Summary
Female sex hormones play an important role in the aetiology and pathophysiology of a variety of musculoskeletal degenerative diseases. Postmenopausal women show accelerated disc degeneration due to relative oestrogen deficiency, resulting in narrower intervertebral disc space in women than age-matched men, increased prevalence of spondylolisthesis, and increased prevalence of facet joint osteoarthritis. Postmenopausal women also show higher osteoporosis related spine fracture rate, particularly at the thoracic–lumbar junction site. I propose the concept that low back pain (LBP) is more prevalent in postmenopausal women than age-matched men and is associated with the physiological changes caused by the relatively lower level of sex hormones after menopause in women. Considering hormone replacement treatment (HRT)'s consistent efficacy reported with menopause-associated osteoarthritis, an in-depth understanding of the role of the gonadal hormones in LBP modulation warrants further study. HRT initiated at early postmenopausal phase may be protective for recurring LBP. If this is the case, further cost–benefit analysis should be performed for optimal HRT regimen in cases of women with high risk of recurring severe LBP.
Keywords: epidemiology, intervertebral disc degeneration, low back pain, oestrogen, physiological sex difference
Oestrogens participate in a variety of biological processes through different molecular mechanisms. Oestrogen has favourable effects on the lipid profile, antioxidant activity, and enhanced fibrinolysis [1]. Female sex hormones also play an important role in the aetiology and pathophysiology of a variety of musculoskeletal degenerative diseases. The prevalence of osteoarthritis (OA) is higher among women than among men, and this prevalence increases considerably after menopause [2], [3]. Moreover, with the same degree of radiographic damage, OA is also more symptomatic in women [2], [3]. Young men are more susceptible to disc degeneration than young women, probably due to increased mechanical stress and physical injury [4], [5], [6]. However, recent evidence suggests that disc degeneration is common or more severe in elderly women than in elderly men [7], [8]. Postmenopausal women show accelerated disc degeneration due to relative oestrogen deficiency [9], [10]. Postmenopausal women also show narrower intervertebral disc space than age-matched men [8], [11], increased prevalence of spondylolisthesis [12], [13], [14], and increased prevalence of facet joint arthritis [15].
In the literature, the reported population-based low back pain (LBP) prevalence varies as it depends on the definitions of LBP as well as the survey method. A number of reports suggest that women have higher prevalence of LBP than men [16], [17], [18], [19], despite the fact that young and middle-aged men have higher prevalence and more severe intervertebral disc degeneration [4], [5], [6]. The higher LBP prevalence in women is probably due to many factors, including heightened pain sensitivity among women [20], [21], menstrual cycle fluctuations, biologic response and stress to pregnancy and childbearing, and perimenopausal abdominal weight gain [19]. Recently, it has been show that genetics also plays a role in the development of LBP [1], [22], [23]. A very recent systematic review, which was limited to population based studies with the same LBP criteria applied to both men and women in the same community, demonstrates, compared with middle-aged individuals, a further increased LBP prevalence in women than in men was noted after menopause age [24]. By contrast, in an evaluation of pain characteristics of adults aged ≥ 65 years referred to a tertiary pain care clinic, the older patients had relatively more physical problems concordant with their complaints, but fewer psychological factors contributing to disability than the younger patients [25], [26].
