Abstract
Purpose
To examine the association between residence in neighborhoods with high rates of incarceration and cardiometabolic disease among non-incarcerated individuals.
Methods
We used data from two community cohort studies (n=1,368) in Atlanta, Georgia – META-Health and Predictive Health (2005-2012) – to assess the association between neighborhood incarceration rate and cardiometabolic disease, adjusting for individual- and neighborhood-level factors. We also examined the interaction between race and neighborhood incarceration rate.
Results
Individuals living in neighborhoods with high incarceration rates were more likely to have dyslipidemia (odds ratio [OR] = 1.47; 95% confidence interval [CI] = 1.03-2.09) and metabolic syndrome (OR = 1.67; 95% CI = 1.07-2.59) in fully-adjusted models. Interactions between race and neighborhood incarceration rate were significant; black individuals living in neighborhoods with high incarceration rates were more likely to have hypertension (OR = 1.59; 95% CI = 1.01-2.49), dyslipidemia (OR = 1.77; 95% CI = 1.12-2.80), and metabolic syndrome (OR = 1.80; 95% CI = 1.09-2.99).
Conclusions
Black individuals living in neighborhoods with high rates of incarceration have worse cardiometabolic health profiles. Criminal justice reform may help reduce race-specific health disparities in the United States.
Keywords: Mass incarceration, cardiovascular health, racial disparities
INTRODUCTION
Social determinants of health are increasingly recognized as drivers of disparities in cardiovascular health the United States. Both individual exposures, such as household income and education, and environmental exposures, such as neighborhood deprivation, crime and food insecurity, have been associated with adverse cardiometabolic disease and events; however, the impact of mass incarceration, especially at the community level, is less well understood [1].
Approximately 7 million people are part of the adult correctional system in the United States [2], and despite recent modest reductions over the past several years, significant racial disparities persist. As of 2015, black men were roughly six times more likely to be incarcerated than white men, and black women were two times more likely to be incarcerated than white women [3]. The negative effects of incarceration on individual health, and specifically, cardiovascular morbidity and mortality, are well established [4]; however, the boundaries within which mass incarceration exerts its effect are expanding. Direct relatives of incarcerated individuals appear to be at greater risk for cardiometabolic disease, and even further removed, general community members who live in neighborhoods with high versus low rates of incarceration experience worse mental health problems [5]. Addressing the problem of mass incarceration, with its combination of profound racial disparities and ever-expanding impact, represents a significant community health opportunity [6].
To better understand the health implications of exposure to mass incarceration, we analyzed whether living in a neighborhood with high levels of incarceration is associated with the cardiometabolic health in non-incarcerated individuals. We further examined the interaction between race and neighborhood incarceration rate on the likelihood of cardiometabolic disease, given established racial disparities in incarceration.
METHODS
Individuals enrolled in two community convenience samples, META-Health and Predictive Health, in Atlanta, GA, from 2005 to 2012 underwent a detailed baseline evaluation using standardized self-report questionnaires and medical records review. Both META-Health and Predictive Health recruited participants without prevalent cardiovascular disease (myocardial infarction, stroke, or heart failure) to study individual- and neighborhood-level risk factors associated with preclinical cardiovascular disease. Age (years) was measured linearly, and sex (male vs. female), race (white vs. black), education (less then college graduate vs. college graduate), income (< $50,000/year vs. ≥ $50,000/year) and smoking (current or former vs. never) were measured categorically, as obtained by self-report. All clinical data were measured linearly. Anthropometric data were measured by trained staff and included systolic blood pressure (SBP, mm Hg) and body mass index (BMI, kg/m2). Routine laboratory data included fasting values of total cholesterol (mg/dL), high-density lipoprotein cholesterol (HDL-C, mg/dL) low-density lipoprotein cholesterol (LDL-C, mg/dL), triglycerides (mg/dL) and glucose (mg/dL). Further details of each cohort have been described previously and were approved by the Emory University and Morehouse School of Medicine Institutional Review Boards [7, 8]. All participants provided written informed consent.
