Abstract
Background and Objectives
Gender-related differences in health care utilization for atrial fibrillation (AF) are increasingly recognized. However, large cohort data for examining gender-related differences in AF are lacking in Asian populations.
Methods
The Registry for Comparison Study of Drugs for Symptom Control and Complication Prevention of AF (CODE-AF Registry) is a prospective observational cohort-study that enrolled participants at 10 tertiary hospitals in South Korea. Baseline characteristics retrieved from the CODE-AF Registry were analyzed.
Results
A total of 6,274 patients were recruited (mean age 67±11 years, mean CHA2DS2-VASc score 2.7±1.7, 63% male, 65% paroxysmal AF) from June 2016 to April 2017. Women underwent less electric cardioversion (12.3% vs. 19.6%, p<0.001), less radiofrequency ablation (12.4% vs. 17.9%, p<0.001), and less antiarrhythmic drug therapy (44.7% vs. 49.5%, p<0.001), despite having more severe symptoms (symptom class III or IV, 45.8% vs. 37.5%, p<0.001). Among patients with a CHA2DS2-VA score of 2 or more, a slightly higher proportion of women were taking oral anticoagulants than men (85.7% vs. 81.9%, p=0.002), and non-vitamin K antagonist oral anticoagulant (NOAC) use was more prevalent in women than men (70.4% vs. 62.3%, p<0.001). Insufficient NOAC dosing was very common, more so in women than men (61.5% vs. 56.3%, p<0.001).
Conclusions
Female patients with AF were treated more conservatively and rhythm control strategies were used less frequently than in males, even though the female patients with AF had more severe symptoms. While insufficient NOAC dosing was common in both sex, it was significantly more frequent in women.
Keywords: Atrial fibrillation, Registries, Sex characteristics, Asian ceancestry group, Anticoagulants
INTRODUCTION
A topic of current interest is whether gender-related differences exist in the use of health care resources for managing atrial fibrillation (AF), and whether/how these differences affect clinical outcomes.1),2),3),4),5) Despite many advances in rhythm control methods, including radiofrequency catheter ablation, women are less likely to be selected for rhythm control strategies based on analyses of data from Europe and North America.3),6),7) Although AF is less prevalent in women than in men, women with AF have a higher risk of stroke and death than men. The risk of developing AF is about 2 times higher in men than in women.8) However, because women live longer than men and the prevalence of AF increases with age, there are more women than men with AF.1) In addition, female sex has been shown to be an independent risk factor for AF-related stroke.9),10) Therefore, improving stroke prevention in women with AF is important for reducing the public health burden of AF. However, it has been reported that women are less likely to undergo anticoagulation, mainly in the warfarin era.5) Non-vitamin K antagonist oral anticoagulants (NOACs) such as the direct thrombin inhibitor dabigatran and the factor Xa inhibitors rivaroxaban, apixaban, and edoxaban are now approved and widely used for stroke prevention in patients with AF.11),12),13),14) However, it is unknown whether there are any gender-related differences in anticoagulation, even in the NOAC era. Moreover, little data from Asian women are available to address this question. Therefore, we investigated whether there are sex-specific differences in the management of AF using a large Korean cohort and compared our findings to those of studies in Western countries.
METHODS
Study population
The Registry for Comparison Study of Drugs for Symptom Control and Complication Prevention of AF (CODE-AF Registry) is a prospective observational cohort study whose goal was to compare the use of different drugs for rate control, rhythm control, and anticoagulation therapy for stroke prevention in patients with AF. The study enrolled participants in 10 tertiary hospitals encompassing all geographical regions of South Korea. The registry was designed and coordinated by the Korea Heart Rhythm Society, which provides support to related committees, national coordinators, and participating centers. Data are entered in a common electronic database that limits inconsistencies and errors and provides online help for key variables. Each center has access to its own data and data from all other participating centers. The number of patients enrolled from each center is shown in previous publication.15) A follow-up visit was scheduled every 6 months, either through personal interview or telephone contact. The study was approved by the ethics committee of each center and all patients provided informed consent for their inclusion. This study is registered at www.ClinicalTrials.gov (NCT02786095).
