Summary
Bone morphogenetic proteins (BMPs) are a group of signalling molecules that belong to the transforming growth factor-β superfamily of proteins. Initially identified for their ability to induce bone formation, recent advances in the understanding of cellular and molecular mechanisms regarding BMPs have led to the use of the growth factor to accelerate bone healing. Recent clinical trials have demonstrated that BMPs, BMP-7 in particular, may present an alternative line of treatment other than the gold standard, autogenous bone grafting, in the treatment of fracture nonunion. We performed a literature search in September 2014 of PubMed and Embase using search terms, including “bone morphogenetic proteins”, “BMP-7”, “non-union”, “fracture healing” and “cost-effectiveness”, reviewing the efficacy, safety, and cost of treatment of nonunions with BMP-7. The authors further canvassed the reference lists of selected articles and used online search tools, such as Google Scholar. BMP-7 uses both the canonical and noncanonical signalling pathways. The treatment of fracture nonunion with recombinant human BMP-7 (rhBMP-7) has a comparable efficacy with that of autogenous bone grafting with an average union rate of 87% compared with 93% for bone grafting. Furthermore, fewer complications have been described with the use of rhBMP-7 compared with traditional bone grafting. We describe the signalling pathways that BMP-7 uses to exert its effect on bone. In nonunions, rhBMP-7 has been shown to have a similar efficacy to bone grafting with fewer complications.
Keywords: autograft, BMP-7, fracture healing, nonunion, osteogenesis
Introduction
In 1965, Urist [1] demonstrated that the demineralised, lyophilised segments of a bone were capable of a new bone formation when implanted into ectopic sites in rabbits. Subsequent research in the 1980s led to the dissociation of the bone-inducing component from the demineralised bone matrix into a soluble component using acid and chaotropic agents [2]. Following a biochemical analysis of the extract, proteins were cloned and tested for in vivo activity. An analysis of these clones indicated that the bone-inductive extract consisted of a highly conserved family of related proteins, named bone morphogenetic proteins (BMPs) [3]. This family consists of dimeric molecules belonging to the transforming growth factor-β (TGF-β) superfamily, containing a highly conserved seven-cysteine TGF-β domain in their C-termini [4]. To date, approximately 20 BMP family members have been identified and characterised [5] (Table 1).
Table 1.
Bone morphogenetic proteins with musculoskeletal function (modified from (5)).
| Identification | Description |
|---|---|
| BMP-2 | Bone and cartilage morphogenesis, osteoinduction, osteoblast differentiation, apoptosis |
| BMP-3 | Negative regulator of bone morphogenesis |
| BMP-3b | Negative regulator of bone morphogenesis |
| BMP-4 | Cartilage, teeth and bone morphogenesis |
| BMP-5 | Limb development, cartilage and bone morphogenesis |
| BMP-6 | Osteoblast differentiation, chondrogenesis |
| BMP-7 | Cartilage and bone morphogenesis |
| BMP-8 | Bone and cartilage morphogenesis |
| BMP-9 | Bone morphogenesis |
| BMP-11 | Axial-skeleton patterning |
| BMP-12 | Ligament and tendon development |
| BMP-13 | Cartilage development |
| BMP-14 | Chondrogenesis, angiogenesis |
BMP = bone morphogenetic protein.
Further evidence that BMPs were responsible for the bone-inductive activity in bone matrix was found in the recombinant expression of each of these proteins. By the use of molecular-biology techniques and sequence information from the bovine molecular clones, the human homologues of each BMP coding sequence were obtained. Mammalian cells were engineered to express the protein by inserting a vector encoding human BMP into the mammalian cell host of choice, resulting in the production of a single BMP molecule on amplification [6]. Early studies utilising this method focused on the function of BMP-7 [6]. Researchers were able to demonstrate that implantation of recombinant human BMP-7 (rhBMP-7) was capable of inducing a new bone formation. Numerous subsequent studies have proven the potency of rhBMP-7 using critical-size long-bone defects. These defects are defined by not being able to heal without therapeutic intervention and the application of exogenous stimuli. The implantation of BMP-7 into surgically created critical-size diaphyseal segmental defects led to the regeneration of a new bone that was fully functional both biologically and biomechanically [7], [8]. The therapeutic potential of BMP-7 has been widely studied in both animal studies and human clinical trials [9], [10]. Given the potential of BMPs in orthopaedic applications, this has resulted in the commercialisation of rhBMP-7.
Due to the supportive preclinical and clinical data, and approval from the Food and Drug Administration, rhBMP-7 (also known as osteogenic protein-1) is now commercially available. BMP-7 is now widely used in a variety of complex orthopaedic conditions either as an adjunct or as an alternative. It is particularly useful in the nonunion of bone as an alternative to conventional autogenous bone grafting (ABG), where the use of ABG alone is not feasible and/or other alternative treatments have failed. Recent studies have shown the efficacy of rhBMP-7 in inducing bone formation in nonunions to be equivalent to ABG. However, the avoidance of considerable issues, including donor-site morbidity, volume constraints, and infection commonly associated with ABG, has made rhBMP-7 an attractive alternative in the stimulation of bone formation [10], [11]. The aim of this review is to discuss recent advances in the molecular mechanism of BMP-7, as well as clinical studies regarding the efficacy of rhBMP-7, in treating fracture nonunion.
