard R.J., Johnson N. Effects of physical activity upon the liver. Eur. J. Appl. Physiol. 2015;115:1–46. doi: 10.1007/s00421-014-3031-6. [DOI] [PubMed] [Google Scholar]
- 5.Niess A.M., Simon P. Response and adaptation of skeletal muscle to exercise—The role of reactive oxygen species. Front. Biosci. 2007;12:4826–4838. doi: 10.2741/2431. [DOI] [PubMed] [Google Scholar]
- 6.Novelli G.P., Bracciotti G., Falsini S. Spin-trappers and vitamin E prolong endurance to muscle fatigue in mice. Free Radic. Biol. Med. 1990;8:9–13. doi: 10.1016/0891-5849(90)90138-9. [DOI] [PubMed] [Google Scholar]
- 7.Gomez-Cabrera M.-C., Domenech E., Viña J. Moderate exercise is an antioxidant: Upregulation of antioxidant genes by training. Free Radic. Biol. Med. 2008;44:126–131. doi: 10.1016/j.freeradbiomed.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Merry T.L., Ristow M. Do antioxidant supplements interfere with skeletal muscle adaptation to exercise training? J. Physiol. 2016;594:5135–5147. doi: 10.1113/JP270654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Powers S.K., Jackson M.J. Exercise-induced oxidative stress: Cellular mechanisms and impact on muscle force production. Physiol. Rev. 2008;88:1243–1276. doi: 10.1152/physrev.00031.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ristow M., Zarse K., Oberbach A., Klöting N., Birringer M., Kiehntopf M., Stumvoll M., Kahn C.R., Blüher M. Antioxidants prevent health-promoting effects of physical exercise in humans. Proc. Natl. Acad. Sci. USA. 2009;106:8665–8670. doi: 10.1073/pnas.0903485106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paulsen G., Cumming K.T., Holden G., Hallén J., Rønnestad B.R., Sveen O., Skaug A., Paur I., Bastani N.E., Ostgaard H.N., et al. Vitamin C and E supplementation hampers cellular adaptation to endurance training in humans: A double-blind randomized controlled trial. J. Physiol. 2014;592:1887–1901. doi: 10.1113/jphysiol.2013.267419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Strobel N.A., Peake J.M., Matsumoto A., Marsh S.A., Coombes J.S., Wadley G.D. Antioxidant Supplementation Reduces Skeletal Muscle Mitochondrial Biogenesis. Med. Sci. Sports Exerc. 2010;43:1017–1024. doi: 10.1249/MSS.0b013e318203afa3. [DOI] [PubMed] [Google Scholar]
- 13.Zingg J.-M., Azzi A. Non-antioxidant activities of vitamin E. Curr. Med. Chem. 2004;11:1113–1133. doi: 10.2174/0929867043365332. [DOI] [PubMed] [Google Scholar]
- 14.Tsiakitzis K., Kourounakis A.P., Tani E., Rekka E.A., Kourounakis P.N. Stress and active oxygen species—Effect of alpha-tocopherol on stress response. Arch. Pharm. (Weinheim) 2005;338:315–321. doi: 10.1002/ardp.200400946. [DOI] [PubMed] [Google Scholar]
- 15.Ohtsuka A., Kojima H., Ohtani T., Hayashi K. Vitamin E reduces glucocorticoid-induced oxidative stress in rat skeletal muscle. J. Nutr. Sci. Vitaminol. (Tokyo) 1998;44:779–786. doi: 10.3177/jnsv.44.779. [DOI] [PubMed] [Google Scholar]
- 16.Fischer C.P., Hiscock N.J., Penkowa M., Basu S., Vessby B., Kallner A., Sjoberg L.B., Pedersen B.K. Supplementation with vitamins C and E inhibits the release of interleukin-6 from contracting human skeletal muscle. J. Physiol. 2004;558:633–645. doi: 10.1113/jphysiol.2004.066779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Higashida K., Kim S.H., Higuchi M., Holloszy J.O., Han D.-H. Normal adaptations to exercise despite protection against oxidative stress. Am. J. Physiol. Endocrinol. Metab. 2011;301:E779–E784. doi: 10.1152/ajpendo.00655.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yfanti C., Nielsen A.R., Akerström T., Nielsen S., Rose A.J., Richter E.A., Lykkesfeldt J., Fischer C.P., Pedersen B.K. Effect of antioxidant supplementation on insulin sensitivity in response to endurance exercise training. Am. J. Physiol. Endocrinol. Metab. 2011;300:E761–E770. doi: 10.1152/ajpendo.00207.2010. [DOI] [PubMed] [Google Scholar]
- 19.Ford E.S., Ajani U.A., Mokdad A.H. Brief communication: The prevalence of high intake of vitamin E from the use of supplements among U.S. adults. Ann. Intern. Med. 2005;143:116–120. doi: 10.7326/0003-4819-143-2-200507190-00010. [DOI] [PubMed] [Google Scholar]
