Abstract
Background
Despite a rise in the prevalence of hepatocellular carcinoma (HCC), data on HCC-related hospitalizations and financial burden are limited. The aim of this study was to evaluate temporal trends of HCC-related hospitalizations and evaluate its financial influence.
Materials and Methods
Patients with the diagnosis of HCC, as reported by International Classification of Diseases-Ninth Revision code, were identified from the National Inpatient Sample databases from 2002–2011. The national estimates of hospitalizations were derived using appropriate sample weights. The change in total average charges per each hospitalization over the study period was calculated after adjusting for inflation.
Results
Hospitalizations related to HCC have increased from 24,024 in 2002 to 50,609 in 2011. Of these admissions, HCC was the principal diagnosis in 10,762 and 16,350 subjects in 2002 and 2011, respectively. Most were white males (male: 70%; white: 55%). The overall inpatient mortality was significantly decreased from 13.5% in 2002 to 9.9% in 2011 (P < 0.01). The same trend was also observed for the length of hospital stay (6.5 versus 5.6 days in 2002 and 2011, respectively). The inflation-adjusted cost per hospitalization increased by approximately 47% during the study period.
Conclusions
Despite the decrease in mortality rate and length-of-stay, hospitalizations and financial burden associated with HCC continued to increase between 2002 and 2011 in the United States.
Key Indexing Terms: Hepatocellular carcinoma, Financial burden, National Inpatient Sample database, Hospitalizations, Liver cancer
BACKGROUND
Hepatocellular carcinoma (HCC) is responsible for significant morbidity and mortality in the United States, and it contributes a substantial economic burden to our healthcare system. Globally, HCC represents the fifth most prevalent cancer in men, the seventh most common cancer in women and is the third leading cause of cancer-related deaths worldwide.1 HCC occurs most frequently in the setting of chronic liver disease and cirrhosis and is most commonly associated with viral hepatitis.2,3 The incidence of HCC within the United States has been increasing over the past several decades, in parallel with the increase in hepatitis C virus and nonalcoholic steatohepatitis associated cirrhosis.2–6
The increase in HCC incidence continues to pose increasing demand for diagnosis, care and treatment.7 Therapeutic approaches for the treatment of HCC have evolved over the past few decades, including surgical resection, ablation therapy, transarterial chemoembolization and liver transplantation. These treatment modalities, while improving and benefitting patients with HCC, also lead to increase in cost and economic burden.2,6–8 Previous studies have evaluated the changing incidence and mortality rates of HCC over the years. However, few have studied the magnitude of change and its economic influence on inpatient hospitalization. The goals of this study are to determine the temporal trends of inpatient volume and evaluate the length-of-stay (LOS), total hospital charges and in-hospital mortality rate of HCC over the last decade.
MATERIALS AND METHODS
The Nationwide Inpatient Sample (NIS) from 2002–2011, developed by the Agency for Healthcare Research and Quality, was the primary data source for the analysis.9 These data are the largest all-payer inpatient care database in the United States, containing data on more than 7 million hospital stays annually from approximately 1,000 hospitals, constituting a 20% stratified sample of all U.S. hospitals. All data were weighted using discharge-level values to produce 100% national estimates.
We identified patients with HCC by using International Classification of Diseases-Ninth Revision, Clinical Modification (ICD-9-CM) discharge diagnosis code 155.0. If this code was listed in the first position, we considered HCC as the primary diagnosis or principal reason leading to hospitalization. Otherwise, we considered HCC as the secondary diagnosis for admission. In this scenario, patients were hospitalized for various causes, which may not be related to the underlying HCC.
The following variables were retrieved from the dataset: patient age, race, sex, household income, the geographic region of the hospitals and payers (i.e., Medicare, Medicaid and private). The types of hospitals were categorized into teaching or nonteaching, small or medium or large depending on the number of beds, and urban or rural location. Outcome-measures were strati-fied for overall, primary and secondary diagnoses of HCC and included in-hospital mortality, LOS, financial charges and discharge disposition.