Methods
A literature search was performed (September 2014) of PubMed and Embase using various combinations of the keyword terms “bone morphogenetic protein”, “BMP”, “BMP-7”, “non-union”, “cost-effectiveness” and “signalling”, and their associated synonyms. The inclusion criteria were papers written in English, peer-reviewed journals, randomised controlled trials, and prospective and retrospective case series. The exclusion criteria were abstracts, case reports, and reviews. For the “signalling” and “complications” sections, reviews were included. The authors further searched the reference lists of selected articles and online search engines, such as Google Scholar.
BMP signalling
The BMP family belongs to the TGF-β superfamily of growth factors, which are involved in vast cellular processes of fundamental importance. For example, TGF-β has been demonstrated to be central to embryogenesis in mammals, controlling the formation of neural tube, limbs, cartilage, and bone [12], [13]. BMPs comprise a large group of phylogenetically conserved growth factors of which 20 members have been identified. In bone, BMPs are produced by osteoprogenitor cells, osteoblasts, chondrocytes, and platelets [14]. BMPs are potent osteoblast-differentiation factors, inducing the differentiation of multipotent mesenchymal cells into both osteochondrogenic lineage cells and osteoblast precursor cells [15], [16]. The molecular basis of their action has been the subject of intensive research in recent years, leading to a growing understanding of their fundamental action at a cellular level. Initially, all BMPs are synthesised as precursor proteins with an N-terminal signal peptide, a prodomain for folding and secretion, and a C-terminal mature peptide. Precursors are produced in the cytoplasm, and then cleaved to generate N- and C-terminal fragments. The C-terminal mature fragment is capable of binding to its receptor [17]. BMPs can signal through both canonical and noncanonical pathways.
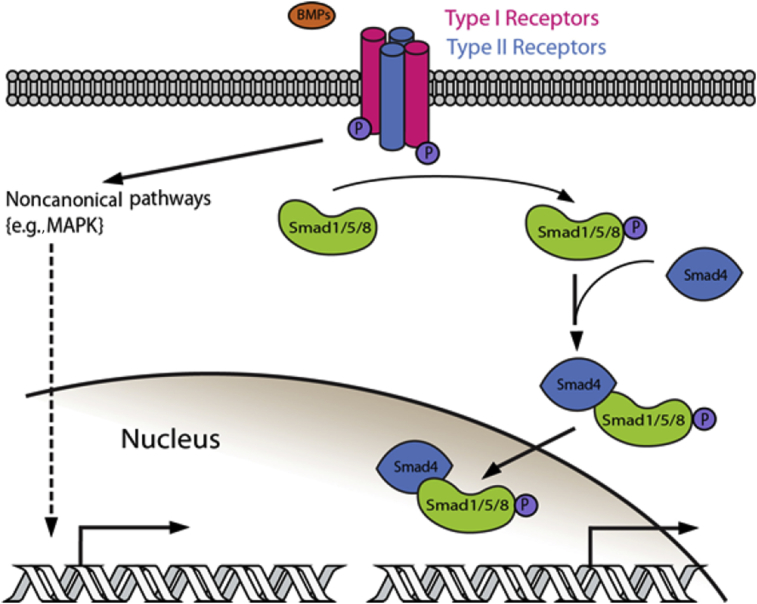
With regard to the canonical pathway, BMPs have been demonstrated to initiate the signal-transduction cascade by binding to cell surface receptors acting as a ligand, and forming a complex that comprises two dimers of type I (BMPR-I) and type II (BMPR-II) serine/threonine kinase receptors (Figure 1) [14], [18]. Six different receptors were identified to bind BMPs. Type I receptors include activin receptor type Ia (ActRIa), BMP receptor type Ia (BRIa) and BMP receptor type Ib. They form hetero-tetrameric complexes with the following type II receptors: BMP receptor type II (BRII), Activin receptors type IIA and IIB (ActRIIA and ActRIIB) (19). In the case of BMP-7, the growth factor has been proposed to first bind to the type II receptor followed by recruitment and phosphorylation of the type I receptor [19]. Subsequently, the activated type I receptors phosphorylate intracellular effector proteins, receptor-regulated Smads, activating Smad1, Smad5, and Smad8 (Smad1/5/8) [20]. The activation of receptor-regulated Smads then allows the formation of a complex with comediator Smad, Smad4, which translocates to the nucleus, functioning as a transcription factor and regulating gene expression. In addition to the Smad-dependent activation, other BMP signalling pathways have also been identified and shown to mediate the osteoinductive signals of BMPs. These include the Smad-independent p38 mitogen-activated protein-kinase pathway and phosphatidylinositol 3-kinase/protein kinase b pathway (noncanonical pathway) [21].