Definition of variables
Nonvalvular AF was defined as AF without moderate or severe rheumatic mitral stenosis and without a mechanical mitral valve. Paroxysmal AF was defined as AF that was terminated before 7 days, with or without medical intervention. Persistent AF was any AF that lasted longer than 7 days continuously. AF was classified as paroxysmal if it terminated within 7 days and persistent if it lasted longer than 7 days.16) Congestive heart failure, hypertension, age >75, diabetes mellitus, prior stroke or transient ischemic attack, vascular disease, age >65, female (CHA2DS2-VASc) and hypertension, abnormal renal/liver function; serum creatinine ≥2.3 mg/dL or bilirubin >2×upper limit of normal, in association with aspartate aminotransferase/alanine aminotransferase/alkaline phosphatase >3×upper limit of normal, stroke, bleeding history or predisposition, labile international normalized ratio, elderly, drugs/alcohol concomitantly (HAS-BLED) scores were calculated for all patients with nonvalvular AF.17)
Statistical analysis
Continuous variables that were normally distributed are reported as means±standard deviations and were compared using Student's t-test. Categorical variables are reported as counts (percentages) and were compared using the χ2 test or Fisher's exact test if any expected cell count was less than 5. Logistic regression models were constructed to identify significant factors that influence anticoagulation decisions. The R package (version 3.2.4; R Foundation for Statistical Computing, Vienna, Austria) was used to perform all statistical evaluations. A 2 tailed p value <0.05 was considered statistically significant.
RESULTS
Baseline characteristics
The CODE-AF study commenced recruitment in June 2016. A total of 6,274 patients were recruited (mean age 67±11 years, mean CHA2DS2-VASc score 2.7±1.7, 63% male, 65% paroxysmal AF) from June 2016 to April 2017. The patient baseline characteristics are shown in Table 1. Compared to male patients, female patients were older and had a higher prevalence of hypertension and dyslipidemia. Female patients also had more severe AF-related symptoms than male patients (European Heart Rhythm Association [EHRA] III or IV: 45.8% vs. 37.5%, p<0.001), and received more permanent pacemakers.
Table 1. Baseline characteristics of the subjects according to gender.
| Female (n=2,308) | Male (n=3,966) | p | |
|---|---|---|---|
| Age (years) | 70.1±9.8 | 65.7±11.1 | <0.001 |
| Height (cm) | 155.3±6.2 | 169.1±6.2 | <0.001 |
| Weight (kg) | 59.2±9.6 | 70.7±10.7 | <0.001 |
| Body mass index (kg/m2) | 24.5±3.7 | 24.7±3.1 | 0.174 |
| Current smoking | 19 (0.8) | 524 (13.2) | <0.001 |
| Alcohol intake | 136 (6.0) | 1,366 (42.0) | <0.001 |
| Paroxysmal AF | 1,546 (67.5) | 2,553 (64.5) | 0.072 |
| Symptomatic AF (EHRA 3 or 4) | 1,049 (45.8) | 1,483 (37.5) | <0.001 |
| CHA2DS2-VASc score | 3.2±1.3 | 1.9±1.3 | <0.001 |
| CHA2DS2-VASc score ≥2 | 2,066 (90.1) | 2,382 (60.2) | <0.001 |
| CHADS2 score | 1.8±1.2 | 1.7±1.2 | <0.001 |
| CHADS2 score ≥2 | 1,268 (55.3) | 1,993 (50.4) | <0.001 |
| CHA2DS2-VA score* | 2.2±1.3 | 1.9±1.3 | <0.001 |
| CHA2DS2-VA score ≥2* | 1,589 (69.3) | 2,382 (60.2) | <0.001 |
| HAS-BLED score | 2.0±1.0 | 1.9±1.1 | 0.001 |
| HAS-BLED score ≥3 | 614 (26.8) | 1,033 (26.1) | 0.571 |
| Hypertension | 1,608 (70.2) | 2,632 (66.5) | 0.012 |
| Diabetes mellitus | 571 (24.9) | 1,026 (25.9) | 0.351 |
| Myocardial infarction | 51 (2.2) | 154 (3.9) | 0.002 |
| Prior valve surgery | 14 (0.6) | 10 (0.3) | 0.086 |
| Congestive heart failure | 254 (11.1) | 378 (9.6) | 0.147 |
| Peripheral vascular disease | 95 (4.1) | 233 (5.9) | 0.011 |
| Stroke or transient ischemic attack | 359 (15.7) | 593 (15.0) | 0.326 |
| Dyslipidemia | 887 (38.7) | 1,297 (32.8) | <0.001 |
| Pacemaker implant | 221 (9.6) | 187 (4.7) | <0.001 |