Additional data regarding radio or chemotherapy, liver biopsy, surgery and transplant interventions were retrieved using various ICD-9 codes. Proportions of HCC-related hospitalizations when intervention was performed and average cost of HCC-related hospitalizations with these interventions are provided in Supplementary Tables 1 and 2.
Statistical Analysis
All statistical analyses were performed using the sampling weights to obtain nationally representative estimates. Descriptive statistics were presented as a mean and frequencies for continuous and categorical variables, respectively. Annual rates of HCC-related hospitalization were calculated by dividing the number of inpatient admissions for HCC, stratified by primary or secondary diagnosis, by the total inpatient admissions in a given year. The financial charges per each hospitalization were calculated and additional cost of hospitalization per year was also calculated after adjusting for the inflation, using year 2002 as the reference. The trend analysis was performed using simple linear regression. All analyses were performed using SAS 9.3 (Cary, NC), and the P < 0.05 was considered statistically significant.
RESULTS
National Estimates of HCC-Related Hospitalization Rates in the United States
We observed an increase in the rate for the overall HCC-related hospitalizations from 0.07% in 2002 to 0.14% in 2011 (P < 0.001). We observed no changes in the rate of admission when HCC was the primary diagnosis (0.03% in 2002 and 0.04% in 2011, P = 0.23). However, the rate of hospitalization when HCC was the secondary diagnosis increased significantly from 0.04% in 2002 to 0.09% in 2011 (P < 0.001, Table 1).
TABLE 1.
National estimates of HCC-related hospitalizations, year 2002–2011.a
| 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Slope | P Value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall HCC-related | ||||||||||||
| n | 24,024 | 29,099 | 31,071 | 31,787 | 29,388 | 36,712 | 46,617 | 44,988 | 48,080 | 50,609 | ||
| % of overall hospitalization | 0.07 | 0.08 | 0.08 | 0.08 | 0.08 | 0.10 | 0.12 | 0.12 | 0.13 | 0.14 | 0.008 | <0.001 |
| Primary diagnosis-related | ||||||||||||
| n | 10,762 | 12,748 | 13,179 | 13,489 | 12,012 | 14,709 | 17,263 | 16,262 | 16,172 | 16,350 | ||
| % of overall hospitalization | 0.03 | 0.03 | 0.04 | 0.04 | 0.03 | 0.04 | 0.05 | 0.04 | 0.04 | 0.04 | 0.001 | 0.227 |
| Secondary diagnosis-related | ||||||||||||
| n | 13,261 | 16,351 | 17,892 | 18,297 | 17,376 | 22,003 | 29,354 | 28,726 | 31,908 | 34,260 | ||
| % of overall hospitalization | 0.04 | 0.04 | 0.05 | 0.05 | 0.05 | 0.06 | 0.08 | 0.08 | 0.09 | 0.09 | 0.006 | <0.001 |
| All hospitalizations in the United States | ||||||||||||
| n | 36,523,831 | 37,074,605 | 37,496,978 | 37,843,039 | 38,076,556 | 38,155,908 | 38,210,889 | 37,734,584 | 37,352,013 | 36,962,415 | ||
| % of overall hospitalization | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | – | – |
HCC, hepatocellular carcinoma.
n = sample size (weighted frequencies reported).
Demographics and Clinical Characteristics of Hospitalized Patients With HCC
The mean age of hospitalized patients with HCC was 60 years. Most were males (70–74%) and white (51–57%). In 2002, almost half of patients were classified as high income (fourth quartile), in contrast to only 19% in 2011 (Table 2).
TABLE 2.