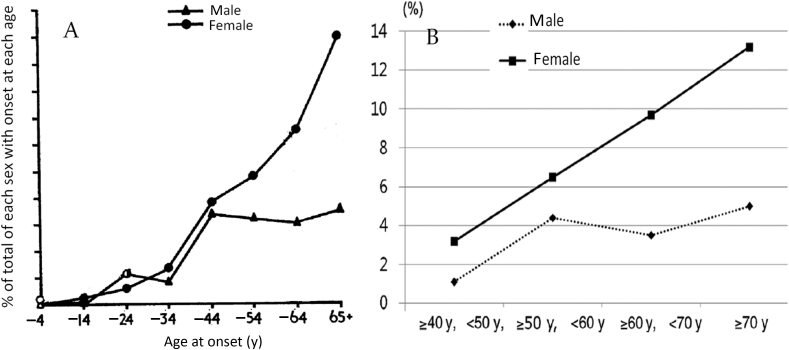
In some studies, LBP is strikingly more prevalent in postmenopausal women than age-matched men. In 1969, Lawrence [27] surveyed 713 men and 809 women aged ≥ 35 years with lumbar radiography in Manchester, UK. Back–hip–sciatic pain was present at the time of the survey in 79 (11%) of the men and in 153 (19%) of the women. In those with pain at the time of the survey, the incidence had risen up to age 40 years in men and then remained constant, but in women it continued to rise sharply up to and over the age of 65 years (Figure S1A). In 1995, Papageorgiou et al [28] reported the South Manchester Back Pain Survey with a study population of 4501 (age 18–75 years). The 1-month period prevalence of LBP was 31.2%, 33.1%, 38.5%, and 34.9% for the age ranges of 18–29 years, 30–44 years, 45–59 years, and ≥ 60 years, respectively, for men; 32.2%, 41.5%, 49.2%, and 43.7% for the age ranges of 18–29 years, 30–44 years, 45–59 years, and ≥ 60 years, respectively, for women. In 2010, Cho et al [29] published LBP data collected for 4181 individuals from a rural farming community in Korea. The participants had a mean age of 56.6 years and 55.5% were women. Six-month prevalence of LBP was 38.5 % for men and 55.6 for women. The prevalence of LBP increased significantly with age in women (Figure S1B). Data from the Osteoporotic Fractures in Men (Hong Kong) and Osteoporotic Fractures in Women (Hong Kong) Studies were published in 2013 [8]; 2000 Chinese men and 2000 Chinese women, aged ≥ 65 years, were prospectively recruited from local communities for a prospective cohort study from August 2001 to March 2003. The LBP prevalence was 30.6% for men and 53.3% for women (p < 0.001). While postmenopausal women also show higher osteoporosis-related spine fracture rate compared with age-matched men, and vertebral fracture is a known cause of back pain and related disability [30], the accelerated spine degeneration caused by the relatively lower level of sex hormones after menopause in women [9], [10], including narrower intervertebral disc space, higher lumbar spondylolisthesis prevalence, and increased prevalence of facet joint osteoarthritis, may be an additional source of LBP in elderly women.
Oestrogen with or without a progestogen prevents early postmenopausal bone loss and augments bone mass in late postmenopause as effectively as the bisphosphonates [29]. Hormone replacement treatment (HRT) has consistently been shown to be protective against menopause-associated OA [31], [32], [33], [34], [35].
However, to date the clinical data on HRT's effects on LBP remain contradictory. For example, Baron et al [36] found that women on HRT maintained intervertebral disc height compared with untreated postmenopausal women. They suggested that the oestrogenic milieu may be relevant because of the significant impact it has on the hydrophilic glycosaminoglycans, the water content, collagen, and elastin of the intervertebral discs. The maintenance of adequate disc height may allow the intervertebral discs to retain their discoid shape and viscoelastic function, containing vertical forces which may threaten spinal architecture leading to vertebral body compression fractures [36]. Kyllönen et al's [37] longitudinal clinical study supports that oestrogen–progestin replacement therapy was beneficial for lumbar spine mobility. In an experimental study, Li et al [38] reported that resveratrol, a phytoestrogen, is a potent anabolic mediator of bovine intervertebral disc cartilage homeostasis to slow the progression of disc degeneration. However, in one study Musgrave et al [39] reported that women taking HRT had more back pain and back pain-related disability than did those not taking HRT. In another study Symmons et al [40] also reported that oestrogen use was more common in the group reporting back pain than in the group without back pain. Considering that HRT is known to decrease vertebral fracture rate [31], and protect intervertebral disc [36], and maybe also facet joint [12], Musgrave et al's [39] and Symmons et al's [40] findings look counterintuitive. In one systemic review, Bressler et al [25] noted that there is an under-representation of the older population in the LBP pain literature. They stressed the need for future studies to improve the reporting of age information to make prevalence studies more informative and applicable.