Figure 1.
BMPs signal via the Smad-dependent pathway (canonical) or various non-Smad dependent pathways. In the canonical BMPs bind type I or type II receptors, forming a heterotetrameric complex. Receptor activation allows the phosphorylation of R-Smads (Smad1/5/8). Phosphorylated R-Smads associate with co-Smad (Smad 4). The complex translocates to the nucleus to regulate gene expression. Non-canonical pathways, including mitogen-actviated protein kinase, can also lead to regulation of gene expression (modified from (17)).
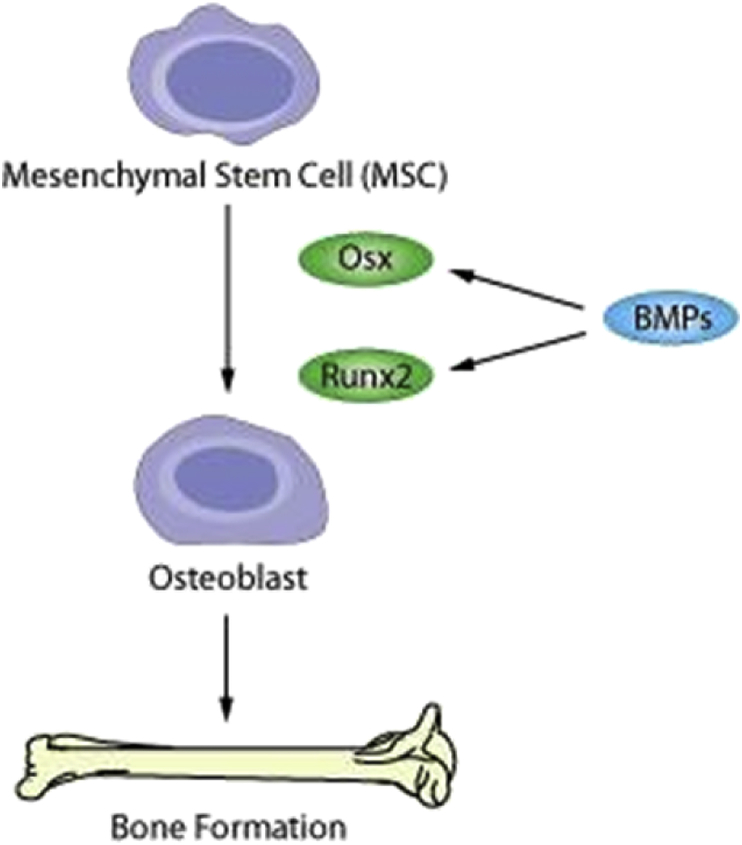
The postulated convergence of the two pathways in relation to osteogenesis occurs at the regulation of various transcription factors, in particular, at the runt-related transcription factor 2 and Osterix genes, key transcription factors in osteoblast differentiation [22], [23]. The deletion of Osterix and runt-related transcription factor 2 has been shown to cause the loss of ossification [24]. This mechanism initiates the signal cascade leading to bone differentiation (Figure 2). At a cellular level, BMPs diffuse through a concentration gradient acting as ligands for receptors present on plasma membranes of various cells, such as osteoblasts as well as mesenchymal stem cells, inducing differentiation and proliferation following a defined spatial arrangement [4]. Ultimately, cells are stimulated to differentiate into chondrocytes within 5–7 days of application of BMP. Upon capillary invasion, the chondrocytes become calcified and hypertrophied, and are subsequently replaced by new formed bone within 9–12 days. The mineralised bone undergoes remodelling and becomes occupied by ossicles filled with functional bone-marrow elements by 14–21 days. This process of bone formation is equivalent to that which occurs physiologically; therefore, BMPs appear to play a central regulatory role in ossification and bone healing. This understanding, as well as the preclinical research, indicates the potential of BMPs as a biological enhancer of bone formation, particularly in cases of nonunion, where this may not be occurring naturally, and has led to further research in a clinical setting.
Figure 2.
Image illustrating the molecular mechanism by which bone morphogenetic proteins stimulate bone formation. Initially, mesenchymal stem cells are stimulated to proceed down the osteogenic lineage. Stimulation occurs due to bone-morphogenetic-protein activity, leading to increased expression of runt-related transcription factor 2 and Osterix, necessary for osteoblast differentiation. BMP = bone morphogenetic protein; Osx = Osterix; Runx2 = runt-related transcription factor 2.