Baseline characteristics of hospitalizations from HCC, year 2002–2011.
| 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age in years, mean (SE) | 59.2 (1.0) | 60.2 (0.7) | 59.6 (0.7) | 59.1 (0.9) | 59.3 (0.8) | 61.2 (0.4) | 60.1 (0.7) | 61.3 (0.5) | 60.8 (0.5) | 61.1 (0.6) |
| Race (%) | ||||||||||
| White | 56.0 | 53.5 | 56.9 | 55.4 | 51.4 | 56.2 | 54.3 | 54.7 | 56.9 | 54.7 |
| Black | 11.8 | 12.8 | 13.6 | 11.4 | 14.2 | 13 | 12.6 | 13.2 | 15.3 | 15.5 |
| Hispanic | 14.9 | 17.1 | 15.0 | 17.9 | 20.0 | 16.1 | 16.6 | 16.6 | 16.4 | 18.0 |
| Others | 17.3 | 16.4 | 14.5 | 15.3 | 14.4 | 14.7 | 16.5 | 15.5 | 11.4 | 11.8 |
| Sex (male, %) | 70.7 | 69.9 | 70.9 | 70.2 | 72.8 | 73.4 | 72.5 | 71.8 | 72.3 | 73.9 |
| Household income (%)a | ||||||||||
| First quartile | 6.9 | 29.1 | 29.3 | 27.2 | 29.6 | 28.7 | 27.1 | 29.0 | 29.8 | 32.4 |
| Second quartile | 17.8 | 26.0 | 25.7 | 23.3 | 23.9 | 23.1 | 25.6 | 24.9 | 24.2 | 23.7 |
| Third quartile | 23.5 | 22.9 | 20.1 | 24.2 | 23.3 | 23.6 | 22.5 | 23.5 | 24.0 | 24.8 |
| Fourth quartile | 51.9 | 22.0 | 24.9 | 25.3 | 23.2 | 24.6 | 24.8 | 22.6 | 22.0 | 19.2 |
HCC, hepatocellular carcinoma; SE, standard error.
2003–2011: median household income (1) $1-$38,999, (2) $39,000-$47,999, (3) $48,000–62,999 and (4) $63,000 or more. 2002: median household income (1) $1-$24,999, (2) $25,000-$34,999, (3) $35,000-$44,999 and (4) $45,000 or more.
Sources of Admission and Types of Facilities for Hospitalized Patients With HCC
Hospitalized patients with HCC were admitted mainly through local emergency departments (Table 3). Most patients (61–70%) were admitted to teaching hospitals.
TABLE 3.
Admission source, type and region of admitting hospitals of hospitalized patients with HCC in the United States from 2002–2011.
| 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Admission source (%) | ||||||||||
| Emergency department | 48.6 | 43.8 | 44.9 | 45.0 | 51.6 | 51.3 | 51.4 | 48.8 | 50.6 | 40.7 |
| Another hospital | 2.9 | 4.4 | 5.1 | 5.2 | 3.0 | 4.3 | 4.0 | 5.7 | 4.7 | 4.3 |
| Other facility including long-term care | 1.2 | 1.0 | 1.1 | 1.5 | 1.6 | 1.1 | 1.5 | 2.0 | 2.5 | 1.4 |
| Other (law enforcement, routine etc.) | 47.3 | 50.8 | 48.9 | 48.3 | 43.8 | 43.3 | 43.1 | 43.5 | 42.2 | 53.6 |
| Hospital location (%) | ||||||||||
| Rural | 7.1 | 6.6 | 6.2 | 6.7 | 5.9 | 5.9 | 5.3 | 5.6 | 5.3 | 4.6 |
| Urban | 92.9 | 93.4 | 93.8 | 93.3 | 94.1 | 94.1 | 94.7 | 94.4 | 94.7 | 95.4 |
| Teaching status of the hospital (%) | ||||||||||
| Nonteaching | 35.3 | 33.3 | 35.0 | 39.2 | 34.9 | 31.6 | 29.7 | 32.4 | 31.1 | 30.9 |
| Teaching | 64.7 | 66.7 | 65.0 | 60.8 | 65.1 | 68.4 | 70.3 | 67.6 | 68.9 | 69.1 |
| Hospital bed size (%) | ||||||||||
| Small | 9.3 | 8.6 | 8.1 | 8.7 | 10.6 | 8.9 | 6.8 | 10.1 | 8.4 | 6.5 |
| Medium | 19.2 | 19.4 | 18.6 | 22.7 | 21.2 | 19.2 | 16.1 | 20.6 | 16.9 | 19.1 |
| Large | 71.5 | 72.0 | 73.3 | 68.6 | 68.2 | 71.9 | 77.1 | 69.3 | 74.7 | 74.4 |
| Region of admitting hospital (%) | ||||||||||
| Northeast | 20.9 | 30.3 | 24.8 | 21.6 | 20.1 | 22.2 | 26.5 | 18.4 | 25.6 | 22.0 |
| Midwest | 18.3 | 15.3 | 16.9 | 16.1 | 15.6 | 16.9 | 15.1 | 21.0 | 17.4 | 18.0 |
| South | 35.0 | 30.9 | 36.6 | 29.3 | 37.3 | 34.6 | 29.4 | 30.4 | 30.9 | 37.9 |
| West | 25.8 | 23.6 | 21.7 | 33.0 | 27.0 | 26.3 | 29.1 | 30.2 | 26.0 | 22.2 |
HCC, hepatocellular carcinoma.