| Implantable cardioverter-defibrillator | 20 (0.9) | 47 (1.2) | 0.212 |
| eGFR (mL/min) | 76.8±23.7 | 76.3±20.3 | 0.375 |
| Chronic kidney disease (eGFR <60 mL/min) | 245 (10.7) | 376 (9.5) | 0.29 |
| Cancer history | 193 (8.4) | 437 (11.0) | 0.003 |
| Any bleeding history | 221 (9.6) | 361 (9.1) | 0.715 |
| LA volume index (mL/m2) | 51.4±27.6 | 45.3±24.5 | <0.001 |
| Left ventricular ejection fraction (%) | 62.5±14.6 | 60.3±9.7 | <0.001 |
| E/E′ | 13.7±6.7 | 11.1±14.8 | <0.001 |
AF = atrial fibrillation; CHA2DS2-VASc = congestive heart failure, hypertension, age >75, diabetes mellitus, prior stroke or transient ischemic attack, vascular disease, age >65, female; E/E′ = early diastolic mitral inflow velocity/mitral annular velocity; eGFR = estimated glomerular filtration rate; EHRA = European Heart Rhythm Association; ESRD = end-stage renal disease; HAS-BLED = hypertension, abnormal renal/liver function; serum creatinine ≥2.3 mg/dL or bilirubin >2 × upper limit of normal, in association with aspartate aminotransferase/alanine aminotransferase/alkaline phosphatase >3 × upper limit of normal, stroke, bleeding history or predisposition, labile international normalized ratio, elderly, drugs/alcohol concomitantly; LA = left atrium.
*Excluding points for sex category.
Body mass index, diabetes, prior valve surgery, prior stroke, chronic kidney disease, and prior bleeding event were not significantly different between males and females.
Male patients were more likely to be smokers, have higher alcohol intake, and had a higher prevalence of myocardial infarction and cancer. Female patients were more likely to have a CHA2DS2-VASc score ≥2 than male patients.
To analyze anticoagulation status according to the recent European guideline, CHA2DS2-VA scores were calculated (without the point for the sex category). Female patients were more likely to have a CHA2DS2-VA score ≥2 (69.3% vs. 60.2%, p<0.001). CHADS2 ≥2 was also more frequent in females (55.3% vs. 50.4%, p<0.001). There was no significant difference in HAS-BLED between men and women.
Rhythm and rate control therapy
Table 2 showed the distribution of rhythm and rate control methods in detail. In women, the attempt of any rhythm control modality was significantly less frequent than in men. Women underwent electric cardioversion less frequently, radiofrequency ablation less frequently, and used anti-arrhythmic drug therapy less frequently. Analysis of individual antiarrhythmic drugs revealed that amiodarone was the only drug that was used significantly less often in women than men. The use of beta blockers and calcium channel blockers was similar between both sexes. However, digitalis was used more frequently in women.
Table 2. Distribution of rhythm and rate control strategies according to gender.
| Female (n=2,308) | Male (n=3,966) | p | |||
|---|---|---|---|---|---|
| Any rhythm control attempt | 1,244 (54.6) | 2,470 (62.7) | <0.001 | ||
| RFCA for AF | 285 (12.4) | 707 (17.9) | <0.001 | ||
| Electrical cardioversion | 282 (12.3) | 775 (19.6) | <0.001 | ||
| Antiarrhythmic drug | 1,018 (44.7) | 1,953 (49.5) | <0.001 | ||
| Amiodarone | 198 (8.7) | 520 (13.2) | <0.001 | ||
| Dronedarone | 62 (2.7) | 94 (2.4) | 0.461 | ||
| Propafenone | 76 (3.3) | 100 (2.5) | 0.079 | ||
| Propafenone SR | 258 (11.3) | 455 (11.5) | 0.833 | ||
| Flecainide | 470 (20.6) | 882 (22.3) | 0.118 | ||
| Sotalol | 20 (0.9) | 50 (1.3) | 0.201 | ||
| Pilsicainide | 49 (2.1) | 75 (1.9) | 0.56 | ||
| Rate control drug usage | |||||
| Beta blocker | 1,120 (49.1) | 1,914 (48.4) | 0.639 | ||
| Calcium channel blocker | 664 (29.1) | 1,131 (28.6) | 0.708 | ||
| Digitalis | 217 (9.5) | 218 (5.5) | <0.001 | ||
AF = atrial fibrillation; RFCA = radiofrequency catheter ablation; SR = sustained release.
