Abstract
Purpose
Prior research regarding the impact of mental health on upper-extremity musculoskeletal function and recovery have frequently grouped catastrophizing, anxiety, and depression. This study was designed to define the relative prevalence of heightened anxiety versus depressive symptoms among a patient population seeking upper-extremity care and to determine if those prevalences varied according to the symptomatic condition.
Methods
All adult patients presenting to a tertiary upper-extremity orthopaedic center between 6/1/2016 and 11/30/2016 (n=3315) completed the PROMIS Anxiety and Depression Computer Adaptive Tests (CATs). Descriptive statistics and multivariable linear regression assessed differences in average PROMIS scores between demographic and diagnostic groups. Patients were also analyzed according to crossing thresholds for heightened Anxiety and Depression scores based on established linkage tables with the Generalized Anxiety Disorder 7 and Patient Health Questionnaire-9 Depression scales respectively. Pearson chi square analysis and binary logistic regression were performed to determine if the proportion of patients crossing these thresholds varied according to the primary symptomatic condition, while accounting for patient age, sex, and race.
Results
African-American patients and those with carpal tunnel syndrome, trapeziometacarpal arthritis, or shoulder conditions reported significantly higher PROMIS Anxiety scores. Higher PROMIS Depression scores only varied by diagnosis. Seventeen percent of patients exceeded the Anxiety symptoms score threshold while 10% of patients exceeded the depressive symptom threshold. In logistic regression modeling, the likelihood of exceeding the anxiety threshold varied by diagnosis and was increased in African-American patients, and females. African-American race was associated with exceeding the depression threshold while accounting for sex and diagnosis.
Conclusions
Patients with upper-extremity conditions more frequently report heightened anxiety than heightened depression. Patient race and diagnosis are independent predictors of anxiety among patients seeking care for upper-extremity conditions.
Level of Evidence
Diagnostic Level II
Keywords: anxiety, depression, PROMIS, upper extremity
INTRODUCTION
The substantial impact of psychosocial factors on patient outcomes has been well established in the orthopedic literature1–6. In patients with upper-extremity musculoskeletal conditions there is a strong correlation between psychological distress and pain intensity with both preoperative and postoperative physical impairment7–11. Mental health measures have a stronger association with patient-reported symptoms of hand arthritis than more objective measures, such as radiographic disease progression and range of motion12,13. Despite increasing evidence linking the symptoms of psychological distress to patient-reported pain and function, further study is needed to define the incidence of heightened anxiety and depression among patients with upper-extremity musculoskeletal conditions.
Twelve percent of 190 patients presenting to one of three academic hospital-based hand surgeons met criteria for major depression based on the PHQ-9 Patient Health Questionnaire14. Symptoms of anxiety and pain interference correlated with depression in this patient sample, but the prevalence of these psychological disorders was not defined. Gaining further understanding of the epidemiology of mental health conditions among patients seeking upper-extremity care will aid our ability to suggest mental health intervention, optimize care, and guide future research.
The National Institute of Health developed the Patient-Reported Outcomes Measurement Information System (PROMIS) to effectively assess a wide range of health domains, including those of anxiety and depression15,16. In its computer adaptive testing format, PROMIS assessments selectively draw from large pools of validated questions, providing a sensitive measure of mental health domains including depression and anxiety while only requiring a patient to answer four to twelve questions17,18.
This study’s primary aim was to determine the prevalence of heightened anxiety and depression in patients seeking specialty care for an upper-extremity musculoskeletal condition. Second, we aimed to determine if the magnitude of PROMIS scores and prevalence of anxiety and depression symptoms varied between upper-extremity musculoskeletal conditions.
METHODS
This cross-sectional study evaluated all new adult patients presenting to one of 12 upper extremity surgeons at an orthopedic tertiary care clinic between 6/1/2016 and 11/30/2016. Our study was exempt from institutional IRB approval as it collected de-identified patient data. All clinic patients used a computer tablet (iPad mini, Apple, Cupertino, CA) at check-in that was preloaded with PROMIS Anxiety-v1.0 and PROMIS Depression-v1.0. PROMIS scores were automatically uploaded into the patients’ electronic health record immediately following completion.