LOS, Discharge Patterns and Payers Related to HCC Hospitalizations
During the study period, there was a significant decrease in the average LOS for all hospitalized patients with HCC (6.5 days in 2002 to 5.6 days in 2011, P-value for trend <0.001). The same trend was observed when we analyzed the data for patients who were admitted with HCC as a primary diagnosis (7.1 days in 2002 to 5.9 days in 2011, P-value for trend <0.001). Interestingly, there were no differences in the LOS when we examined the data for those who were admitted with HCC as the secondary diagnosis (6.0 days in 2002 to 5.5 days in 2011, P-value for trend =0.09, Table 4).
TABLE 4.
Length of hospital stay, clinical outcomes, payer and hospital charges of HCC-related hospitalizations in the United States from 2002–2011.
| 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Slope | P Value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Length-of-stay [days, mean (SE)] | ||||||||||||
| Overall HCC-related | 6.5 (0.2) | 6.3 (0.3) | 6.2 (0.2) | 6.4 (0.2) | 6.0 (0.1) | 5.9 (0.1) | 6.0 (0.2) | 5.8 (0.1) | 5.8 (0.1) | 5.6 (0.1) | −0.090 | <0.001 |
| Primary diagnosis | 7.1 (0.2) | 6.9 (0.3) | 6.9 (0.4) | 6.8 (0.4) | 6.4 (0.1) | 6.1 (0.2) | 6.4 (0.2) | 6.2 (0.1) | 5.9 (0.2) | 5.9 (0.2) | −0.138 | <0.001 |
| Secondary diagnosis | 6.0 (0.2) | 5.8 (0.3) | 5.6 (0.2) | 6.2 (0.2) | 5.7 (0.2) | 5.8 (0.2) | 5.8 (0.2) | 5.6 (0.2) | 5.7 (0.1) | 5.5 (0.2) | −0.038 | 0.091 |
| Patient disposition (%) | ||||||||||||
| Routine discharge to home | 62.6 | 60.8 | 59.0 | 57.1 | 57.4 | 57.0 | 58.7 | 57.1 | 55.5 | 55.4 | −0.648 | 0.001 |
| Short-term hospital | 1.9 | 2.0 | 2.2 | 2.1 | 2.6 | 2.6 | 2.3 | 2.5 | 2.6 | 2.5 | 0.071 | 0.005 |
| Skilled nursing facility | 9.5 | 9.7 | 10.4 | 11.7 | 11.5 | 12.3 | 11.5 | 12.3 | 13.1 | 13.3 | 0.410 | <0.001 |
| Home healthcare | 11.6 | 13.8 | 14.5 | 15.5 | 15.3 | 15.8 | 16.4 | 16.4 | 17.9 | 18.1 | 0.605 | <0.001 |
| Against medical advice | 0.7 | 0.5 | 0.6 | 0.6 | 0.5 | 0.7 | 0.7 | 0.8 | 0.8 | 0.7 | 0.021 | 0.061 |
| Other (alive but destination unknown, died, etc.) | 13.7 | 13.2 | 13.3 | 13 | 12.7 | 11.6 | 10.4 | 10.9 | 10.1 | 10 | −0.460 | <0.001 |
| In-hospital mortality (%) | ||||||||||||
| Overall HCC-related | 13.5 | 13.1 | 13.1 | 12.5 | 12.4 | 11.3 | 10.3 | 10.4 | 9.6 | 9.9 | −0.470 | <0.001 |