rhBMP-7 and fracture healing
Over the past decade, there have been several studies regarding the use of rhBMP-7 in the setting of fracture healing. Nonunion can occur following long-bone fracture, with a prevalence estimated to be approximately 10% of all fractures, increasing to 50% for open tibial fractures [25], [26]. Nonunion is defined as the absence of bone union following a fracture that requires additional treatment before healing can occur (>9 months), characterised by sclerotic fracture edges with sealing of medullary canals often being described as pseudarthrosis (false joint) [27]. Nonunions are further divided into hypertrophic, normotrophic, and atrophic dependent on the degree of callus formation. The surgical treatment for all types may involve the removal of ineffective or infected hardware, bone stabilisation, and eradication of infection if present [28]. In atrophic nonunions, characterised by the absence of callus and atrophic bone ends with deficient vascularity, further debridement of necrotic tissue with opposition of viable and vascular bone fragments is necessary. In addition, biological stimulation is required, as nonunion is incapable of a sufficient biological reaction. Autogenous cancellous bone grafting remains the gold-standard method for inducing union at the fracture site. Bone matrix represents a natural reservoir able to deliver various proteins and growth factors in significant quantities at the fracture site, including collagen-I, insulin-like growth factor-1, TGF-β, acidic fibroblast growth factor, vascular endothelial growth factor, and platelet-derived growth factor [29]. Bone matrix is therefore harvested from donor sites, such as the iliac crest of the patient, and is used as a stimulant to induce bone formation at the site of nonunion. However, the limited availability of bone suitable for grafting, as well as the considerable morbidity and complications associated with grafting [30], [31], [32], have led to the development of alternative biologically stimulating agents, such as rhBMP-7.
Several randomised controlled trials and cohort studies (Table 2) have been published with regard to fracture nonunion treatment [10], [33], [34], [35], [36], [37]. Friedlaender et al [35] published a prospective randomised controlled trial comparing the treatment of tibial fracture nonunions with rhBMP-7 and ABG. One hundred and twenty-two patients were enrolled in the multicentre trial, and each patient was treated by insertion of an intramedullary rod, accompanied by either rhBMP-7 in a type I collagen carrier (3.5 mg) or by bone autograft. Follow up, 9 months after the operative procedures, demonstrated that 81% of nonunions treated with rhBMP-7 had united, compared with 85% of those receiving autogenous bone. At 2 years follow up, there was no significant difference in the union rate between the two groups, demonstrating a comparable efficacy between the two treatment groups. Friedlaender et al [35] provided level 1 evidence that rhBMP-7 is as effective as ABG in the treatment of tibial nonunion when used with intramedullary rod fixation.
Table 2.
Clinical studies on the application of bone morphogenetic proteins at various anatomical sites with an indication of nonunion.
| Authors | Type of study | Level of evidence | No. of cases of BMPs | Carrier method and dose | Indication (anatomical site of nonunion) | Union rates (%) | Mean time to union (mo) | Reoperation (%) |
|---|---|---|---|---|---|---|---|---|
| Friedlaender et al 2001 [35] | Prospective randomised controlled (BMP-7 vs. ABG) | II | 63 | Collagen 3.5 mg | Tibial | 75–81 | 9 | 5 |
| Dimitriou et al 2005 [33] | Prospective observational (BMP-7) | IV | 25 | Collagen 3.5 mg | Tibial–femoral–humeral–forearm | 92.3 | 5.6 | 12 |
| Kanakaris et al 2009 [10] | Prospective observational (BMP-7) | IV | 30 | Collagen 3.5 mg | Femoral | 86.7 | 6 | 13 |
| Giannoudis and Tzioupis 2005 [36] | Retrospective cohort study (BMP-7) | IV | 395 | Collagen 3.5 mg | Femoral–tibial–clavicle–ankle–radius–scaphoid–ankle–humerus–olecranon | 82 | n/a | n/a |
| Desmyter et al 2008 [37] | Retrospective cohort study | IV | 62 | Collagen 3.5 mg | Tibial | 84.9 | 7.5 | 14 |
| Calori et al 2008 [34] | Prospective randomised controlled (BMP-7 vs. PRP) | III | 5 | Collagen 3.5 mg | Femoral | 100 | 8 | 6.2 |
ABG = autogenous bone grafting; BMP = bone morphogenetic protein; PRP = Platelet-rich plasma.
More recently, Kanakaris et al [10] conducted an observational study describing the management of femoral fracture nonunions using rhBMP-7 in six different European university centres over a period of 5 years. The study included 30 patients that had undergone a median of one revision operation before rhBMP-7 application, and were followed up for a median of 24 months. In 23 cases, the application of rhBMP-7 was combined with a revision of fixation, and 12 cases also included autograft. The BMP-treated patients were treated with 3.5 mg rhBMP-7. Nonunion healing occurred in 86.7% of the cases in a median period of 6 months, which is comparable with the conventional gold-standard treatment with ABG [11]. No systemic allergic reactions or adverse effects were noted following the application of rhBMP-7, and no complications related to the bone substitute were observed. Thus, this study showed that BMP-7 is as effective as ABG for femoral fracture nonunions.
A retrospective study carried out in the UK by Giannoudis and Tzioupis [36] reported on 395 patients affected by nonunion. A single application of 3.5 mg rhBMP-7 was used during a concurrent treatment with appropriate surgical stabilisation of the fracture nonunion. The overall success rate was up to 82%. No systemic complications or adverse effects from the application of rhBMP-7 were reported. A similar study in Belgium regarding tibial fracture nonunions observed a union rate of 84.9% in the average of 7.5 months [37].