PROMIS modules have been developed to be scored with a T-metric so that a score of 50 represents the normative population mean with a standard deviation of 1019. Higher scores represent more of each health domain. For example, a PROMIS Anxiety score of 60 represents anxiety symptoms one standard deviation greater than the normative population, while a Depression score of 40 represents less depressive symptoms than the normative population. A minimal clinically important difference (MCID) of 3.0 to 5.5 points has been suggested, with score changes of 3.0 to 4.5 in mental health domains being clinically relevant in a population of cancer patients20,21. However, because a clinically important difference for upper extremity patients has not yet been established, we chose to utilize both the upper and lower ends of the range (3 to 4.5) as a proxy for a clinically relevant difference between groups.
The PROMIS Anxiety module measures emotional distress caused by fear, anxious misery, hyperarousal, and related somatic symptoms17. Using item response theory (IRT), a crosswalk linking table exists to convert PROMIS Anxiety scores to the GAD-7, a seven-item instrument established to identify likely cases of Generalized Anxiety Disorder (GAD). A score of 10 or higher on the GAD-7 maximizes the sensitivity and specificity when judged against a diagnosis of GAD22,23. A score of 10 on the GAD-7 corresponds to a PROMIS anxiety score of 62.324. Thus, a score of 62.3 was chosen as a minimum threshold value indicating a patient being affected by anxiety symptoms for PROMIS Anxiety for this study.
PROMIS Depression captures the respondent’s negative mood, views of self, affect, and social cognition17. A linkage table has been developed to convert between PROMIS Depression scores and the Patient Health Questionnaire-9, or PHQ-9. A score greater than 10 on the PHQ-9, which corresponds to a PROMIS Depression score of 59.9 or greater, indicates moderate depression and allows for the highest sensitivity and specificity when judged against a diagnosis of major depression25,26. Therefore, a minimum threshold PROMIS Depression score of 59.9 was chosen indicating a patient being affected by depressive symptoms.
Statistical Analysis
Descriptive univariate statistics were used to evaluate the demographic data, average PROMIS scores, and prevalence of patients scoring above the designated PROMIS diagnostic thresholds in the study population. One-way ANOVA with Tukey’s post-hoc analysis evaluated differences in average PROMIS scores between demographic groups. Pearson’s chi-square analysis evaluated differences in the prevalence of those reaching PROMIS score thresholds between demographic groups.
Patients were then categorized as presenting for treatment of one of the following conditions: carpal tunnel syndrome, cubital tunnel syndrome, trapeziometacarpal arthritis, trigger finger(s), De Quervain tenosynovitis, Dupuytren contracture, ganglion cyst, rotator cuff tendinopathy, shoulder osteoarthritis, adhesive capsulitis, or other (Appendix 1). Pearson’s chi-square analyzed the differences in prevalence of patients reaching PROMIS score thresholds between diagnostic groups.
Multivariable linear regression with forced entry was used to model the effects of age (continuous variable), sex (categorically defined with male as the reference group), race (categorically defined with Caucasian as the reference group), and upper extremity diagnosis (categorically defined with ganglion cyst, the group with the lowest frequency of Anxiety or Depression scores over the threshold, as the reference group) on the continuous dependent variable, PROMIS Anxiety score. Dummy variables were utilized for the categorical variables race and upper extremity diagnosis. This same procedure was repeated for the dependent variable, PROMIS Depression score.
Binary logistic regression was used to model the relationship between reaching the Anxiety score threshold (dependent variable) with forced entry of age (continuous level), sex (categorically defined with males as the reference group), race (categorically defined with Caucasians as the reference group), and diagnosis (categorically defined with ganglion cyst as the reference group). A backwards stepwise selection procedure was used to establish the final model with an alpha of .05 for removal. Model explanatory power and fit was assessed using the c-statistic and the Hosmer-Lemeshow lack-of-fit test. An unadjusted alpha of .05 level of significance was used for all tests. This same methodology was used to create a second regression model for the dependent variable of reaching the Depression score threshold.
