Abstract
Background
Propofol is recommended for sedation in gastrointestinal endoscopy (GE), but preliminary data suggest addictive potentials.
Objective
The objective of this article is to evaluate the frequency of predominantly euphoric reaction after GE and patients’ subsequent reminiscences.
Methods
Eighty-two patients undergoing elective GE under propofol sedation were enrolled in a prospective observational study. The grade of anxiety, expectation or relief about the examination’s result and affective state in terms of cheerfulness, relaxation, activation, sedation and anxiety were surveyed using a numeric rating scale (1 to 10) immediately before (t1), after GE (t2) and seven days (t3) later. Statistics: hierarchical cluster analysis, heat map, χ2 test and paired t test.
Results
Mean propofol dosage was 264 ± 120 mg. Two clusters of mood changes emerged (t1 vs. t2). One (n = 46, 56.1%) was characterized by an unease reaction pattern with equal values regarding cheerfulness, relaxation and anxiety, while relaxation decreased; the other cluster showed a euphoric reaction pattern (n = 36, 43.9%) with markedly increased cheerfulness, relaxation and decreased anxiety. These effects intensified at recall (t3). Despite similar endoscopy results, euphoric cluster patients rated these more positively.
Conclusion
Propofol induces euphoria in nearly half of the patients undergoing elective GE with persisting, even enhanced reminiscence (germanctr.de, trial number DRKS00011202).
Keywords: Gastrointestinal endoscopy, propofol sedation, psychotropic effects, addiction
Key summary
Summarize the established knowledge on this subject.
Propofol is recommended for sedation in gastrointestinal endoscopy.
Propofol has shown euphoric reaction patterns and addictive potentials in healthy volunteers.
What are the significant and/or new findings of this study?
Propofol induces euphoria in nearly half of the patients undergoing gastrointestinal endoscopy.
The memory of euphoria persists and even enhances over time.
Introduction
Propofol is used worldwide for sedation in patients undergoing gastrointestinal endoscopy.1 Severe respiratory and cardiovascular side effects are rare; therefore, propofol is the drug of first choice for sedation supervised by non-anesthesiologists or trained nurses.2–4 Since propofol stimulates the dopamine expression in the central reward system, however, it bears a potential risk of addiction and induces addiction-like behavior in animal models.5–7 Additionally, a subgroup of healthy volunteers reported having experienced euphoric moods after propofol administration.8 The relative addictive risk of propofol is thought to be moderate,6,9 but there is an increasing number of reports of propofol addiction in physicians and nurses during the last two decades associated with high mortality.10–13
The situation is amended by reports of patients and medical laymen who developed propofol addiction and feigned an indication for endoscopy to receive propofol.14,15 Surviving physicians after propofol abuse also reported that the abiding memory of the intense relaxation after narcosis many years ago was a major reason to abuse propofol years thereafter.15,16 However, it is hitherto unknown how many patients develop a euphoric drug reaction after endoscopy. Experiences with other drugs lead to the assumption that the frequency and the amount of euphoriant side effects explain the risk of later propofol abuse. This could be enhanced in patients with a prior high level of anxiety regarding the possible result of endoscopy, which may be attenuated by the specific drug.17,18 Consequently, we hypothesized that some patients undergoing endoscopy under propofol sedation experience a euphoric reaction pattern that superposes negative feelings and that this specific reminiscence will survive.
Materials and methods
Study population
Patients of at least 18 years of age undergoing elective gastrointestinal endoscopy under propofol sedation (i.e. esophagogastroduodenoscopy, ileocolonoscopy or both) were enrolled in two centers in a prospective observational study. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki, and has been approved by the ethical review board of the Ruhr-University Bochum (November 15, 2013, registry number 4817-2013) and registered in the German Clinical Trial Registry (DRKS00011202), Written, informed consent was obtained from each patient.
Objectives
The aim of the present study was (1) to evaluate the frequency of a predominantly euphoric reaction pattern immediately after the intervention, (2) to characterize the reminiscence one week later and (3) to investigate the superposition of negative feelings. Secondary objectives were to analyze the influence of pre-intervention psychological parameters, such as anxiety, pain, previous experience with propofol, anxiety disorders, addictive behavior like smoking and alcohol consumption, or specific personality traits.
Schedule
All patients completed a questionnaire at least 24 hours prior to endoscopy in which biographic data relevant to addiction (e.g. use of psychotropic or sedative drugs, prior psychotherapy or psychiatric treatment, comorbidities and previous experience with propofol, depression and anxiety disorders) were collected. Directly before endoscopy (t1), all participants completed a multidimensional questionnaire to survey the current level of anxiety, the expectation about the result of the forthcoming endoscopic examination and the mood. The questionnaire was repeated two hours after endoscopy (t2), and seven days later (t3, evaluation by telephone call).