The expert views of HRT have evolved during the past 10 years since the publication of Women's Health Initiative trials [41], [42]. Since the initial publication of the Women's Health Initiative hormone trial results, multiple secondary analyses have yielded interesting data that suggested that the risk of coronary heart disease was dependent upon both the timing of initiating hormone exposure as well as the age of the woman at the time of HRT initiation [43], [44]. Specifically, in the oestrogen-alone trial, a nonstatistically significant reduction in coronary heart disease risk was noted in participants aged 50–59 years [44]. Dose regimen, combination of oestrogen with progestins versus oestrogen alone, the administration route, and duration of treatment such as the choice of repetitive or periodic administration simulating the menstrual cycle are some of the factors that may be involved in benefit discrepancies. The Estrogen and Thromboembolism Risk study confirmed that oral oestrogens increased venous thromboembolism risk, whereas transdermal oestrogens had little or no impact on the development of thrombosis [45]. Recent Korean data do not support HRT history for the risk of breast cancer in women [46]. The presence of gene polymorphisms may also be implicated. HRT may benefit a large number of postmenopausal women, but a subset of women may have higher risk of cardiovascular and thrombotic complications [47]. Oestrogen receptor modulators and phytoestrogens may retain the desired effects but avoid undesirable effects [48]. Considering HRT's efficacy reported with menopause-associated OA in many studies, an in-depth understanding of the role of the gonadal hormones in LBP modulation warrants further study. HRT initiated at early postmenopausal phase may be protective for recurring LBP, as LBP tends to be a recurring phenomenon in nature. HRT protects both bone [31] and disc tissue [12], [36]. If this is the case, further cost–benefit analysis should be performed for optimal HRT regimen in cases of women with high risk of recurring severe LBP.
Conflicts of interest
The author has no conflicts of interest to declare.
Footnotes
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.jot.2016.05.012.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
Figure S1.
(A) Incidence of present back–hip–sciatic pain, by age and sex. (B) Prevalence of Grade 3–4 low back pain according to age and sex. The data show that after menopause, women have progressively higher low back pain prevalence than age-matched men. Note.Figure S1A is modified from “Disc degeneration. Its frequency and relationship to symptoms,” by Lawrence, 1969, Annals of the Rheumatic Diseases, 28, p. 121–138. Copyright 1969, BMJ Publishing Group Ltd & European League Against Rheumatism. Adapted with permission. Note.Figure S1B is modified from “The prevalence and risk factors of low back pain in rural community residents of Korea,” Cho et al, 2012, Spine, 37, p. 2001–2010. Copyright 2012, Lippincott Williams & Wilkins, Inc. Adapted with permission.
References
- 1.Tostes R.C., Nigro D., Fortes Z.B., Carvalho M.H. Effects of estrogen on the vascular system. Braz J Med Biol Res. 2003;36:1143–1158. doi: 10.1590/s0100-879x2003000900002. [DOI] [PubMed] [Google Scholar]
- 2.Srikanth V.K., Fryer J.L., Zhai G., Winzenberg T.M., Hosmer D., Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage. 2005;13:769–781. doi: 10.1016/j.joca.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 3.Lawrence R.C., Helmick C.G., Arnett F.C., Deyo R.A., Felson D.T., Giannini E.H. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778–799. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 4.Miller J.A., Schmatz C., Schultz A.B. Lumbar disc degeneration: correlation with age, sex, and spine level in 600 autopsy specimens. Spine. 1988;13:173–178. [PubMed] [Google Scholar]