RESULTS
3388 new patients presented during the study inclusion period. Of this group, 3315 had valid PROMIS scores necessary for study inclusion. The study population was predominantly female (54.2%), Caucasian (84.9%), and presented for hand conditions as opposed to shoulder conditions (64.7%). Patients averaged 53 (SD 17) years of age. The study population’s average PROMIS Anxiety (51.6, SD 10.5) and Depression scores (46.4, SD 9.8) approximated the theoretical population mean of 50. African-American patients reported higher Anxiety scores than patients of other races (+5.3, 95% CI 4.2 – 6.5). There were no other clinically relevant differences in average PROMIS scores between demographic groups.
When accounting for diagnosis and demographic factors via linear regression, African-American patients and those with carpal tunnel syndrome, trapeziometacarpal arthritis, or shoulder conditions reported significantly higher PROMIS Anxiety scores than Caucasian patients or those with a diagnosis of a ganglion cyst (Table 1). A diagnosis of carpal tunnel syndrome, trapeziometacarpal arthritis, or adhesive capsulitis were the only statistically significant predictors of increasing Depression scores in multivariable analysis.
Table 1.
Significant independent predictors of increasing PROMIS scores on multivariable linear regression.
| PROMIS Anxiety | PROMIS Depression | |||
|---|---|---|---|---|
| Predictors | Unstandardized β coefficient | 95% CI | Unstandardized β coefficient | 95% CI |
| African-American race† | 5.1** | 4.0–6.3 | 2.9 | 1.8–3.9 |
| Age | 0.04 | 0.01–0.06 | 0.05 | 0.02–0.07 |
| ††Female Sex | 2.3 | 1.6–3.0 | 1.6 | 0.9–2.3 |
| Diagnosis‡ | ||||
| Adhesive Capsulitis | 7.5** | 3.6–11.3 | 5.0** | 1.3–8.6 |
| Rotator Cuff Tear | 4.8** | 2.3–7.3 | ||
| Carpal Tunnel Syndrome | 4.5** | 2.0–7.0 | 3.0* | 0.6–5.3 |
| Shoulder Osteoarthritis | 4.1* | 1.3–6.9 | ||
| Trapeziometacarpal Arthritis | 3.2* | 0.5–5.9 | 3.0* | 0.4–5.5 |
Reference category: Caucasian race
Reference category: male sex
Reference category: ganglion cysts
Clinically relevant at Δ3 points
Clinically relevant at Δ4.5 points
Anxiety and Depression Thresholds
Overall, 16.6% of the study population exceeded the PROMIS Anxiety threshold while 9.5% of the population exceeded the threshold for Depression, 85% of whom also met the threshold for Anxiety (p<0.05). African-American patients, and those presenting with shoulder or elbow complaints, were more likely than Caucasian or patients with hand complaints to exceed thresholds for being affected by anxiety and depression. Females reported anxiety more frequently than males (Table 2). There were no differences in age between affected and unaffected patients.
Table 2.
Percentage of patients reaching the PROMIS Anxiety and Depression score thresholds.
| Anxiety ≥62.3) | Depression (≥59.9) | |
|---|---|---|
|
| ||
| Female | 18.5% (n=333)* | 9.9% (n=177) |
| Male | 14.4% (n=218) | 9.0% (n=136) |
|
| ||
| African-American | 36.5% (n=133)* | 18.7% (n=68)* |
| Caucasian | 14.0% (n=393) | 8.3% (n=232) |
|
| ||
| Shoulder/Elbow | 21.1% (n=247)* | 10.7% (n=124)* |
| Hand | 14.2% (n=304) | 8.8% (n=189) |
Statistically significant at p<0.05
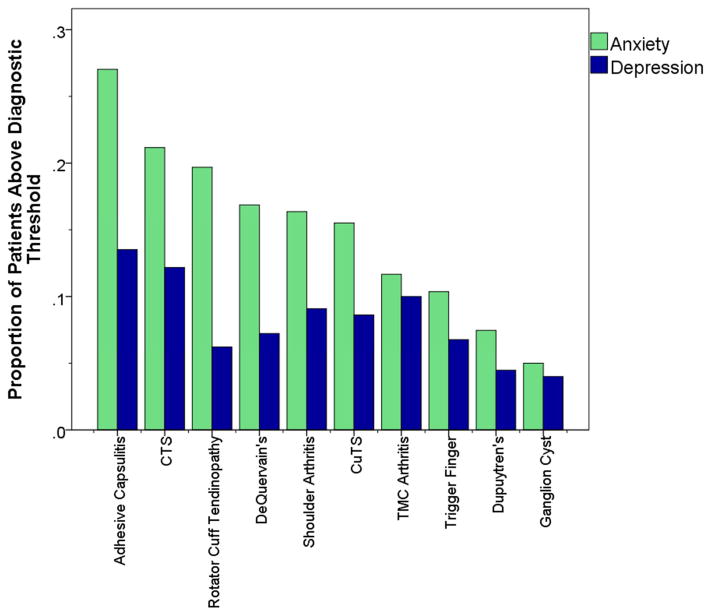
Patients with adhesive capsulitis, carpal tunnel syndrome, or rotator cuff tendinopathy reported the highest prevalence of PROMIS Anxiety scores above the treatment threshold (Figure 1), while those with ganglion cysts or Dupuytren’s contracture reported the lowest. Patients with trigger fingers or ganglion cysts had the lowest rates of Depression scores above the threshold.