| Primary diagnosis | 17.0 | 16.1 | 17.0 | 16.0 | 15.0 | 12.3 | 11.8 | 11.8 | 11.0 | 9.8 | −0.859 | <0.001 |
| Secondary diagnosis | 10.7 | 10.7 | 10.0 | 9.9 | 10.6 | 10.6 | 9.4 | 9.6 | 8.9 | 9.9 | −0.141 | 0.027 |
| Primary expected payer (%) | ||||||||||||
| Medicare | 44.4 | 44.3 | 44.2 | 44.9 | 43.1 | 45.7 | 42.8 | 43.2 | 43.7 | 45.4 | −0.023 | 0.841 |
| Medicaid | 16.3 | 17.4 | 16.3 | 16.4 | 18.0 | 16.1 | 18.0 | 18.4 | 19.2 | 19.4 | 0.327 | 0.006 |
| Private insurance (including HMO) | 32.2 | 32.1 | 32.9 | 31.1 | 28.9 | 30.0 | 31.9 | 29.5 | 29.0 | 26.7 | −0.513 | 0.006 |
| Self-pay | 3.9 | 2.7 | 3.4 | 4.1 | 4.2 | 3.5 | 3.2 | 4.7 | 4.0 | 3.7 | 0.063 | 0.343 |
| Others | 3.2 | 3.5 | 4.3 | 3.5 | 5.8 | 4.7 | 4.1 | 4.2 | 4.1 | 4.8 | 0.114 | 0.186 |
| Total charges [$, mean (SE)] | ||||||||||||
| Overall HCC-related | 32,405 (2,667.7) | 37,783 (3,400.7) | 35,070 (2,511.8) | 42,612 (3,336.8) | 38,093 (2,716.1) | 46,010 (3,602.7) | 54,820 (4,373.7) | 58,048 (4,600.5) | 57,686 (3,951.3) | 59,465 (4,487.8) | 3,286.6 | <0.001 |
| Primary diagnosis | 33188 (2,842.4) | 38028 (2,767.7) | 36468 (2,544.0) | 43271 (3,401.9) | 39359 (2,163.2) | 44921 (2,862.6) | 56404 (3,667.6) | 62514 (5,146.7) | 58293 (3,500.0) | 64397 (5,481.7) | 3,623.8 | <0.001 |
| Secondary diagnosis | 31,767 (2,716.3) | 37,588 (4,399.2) | 34,014 (2,717.3) | 42,111 (3,794.6) | 37,218 (3,363.3) | 46,739 (4,298.2) | 53,882 (5,076.8) | 55,523 (4,652.9) | 57,379 (4,412.5) | 57,128 (4,362.0) | 3,146.5 | <0.001 |
HCC, hepatocellular carcinoma; HMO, Health Maintenance Organization; SE, standard error.
When we analyzed disposition data, we found a significant decrease in the percentage of patients who were discharged directly to home (62.6% in 2002 versus 55.4% in 2011, P-value for trend =0.001). There was a shift in the discharge patterns toward skilled nursing facilities (9.5% in 2002 to 13.3% in 2011, P-value for trend <0.001) and home healthcare (11.6% in 2002 to 18.1% in 2011, P-value for trend <0.001).
The 2 main payers for the hospitalizations were Medicare (43–46%) and private insurance (27–33%). We observed a decrease in the percentage of patients with private insurance as the primary payer (32.2% in 2002 to 26.7% in 2011, P-value for trend =0.006, Table 4).