Antithrombotic therapy
Oral anticoagulants were prescribed to 69% of the patients overall, including warfarin (17%) and NOACs (52%). Oral anticoagulant usage was more frequent in women than men (76.7% vs. 64.6%, p<0.001) and warfarin was used more frequently in men than in women (14.9% vs. 18.9%, p=0.001, Table 3). However, NOACs were prescribed far more frequently for women than men (61.8% vs. 45.8%, p<0.001). The use of dabigatran was not significantly different between female and male patients. Rivaroxaban, apixaban, and edoxaban were all used more frequently in females than males.
Table 3. Comparison of anticoagulation status between males and females.
| Female (n=2,308) | Male (n=3,966) | p | |||
|---|---|---|---|---|---|
| Any anticoagulant | 1,771 (76.7) | 2,564 (64.6) | <0.001 | ||
| Warfarin | 344 (14.9) | 748 (18.9) | <0.001 | ||
| NOAC | 1,427 (61.8) | 1,818 (45.8) | <0.001 | ||
| Dabigatran | 331 (14.3) | 541 (13.6) | 0.462 | ||
| Rivaroxaban | 332 (14.4) | 439 (11.1) | <0.001 | ||
| Apixaban | 561 (24.3) | 637 (16.1) | <0.001 | ||
| Edoxaban | 204 (8.8) | 203 (5.1) | <0.001 | ||
| NOAC dosing adequacy* | <0.001 | ||||
| Guideline-recommended dose | 515 (36.6) | 772 (43.0) | |||
| Insufficient dose | 867 (61.5) | 1,011 (56.3) | |||
| Over dose | 27 (1.9) | 13 (0.7) | |||
| Anticoagulation rate for patients with | |||||
| CHA2DS2-VA score=1† | 335 (70.2) | 429 (44.1) | <0.001 | ||
| Warfarin | 63 (13.2) | 197 (20.2) | 0.001 | ||
| NOAC | 272 (57.0) | 232 (23.8) | <0.001 | ||
| CHA2DS2-VA score=2 or higher† | 1,361 (85.7) | 1,952 (81.9) | 0.002 | ||
| Warfarin | 243 (15.3) | 469 (19.7) | <0.001 | ||
| NOAC | 1,118 (70.4) | 1,485 (62.3) | <0.001 | ||
| CHADS2 score=1 | 544 (74.3) | 684 (53.3) | <0.001 | ||
| CHADS2 score=2 or higher | 1,092 (86.1) | 1,629 (81.7) | 0.001 | ||
| Antiplatelets | |||||
| Aspirin | 318 (14.6) | 828 (21.5) | <0.001 | ||
| Clopidogrel | 111 (5.1) | 298 (7.7) | <0.001 | ||
NOAC = non-vitamin K antagonist oral anticoagulant.
*Information about the NOAC dosage was missing in 28 female and 22 male patients; †Excluding points for sex category.
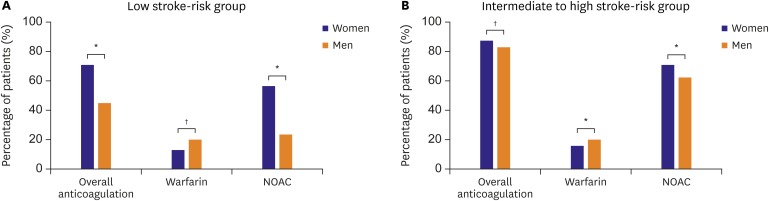
Anticoagulation status was next analyzed according to the 2016 European Society of Cardiology guideline. Among patients with a CHA2DS2-VA score of 1, the proportion of patients taking oral anticoagulation medication was significantly higher in women than men. In patients with a CHA2DS2-VA score of 2 or more, the rate of anticoagulation usage was also higher in women than men, although the difference was small (85.7% vs. 81.9%, p=0.002, Table 3, Figure 1).