Discussion
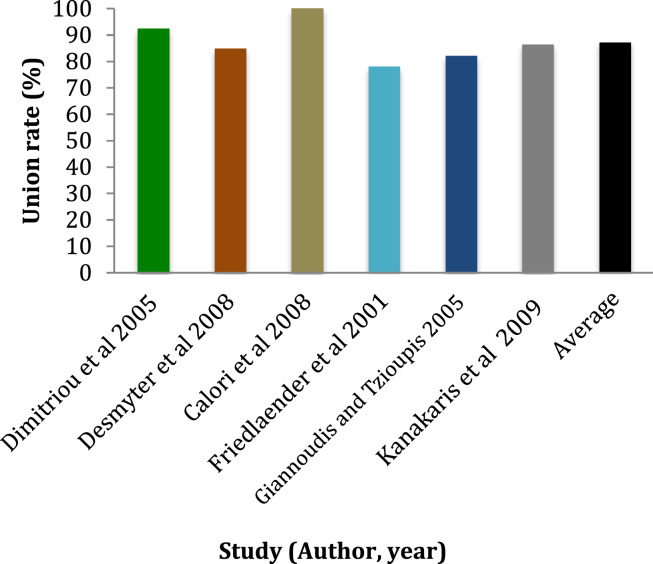
The nature of bone induction and regeneration is now better understood. BMP-7 has demonstrated its ability in a number of animal models to induce bone formation and favourably influence the process of bone repair. The growth factor has been demonstrated to have the capacity to recruit and stimulate differentiation and proliferation of osteogenic cell populations. The increased interest in rhBMP-7 as a novel treatment for fracture healing in recent years has led to clinical trials that show both safety and efficacy comparable with the current gold standard, ABG. A series of studies over the past decade have also shown healing rates for rhBMP-7 between 75% and 100% (Figure 3) [10], [33], [34], [35], [36], [37]. ABG has shown a healing rate of 87–100% for tibial nonunion [11]. These results should be interpreted in the context of other factors involved in treatment options, such as indications, contraindications, complication rate, and economic factors. It is important to recognise the need to follow established surgical principles, including the establishment of a bacteriologically clean, viable, and well-vascularised surgical site with adequate stabilisation of fracture, perquisites to the success of any osteogenic stimulus [28].
Figure 3.
Graph illustrating the union rate demonstrated in various studies regarding the efficacy of recombinant human bone morphogenetic protein-7 in healing fracture nonunions and the calculated average overall of all reviewed studies.
Treatment with rhBMP-7 shows a lower morbidity and mortality rate than ABG. Goulet et al [38] studied the complications seen in the harvesting of ABGs, and found an incidence of 2.4% for major complications (defined as a requirement for additional hospitalisation related to the wound site) and 21.8% for minor complications (defined as complications at the wound site requiring additional medical attention, but no further hospitalisation). Some patients (37.9%) reported pain at the graft harvest site 6 months postoperatively. The potential to avoid these complications is an advantage of the rhBMP-7 treatment.
Conversely, treatment with rhBMP-7 is associated with few complications. Kanakaris et al [10] reported that no adverse effects directly related to the procedure were seen in their case series. Courvoisier et al [39] completed a literature review to determine the safety of rhBMP-7 for use in long-bone nonunion, and were able to recommend the product for this purpose. The only notable adverse effect was transient aseptic wound swelling, seen more often when the BMP is located superficially. Certain immunologic problems have been reported, with both anticollagen and anti-rhBMP proteins identified, however, these do not necessarily or often predict adverse clinical outcomes [40]. Poynton and Lane [40] reported that low-titre immune responses were recorded in 38% of patients treated with rhBMP-7, with no associated clinical adverse effects; however, they did not recommend the repeated use of rhBMP-7 for this reason. The observed immunologic responses have been demonstrated to be positively correlated with higher doses of BMP and collagen. Poynton and Lane [40] also concluded that rhBMP-7 is safe for normal clinical use, with no systemic or local toxicity, and no organ damage or carcinogenicity found. The long-term effects of these low-titre immune responses need to be investigated for potential delayed host reactions.
The current typical dosage of BMP-7 is 3.5 mg, and it is generally administered bound to 1 g of bovine-collagen granules that act as a scaffold for bone formation (see Table 2). This produces a concentration of BMP-7 that is many times above the physiological level. Given that Shields et al [41] suggest that the complication rate of BMP-2 usage is dose dependent, it may be possible to further reduce complication rates by decreasing the amount of BMP-7 administered. Priddy et al [42] developed a novel method for delivering BMP-2 in an oxidised alginate hydrogel, which allowed them to use a lower concentration of the drug with no loss of efficacy. This constitutes an area for future research in BMP-7 technology due to the paucity of data presently.