In-Hospital Mortality and Financial Charges for Hospitalizations Related to HCC
The overall in-hospital mortality of patients with HCC decreased significantly from 13.5% in 2002 to 9.9% in 2011 (P-value for trend <0.001). In the detailed analysis, in-hospital mortality rates significantly decreased regardless of whether patients were admitted with HCC as the primary (17% in 2002 to 9.8% in 2011, P-value for trend <0.001) or secondary diagnosis (10.7% in 2002 to 9.9% in 2011, P-value for trend =0.027, Table 4).
The overall financial charges per hospitalization increased substantially from $32,405 in 2002 to $59,465 in 2011 (P-value for trend <0.001, Table 4). The increase was observed for the hospitalizations in which HCC was the primary diagnosis ($33,188 in 2002 to $64,397 in 2011, P-value for trend <0.001) and secondary diagnosis ($31,767 in 2002 to $57,128 in 2011, P-value for trend <0.001) (Table 4). After accounting for inflation, the additional cost per hospitalization increased by $15,153 in 2011 in reference to the charges in 2002 (Figure).
FIGURE.
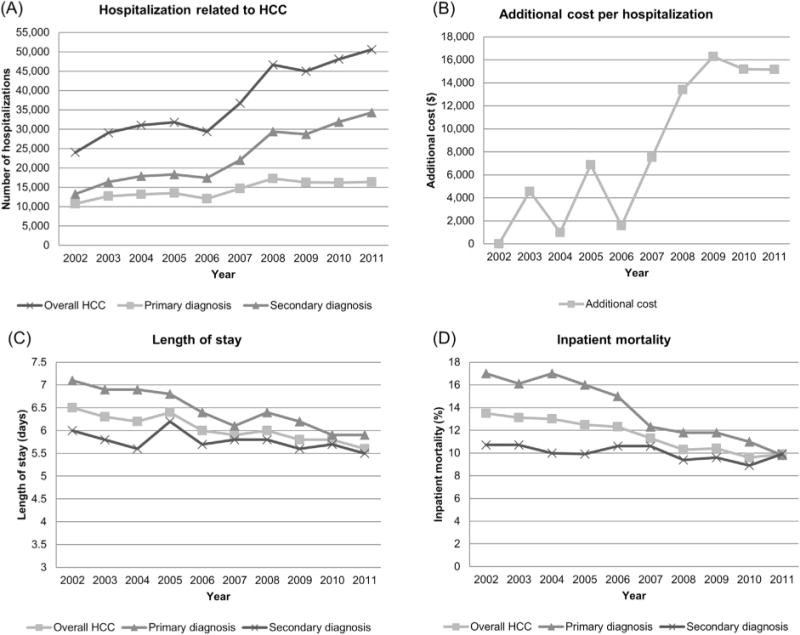
(A) Hospitalization related to the diagnosis of HCC in the United States from 2002–2011; (B) additional total hospital charges after adjusting for inflation for the diagnosis of HCC from 2002–2011, using the charges in 2002 as the reference; (C) average length-of-stay of hospitalization for the diagnosis of HCC from 2002–2011; and (D) inpatient mortality for the diagnosis of HCC from 2002–2011. HCC, hepatocellular carcinoma.
DISCUSSION
Our study has a few notable findings, including a temporal increase in the overall HCC-related hospitalization, particularly among those in whom HCC was the secondary diagnosis; a significant decrease in the percentage of hospitalized patients in the high-income bracket; a significant decrease in the average LOS for all hospitalized patients with HCC, notably for those with HCC as the primary diagnosis; a shift in the discharge patterns toward skilled nursing facilities or home healthcare; a significant decrease in the in-hospital mortality rate; and a significant increase in the financial charges related to hospitalization for patients with HCC.