Figure 1. Proportions of anticoagulation use in men and women according to stroke risk scores (Low stroke-risk group=CHA2DS2-VA score of 1, intermediate to high stroke-risk group= CHA2DS2-VA score of 2 or more).
NOAC = non-vitamin K antagonist oral anticoagulant.
*p<0.01; †p<0.001.
In the fall of 2015, the Korean reimbursement guideline changed from using the CHADS2 score to the CHA2DS2-VASc score. Therefore, we also compared anticoagulation prescription patterns for patients with AF according to CHADS2 score. Among patients with a CHADS2 score of 1, the proportion of females taking oral anticoagulation was significantly higher than that of males (74.3% vs. 53.3%, p<0.001). In patients with a CHADS2 ≥2 score of 2 or more, the anticoagulation rate was also higher in women than in men (86.1% vs. 81.7%, p=0.001).
NOAC dose relevance was also analyzed according to each manufacturer's recommendation. The information about the dose of NOAC was available in 1,409 patients. The guideline-recommended dose was used less often in women than in men (36.6% vs. 43.0%, p<0.001). In women, insufficient NOAC dosing (61.5%) and overdosing (1.9%) were more common than in men (p<0.001). Men received more aspirin; this finding may be due to the fact that history of myocardial infarction and history of coronary disease were more common in men.
DISCUSSION
We found that female patients with AF were treated more conservatively than male patients with AF, i.e., the females received less antiarrhythmic drugs, underwent less electric cardioversion, and had less radiofrequency catheter ablation.
In patients with a CHA2DS2-VA score of 1, the percentage of female patients taking oral anticoagulation medication was significantly higher than that of male patients. While insufficient NOAC dosing was common in both sexes, it was significantly more frequent in women.
In our data, female subjects were older and had more severe symptoms than males, consistent with previous analyses of data from Western countries.3) Analysis of a European cohort found that heart failure was more frequent in women, but we found that heart failure had the same prevalence across the 2 gender groups (11.1% vs. 9.6%, p=0.147). Female gender is a risk factor of stroke based on many analyses of Western cohorts.9),10),18) However, it is controversial whether this is also true in Asian populations. Recent reports of Asian populations have suggested that female sex might not be a risk factor for stroke in patients with AF.19),20),21),22) Consistent with this finding, we found that the proportions of patients with previous stroke were not significantly different between men and women, even though women were older and had more frequent hypertension. Our results, along with analysis of a cohort in Japan, suggest that female gender is not so strongly related to stroke in Asian populations with AF.
Despite experiencing more severe symptoms, women were less likely to receive rhythm control treatment than men. In the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF) study, the use of antiarrhythmic drug therapy was similar in men and women. However, women were less likely to undergo electric cardioversion and radiofrequency catheter ablation.6)
In the EURObservational Research Programme Atrial Fibrillation (EORP-AF) registry, women with symptomatic AF were more likely to receive rate control therapy alone than men.3) In this European registry, women were less likely to receive both electric cardioversion and pharmacological conversion, but catheter ablation was performed on similar percentages of males and females.
Our data are generally consistent with previous reports. We found that women received all 3 kinds of rhythm control strategies less frequently than men. Women had more severe symptoms than men and rhythm control therapy was used inadequately in women. These conclusions are shared by almost all previous reports.1),2),3),4),6) One potential explanation for this finding is the lower economic status of women in Korea. According to previous articles, gender wage gaps are still exist in Korea.23) Married women have relatively low employment rates in Korea. In addition, women are still under-employed in managerial and professional positions and more commonly employed in irregular jobs with lower levels of wage and job security.23),24) Therefore, expensive procedures were performed more frequently in men.