Another factor that must be considered when discussing a new treatment option is the overall economic cost to the patient. The use of rhBMP-7 compares favourably with ABG in this regard, in terms of length of hospital stay (8.66–10.66 days) and length of convalescence (5.5–6.9 months) [43]. The total bill for direct medical costs was found to be 6.78% higher in the rhBMP-7 group than in the ABG group, largely due to the high cost of the rhBMP-7 itself; however, given the significant reduction in hospital stay, morbidity and mortality, and convalescence of the rhBMP-7 group, Dahabreh et al [43] were able to advocate in favour of the overall economic benefits of rhBMP-7 treatment. In addition, Garrison et al [44] concluded from the available evidence that the economic benefits of rhBMP-7 are likely to be more pronounced in serious fractures that would otherwise result in longer convalescent times.
The use of rhBMP-7 in combination with ABG has been studied and found to show higher rates of fracture healing than either method alone. Giannoudis et al [45] applied this treatment rationale to 45 patients with nonunion of a long bone and median of two previous operations, and were able to demonstrate clinical and radiologic healing in 100% of those patients.
Conclusion
When viewed in the wider context of economic and clinical benefits compared with the existing gold standard, rhBMP-7 appears to be a promising line of treatment that shows particular potential in the treatment of fractures resistant to healing. Clinical trials provide evidence to support the equivalent efficacy of rhBMP-7 and ABG in terms of healing rates, showing similar results for the two treatment methods (87% vs. 93%). However, the favourable safety profile of rhBMP-7, and the obviation of a bone autograft donor site and its associated morbidity and mortality support rhBMP-7 as the preferred method of therapeutic intervention in nonunions. Existing data suggest that rhBMP-7 should be reserved for more difficult cases, particularly in cases of recalcitrant nonunions, although growing clinical experience using this evolving technology will more than likely see the expansion of clinical applications of rhBMP-7.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Urist M.R. Bone: formation by autoinduction. Science. 1965 Nov 12;150(3698):893–899. doi: 10.1126/science.150.3698.893. [DOI] [PubMed] [Google Scholar]
- 2.Sampath T.K., Reddi A.H. Dissociative extraction and reconstitution of extracellular matrix components involved in local bone differentiation. Proc Natl Acad Sci U S A. 1981 Dec;78(12):7599–7603. doi: 10.1073/pnas.78.12.7599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Celeste A.J., Iannazzi J.A., Taylor R.C., Hewick R.M., Rosen V., Wang E.A. Identification of transforming growth factor beta family members present in bone-inductive protein purified from bovine bone. Proc Natl Acad Sci. 1990 Dec 1;87(24):9843–9847. doi: 10.1073/pnas.87.24.9843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matthews S.J.E. Biological activity of bone morphogenetic proteins (BMP’s) Injury. 2005 Nov;36(Suppl 3):S34–S37. doi: 10.1016/j.injury.2005.07.032. [DOI] [PubMed] [Google Scholar]
- 5.Bessa P.C., Casal M., Reis R.L. Bone morphogenetic proteins in tissue engineering: the road from the laboratory to the clinic, part I (basic concepts) J Tissue Eng Regen Med. 2008 Jan;2(1):1–13. doi: 10.1002/term.63. [DOI] [PubMed] [Google Scholar]
- 6.Israel D.I., Nove J., Kerns K.M., Moutsatsos I.K., Kaufman R.J. Expression and characterization of bone morphogenetic protein-2 in Chinese hamster ovary cells. Growth Factors Chur Switz. 1992;7(2):139–150. doi: 10.3109/08977199209046403. [DOI] [PubMed] [Google Scholar]
- 7.Cook S.D., Baffes G.C., Wolfe M.W., Sampath T.K., Rueger D.C. Recombinant human bone morphogenetic protein-7 induces healing in a canine long-bone segmental defect model. Clin Orthop. 1994 Apr;(301):302–312. [PubMed] [Google Scholar]
- 8.Cook S.D., Baffes G.C., Wolfe M.W., Sampath T.K., Rueger D.C., Whitecloud T.S. The effect of recombinant human osteogenic protein-1 on healing of large segmental bone defects. J Bone Joint Surg Am. 1994 Jun;76(6):827–838. doi: 10.2106/00004623-199406000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Hak D.J., Makino T., Niikura T., Hazelwood S.J., Curtiss S., Reddi A.H. Recombinant human BMP-7 effectively prevents non-union in both young and old rats. J Orthop Res Off Publ Orthop Res Soc. 2006 Jan;24(1):11–20. doi: 10.1002/jor.20022. [DOI] [PubMed] [Google Scholar]