Questionnaires
Patients’ psychopathological risk factors
The Patient Health Questionnaire (PHQ-D) was used to identify depression and anxiety.19 The Alcohol Use Disorders Identification Test,20 the Fagerstrom Test21 and further queries were used to evaluate the consumption of alcohol, nicotine and psychotropic drugs as well as previous anesthesia and its positive and negative effects, respectively.
Affective state before endoscopy
Directly before endoscopy (t1), several adjectives selected from well-established dimension-analytical procedures22 and the Biphasic Alcohol Effects Scale23 were requested to identify cheerfulness, relaxation, activation, sedation and anxiety (see Table S-1, supplementary material). Every item was represented by five adjectives, which had to be estimated on a 10-point scale. Additionally, the dimensions buoyant, gleeful, happy, cheerful, optimistic, relaxed, in a chilled manner and overexcited were summarized as a euphoric reaction, while concerned, worried, anxious and nervous represented a reaction of unease. A further six queries (Cognitive-Autonomic-Somatic Anxiety Symptoms (KASA)) were used to record the level of anxiety on a four-stage Likert scale.24
Affective state after endoscopy
The same pre-endoscopic queries were used immediately and seven days after endoscopy (t2, t3). The grade of relief after anesthesia was measured complementarily to the evaluation of anxiety before anesthesia.
Personality traits
Personality traits were gathered by means of a validated short version of a Big Five Questionnaire.25 The central idea claims that differences in personality between individuals who express differing behavior and experience can be ascribed to openness to experiences, conscientiousness, extraversion, agreeableness and neuroticism. Individuals judged themselves on a 10-point visual analog scale. Any scoring between 4 and 6 points were rated as being average, 3 points or less as below and 7 points or more as above average.
Endoscopy and sedation
All endoscopies were performed by experienced gastroenterologists. Propofol sedation was non-anesthesiologist administered, following national and international guidelines.2,3,26
Statistical analysis
Statistical analysis was performed with R 3.3.2 with packages stats and RColorBrewer (https://cran.r-project.org/). Descriptive methods were used to rule out basic characteristics, overall endoscopy and sedation parameters, behavior of mood, feelings and personality traits. Metric variables were described by arithmetic mean and standard deviation; relative frequency is presented for categorical data.
A hierarchical cluster analysis with maximum linkage and Euclidian distance was performed with a focus on the euphoric reaction pattern. General sociodemographic variables, previous anesthesia and sedation experiences, psychopathological features and anamnestic characteristics of addiction as covariates were analyzed between the resulting clusters. A t test was used for the statistical comparison of metric variables. Group comparisons of categorical data were conducted using χ2 tests. A two-tailed p value of <0.05 was considered statistically significant.
Results
Eighty-two patients were included (38 female patients (46%), mean age 56.4 ± 16.0 years. Fifty-nine patients (72%) underwent esophagogastroduodenoscopy, 20 (24%) colonoscopy and three (4%) both at the same session; 35 examinations (43%) were performed on inpatients (see Table 1). Sedation parameters are detailed in Table 1. At least one comorbidity was present in 69% of patients (see Table S-2, supplementary material). Most patients were characterized by American Society of Anesthesiologists (ASA) scores 1 and 2 (42% and 40%, respectively).
Table 1.
Endoscopy and sedation parameters.