In the Practice INNovation And CLinical Excellence (PINNACLE) registry, women with moderate-to-high risk of stroke were more likely to receive aspirin therapy than oral anticoagulants compared to men.25) Furthermore, in a survey of general practitioners in the United Kingdom, women with AF and at moderate-to-high risk of stroke were significantly less likely to receive oral anticoagulant therapy than men (47% vs. 52%, p=0.006).5) However, more recent studies reported that the anticoagulation rate did not differ by gender.6),26) This discrepancy may reflect differences in general physician/private care vs. cardiology/academic care. Specifically, cardiology specialist care is associated with higher anticoagulation rates and better guideline adherence in stroke prevention in AF.27),28)
In the ORBIT-AF II and GARFIELD studies, gender was not a significant predictor of NOAC use.26),28) In our analysis, NOACs were used more frequently in women. Particularly in patients with a CHA2DS2-VA score of 1, more females than males were taking oral anticoagulation medication (70.2% vs. 44.1%, p<0.001, Figure 1). This difference was driven by the more frequent NOAC use in female patients with a CHA2DS2-VA score of 1 (overall NOAC 57.0% vs. 23.8%, p<0.001; dabigatran 12.8% vs. 8.7%, p=0.021; rivaroxaban 13.0% vs 5.9%, p<0.001; apixaban 20.8% vs. 6.3%, p<0.001; edoxaban 10.5% vs. 3.0%, p<0.001). This result is a consequence of the National Health Insurance policy in Korea. Specifically, Korea's national insurance reimbursement policy for NOAC use is based on the CHA2DS2-VASc score. A CHA2DS2-VASc score of 2 or more is required for national insurance in Korea to cover the cost of NOAC treatment; therefore, women with one additional risk factor can receive NOACs, but men with one risk factor cannot be reimbursed for NOAC use. This may explain why warfarin use is more frequent in men than in women.
In our registry, NOACs were used more frequently in women; however, insufficient dosing was also much higher in females. In the real world, insufficient dosing is a common issue. A population-based cohort study of patients from the province of Quebec reported that women with AF were more likely to be treated with a lower dose of dabigatran than men.29) An important conclusion is that adequate dosage should be advocated in Korea.
This was a cross-sectional study; therefore, we could not assess the impact of gender differences over time. Follow-up data will be analyzed in a future study. Furthermore, the study population size may be too small to have sufficient statistical power to assess individual NOAC differences in distribution. As the female subjects were older and had higher risk, these differences may have affected some of the observed differences in our modestly sized cohort. We did not have data on anticoagulation control quality, such as drug compliance or time in therapeutic range (TTR) data. Moreover, we could not determine how much treatment differences between men and women were influenced by patient preference as opposed to baseline differences and/or physician bias. Although our data have several limitations, few studies have used large data sets from an Asian population to investigate gender differences in AF. Our study provides important data for analyzing differences in healthcare utilization between men and women in Asia.
In conclusion, in Korea, female patients with AF were treated more conservatively than male patients with AF. Specifically, the female patients were prescribed antiarrhythmic drugs less frequently, underwent electric cardioversion less frequently, and had radiofrequency catheter ablation less frequently than the male patients. Female patients received NOACs more frequently than male patients. While insufficient NOAC dosing was common in both sexes, it was significantly more frequent in women. Further studies are needed to determine whether these differences have clinically meaningful impact.
Footnotes
Funding: This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), which is funded by the Ministry of Science, ICT & Future Planning (NRF-2012R1A2A2A02045367, 2010-0021993). This work was also supported by grants from the Korean Healthcare Technology R & D Project, which is funded by the Ministry of Health & Welfare (HI12C1552, HI16C0058, and HI15C1200).
Conflicts of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Kim JB, Lee JM, Kim TH, Park HW, Joung B.
- Data curation: Kim JB, Lee JM, Kim TH, Cha MJ, Park HW, Lee YS, Choi EK, Kim CS, Joung B.
- Formal analysis: Kim JB, Lee JM, Kim TH, Cha MJ, Park HW, Lee YS, Joung B.
- Funding acquisition: Kim JB, Lee JM, Cha MJ, Park J, Uhm JS, Lee YS, Kim CS, Joung B.
- Investigation: Kim JB, Lee JM, Park J, Kim J, Kim CS, Joung B.
- Methodology: Kim JB, Lee JM, Park J, Park JK, Choi EK, Joung B.