Figure 1.
Proportion of patients reaching PROMIS Anxiety and Depression treatment thresholds. Error bars represent 95% confidence intervals.
The binary logistic regression model for predicting anxiety symptoms over the threshold was statistically significant (LR Chi-square=141.2, df=4, p<0.05) with a c-statistic of 0.63. African-American race (OR 3.6, 95% CI 2.8–4.5) and female sex (OR 1.3, 95%CI 1.1–1.6) as well as several shoulder conditions (adhesive capsulitis OR 8.6, 95%CI 2.7–27.7; rotator cuff tendinopathy OR 5.5, 95% CI 2.1–114.7; shoulder osteoarthritis OR 4.6, 95% CI 1.6–13.2) and hand conditions (carpal tunnel syndrome OR 5.0, 95% CI 1.9–13.4; cubital tunnel syndrome OR 3.7, 95% CI 1.2–11.9; trapeziometacarpal arthritis OR 3.2, 95% CI 1.1–9.2) were significant predictors for being affected by anxiety. The overall regression model for predicting depression was also significant (LR Chi-square= 33.8, df=4, p<0.05, c-statistic=0.56), with African-American race (OR 2.7, 95% CI 1.6–4.6) as the sole predictor associated with being affected by depressive symptoms exceeding the threshold.
DISCUSSION
There is substantial variability in the reported prevalence of anxiety (13–29%) and depression (7–38%) in orthopedic patient populations. This is likely due to the heterogeneity of the populations studied and the instruments used to measure these psychological parameters5,6,14,27–31. Our study delivered PROMIS CATs to all patients presenting to our institution’s upper-extremity clinic. Patients complete PROMIS modules at every visit, providing a large sample of PROMIS data and minimizing selection bias. Our results are consistent with smaller studies in which the prevalence of anxiety was equal to, or higher than, that of depression in upper-extremity populations5,14,31. This finding was substantiated in a meta-analysis that also identified anxiety (21.3%) as more prevalent than depression (19.9%) in patients with osteoarthritis32. Although our estimated prevalences of anxiety (16.6%) and depression (9.5%) were slightly smaller, it is clear that there is a meaningful prevalence of psychological distress in the form of both anxiety and depression present in patients with upper-extremity musculoskeletal conditions. If unable to universally assess all patients, our data indicate that screening for anxiety may be most efficient in women, African-American patients, and patients with select diagnoses among those who present to upper extremity clinics.
Ganglion cysts and Dupuytren’s contracture were associated with the lowest levels of anxiety and depression scores. We suspect that this is attributable to those conditions frequently being painless. In our experience, patients are most likely to exhibit catastrophic thinking and become anxious when in pain. To this end, surgeons can provide a great service by explaining conditions in an understandable manner that builds resiliency and conveys empathy while eliminating misconceptions about conditions.