- 20.Hoene M., Weigert C. The stress response of the liver to physical exercise. Exerc. Immunol. Rev. 2010;16:163–183. [PubMed] [Google Scholar]
- 21.Pillon Barcelos R., Freire Royes L.F., Gonzalez-Gallego J., Bresciani G. Oxidative stress and inflammation: Liver responses and adaptations to acute and regular exercise. Free Radic. Res. 2017;51:222–236. doi: 10.1080/10715762.2017.1291942. [DOI] [PubMed] [Google Scholar]
- 22.Hoene M., Lehmann R., Hennige A.M., Pohl A.K., Häring H.U., Schleicher E.D., Weigert C. Acute regulation of metabolic genes and insulin receptor substrates in the liver of mice by one single bout of treadmill exercise. J. Physiol. 2009;587:241–252. doi: 10.1113/jphysiol.2008.160275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoene M., Li J., Li Y., Runge H., Zhao X., Häring H.-U., Lehmann R., Xu G., Weigert C. Muscle and liver-specific alterations in lipid and acylcarnitine metabolism after a single bout of exercise in mice. Sci. Rep. 2016;6:22218. doi: 10.1038/srep22218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Traber M.G., Arai H. Molecular mechanisms of vitamin E transport. Annu. Rev. Nutr. 1999;19:343–355. doi: 10.1146/annurev.nutr.19.1.343. [DOI] [PubMed] [Google Scholar]
- 25.Bernal-Mizrachi C., Weng S., Feng C., Finck B.N., Knutsen R.H., Leone T.C., Coleman T., Mecham R.P., Kelly D.P., Semenkovich C.F. Dexamethasone induction of hypertension and diabetes is PPAR-alpha dependent in LDL receptor-null mice. Nat. Med. 2003;9:1069–1075. doi: 10.1038/nm898. [DOI] [PubMed] [Google Scholar]
- 26.Koliwad S.K., Kuo T., Shipp L.E., Gray N.E., Backhed F., So A.Y.-L., Farese R.V., Wang J.-C. Angiopoietin-like 4 (ANGPTL4, fasting-induced adipose factor) is a direct glucocorticoid receptor target and participates in glucocorticoid-regulated triglyceride metabolism. J. Biol. Chem. 2009;284:25593–25601. doi: 10.1074/jbc.M109.025452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuo T., Harris C.A., Wang J.-C. Metabolic functions of glucocorticoid receptor in skeletal muscle. Mol. Cell. Endocrinol. 2013;380:79–88. doi: 10.1016/j.mce.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rimbach G., Moehring J., Huebbe P., Lodge J.K. Gene-regulatory activity of alpha-tocopherol. Molecules. 2010;15:1746–1761. doi: 10.3390/molecules15031746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Böhm A., Hoffmann C., Irmler M., Schneeweiss P., Schnauder G., Sailer C., Schmid V., Hudemann J., Machann J., Schick F., et al. TGF-β Contributes to Impaired Exercise Response by Suppression of Mitochondrial Key Regulators in Skeletal Muscle. Diabetes. 2016;65:2849–2861. doi: 10.2337/db15-1723. [DOI] [PubMed] [Google Scholar]
- 30.Saeed A.I., Sharov V., White J., Li J., Liang W., Bhagabati N., Braisted J., Klapa M., Currier T., Thiagarajan M., et al. TM4: A free, open-source system for microarray data management and analysis. BioTechniques. 2003;34:374–378. doi: 10.2144/03342mt01. [DOI] [PubMed] [Google Scholar]
- 31.Wen A.Y., Sakamoto K.M., Miller L.S. The role of the transcription factor CREB in immune function. J. Immunol. 2010;185:6413–6419. doi: 10.4049/jimmunol.1001829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hansen J.S., Zhao X., Irmler M., Liu X., Hoene M., Scheler M., Li Y., Beckers J., Hrabĕ de Angelis M., Häring H.-U., et al. Type 2 diabetes alters metabolic and transcriptional signatures of glucose and amino acid metabolism during exercise and recovery. Diabetologia. 2015;58:1845–1854. doi: 10.1007/s00125-015-3584-x. [DOI] [PubMed] [Google Scholar]
- 33.Pégorier J.-P., Le May C., Girard J. Control of gene expression by fatty acids. J. Nutr. 2004;134:2444S–2449S. doi: 10.1093/jn/134.9.2444S. [DOI] [PubMed] [Google Scholar]