- Project administration: Kim JB, Lee JM, Park J, Park JK, Kang KW, Kim J, Choi EK, Joung B.
- Resources: Lee JM, Park J, Uhm JS, Kim CS, Joung B.
- Software: Kim JB, Lee JM, Park JK, Kang KW, Uhm JS, Kim CS.
- Supervision: Lee JM, Kang KW, Shim J, Kim J, Joung B.
- Validation: Lee JM, Shim J.
- Visualization: Kim JB, Lee JM, Shim J.
- Writing - original draft: Kim JB, Lee JM.
- Writing - review & editing: Kim JB, Lee JM, Joung B.
References
- 1.Gillis AM. Atrial fibrillation and ventricular arrhythmias: sex differences in electrophysiology, epidemiology, clinical presentation, and clinical outcomes. Circulation. 2017;135:593–608. doi: 10.1161/CIRCULATIONAHA.116.025312. [DOI] [PubMed] [Google Scholar]
- 2.Ko D, Rahman F, Martins MA, et al. Atrial fibrillation in women: treatment. Nat Rev Cardiol. 2017;14:113–124. doi: 10.1038/nrcardio.2016.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lip GY, Laroche C, Boriani G, et al. Sex-related differences in presentation, treatment, and outcome of patients with atrial fibrillation in Europe: a report from the Euro Observational Research Programme Pilot survey on Atrial Fibrillation. Europace. 2015;17:24–31. doi: 10.1093/europace/euu155. [DOI] [PubMed] [Google Scholar]
- 4.Rienstra M, Van Veldhuisen DJ, Hagens VE, et al. Gender-related differences in rhythm control treatment in persistent atrial fibrillation: data of the Rate Control Versus Electrical Cardioversion (RACE) study. J Am Coll Cardiol. 2005;46:1298–1306. doi: 10.1016/j.jacc.2005.05.078. [DOI] [PubMed] [Google Scholar]
- 5.Shantsila E, Wolff A, Lip GY, Lane DA. Gender differences in stroke prevention in atrial fibrillation in general practice: using the GRASP-AF audit tool. Int J Clin Pract. 2015;69:840–845. doi: 10.1111/ijcp.12625. [DOI] [PubMed] [Google Scholar]
- 6.Piccini JP, Simon DN, Steinberg BA, et al. Differences in clinical and functional outcomes of atrial fibrillation in women and men: two-year results from the ORBIT-AF Registry. JAMA Cardiol. 2016;1:282–291. doi: 10.1001/jamacardio.2016.0529. [DOI] [PubMed] [Google Scholar]
- 7.Vallakati A, Reddy M, Sharma A, et al. Impact of gender on outcomes after atrial fibrillation ablation. Int J Cardiol. 2015;187:12–16. doi: 10.1016/j.ijcard.2015.03.341. [DOI] [PubMed] [Google Scholar]
- 8.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–988. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- 9.Andersson T, Magnuson A, Bryngelsson IL, et al. Gender-related differences in risk of cardiovascular morbidity and all-cause mortality in patients hospitalized with incident atrial fibrillation without concomitant diseases: a nationwide cohort study of 9519 patients. Int J Cardiol. 2014;177:91–99. doi: 10.1016/j.ijcard.2014.09.092. [DOI] [PubMed] [Google Scholar]
- 10.Friberg L, Benson L, Rosenqvist M, Lip GY. Assessment of female sex as a risk factor in atrial fibrillation in Sweden: nationwide retrospective cohort study. BMJ. 2012;344:e3522. doi: 10.1136/bmj.e3522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–1151. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- 12.Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–2104. doi: 10.1056/NEJMoa1310907. [DOI] [PubMed] [Google Scholar]
- 13.Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–992. doi: 10.1056/NEJMoa1107039. [DOI] [PubMed] [Google Scholar]
- 14.Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–891. doi: 10.1056/NEJMoa1009638. [DOI] [PubMed] [Google Scholar]