The orthopedic literature often group coping abilities, anxiety, and depression together as “psychological distress”, but we would argue it may be prudent to view these entities separately. In a study of the association between psychological distress and DASH and QuickDASH scores, both traditional screening tools for depression (Center for Epidemiologic Studies Depression Scale) and anxiety (Pain Anxiety Symptoms Scale) each remained as significant independent predictors in multivariable modeling, which indicated that each contributed a unique influence on patients’ perceived physical function33. Furthermore, in patients after distal radius fracture surgery, catastrophic thinking (poor coping strategy), but not depressive symptoms, predicted finger stiffness34. Similarly, anxiety, but not depression, was associated with reduced satisfaction in a cohort after carpal tunnel release8. Thus, given their differing prevalences and potentially unique impact on a patient’s response to treatment, we see value in recognizing anxiety and depressive symptoms as two distinct entities in both research and patient care8,33.
The identification of increased mean anxiety levels among females is consistent with multiple publications35–37. However, the greater number of African-American patients exceeding the anxiety and depression thresholds contradicts national epidemiologic studies38–41. Among 11,710 Americans, African-Americans and Caribbean Blacks were less likely than non-Hispanic white Americans to meet DSM-IV criteria for generalized anxiety disorder, panic disorder, and social anxiety in face-to-face interviews40. Reduced prevalence of anxiety disorders among non-Hispanic Blacks was confirmed by Breslau et al41. The discrepancy between our data and findings from the general population may be related to study methodology or access to healthcare. First, the referenced epidemiologic studies each used personal interviews, which risks responders minimizing anxiety or depressive symptoms as opposed our patients completing a self-administered survey. Second, in epidemiologic studies of the United States, minority populations are often more socio-economically disadvantaged which may prevent healthcare access and reduce the likelihood of mental health diagnoses. The National Institute of Mental Health reported that black adults sought mental health care only 52% as frequently as white adults, with the most commonly cited reason being cost of treatment or lack of insurance42. Notably, all patients in our study have demonstrated the resources to access specialty orthopedic care which likely removed any racially-based disparities in access to care that affect population studies. However, we cannot rule out socioeconomic status as a confounding variable for differences that we attributed to race. The higher average anxiety scores among African American patients was less surprising as epidemiologic studies report that, when affected, Hispanic and black individuals have increased severity, duration, and overall anxiety burden38,39.
The cross-sectional nature of this study limits our ability to determine if the prevalence of anxiety and depression has an impact on treatment choice. Additionally, the upper-extremity diagnoses for this study are based on ICD-10 codes which do not allow for the assessment of the severity or duration of symptoms. Finally, this study uses patient-reported symptoms from the PROMIS Anxiety and Depression CATs to determine clinically relevant anxiety and depressive symptoms. This is not equivalent to an evaluation and diagnosis by a mental health professional. There is, however, evidence that the thresholds used in this study indicate symptoms that may warrant intervention based on other established mental health assessments22,24,43. Using thresholds to categorize patients is often needed when delivering treatment (e.g., perform a surgery or not, prescribe a drug or not) and is frequently used to characterize populations. However, some would argue against such categorization and encourage a focus on all health facets as a continuum. Thus, it is reasonable to assume that some patients who scored below the threshold would still benefit from intervention to reduce anxiety or depression.
The Institute of Medicine has called for an improved understanding of the interactions between social, behavioral, and physical health, in order to best serve our patients44. This study used a standardized metric, PROMIS, that effectively and efficiently assesses mental health, to reveal a substantial prevalence of anxiety, and to a lesser degree depression, that may warrant treatment in a population of patients with upper-extremity conditions. In high risk groups, such as females, African Americans, and patients with adhesive capsulitis or carpal tunnel syndrome, it is especially important for providers to be aware of the negative effect depression and anxiety can have on patient outcomes10,11,45,46. We hope that upper extremity surgeons will screen for these conditions, direct patients with heightened anxiety and depression toward treatment, and also remain cognizant of their language during their interactions with patients to best aid in their recovery.
Acknowledgments
Funding: Research reported in this publication was supported by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR000448 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH. NIH sub award number TL1 TR000449 – ICTS Clinical Research Predoctoral Training Program.