- 5.Łebkowski W.J. Autopsy evaluation of the extent of degeneration of the lumbar intervertebral discs. Pol Merkuriusz Lek. 2002;13:188–190. [in Polish] [PubMed] [Google Scholar]
- 6.Takatalo J., Karppinen J., Niinimäki J., Taimela S., Näyhä S., Järvelin M.R. Prevalence of degenerative imaging findings in lumbar magnetic resonance imaging among young adults. Spine. 2009;34:1716–1721. doi: 10.1097/BRS.0b013e3181ac5fec. [DOI] [PubMed] [Google Scholar]
- 7.Wang Y.X., Kwok A.W., Griffith J.F., Leung J.C., Ma H.T., Ahuja A.T. Relationship between gender, bone mineral density, and disc degeneration in the lumbar spine: a study in elderly subjects using an eight level MRI-based disc degeneration grading system. Osteoporos Int. 2011;22:91–96. doi: 10.1007/s00198-010-1200-y. [DOI] [PubMed] [Google Scholar]
- 8.Wang Y.X., Griffith J.F., Zeng X.J., Deng M., Kwok A.W., Leung J.C. Prevalence and sex difference of lumbar disc space narrowing in elderly Chinese men and women: osteoporotic fractures in men (Hong Kong) and osteoporotic fractures in women (Hong Kong) studies. Arthritis Rheum. 2013;65:1004–1010. doi: 10.1002/art.37857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Y.X., Griffith J.F. Effect of menopause on lumbar disk degeneration: potential etiology. Radiology. 2010;257:318–320. doi: 10.1148/radiol.10100775. [DOI] [PubMed] [Google Scholar]
- 10.Wang Y.X., Wáng J.Q., Káplár Z. Postmenopausal Chinese women show accelerated lumbar disc degeneration compared with Chinese men. J Orthop Transl. 2015;3:205–211. doi: 10.1016/j.jot.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Schepper E.I., Damen J., van Meurs J.B., Ginai A.Z., Popham M., Hofman A. The association between lumbar disc degeneration and low back pain: the influence of age, gender, and individual radiographic features. Spine. 2010;35:531–536. doi: 10.1097/BRS.0b013e3181aa5b33. [DOI] [PubMed] [Google Scholar]
- 12.He L.C., Wang Y.X., Gong J.S., Griffith J.F., Zeng X.J., Kwok A.W. Prevalence and risk factors of lumbar spondylolisthesis in elderly Chinese men and women. Eur Radiol. 2014;24:441–448. doi: 10.1007/s00330-013-3041-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Imada K., Matsui H., Tsuji H. Oophorectomy predisposes to degenerative spondylolisthesis. J Bone Joint Surg Br. 1995;77:126–130. [PubMed] [Google Scholar]
- 14.DeVine J.G., Schenk-Kisser J.M., Skelly A.C. Risk factors for degenerative spondylolisthesis: a systematic review. Evid Based Spine Care J. 2012;3:25–34. doi: 10.1055/s-0031-1298615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kalichman L., Li L., Kim D.H., Guermazi A., Berkin V., O'Donnell C.J. Facet joint osteoarthritis and low back pain in the community–based population. Spine. 2008;33:2560–2565. doi: 10.1097/BRS.0b013e318184ef95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nagi S.Z., Riley L.E., Newby L.G. A social epidemiology of back pain in a general population. J Chronic Dis. 1973;26:769–779. [Google Scholar]
- 17.Reisbord L.S., Greenland S. Factors associated with self-reported back-pain prevalence: a population-based study. J Chronic Dis. 1985;38:691–702. doi: 10.1016/0021-9681(85)90023-2. [DOI] [PubMed] [Google Scholar]
- 18.Calvo-Muñoz I., Gómez-Conesa A., Sánchez-Meca J. Prevalence of low back pain in children and adolescents: a meta-analysis. BMC Pediatr. 2013;13:14. doi: 10.1186/1471-2431-13-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bailey A. Risk factors for low back pain in women: still more questions to be answered. Menopause. 2009;16:3–4. doi: 10.1097/gme.0b013e31818e10a7. [DOI] [PubMed] [Google Scholar]