- 34.Jiang X.-C. Phospholipid transfer protein: Its impact on lipoprotein homeostasis and atheroslcerosis. J. Lipid Res. 2018 doi: 10.1194/jlr.R082503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Djurhuus C.B., Gravholt C.H., Nielsen S., Mengel A., Christiansen J.S., Schmitz O.E., Møller N. Effects of cortisol on lipolysis and regional interstitial glycerol levels in humans. Am. J. Physiol. Endocrinol. Metab. 2002;283:E172–E177. doi: 10.1152/ajpendo.00544.2001. [DOI] [PubMed] [Google Scholar]
- 36.Jhala U.S., Canettieri G., Screaton R.A., Kulkarni R.N., Krajewski S., Reed J., Walker J., Lin X., White M., Montminy M. cAMP promotes pancreatic beta-cell survival via CREB-mediated induction of IRS2. Genes Dev. 2003;17:1575–1580. doi: 10.1101/gad.1097103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Buler M., Aatsinki S.-M., Skoumal R., Komka Z., Tóth M., Kerkelä R., Georgiadi A., Kersten S., Hakkola J. Energy-sensing factors coactivator peroxisome proliferator-activated receptor γ coactivator 1-α (PGC-1α) and AMP-activated protein kinase control expression of inflammatory mediators in liver: Induction of interleukin 1 receptor antagonist. J. Biol. Chem. 2012;287:1847–1860. doi: 10.1074/jbc.M111.302356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Singh U., Jialal I. Anti-inflammatory effects of alpha-tocopherol. Ann. N. Y. Acad. Sci. 2004;1031:195–203. doi: 10.1196/annals.1331.019. [DOI] [PubMed] [Google Scholar]
- 39.Pedersen B.K. Special feature for the Olympics: Effects of exercise on the immune system: Exercise and cytokines. Immunol. Cell Biol. 2000;78:532–535. doi: 10.1111/j.1440-1711.2000.t01-11-.x. [DOI] [PubMed] [Google Scholar]
- 40.Fritsche L., Hoene M., Lehmann R., Ellingsgaard H., Hennige A.M., Pohl A.K., Häring H.U., Schleicher E.D., Weigert C. IL-6 deficiency in mice neither impairs induction of metabolic genes in the liver nor affects blood glucose levels during fasting and moderately intense exercise. Diabetologia. 2010;53:1732–1742. doi: 10.1007/s00125-010-1754-4. [DOI] [PubMed] [Google Scholar]
- 41.Venditti P., Napolitano G., Barone D., Di Meo S. Effect of training and vitamin E administration on rat liver oxidative metabolism. Free Radic. Res. 2014;48:322–332. doi: 10.3109/10715762.2013.867959. [DOI] [PubMed] [Google Scholar]
- 42.Griffiths M.A., Baker D.H., Yu X.X., Novakofski J., Oscai L., Ji L.L. Effects of acute exercise on hepatic lipogenic enzymes in fasted and refed rats. J. Appl. Physiol. 1995;79:879–885. doi: 10.1152/jappl.1995.79.3.879. [DOI] [PubMed] [Google Scholar]
- 43.Pillon N.J., Bilan P.J., Fink L.N., Klip A. Cross-talk between skeletal muscle and immune cells: Muscle-derived mediators and metabolic implications. Am. J. Physiol. Endocrinol. Metab. 2013;304:E453–E465. doi: 10.1152/ajpendo.00553.2012. [DOI] [PubMed] [Google Scholar]
- 44.Gleeson M., Bishop N.C., Stensel D.J., Lindley M.R., Mastana S.S., Nimmo M.A. The anti-inflammatory effects of exercise: Mechanisms and implications for the prevention and treatment of disease. Nat. Rev. Immunol. 2011;11:607–615. doi: 10.1038/nri3041. [DOI] [PubMed] [Google Scholar]
- 45.Krüger K., Mooren F.-C., Pilat C. The Immunomodulatory Effects of Physical Activity. Curr. Pharm. Des. 2016;22:3730–3748. doi: 10.2174/1381612822666160322145107. [DOI] [PubMed] [Google Scholar]
- 46.Lancaster G.I., Febbraio M.A. The immunomodulating role of exercise in metabolic disease. Trends Immunol. 2014;35:262–269. doi: 10.1016/j.it.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 47.Huber Y., Gehrke N., Biedenbach J., Helmig S., Simon P., Straub B.K., Bergheim I., Huber T., Schuppan D., Galle P.R., et al. Voluntary distance running prevents TNF-mediated liver injury in mice through alterations of the intrahepatic immune milieu. Cell Death Dis. 2017;8:e2893. doi: 10.1038/cddis.2017.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hadi H.E., Vettor R., Rossato M. Vitamin E as a Treatment for Nonalcoholic Fatty Liver Disease: Reality or Myth? Antioxidants. 2018;7:12. doi: 10.3390/antiox7010012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brigelius-Flohe R., Galli F. Vitamin E: A vitamin still awaiting the detection of its biological function. Mol. Nutr. Food Res. 2010;54:583–587. doi: 10.1002/mnfr.201000091. [DOI] [PubMed] [Google Scholar]