Neighborhood prison admission rates were obtained from The Justice Atlas of Sentencing and Corrections [9]. Data were linked to subject-reported zip code of residence and dichotomized at the 75th percentile (2.77 prison admissions per 1000 adult residents), as previously described [5]. Neighborhood crime was measured using an indexed score from the Federal Bureau of Investigation Uniform Crime Report, with 100 representing average national crime [10]. Neighborhood measures of poverty and access to healthy foods were determined using the United States Department of Agriculture Food Desert Research Atlas. Low income zip codes were defined by a poverty rate ≥ 20% or a median family income ≤ 80% of the state-wide median family income. Areas with poor access to healthy foods had no supermarkets or large grocery stores within 1 mile (if urban) or 10 miles (if rural) of a significant number (at least 500 people) or share (at least 33 percent) of the population [11].
Hypertension was defined as SBP ≥140 mm Hg, DBP ≥90 mm Hg, or current use of any antihypertensive medication [12]. Dyslipidemia was defined as triglycerides ≥150 mg/dL, HDL-C <40 mg/dL (for men) or HDL-C <50 mg/dL (for women), or current use of any lipid-lower medication [13]. Diabetes or impaired fasting glucose (IFG) was defined as fasting glucose ≥100 mg/dL, current diagnosis of diabetes, or current use of any medication to treat diabetes [14]. Finally, metabolic syndrome was defined by criteria from the Adult Treatment Panel III [13] by prevalence of any three of the following criteria: obesity (waist circumference >40 inches [for men] or >35 inches [for women]); diabetes or IFG (as previously defined); dyslipidemia (as previously defined); or hypertension (SBP >130 mm Hg, DBP >85 mm Hg, or antihypertensive medication use) [14]. All clinical risk factor components were determined from patient history and confirmed with physical exam, medication use and laboratory findings.
Baseline descriptive statistics were reported as frequency (percentage), mean ± standard deviation or median [interquartile range]. Differences between individuals in neighborhoods with high (n = 343) versus low (n = 1025) incarceration rates were assessed by t-test, Mann-Whitney U test and chi-square test for normal, non-normal and categorical variables, respectively. We tested the association between neighborhood incarceration rate and cardiometabolic disease with stepwise binary logistic regression models: Model 1: adjusted for study cohort; Model 2: adjusted for age, sex, race, income, education, crime index and study cohort; Model 3: adjusted for Model 2 plus BMI and smoking history; Model 4: adjusted for Model 3 plus BMI, smoking history, hypertension, heart failure, diabetes, dyslipidemia, prior MI, prior revascularization, obstructive CAD on cardiac catheterization, acute coronary syndrome (ACS) on presentation, systolic blood pressure, LDL-cholesterol, antihypertensive use, statin use, aspirin use and clopidogrel use. Interactions for race × neighborhood incarceration, sex × neighborhood incarceration and race × sex × neighborhood incarceration were tested, and subgroup analyses were performed for those outcomes with significant interactions. Two-tailed P-value < .05 was considered statistically significant. All analyses were performed using SAS 9.4 (Cary, NC).
RESULTS
Baseline characteristics of the cohort are presented in Table 1 – the mean age was 49 years (range: 18-84 years) and most were female, white, had graduated college and had a yearly income ≥ $50,000. Individuals from neighborhoods with high incarceration rates were more likely to be black and more likely to report income less than $50,000 per year compared to individuals from neighborhoods with low incarceration rates, Table 1. They also had greater rates of neighborhood poverty, less access to healthy foods and greater neighborhood crime indices, Table 1. Behavioral risk factors such as history of smoking, and elevated BMI were more prevalent among individuals from neighborhoods with high rates of incarceration, Table 1. There were no differences in systolic blood pressure, cholesterols, fasting glucose, or Framingham Risk Score between individuals living in neighborhoods with high or low incarceration rates, Table 1.