- 20.Wolfe F., Ross K., Anderson J., Russell I.J. Aspects of fibromyalgia in the general population: sex, pain threshold, and fibromyalgia symptoms. J Rheumatol. 1995;22:151–156. [PubMed] [Google Scholar]
- 21.Rollman G.B., Lautenbacher S. Sex differences in musculoskeletal pain. Clin J Pain. 2001;17:20–24. doi: 10.1097/00002508-200103000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Hestbaek L., Iachine I.A., Leboeuf-Yde C., Kyvik K.O., Manniche C. Heredity of low back pain in a young population: a classical twin study. Twin Res. 2004;7:16–26. doi: 10.1375/13690520460741408. [DOI] [PubMed] [Google Scholar]
- 23.Pinheiro M.B., Ferreira M.L., Refshauge K., Colodro-Conde L., Carrillo E., Hopper J.L. Genetics and the environment affect the relationship between depression and low back pain: a co-twin control study of Spanish twins. Pain. 2015;156:496–503. doi: 10.1097/01.j.pain.0000460330.56256.25. [DOI] [PubMed] [Google Scholar]
- 24.Wáng Y.X., Wáng J.Q., Káplár Z. Increased low back pain prevalence in females than in males after menopause age: evidences based on synthetic literature review. Quant Imaging Med Surg. 2016;6:199–206. doi: 10.21037/qims.2016.04.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bressler H.B., Keyes W.J., Rochon P.A., Badley E. The prevalence of low back pain in the elderly. A systematic review of the literature. Spine. 1999;24:1813–1819. doi: 10.1097/00007632-199909010-00011. [DOI] [PubMed] [Google Scholar]
- 26.Mailis-Gagnon A., Nicholson K., Yegneswaran B., Zurowski M. Pain characteristics of adults 65 years of age and older referred to a tertiary care pain clinic. Pain Res Manag. 2008;13:389–394. doi: 10.1155/2008/541963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lawrence J.S. Disc degeneration. Its frequency and relationship to symptoms. Ann Rheum Dis. 1969;28:121–138. doi: 10.1136/ard.28.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Papageorgiou A.C., Croft P.R., Ferry S., Jayson M.I., Silman A.J. Estimating the prevalence of low back pain in the general population. Evidence from the South Manchester Back Pain Survey. Spine. 1995;20:1889–1894. doi: 10.1097/00007632-199509000-00009. [DOI] [PubMed] [Google Scholar]
- 29.Cho N.H., Jung Y.O., Lim S.H., Chung C.K., Kim H.A. The prevalence and risk factors of low back pain in rural community residents of Korea. Spine. 2012;37:2001–2010. doi: 10.1097/BRS.0b013e31825d1fa8. [DOI] [PubMed] [Google Scholar]
- 30.Nevitt M.C., Ettinger B., Black D.M., Stone K., Jamal S.A., Ensrud K. The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med. 1998;128:793–800. doi: 10.7326/0003-4819-128-10-199805150-00001. [DOI] [PubMed] [Google Scholar]
- 31.Santen R.J., Allred D.C., Ardoin S.P., Archer D.F., Boyd N., Braunstein G.D. Postmenopausal hormone therapy: an Endocrine Society scientific statement. J Clin Endocrinol Metab. 2010;95(7 Suppl 1):s1–66. doi: 10.1210/jc.2009-2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wluka A.E., Davis S.R., Bailey M., Stuckey S.L., Cicuttini F.M. Users of oestrogen replacement therapy have more knee cartilage than non-users. Ann Rheum Dis. 2001;60:332–336. doi: 10.1136/ard.60.4.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ham K.D., Loeser R.F., Lindgren B.R., Carlson C.S. Effects of long-term estrogen replacement therapy on osteoarthritis severity in cynomolgus monkeys. Arthritis Rheum. 2002;46:1956–1964. doi: 10.1002/art.10406. [DOI] [PubMed] [Google Scholar]