Appendix 1. ICD-10 codes for categorizing diagnoses
| Carpal Tunnel Syndrome | G56.00 | G56.03 | G56.11 |
| G56.01 | G56.10 | G56.12 | |
| G56.02 | |||
|
| |||
| Cubital Tunnel Syndrome | G56.20 | G56.21 | G56.22 |
| G56.23 | |||
|
| |||
| Trapeziometacarpal Arthritis | M18.9 | M18.12 | M18.10 |
| M18.0 | M18.31 | M18.51 | |
| M18.11 | M18.2 | ||
|
| |||
| Trigger Finger | M65.30 | M65.329 | M65.342 |
| M65.311 | M65.331 | M65.349 | |
| M65.312 | M65.332 | M65.351 | |
| M65.319 | M65.339 | M65.352 | |
| M65.321 | M65.341 | M65.359 | |
| M65.322 | |||
|
| |||
| Ganglion Cyst | M67.431 | M67.40 | M67.439 |
| M67.441 | M67.442 | M67.449 | |
| M67.432 | |||
|
| |||
| Dupuytren Contracture | M72.0 | ||
|
| |||
| De Quervain Tendonitis | M65.4 | ||
|
| |||
| Rotator Cuff Tendinopathy | M75.100 | M75.111 | M75.121 |
| M75.101 | M75.112 | M75.122 | |
| M75.102 | M75.120 | ||
|
| |||
| Shoulder Osteoarthritis | M19.011 | M19.019 | M19.112 |
| M19.012 | M19.111 | M19.211 | |
|
| |||
| Adhesive Capsulitis | M75.00 | M75.01 | M75.02 |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rosenberger PH, Jokl P, Ickovics J. Psychosocial factors and surgical outcomes: an evidence-based literature review. J Am Acad Orthop Surg. 2006;14(7):397–405. doi: 10.5435/00124635-200607000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Gatchel RJ, Polatin PB, Mayer TG. The dominant role of psychosocial risk factors in the development of chronic low back pain disability. Spine (Phila Pa 1976) 1995;20(24):2702–2709. doi: 10.1097/00007632-199512150-00011. [DOI] [PubMed] [Google Scholar]
- 3.Burton AK, Tillotson KM, Main CJ, Hollis S. Psychosocial predictors of outcome in acute and subchronic low back trouble. Spine (Phila Pa 1976) 1995;20(6):722–728. doi: 10.1097/00007632-199503150-00014. [DOI] [PubMed] [Google Scholar]
- 4.Khatib Y, Madan A, Naylor JM, Harris IA. Do Psychological Factors Predict Poor Outcome in Patients Undergoing TKA? A Systematic Review. Clin Orthop Relat Res. 2015;473(8):2630–2638. doi: 10.1007/s11999-015-4234-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koorevaar RC, van’t Riet E, Gerritsen MJ, Madden K, Bulstra SK. The Influence of Preoperative and Postoperative Psychological Symptoms on Clinical Outcome after Shoulder Surgery: A Prospective Longitudinal Cohort Study. PLoS One. 2016;11(11):e0166555. doi: 10.1371/journal.pone.0166555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duivenvoorden T, Vissers MM, Verhaar JA, et al. Anxiety and depressive symptoms before and after total hip and knee arthroplasty: a prospective multicentre study. Osteoarthritis Cartilage. 2013;21(12):1834–1840. doi: 10.1016/j.joca.2013.08.022. [DOI] [PubMed] [Google Scholar]
- 7.Nunez F, Vranceanu AM, Ring D. Determinants of pain in patients with carpal tunnel syndrome. Clin Orthop Relat Res. 2010;468(12):3328–3332. doi: 10.1007/s11999-010-1551-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hobby JL, Venkatesh R, Motkur P. The effect of psychological disturbance on symptoms, self-reported disability and surgical outcome in carpal tunnel syndrome. J Bone Joint Surg Br. 2005;87(2):196–200. doi: 10.1302/0301-620x.87b2.15055. [DOI] [PubMed] [Google Scholar]
- 9.Lozano Calderon SA, Paiva A, Ring D. Patient satisfaction after open carpal tunnel release correlates with depression. J Hand Surg Am. 2008;33(3):303–307. doi: 10.1016/j.jhsa.2007.11.025. [DOI] [PubMed] [Google Scholar]