Table 1.
Clinical characteristics of subjects, stratified by incarceration rate
| Variables | All (N=1368) | High Incarceration (N=343) | Low Incarceration (N=1025) | P-value |
|---|---|---|---|---|
| Age, years | 49 ± 10 | 49 ± 9 | 49 ± 10 | 0.299 |
| Female, n (%) | 850 (62.1%) | 206 (60.1%) | 644 (62.8%) | 0.369 |
| Black race, n (%) | 560 (40.9%) | 246 (71.7%) | 314 (30.6%) | <0.001 |
| College graduate, n (%) | 879 (67.2%) | 147 (46.1%) | 732 (73.9%) | <0.001 |
| Yearly income < $50,000, n (%) | 382 (30.4%) | 181 (58.6%) | 201 (21.2%) | <0.001 |
|
| ||||
| Prison admission rates, per 1000 adults | 1.21 (0.58-2.77) | 4.12 (3.28-5.49) | 0.78 (0.45-1.66) | <0.001 |
| Neighborhood crime index | 205 (94-308) | 231 (133-421) | 186 (77-297) | <0.001 |
| Neighborhood poverty, % | 450 (32.9%) | 226 (65.9%) | 224 (21.9%) | <0.001 |
| Food scarcity, % | 853 (62.3%) | 248 (71.4%) | 608 (59.3%) | <0.001 |
|
| ||||
| Smoking, n (%) | 220 (17.4%) | 91 (28.5%) | 129 (13.6%) | <0.001 |
| Body mass index, kg/m2 | 29.0 ± 7.1 | 30.2 ± 7.8 | 28.6 ± 6.9 | <0.001 |
| Systolic BP, mmHg | 121 ± 17 | 123 ± 20 | 121 ± 16 | 0.052 |
| Total Cholesterol, mg/dL | 197 ± 38 | 196 ± 38 | 197 ± 38 | 0.519 |
| LDL Cholesterol, mg/dL | 115 ± 33 | 115 ± 34 | 115 ± 33 | 0.957 |
| HDL Cholesterol, mg/dL | 61 ± 18 | 60 ± 18 | 61 ± 18 | 0.206 |
| Triglycerides, mg/dL | 92 (69-129) | 92 (68-128) | 93 (69-129) | 0.896 |
| Fasting glucose, mg/dL | 88 (82-94) | 88 (82-95) | 88 (82-94) | 0.866 |
| Framingham Risk Score | 5.7 (2.9-10.4) | 6.0 (3.1-11.1) | 5.7 (2.8-10.2) | 0.251 |
|
| ||||
| Diabetes/IFG, n (%) | 187 (14.4%) | 59 (18.4%) | 128 (13.1%) | 0.02 |
| Hypertension, n (%) | 522 (38.6%) | 158 (46.8%) | 364 (35.8%) | <0.001 |
| Dyslipidemia, n (%) | 536 (40.4%) | 167 (51.2%) | 369 (36.8%) | <0.001 |
| Metabolic syndrome, n (%) | 308 (22.7%) | 95 (28.1%) | 213 (20.9%) | 0.007 |
Values are number (% prevalence) for categorical variables, mean ± SD for normal continuous variables and median (IQR) for non-normal continuous variables.
Abbreviations: BP = blood pressure, LDL = low-density lipoprotein, HDL = high-density lipoprotein, IFG = impaired fasting glucose
In unadjusted models, individuals living in neighborhoods with high incarceration rates had higher odds of hypertension (odds ratio [OR] = 1.57; 95% confidence interval [CI] = 1.23-2.02), dyslipidemia (OR = 1.80; 95% CI =1.40-2.32), diabetes/IFG (OR = 1.50; 95% CI = 1.07-2.10), and metabolic syndrome (OR = 1.48; 95% CI = 1.12-1.96).