- 34.Cirillo D.J., Wallace R.B., Wu L., Yood R.A. Effect of hormone therapy on risk of hip and knee joint replacement in the Women's Health Initiative. Arthritis Rheum. 2006;54:3194–3204. doi: 10.1002/art.22138. [DOI] [PubMed] [Google Scholar]
- 35.Chlebowski R.T., Cirillo D.J., Eaton C.B., Stefanick M.L., Pettinger M., Carbone L.D. Estrogen alone and joint symptoms in the Women's Health Initiative randomized trial. Menopause. 2013;20:600–608. doi: 10.1097/GME.0b013e31828392c4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baron Y.M., Brincat M.P., Galea R., Calleja N. Intervertebral disc height in treated and untreated overweight post-menopausal women. Hum Reprod. 2005;20:3566–3570. doi: 10.1093/humrep/dei251. [DOI] [PubMed] [Google Scholar]
- 37.Kyllönen E.S., Heikkinen J.E., Väänänen H.K., Kurttila-Matero E., Wilen-Rosenqvist G., Lankinen K.S. Influence of estrogen-progestin replacement therapy and exercise on lumbar spine mobility and low back symptoms in a healthy early postmenopausal female population: a 2-year randomized controlled trial. Eur Spine J. 1998;7:381–386. doi: 10.1007/s005860050094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li X., Phillips F.M., An H.S., Ellman M., Thonar E.J., Wu W. The action of resveratrol, a phytoestrogen found in grapes, on the intervertebral disc. Spine. 2008;33:2586–2595. doi: 10.1097/BRS.0b013e3181883883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Musgrave D.S., Vogt M.T., Nevitt M.C., Cauley J.A. Back problems among postmenopausal women taking estrogen replacement therapy: the study of osteoporotic fractures. Spine. 2001;26:1606–1612. doi: 10.1097/00007632-200107150-00023. [DOI] [PubMed] [Google Scholar]
- 40.Symmons D.P.L., van Hemert A.M., Vandenbroucke J.P., Valkenburg H.A. A longitudinal study of back pain and radiological changes in the lumbar spines of middle aged women: I. Clinical findings. Ann Rheum Dis. 1991;50:158–161. doi: 10.1136/ard.50.3.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ghazal S., Pal L. Perspective on hormone therapy 10 years after the WHI. Maturitas. 2013;76:208–212. doi: 10.1016/j.maturitas.2013.08.014. [DOI] [PubMed] [Google Scholar]
- 42.Lobo R.A., Davis S.R., De Villiers T.J., Gompel A., Henderson V.W., Hodis H.N. Prevention of diseases after menopause. Climacteric. 2014;17:540–556. doi: 10.3109/13697137.2014.933411. [DOI] [PubMed] [Google Scholar]
- 43.Hsia J., Langer D., Manson J.E., Kuller L., Johnson K.C., Hendrix S.L. Conjugated equine estrogens and the risk of coronary heart disease. Arch Intern Med. 2006;166:357–365. doi: 10.1001/archinte.166.3.357. [DOI] [PubMed] [Google Scholar]
- 44.Rossouw J.E., Prentice R.L., Manson J.E., Wu L., Barad D., Barnabei V.M. Postmenopausal hormone therapy and risk of cardiovascular disease by age and years since menopause. JAMA. 2007;297:1465–1477. doi: 10.1001/jama.297.13.1465. [DOI] [PubMed] [Google Scholar]
- 45.Scarabin P.Y., Oger E., Plu-Bureau G. Differential association of oral and transdermal oestrogen-replacement therapy with venous thromboembolism risk. Lancet. 2003;362:428–432. doi: 10.1016/S0140-6736(03)14066-4. [DOI] [PubMed] [Google Scholar]
- 46.Bae J.M., Kim E.H. Hormone replacement therapy and risk of breast cancer in Korean women: a quantitative systematic review. J Prev Med Public Health. 2015;48:225–230. doi: 10.3961/jpmph.15.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Herrington D.M., Klein K.P. Invited review: pharmacogenetics of estrogen replacement therapy. J Appl Physiol (1985) 2001;91:2776–2784. doi: 10.1152/jappl.2001.91.6.2776. [DOI] [PubMed] [Google Scholar]
- 48.Mirkin S., Pickar J.H. Selective estrogen receptor modulators (SERMs): a review of clinical data. Maturitas. 2015;80:52–57. doi: 10.1016/j.maturitas.2014.10.010. [DOI] [PubMed] [Google Scholar]