- 10.London DA, Stepan JG, Boyer MI, Calfee RP. The impact of depression and pain catastrophization on initial presentation and treatment outcomes for atraumatic hand conditions. J Bone Joint Surg Am. 2014;96(10):806–814. doi: 10.2106/JBJS.M.00755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vranceanu AM, Jupiter JB, Mudgal CS, Ring D. Predictors of pain intensity and disability after minor hand surgery. J Hand Surg Am. 2010;35(6):956–960. doi: 10.1016/j.jhsa.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Lozano-Calderon SA, Souer JS, Jupiter JB, Ring D. Psychological differences between patients that elect operative or nonoperative treatment for trapeziometacarpal joint arthrosis. Hand (N Y) 2008;3(3):271–275. doi: 10.1007/s11552-008-9098-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Becker SJ, Makarawung DJ, Spit SA, King JD, Ring D. Disability in patients with trapeziometacarpal joint arthrosis: incidental versus presenting diagnosis. J Hand Surg Am. 2014;39(10):2009–2015. e2008. doi: 10.1016/j.jhsa.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 14.Oflazoglu K, Mellema JJ, Menendez ME, Mudgal CS, Ring D, Chen NC. Prevalence of and Factors Associated With Major Depression in Patients With Upper Extremity Conditions. J Hand Surg Am. 2016;41(2):263–269. e261–267. doi: 10.1016/j.jhsa.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 15.Cella D, Riley W, Stone A, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63(11):1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stone AA, Broderick JE, Junghaenel DU, Schneider S, Schwartz JE. PROMIS fatigue, pain intensity, pain interference, pain behavior, physical function, depression, anxiety, and anger scales demonstrate ecological validity. J Clin Epidemiol. 2016;74:194–206. doi: 10.1016/j.jclinepi.2015.08.029. [DOI] [PubMed] [Google Scholar]
- 17.Pilkonis PA, Choi SW, Reise SP, et al. Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS(R)): depression, anxiety, and anger. Assessment. 2011;18(3):263–283. doi: 10.1177/1073191111411667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Amtmann D, Cook KF, Jensen MP, et al. Development of a PROMIS item bank to measure pain interference. Pain. 2010;150(1):173–182. doi: 10.1016/j.pain.2010.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bevans M, Ross A, Cella D. Patient-Reported Outcomes Measurement Information System (PROMIS): efficient, standardized tools to measure self-reported health and quality of life. Nurs Outlook. 2014;62(5):339–345. doi: 10.1016/j.outlook.2014.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yost KJ, Eton DT, Garcia SF, Cella D. Minimally important differences were estimated for six Patient-Reported Outcomes Measurement Information System-Cancer scales in advanced-stage cancer patients. J Clin Epidemiol. 2011;64(5):507–516. doi: 10.1016/j.jclinepi.2010.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amtmann D, Kim J, Chung H, Askew RL, Park R, Cook KF. Minimally important differences for Patient Reported Outcomes Measurement Information System pain interference for individuals with back pain. J Pain Res. 2016;9:251–255. doi: 10.2147/JPR.S93391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 23.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 24.Appendix Table 34: Raw Score to T-Score Conversion Table (IRT Fixed Parameter Calibration Linking) for GAD-7 to PROMIS Anxiety. PROsetta Stone - PROMIS Anxiety and GAD-7.
- 25.Appendix Table 46: Raw Score to T-Score Conversion Table (IRT Fixed Parameter Calibration Linking) for PHQ-9 to PROMIS Depression PROsetta Stone - PROMIS Depression and PHQ-9.