- 15.Kim H, Kim TH, Cha MJ, et al. A prospective survey of atrial fibrillation management for real-world guideline adherence: COmparison study of Drugs for symptom control and complication prEvention of Atrial Fibrillation (CODE-AF) Registry. Korean Circ J. 2017;47:877–887. doi: 10.4070/kcj.2017.0146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64:e1–e76. doi: 10.1016/j.jacc.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 17.Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138:1093–1100. doi: 10.1378/chest.10-0134. [DOI] [PubMed] [Google Scholar]
- 18.Friberg L, Rosenqvist M, Lip GY. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: the Swedish Atrial Fibrillation cohort study. Eur Heart J. 2012;33:1500–1510. doi: 10.1093/eurheartj/ehr488. [DOI] [PubMed] [Google Scholar]
- 19.Tomita H, Okumura K, Inoue H, et al. Validation of risk scoring system excluding female sex from CHA2DS2-VASc in Japanese patients with nonvalvular atrial fibrillation - subanalysis of the J-RHYTHM Registry. Circ J. 2015;79:1719–1726. doi: 10.1253/circj.CJ-15-0095. [DOI] [PubMed] [Google Scholar]
- 20.Okumura K, Inoue H, Atarashi H, et al. Validation of CHA(2)DS(2)-VASc and HAS-BLED scores in Japanese patients with nonvalvular atrial fibrillation: an analysis of the J-RHYTHM Registry. Circ J. 2014;78:1593–1599. doi: 10.1253/circj.cj-14-0144. [DOI] [PubMed] [Google Scholar]
- 21.Suzuki S, Yamashita T, Okumura K, et al. Incidence of ischemic stroke in Japanese patients with atrial fibrillation not receiving anticoagulation therapy--pooled analysis of the Shinken Database, J-RHYTHM Registry, and Fushimi AF Registry. Circ J. 2015;79:432–438. doi: 10.1253/circj.CJ-14-1131. [DOI] [PubMed] [Google Scholar]
- 22.Lee JM, Kim JB, Uhm JS, Pak HN, Lee MH, Joung B. Additional value of left atrial appendage geometry and hemodynamics when considering anticoagulation strategy in patients with atrial fibrillation with low CHA2DS2-VASc scores. Heart Rhythm. 2017;14:1297–1301. doi: 10.1016/j.hrthm.2017.05.034. [DOI] [PubMed] [Google Scholar]
- 23.Cooke FL. Women’s participation in employment in Asia: a comparative analysis of China, India, Japan and South Korea. Int J Hum Resour Manage. 2010;21:2249–2270. [Google Scholar]
- 24.Patterson L, Walcutt B. Korean workplace gender discrimination research analysis: a review of the literature from 1990 to 2010. Asia Pac Bus Rev. 2013;19:85–101. [Google Scholar]
- 25.Hsu JC, Maddox TM, Kennedy K, et al. Aspirin instead of oral anticoagulant prescription in atrial fibrillation patients at risk for stroke. J Am Coll Cardiol. 2016;67:2913–2923. doi: 10.1016/j.jacc.2016.03.581. [DOI] [PubMed] [Google Scholar]
- 26.Lip GY, Rushton-Smith SK, Goldhaber SZ, et al. Does sex affect anticoagulant use for stroke prevention in nonvalvular atrial fibrillation? The prospective global anticoagulant registry in the FIELD-Atrial Fibrillation. Circ Cardiovasc Qual Outcomes. 2015;8:S12–S20. doi: 10.1161/CIRCOUTCOMES.114.001556. [DOI] [PubMed] [Google Scholar]
- 27.Perino AC, Fan J, Schmitt SK, et al. Treating specialty and outcomes in newly diagnosed atrial fibrillation: from the TREAT-AF Study. J Am Coll Cardiol. 2017;70:78–86. doi: 10.1016/j.jacc.2017.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Steinberg BA, Shrader P, Thomas L, et al. Factors associated with non-vitamin K antagonist oral anticoagulants for stroke prevention in patients with new-onset atrial fibrillation: results from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation II (ORBIT-AF II) Am Heart J. 2017;189:40–47. doi: 10.1016/j.ahj.2017.03.024. [DOI] [PubMed] [Google Scholar]
- 29.Avgil Tsadok M, Jackevicius CA, Rahme E, Humphries KH, Pilote L. Sex Differences in dabigatran use, safety, and effectiveness in a population-based cohort of patients with atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2015;8:593–599. doi: 10.1161/CIRCOUTCOMES.114.001398. [DOI] [PubMed] [Google Scholar]