The increase in the overall HCC-related hospitalizations, particularly among those with HCC as a secondary diagnosis likely reflects an increase in admissions due to underlying cirrhosis and end-stage liver disease– related complications such as hepatic encephalopathy, infection or sepsis, and acute renal failure.10,11
We found a significant decrease in the percentage of hospitalized patients in the high-income bracket. Previous studies have shown that a low socioeconomic status has been associated with chronic conditions including diabetes, obesity, metabolic syndrome, alcoholism and hepatitis C; all of which are risk factors for cirrhosis and have been shown to increase the risk for HCC.2,12,13 A plausible explanation for this is the expansion of accessibility to healthcare, and hence more patients in the lower income quartiles are being diagnosed and hospitalized with HCC and its complications. Furthermore, patients within a higher socioeconomic class are most likely to benefit from HCC screening and thus earlier detection. Early detection improves response to therapy, and thus reduces the complications and frequency of hospitalizations of these patients.14–16 However, the effect of early detection is expected to be small as our study population focused mainly on hospitalized patients with HCC, which are usually patients with advanced HCC.
We also observed a significant decrease in the average LOS for all hospitalized patients with HCC, notably for those with HCC as the primary diagnosis. The reasons behind this observation are not clear; however, it is plausible that this reflects the improvement in the treatment modalities for HCC and the improvement in the overall medical care for hospitalized patients with cirrhosis. These factors might also lead to a significant decrease in the in-hospital mortality rate for patients with HCC. Additionally, the shortened LOS might be due to a shift in transitioning care toward skilled nursing facilities and home healthcare once a patient can otherwise be discharged from the hospital. Use of these transition services has increased over the last decade.17
Despite the decrease in LOS and in-hospital mortality rate, the overall inflation-adjusted financial charges for hospitalizations related to HCC increased substantially during the study period, regardless of whether HCC was the primary or secondary cases for admission. This is likely due to the increase in the overall healthcare costs in the United States and the increased use of healthcare resources with access to more advanced and more expensive therapeutic modalities for HCC, such as liver transplantation, surgical resection, ablation therapy, etc. As seen in Supplementary Tables 1 and 2, the rate of such interventions appear to be decreasing over the past few years though the cost of hospitalization during which these interventions were performed seems to have increased significantly. These results should be interpreted cautiously owing to inherent limitations of the NIS database in providing details of each hospitalization. A vast majority of hospitalized patients with HCC were admitted to teaching hospitals in the urban area. This observation is not surprising because of the complexity of the disease and the treatment which ideally requires a multidisciplinary approach—services which can be provided more readily in tertiary or quaternary care centers.
Our study has a few limitations. We used ICD-9 codes as the primary way to identify subjects with HCC. Additionally, NIS data does not include specifics on laboratory test results, imaging modalities, as well as the staging of the HCC. Thus, we cannot further analyze the effect of these parameters on LOS and in-hospital mortality. Lastly, the mortality rate reported herein is limited to only in-hospital mortality. We do not have information to extrapolate our results for the short- and long-term outcomes of these patients. Despite these shortcomings, our study is strengthened by the use of a large database that represents many US medical centers and patient populations to capture the inpatient burden of HCC.
CONCLUSIONS
Despite the decrease in in-hospital mortality rate and LOS, overall hospitalizations and financial burden associated with HCC continue to increase over the last decade in the United States.
Supplementary Material
Acknowledgments
This study is supported by K08 AA016570 from the National Institutes of Health/National Institute on Alcohol Abuse and Alcoholism, 1I01CX000361-01 from the Veterans Affairs Research and Administration and W81XWH-12-1-0497 from U. S. Department of Defense, United States (All to S.L.).
Appendix A. Supporting information
Supplementary data associated with this article can be found in the online version at http://dx.doi.org/10. 1016/j.amjms.2017.05.016.
Footnotes
AUTHORS CONTRIBUTION
R.J. and R.S.—study design; A.S. and A.L.—literature search; R.J., S.L. and R.S.—analysis and interpretation of data; R.J., A.L., A.S., K.J.—drafted manuscript; S.L. and R.S.—made critical revisions to manuscript.
The authors have no conflicts of interest to disclose.
Contributor Information
Raxitkumar Jinjuvadia, Division of Gastroenterology and Hepatology, Henry Ford Hospital, Detroit, Michigan.
Augustine Salami, Division of Gastroenterology and Hepatology, Henry Ford Hospital, Detroit, Michigan.