- 10.Kanakaris N.K., Lasanianos N., Calori G.M., Verdonk R., Blokhuis T.J., Cherubino P. Application of bone morphogenetic proteins to femoral non-unions: A 4-year multicentre experience. Injury. 2009 Dec;40(Supplement 3):S54–S61. doi: 10.1016/S0020-1383(09)70013-0. [DOI] [PubMed] [Google Scholar]
- 11.Sen M.K., Miclau T. Autologous iliac crest bone graft: should it still be the gold standard for treating nonunions? Injury. 2007 Mar;38(Suppl 1):S75–S80. doi: 10.1016/j.injury.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 12.Tsumaki N., Yoshikawa H. The role of bone morphogenetic proteins in endochondral bone formation. Cytokine Growth Factor Rev. 2005 Jun;16(3):279–285. doi: 10.1016/j.cytogfr.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 13.Bragdon B., Moseychuk O., Saldanha S., King D., Julian J., Nohe A. Bone morphogenetic proteins: a critical review. Cell Signal. 2011 Apr;23(4):609–620. doi: 10.1016/j.cellsig.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Nohe A., Keating E., Knaus P., Petersen N.O. Signal transduction of bone morphogenetic protein receptors. Cell Signal. 2004 Mar;16(3):291–299. doi: 10.1016/j.cellsig.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 15.Shen B., Wei A., Whittaker S., Williams L.A., Tao H., Ma D.D.F. The role of BMP-7 in chondrogenic and osteogenic differentiation of human bone marrow multipotent mesenchymal stromal cells in vitro. J Cell Biochem. 2010 Feb 1;109(2):406–416. doi: 10.1002/jcb.22412. [DOI] [PubMed] [Google Scholar]
- 16.Yeh L.-C.C., Tsai A.D., Lee J.C. Osteogenic protein-1 (OP-1, BMP-7) induces osteoblastic cell differentiation of the pluripotent mesenchymal cell line C2C12. J Cell Biochem. 2002;87(3):292–304. doi: 10.1002/jcb.10315. [DOI] [PubMed] [Google Scholar]
- 17.Harrison C.A., Al-Musawi S.L., Walton K.L. Prodomains regulate the synthesis, extracellular localisation and activity of TGF-β superfamily ligands. Growth Factors Chur Switz. 2011 Oct;29(5):174–186. doi: 10.3109/08977194.2011.608666. [DOI] [PubMed] [Google Scholar]
- 18.Wang R.N., Green J., Wang Z., Deng Y., Qiao M., Peabody M. Bone Morphogenetic Protein (BMP) signaling in development and human diseases. Genes Dis. 2014 Sep;1(1):87–105. doi: 10.1016/j.gendis.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Caestecker M. The transforming growth factor-beta superfamily of receptors. Cytokine Growth Factor Rev. 2004 Feb;15(1):1–11. doi: 10.1016/j.cytogfr.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 20.Miyazono K., Kamiya Y., Morikawa M. Bone morphogenetic protein receptors and signal transduction. J Biochem (Tokyo) 2010 Jan;147(1):35–51. doi: 10.1093/jb/mvp148. [DOI] [PubMed] [Google Scholar]
- 21.Aubin J., Davy A., Soriano P. In vivo convergence of BMP and MAPK signaling pathways: impact of differential Smad1 phosphorylation on development and homeostasis. Genes Dev. 2004 Jun 15;18(12):1482–1494. doi: 10.1101/gad.1202604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen G., Deng C., Li Y.-P. TGF-Beta and BMP signaling in osteoblast differentiation and bone formation. Int J Biol Sci. 2012 Jan 21;8(2):272–288. doi: 10.7150/ijbs.2929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Komori T. Regulation of osteoblast differentiation by Runx2. Adv Exp Med Biol. 2010;658:43–49. doi: 10.1007/978-1-4419-1050-9_5. [DOI] [PubMed] [Google Scholar]
- 24.Carreira A.C., Alves G.G., Zambuzzi W.F., Sogayar M.C., Granjeiro J.M. Bone morphogenetic proteins: structure, biological function and therapeutic applications. Arch Biochem Biophys. 2014 Nov 1;561:64–73. doi: 10.1016/j.abb.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 25.Phieffer L.S., Goulet J.A. Delayed unions of the tibia. J Bone Jt Surg. 2006 Jan 1;88(1):205–216. doi: 10.2106/00004623-200601000-00026. [DOI] [PubMed] [Google Scholar]
- 26.Dickson K., Katzman S., Delgado E., Contreras D. Delayed unions and nonunions of open tibial fractures. Correlation with arteriography results. Clin Orthop. 1994 May;(302):189–193. [PubMed] [Google Scholar]
- 27.Frölke J.P.M., Patka P. Definition and classification of fracture non-unions. Injury. 2007 May;38(Supplement 2):S19–S22. doi: 10.1016/s0020-1383(07)80005-2. [DOI] [PubMed] [Google Scholar]
- 28.Giannoudis P.V., Einhorn T.A., Marsh D. Fracture healing: the diamond concept. Injury. 2007 Sep;38(Suppl 4):S3–S6. doi: 10.1016/s0020-1383(08)70003-2. [DOI] [PubMed] [Google Scholar]