| CURP | CERP | Total | p | |
|---|---|---|---|---|
| (n = 46) | (n = 36) | (n = 82) | aχ2 test bt test | |
| Intervention data | ||||
| Kind of endoscopy, n (%) | 0.399a | |||
| Gastroscopy | 36 (77) | 26 (68) | 62 (73) | |
| Colonoscopy | 11 (23) | 12 (32) | 23 (27) | |
| Indication for endoscopy, n (%) | 40 | 29 | 69 | 0.889a |
| Prevention/follow-up tumor | 5 (13) | 6 (21) | 11 (16) | |
| Gastrointestinal hemorrhage | 7 (18) | 6 (21) | 13 (19) | |
| Suspected/known chronic inflammatory bowel disease | 4 (10) | 2 (7) | 6 (9) | |
| Unspecific abdominal discomfort | 17 (43) | 11 (38) | 28 (41) | |
| Unspecific thoracic discomfort | 5 (13) | 2 (7) | 7 (10) | |
| Other | 2 (5) | 2 (7) | 4 (6) | |
| Final diagnosis (proven by endoscopy), n (%) | 46 | 36 | 82 | 0.821a |
| Normal finding/non-relevant benign alterations | 9 (20) | 7 (19) | 16 (20) | |
| Other functional disease (irritable colon and stomach) | 3 (7) | 2 (6) | 5 (6) | |
| Inflammatory disease (Crohn’s disease, infectious colitis, diverticulitis) | 29 (63) | 21 (58) | 50 (61) | |
| Benign neoplasia/angiodysplasia | 5 (11) | 5 (14) | 10 (12) | |
| Malign neoplasia | – | 1 (3) | 1 (1) | |
| Sedation | ||||
| Propofol dosage, mean ± SD (mg) | 256 ± 136 | 275 ± 98 | 264 ± 120 | 0.483b |
| Duration of sedation, mean ± SD (min) | 28 ± 20 | 29 ± 15 | 28 ± 18 | 0.69b |
| Dosage per minute, mean ± SD (mg/min) | 12.01 ± 6.43 | 11.56 ± 5.41 | 11.81 ± 5.97 | 0.737b |
| First dose, mean ± SD (mg) | 51 ± 13 | 49 ± 11 | 50 ± 12 | 0.602b |
| Dosage of the first bolus, mean ± SD (mg) | 32 ± 13 | 33 ± 9 | 32 ± 11 | 0.966b |
| Number of all boluses (including starting dose), mean ± SD | 8 ± 5 | 9 ± 4 | 9 ± 4 | 0.405b |
| Dosage per kg, n | 43 | 36 | 79 | |
| Dosage per kg, mean ± SD (mg/kg) | 3.4 ± 1.8 | 3.5 ± 1.6 | 3.5 ± 1.7 | 0.748b |
| Dosage per kg per minute, mean ± SD (mg/kg/min) | 0.1585 ± 0.0824 | 0.1452 ± 0.0782 | 0.1524 ± 0.0803 | 0.465b |
CURP: cluster of uneasy reaction pattern; CERP: cluster of euphoric reaction pattern. Endoscopy and sedation parameters did not differ between study groups.
Psychopathological screening
Smoking habits, alcohol consumption and medication are displayed in Table S-2, supplementary material. The PHQ-D revealed depression to be present in 43% and panic disorder in 3% (see Tables S-3 and S-4, supplementary material). Overall, 72% underwent previous short sedation within the last five years, most of them including propofol; the emotional perception is detailed in Table S-4, supplementary material.
Conscientiousness was present on average in 74%, below average in 20% and above average in 7% of patients (see Table 2). Extraversion occurred on average in 70%, below average in 16% and above average in 14%, and agreeableness in 61%, 22% and 17%, respectively. Patients showed openness to experience on an average scale in 77%, below average in 17% and above average in 16%, and to neuroticism in 72%, 13%, and 11%, respectively.
Table 2.
Personality traits of study population.
| CURP | CERP | Total | p | |
|---|---|---|---|---|
| (n = 46) | (n = 36) | (n = 82) | aχ2 test | |
| Big Five Questionnaire | ||||
| Pronounced personality dimensions, n (%) | 43 | 33 | 76 | |
| Conscientiousness | 36 (84) | 28 (85) | 64 (84) | 0.894a |
| Extraversion | 20 (47) | 16 (48) | 36 (47) | 0.864a |
| Agreeableness | 37 (86) | 23 (70) | 60 (79) | 0.083a |
| Openness to experience | 21 (49) | 15 (45) | 36 (47) | 0.77a |
| Neuroticism | 11 (26) | 11 (33) | 22 (29) | 0.46a |
| Conscientiousness, n (%) | ||||
| Below average | 8 (19) | 7 (21) | 15 (20) | 0.025a |
| On average | 35 (81) | 21 (64) | 56 (74) | |
| Above average | – | 5 (15) | 5 (7) | |
| Extraversion, n (%) | ||||
| Below average | 6 (14) | 6 (18) | 12 (16) | 0.857a |
| On average | 31 (72) | 22 (67) | 53 (70) | |
| Above average | 6 (14) | 5 (15) | 11 (14) | |
| Agreeableness, n (%) | ||||
| Below average | 10 (23) | 7 (21) | 17 (22) | 0.537a |
| On average | 24 (56) | 22 (67) | 46 (61) | |
| Above average | 9 (21) | 4 (12) | 13 (17) | |
| Openness to experience, n (%) | ||||
| Below average | 7 (16) | 6 (18) | 13 (17) | 0.837a |
| On average | 30 (70) | 21 (64) | 51 (67) | |
| Above average | 6 (14) | 6 (18) | 12 (16) | |
| Neuroticism, n (%) | ||||
| Below average | 7 (16) | 3 (9) | 10 (13) | 0.656a |
| On average | 30 (70) | 25 (76) | 55 (72) | |
| Above average | 6 (14) | 5 (15) | 11 (14) | |
| PHQ-D | ||||
| Depression, n (%) | 42 | 32 | 74 | |
| Severe depression | 2 (5) | – | – | 0.349a |
| Moderate depression | 4 (10) | 6 (19) | 10 (14) | |
| Mild depression | 13 (31) | 7 (22) | 20 (27) | |
| No depression | 23 (55) | 19 (59) | 42 (57) | |
| Panic disorder, n (%) | 43 | 34 | 77 | |
| – | 2 (6) | 2 (3) | 0.107a |
Personality traits have been assessed by means of a standardized Big Five Questionnaire. There were slight, but significant differences concerning conscientiousness with more patients above average in CERP. By contrast, there was a tendency of CURP patients to show higher levels of agreeableness. The distribution of depression and panic disorders did not differ.