After adjusting for individual (age, race, sex, income, education, smoking history, body mass index, cohort participation) and neighborhood (poverty, access to healthy food, crime) factors, living in a neighborhood with high incarceration rate was associated with statistically significant increased odds of dyslipidemia (OR = 1.47; 95% CI = 1.03-2.09) and metabolic syndrome (OR = 1.67; 95% CI = 1.07-2.59), but not hypertension (OR = 1.39; 95% CI = 0.97-1.97) or diabetes/IFG (OR = 1.36; 95% CI = 0.83-2.24), Table 2.
Table 2.
Odds ratios for the prevalence of cardiometabolic disease in subjects living in areas with high incarceration rate
| Model 1
|
Model 2
|
Model 3
|
Model 4
|
Model 5
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) |
p | OR (95% CI) |
p | OR (95% CI) |
p | OR (95% CI) |
p | OR (95% CI) |
p | |
| Metabolic syndrome | 1.48 (1.12-1.96) |
0.007 | 1.44 (1.04-1.99) |
0.030 | 1.44 (1.01-2.04) |
0.043 | 1.47 (1.01-2.16) |
0.046 | 1.67 (1.07-2.59) |
0.024 |
| Hypertension | 1.57 (1.23-2.02) |
<0.001 | 1.22 (0.91-1.62) |
0.180 | 1.33 (0.95-1.80) |
0.072 | 1.32 (0.95-1.84) |
0.103 | 1.39 (0.97-1.97) |
0.070 |
| Dyslipidemia | 1.80 (1.40-2.32) |
<0.001 | 1.27 (0.95-1.70) |
0.106 | 1.31 (0.96-1.80) |
0.090 | 1.39 (0.99-1.96) |
0.058 | 1.47 (1.03-2.09) |
0.034 |
| Diabetes/IFG | 1.50 (1.07-2.10) |
0.019 | 1.34 (0.91-1.98) |
0.142 | 1.24 (0.82-1.89) |
0.308 | 1.33 (0.84-2.11) |
0.225 | 1.36 (0.83-2.24) |
0.227 |
Abbreviations: OR, odds ratio; IFG, impaired fasting glucose
P < 0.05
Model 1: Crude
Model 2: Adjusted for age, sex, race and study cohort
Model 3: Adjusted for Model 2, income and education
Model 4: Adjusted for Model 3, neighborhood poverty, access to healthy foods and crime index
Model 5: Adjusted for Model 4, BMI and smoking history
Tests for the interaction between race and neighborhood incarceration were significant for all outcomes of interest, Figure 1. Fully-adjusted, race-stratified analyses showed that black subjects living in neighborhoods with high incarceration rates had statistically significant increased odds of hypertension (OR = 1.59; 95% CI = 1.01-2.49), dyslipidemia (OR = 1.77; 95% CI = 1.12-2.80), and metabolic syndrome (OR = 1.80; 95% CI = 1.09-2.99), and a non-significant trend towards an increase in diabetes/IFG (OR = 1.72; 95% CI = 0.96-3.10). There were no associations between cardiometabolic disease and neighborhood incarceration rate for white subjects, Figure 1.
Figure 1.
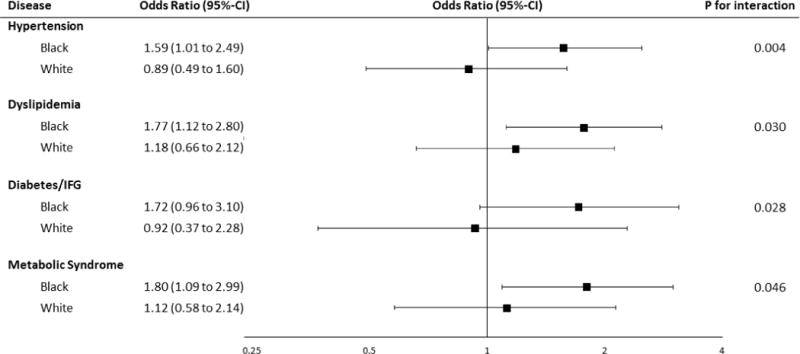
Odds of cardiometabolic disease for individuals in neighborhoods with high incarceration rates. Black subjects living in neighborhoods with high incarceration rates had significantly increased odds of hypertension, dyslipidemia, and metabolic syndrome in fully-adjusted models. IFG = impaired fasting glucose.