- 29.Wildemann B., Kadow-Romacker A., Haas N.P., Schmidmaier G. Quantification of various growth factors in different demineralized bone matrix preparations. J Biomed Mater Res A. 2007 May;81(2):437–442. doi: 10.1002/jbm.a.31085. [DOI] [PubMed] [Google Scholar]
- 30.Palmer W., Crawford-Sykes A., Rose R.E.C. Donor site morbidity following iliac crest bone graft. West Indian Med J. 2008 Nov;57(5):490–492. [PubMed] [Google Scholar]
- 31.Banwart J.C., Asher M.A., Hassanein R.S. Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine. 1995 May 1;20(9):1055–1060. doi: 10.1097/00007632-199505000-00012. [DOI] [PubMed] [Google Scholar]
- 32.Younger E.M., Chapman M.W. Morbidity at bone graft donor sites. J Orthop Trauma. 1989;3(3):192–195. doi: 10.1097/00005131-198909000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Dimitriou R., Dahabreh Z., Katsoulis E., Matthews S.J., Branfoot T., Giannoudis P.V. Application of recombinant BMP-7 on persistent upper and lower limb non-unions. Injury. 2005 Nov;36(4, Supplement):S51–S59. doi: 10.1016/j.injury.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 34.Calori G.M., Tagliabue L., Gala L., d’Imporzano M., Peretti G., Albisetti W. Application of rhBMP-7 and platelet-rich plasma in the treatment of long bone non-unions: A prospective randomised clinical study on 120 patients. Injury. 2008 Dec;39(12):1391–1402. doi: 10.1016/j.injury.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 35.Friedlaender G.E., Perry C.R., Dean Cole J., Cook S.D., Cierny G., Muschler G.F. Osteogenic protein-1 (bone morphogenetic protein-7) in the treatment of tibial nonunions. J Bone Joint Surg Am. 2001;83-A(Suppl 1(Pt 2)):S151–S158. [PMC free article] [PubMed] [Google Scholar]
- 36.Giannoudis P.V., Tzioupis C. Clinical applications of BMP-7: The UK perspective. Injury. 2005 Nov;36(3, Supplement):S47–S50. doi: 10.1016/j.injury.2005.07.035. [DOI] [PubMed] [Google Scholar]
- 37.Desmyter S., Goubau Y., Benahmed N., de Wever A., Verdonk R. The role of bone morphogenetic protein-7 (Osteogenic Protein-1) in the treatment of tibial fracture non-unions. An overview of the use in Belgium. Acta Orthop Belg. 2008 Aug;74(4):534–537. [PubMed] [Google Scholar]
- 38.Goulet J.A., Senunas L.E., DeSilva G.L., Greenfield M.L. Autogenous iliac crest bone graft. Complications and functional assessment. Clin Orthop. 1997 Jun;(339):76–81. doi: 10.1097/00003086-199706000-00011. [DOI] [PubMed] [Google Scholar]
- 39.Courvoisier A., Sailhan F., Laffenêtre O., Obert L., French Study Group of BMP in Orthopedic Surgery Bone morphogenetic protein and orthopaedic surgery: can we legitimate its off-label use? Int Orthop. 2014 Dec;38(12):2601–2605. doi: 10.1007/s00264-014-2534-4. [DOI] [PubMed] [Google Scholar]
- 40.Poynton A.R., Lane J.M. Safety profile for the clinical use of bone morphogenetic proteins in the spine. Spine. 2002 Aug 15;27(16 Suppl 1):S40–S48. doi: 10.1097/00007632-200208151-00010. [DOI] [PubMed] [Google Scholar]
- 41.Shields L.B.E., Raque G.H., Glassman S.D., Campbell M., Vitaz T., Harpring J. Adverse effects associated with high-dose recombinant human bone morphogenetic protein-2 use in anterior cervical spine fusion. Spine. 2006 Mar;31(5):542–547. doi: 10.1097/01.brs.0000201424.27509.72. [DOI] [PubMed] [Google Scholar]
- 42.Priddy L.B., Chaudhuri O., Stevens H.Y., Krishnan L., Uhrig B.A., Willett N.J. Oxidized alginate hydrogels for bone morphogenetic protein-2 delivery in long bone defects. Acta Biomater. 2014 Oct;10(10):4390–4399. doi: 10.1016/j.actbio.2014.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dahabreh Z., Calori G.M., Kanakaris N.K., Nikolaou V.S., Giannoudis P.V. A cost analysis of treatment of tibial fracture nonunion by bone grafting or bone morphogenetic protein-7. Int Orthop. 2009 Oct;33(5):1407–1414. doi: 10.1007/s00264-008-0709-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Garrison K.R., Shemilt I., Donell S., Ryder J.J., Mugford M., Harvey I. Bone morphogenetic protein (BMP) for fracture healing in adults. Cochrane Database Syst Rev. 2010;(6):CD006950. doi: 10.1002/14651858.CD006950.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Giannoudis P.V., Kanakaris N.K., Dimitriou R., Gill I., Kolimarala V., Montgomery R.J. The synergistic effect of autograft and BMP-7 in the treatment of atrophic nonunions. Clin Orthop. 2009 Dec;467(12):3239–3248. doi: 10.1007/s11999-009-0846-2. [DOI] [PMC free article] [PubMed] [Google Scholar]