- 26.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ding H, Tang Y, Xue Y, et al. A report on the prevalence of depression and anxiety in patients with frozen shoulder and their relations to disease status. Psychol Health Med. 2014;19(6):730–737. doi: 10.1080/13548506.2013.873814. [DOI] [PubMed] [Google Scholar]
- 28.Degen RM, MacDermid JC, Grewal R, Drosdowech DS, Faber KJ, Athwal GS. Prevalence of Symptoms of Depression, Anxiety, and Posttraumatic Stress Disorder in Workers With Upper Extremity Complaints. J Orthop Sports Phys Ther. 2016;46(7):590–595. doi: 10.2519/jospt.2016.6265. [DOI] [PubMed] [Google Scholar]
- 29.Wood TJ, Thornley P, Petruccelli D, Kabali C, Winemaker M, de Beer J. Preoperative Predictors of Pain Catastrophizing, Anxiety, and Depression in Patients Undergoing Total Joint Arthroplasty. J Arthroplasty. 2016;31(12):2750–2756. doi: 10.1016/j.arth.2016.05.056. [DOI] [PubMed] [Google Scholar]
- 30.Demir B, Gursu S, Yildirim T, Er T. Evaluation of anxiety levels in patients with chronic orthopedic diseases. Acta Orthop Traumatol Turc. 2012;46(6):420–424. doi: 10.3944/aott.2012.2756. [DOI] [PubMed] [Google Scholar]
- 31.Archer KR, Abraham CM, Obremskey WT. Psychosocial Factors Predict Pain and Physical Health After Lower Extremity Trauma. Clin Orthop Relat Res. 2015;473(11):3519–3526. doi: 10.1007/s11999-015-4504-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stubbs B, Aluko Y, Myint PK, Smith TO. Prevalence of depressive symptoms and anxiety in osteoarthritis: a systematic review and meta-analysis. Age Ageing. 2016;45(2):228–235. doi: 10.1093/ageing/afw001. [DOI] [PubMed] [Google Scholar]
- 33.Niekel MC, Lindenhovius AL, Watson JB, Vranceanu AM, Ring D. Correlation of DASH and QuickDASH with measures of psychological distress. J Hand Surg Am. 2009;34(8):1499–1505. doi: 10.1016/j.jhsa.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 34.Teunis T, Bot AG, Thornton ER, Ring D. Catastrophic Thinking Is Associated With Finger Stiffness After Distal Radius Fracture Surgery. J Orthop Trauma. 2015;29(10):e414–420. doi: 10.1097/BOT.0000000000000342. [DOI] [PubMed] [Google Scholar]
- 35.McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. 2011;45(8):1027–1035. doi: 10.1016/j.jpsychires.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Faravelli C, Alessandra Scarpato M, Castellini G, Lo Sauro C. Gender differences in depression and anxiety: the role of age. Psychiatry Res. 2013;210(3):1301–1303. doi: 10.1016/j.psychres.2013.09.027. [DOI] [PubMed] [Google Scholar]
- 37.Patel R, Biros MH, Moore J, Miner JR. Gender differences in patient-described pain, stress, and anxiety among patients undergoing treatment for painful conditions in the emergency department. Acad Emerg Med. 2014;21(12):1478–1484. doi: 10.1111/acem.12543. [DOI] [PubMed] [Google Scholar]
- 38.Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, Kessler RC. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychol Med. 2005;35(3):317–327. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Williams DR, Gonzalez HM, Neighbors H, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64(3):305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 40.Himle JA, Baser RE, Taylor RJ, Campbell RD, Jackson JS. Anxiety disorders among African Americans, blacks of Caribbean descent, and non-Hispanic whites in the United States. J Anxiety Disord. 2009;23(5):578–590. doi: 10.1016/j.janxdis.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Breslau J, Aguilar-Gaxiola S, Kendler KS, Su M, Williams D, Kessler RC. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychol Med. 2006;36(1):57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Administration SAaMHS. Racial/Ethnic Differences in Mental Health Service Use among Adults. Rockville, MD: 2105. [Google Scholar]
- 43.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 44.Medicine CotRSaBDaMfEHRBoPHaPHPIo. Capturing Social and Behavioral Domains in Electronic Health Records: Phase 1. Washington (DC): Nathional Academics Press (US); 2014. Jun 23, [PubMed] [Google Scholar]
- 45.Sinikallio S, Aalto T, Airaksinen O, et al. Depression is associated with poorer outcome of lumbar spinal stenosis surgery. Eur Spine J. 2007;16(7):905–912. doi: 10.1007/s00586-007-0349-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Riediger W, Doering S, Krismer M. Depression and somatisation influence the outcome of total hip replacement. Int Orthop. 2010;34(1):13–18. doi: 10.1007/s00264-008-0688-7. [DOI] [PMC free article] [PubMed] [Google Scholar]