Tests for the interaction between sex and neighborhood incarceration were significant for dyslipidemia only (ORfemale = 1.55; 95% CI = 1.00-2.39 vs. ORmale = 1.25; 95% CI = 0.66-2.34), P-interaction=0.02); however, all other sex × neighborhood incarceration interactions, as well as the race × sex × neighborhood incarceration interactions, were non-significant.
CONCLUSIONS
We found that non-incarcerated black individuals living in neighborhoods with high rates of incarceration had greater rates of cardiometabolic disease, independent of individual- and neighborhood-level factors including crime and poverty. While the effect of exposure to mass incarceration at the community level has been explored in other diseases, and with varying results [5, 15], to our knowledge, this is the first study to examine its association with cardiometabolic disease.
Our findings, specifically, that only black individuals were adversely affected by high community rates of incarceration, raise interesting questions regarding the mechanism of effect. Mass incarceration disproportionately affects people and communities of color [3], and these differences are not explained by racial disparities in criminal offense rates or neighborhood contextual factors, especially for low-level offenses [16]. Threat of arrest in these neighborhoods, specifically for black individuals, may contribute to subclinical chronic stress and trigger inflammatory responses that increase rates of cardiometabolic disease [17, 18]. Additionally, adverse neighborhood characteristics have been linked to dysregulation of the hypothalamic-pituitary-adrenal axis and cortisol [19], which may explain the findings of increased obesity-related diseases. Future studies exploring the associations between race, neighborhood, stress and inflammation are needed to better elucidate the mechanism for increased cardiometabolic disease in neighborhoods with high rates of incarceration.
This study has several limitations, including its cross-sectional design, which prevents inference of causal relationships, and an inability to account for unmeasured confounders, such as perceived neighborhood safety, racial segregation, or individual stress. Additionally, individual history of incarceration is unmeasured and may confound the association between neighborhood incarceration rate and cardiometabolic disease, as former incarceration is a known risk factor for diseases such as hypertension [20]. Lastly, because our data was restricted to zip codes as a surrogate for neighborhood, there is likely greater demographic heterogeneity than with other geographic clusters, such as census tracts or blocks. Despite these limitations, it is the first study to assess the association between incarceration rates and risk for cardiometabolic disease in a large, diverse, community-based population. These findings suggest that interventions addressing mass incarceration may benefit the broader community in addition to those individuals who are incarcerated, and further studies are needed to determine the relationship and impact of neighborhood incarceration rate within the spectrum of other social determinants of health.
Acknowledgments
We would like to thank all of the participants of the Morehouse and Emory Team Up to Eliminate Health Disparities (META-Health) Study and the Emory Predictive Health Initiative.
Funding: This research was supported by grants from the National Institutes of Health (UL1 RR025008, U01 HL079156-01, T32 HL130025-02) and the American Heart Association Strategically Focused Research Network on Disparities (Grant 0000031288).