Adrienne Lenhart, Division of Gastroenterology and Hepatology, Henry Ford Hospital, Detroit, Michigan.
Kartikkumar Jinjuvadia, Division of Gastroenterology and Hepatology, Wayne State University, Detroit, Michigan.
Suthat Liangpunsakul, Division of Gastroenterology/Hepatology, Roudebush Veterans Administration Medical Center, Indiana University School of Medicine, Indianapolis, Indiana; Department of Biochemistry and Molecular Biology, Indiana University School of Medicine, Indianapolis, Indiana.
Reena Salgia, Division of Gastroenterology and Hepatology, Henry Ford Hospital, Detroit, Michigan.
References
- 1.Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127(12):2893–917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011;365(12):1118–27. doi: 10.1056/NEJMra1001683. [DOI] [PubMed] [Google Scholar]
- 3.El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology. 2012;142(6):1264–1273.e1. doi: 10.1053/j.gastro.2011.12.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Altekruse SF, McGlynn KA, Reichman ME. Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. J Clin Oncol. 2009;27(9):1485–91. doi: 10.1200/JCO.2008.20.7753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.El-Serag HB, Davila JA, Petersen NJ, et al. The continuing increase in the incidence of hepatocellular carcinoma in the United States: an update. Ann Intern Med. 2003;139(10):817–23. doi: 10.7326/0003-4819-139-10-200311180-00009. [DOI] [PubMed] [Google Scholar]
- 6.Salgia R, Singal AG. Hepatocellular carcinoma and other liver lesions. Med Clin North Am. 2014;98(1):103–18. doi: 10.1016/j.mcna.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 7.Thein HH, Isaranuwatchai W, Campitelli MA, et al. Health care costs associated with hepatocellular carcinoma: a population-based study. Hepatology. 2013;58(4):1375–84. doi: 10.1002/hep.26231. [DOI] [PubMed] [Google Scholar]
- 8.Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet. 2012;379(9822):1245–55. doi: 10.1016/S0140-6736(11)61347-0. [DOI] [PubMed] [Google Scholar]
- 9.AHRQ. National Inpatient Sample database. Available from: http://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp.
- 10.Nguyen GC, Segev DL, Thuluvath PJ. Nationwide increase in hospitalizations and hepatitis C among inpatients with cirrhosis and sequelae of portal hypertension. Clin Gastroenterol Hepatol. 2007;5(9):1092–9. doi: 10.1016/j.cgh.2007.04.027. [DOI] [PubMed] [Google Scholar]
- 11.Volk ML, Tocco RS, Bazick J, et al. Hospital readmissions among patients with decompensated cirrhosis. Am J Gastroenterol. 2012;107(2):247–52. doi: 10.1038/ajg.2011.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Loucks EB, Rehkopf DH, Thurston RC, et al. Socioeconomic disparities in metabolic syndrome differ by gender: evidence from NHANES III. Ann Epidemiol. 2007;17(1):19–26. doi: 10.1016/j.annepidem.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 13.Rogers R, Eagle TF, Sheetz A, et al. The relationship between childhood obesity, low socioeconomic status, and race/ethnicity: lessons from Massachusetts. Child Obes. 2015;11:691–5. doi: 10.1089/chi.2015.0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Della Corte C, Colombo M. Surveillance for hepatocellular carcinoma. Semin Oncol. 2012;39(4):384–98. doi: 10.1053/j.seminoncol.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 15.Taura N, Hamasaki K, Nakao K, et al. Clinical benefits of hepatocellular carcinoma surveillance: a single-center, hospital-based study. Oncol Rep. 2005;14(4):999–1003. [PubMed] [Google Scholar]
- 16.Yuen MF, Cheng CC, Lauder IJ, et al. Early detection of hepatocellular carcinoma increases the chance of treatment: Hong Kong experience. Hepatology. 2000;31(2):330–5. doi: 10.1002/hep.510310211. [DOI] [PubMed] [Google Scholar]
- 17.Medicare Payment Advisory Commission. A Data Book: Healthcare Spending and the Medicare Program. 2014 Jun; [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