Footnotes
Competing interests: None
References
- 1.Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2015;132(9):873–98. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 2.Kaeble D, Glaze L. Correctional Populations in the United States, 2015. Washington D.C: U.S. Department of Justice, Programs OoJ; 2016. NCJ 250374 Contract No.: NCJ 250374. [Google Scholar]
- 3.Carson EA, Anderson E. Prisoners in 2015. Washington D.C: U.S. Department of Justice, Programs OoJ; 2016. NCJ 250229 Contract No.: NCJ 250229. [Google Scholar]
- 4.Wang EA, Redmond N, Dennison Himmelfarb CR, Pettit B, Stern M, Chen J, et al. Cardiovascular Disease in Incarcerated Populations. Journal of the American College of Cardiology. 2017;69(24):2967–76. doi: 10.1016/j.jacc.2017.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hatzenbuehler ML, Keyes K, Hamilton A, Uddin M, Galea S. The Collateral Damage of Mass Incarceration: Risk of Psychiatric Morbidity Among Nonincarcerated Residents of High-Incarceration Neighborhoods. Am J Public Health. 2015;105(1):138–43. doi: 10.2105/AJPH.2014.302184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cloud DH, Parsons J, Delany-Brumsey A. Addressing mass incarceration: a clarion call for public health. Am J Public Health. 2014;104(3):389–91. doi: 10.2105/AJPH.2013.301741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kelli HM, Hammadah M, Ahmed H, Ko YA, Topel M, Samman-Tahhan A, et al. Association Between Living in Food Deserts and Cardiovascular Risk. Circ Cardiovasc Qual Outcomes. 2017;10(9) doi: 10.1161/CIRCOUTCOMES.116.003532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morris AA, Zhao L, Ahmed Y, Stoyanova N, De Staercke C, Hooper WC, et al. Association between depression and inflammation–differences by race and sex: the META-Health study. Psychosomatic medicine. 2011;73(6):462–8. doi: 10.1097/PSY.0b013e318222379c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Justice Mapping Center. Justice Atlas of Sentencing and Corrections. 2008 [Available from: http://www.justiceatlas.org/
- 10.Herries J. Crime Rate Comparison Map. Living Atlas of the World ArcGIS/ESRI2012. [Available from: https://www.arcgis.com/home/item.html?id=8125e8f4244a47d986f4cd840824eef3.
- 11.United States Department of Agriculture. Food Access Research Atlas. 2015 [Available from: http://www.ers.usda.gov/data-products/food-access-research-atlas/documentation.aspx.
- 12.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311(5):507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 13.National Cholesterol Education Program Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–421. [PubMed] [Google Scholar]
- 14.American Diabetes A. 2. Classification and Diagnosis of Diabetes. Diabetes Care. 2016;39(Suppl 1):S13–22. doi: 10.2337/dc16-S005. [DOI] [PubMed] [Google Scholar]
- 15.Frank JW, Hong CS, Subramanian SV, Wang EA. Neighborhood incarceration rate and asthma prevalence in New York City: a multilevel approach. Am J Public Health. 2013;103(5):e38–44. doi: 10.2105/AJPH.2013.301255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mitchell O, Caudy MS. Examining Racial Disparities in Drug Arrests. Justice Q. 2015;32(2):288–313. [Google Scholar]
- 17.Schneiderman N, Ironson G, Siegel SD. Stress and health: psychological, behavioral, and biological determinants. Annu Rev Clin Psychol. 2005;1:607–28. doi: 10.1146/annurev.clinpsy.1.102803.144141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.von Kanel R, Hepp U, Kraemer B, Traber R, Keel M, Mica L, et al. Evidence for low-grade systemic proinflammatory activity in patients with posttraumatic stress disorder. J Psychiatr Res. 2007;41(9):744–52. doi: 10.1016/j.jpsychires.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 19.Dulin-Keita A, Casazza K, Fernandez JR, Goran MI, Gower B. Do neighbourhoods matter? Neighbourhood disorder and long-term trends in serum cortisol levels. J Epidemiol Community Health. 2012;66(1):24–9. doi: 10.1136/jech.2009.092676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang EA, Pletcher M, Lin F, et al. Incarceration, incident hypertension, and access to health care: Findings from the coronary artery risk development in young adults (cardia) study. Archives of Internal Medicine. 2009;169(7):687–93. doi: 10.1001/archinternmed.2009.26. [DOI] [PMC free article] [PubMed] [Google Scholar]