CURP: cluster of uneasy reaction pattern; CERP: cluster of euphoric reaction pattern; PHQ-D: Patient Health Questionnaire.
Characteristics of mood and clustering of patients
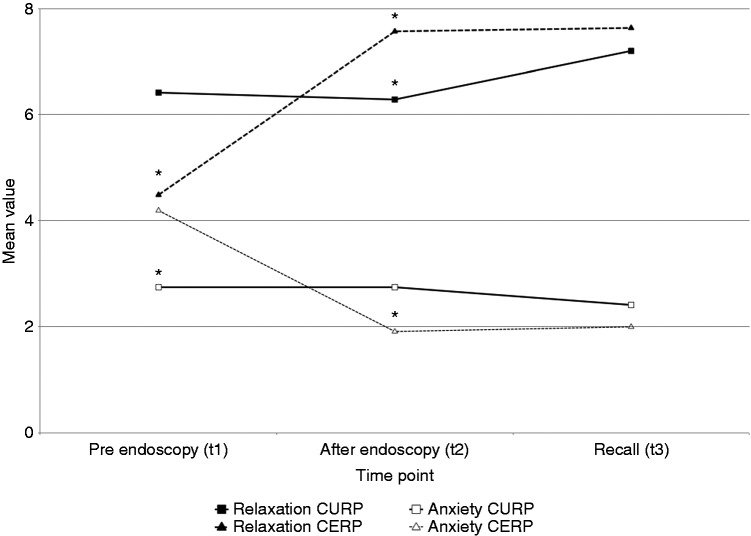
A total of 54% of patients were worried and 45% felt depressed and anxious before endoscopy. The distribution did not change immediately after endoscopy (p = 0.815, χ2 test), but the level of confidence rose from 6.6 ± 2.4 to 8.2 ± 2.2 (p < 0.001 each, t test) and returned to base level one week later. On the other hand, the index of euphoria increased steadily from 4.6 ± 2.0 before (t1) to 5.8 ± 1.9 immediately after (t2) to 6.2 ± 2.0 a week after (t3) endoscopy (p < 0.001 each, t test). Coincidently, the index of unease decreased from 3.3 ± 2.1 to 2.4 ± 1.8 and 2.2 ± 1.7, respectively (p < 0.01 each, t test, see Table S-6 in the supplementary material and Figure 1).
Figure 1.
Overall development of euphoria and discomfort.
The index of euphoria (highlighted in dark gray in the left columns) is calculated as mean value from the adjectives buoyant, gleeful, happy, cheerful, optimistic, relaxed, in a chilled manner and overexcited, while discomfort (highlighted in light gray in the right columns) contained the adjectives concerned, worried, anxious and nervous (*p < 0.05).
All different aspects of moods and feelings changed after endoscopy. The indices of cheerfulness changed from 4.7 ± 2.2 to 5.9 ± 2.1, of relaxation from 5.6 ± 2.2 to 6.9 ± 2.1, of activation from 4.6 ± 1.9 to 5.0 ± 1.9, of sedation from 2.6 ± 1.4 to 3.4 ± 1.8 and of anxiety from 3.4 ± 2.1 to 2.4 ± 1.8 (see Table 3).
Table 3.
Cluster-associated development of feelings.
| CURP (n = 46) |
CERP (n = 36) |
CURP t1 vs. CERP t1 | CURP t2 vs. CERP t2 | CURP t3 vs. CERP t3 | CURP t1 vs CURP t2 | CURP t2 vs. CURP t3 | CURP t1 vs. CURP t3 | CERP t1 vs. CERP t2 | CERP t2 vs. CERP t3 | CERP t1 vs. CERP t3 | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time point | |||||||||||||||
| t1 | t1 | t3 | t1 | t2 | t3 | p | |||||||||
| Cheerfulness | 5.5 ± 2.4 | 5.4 ± 2.2 | 5.5 ± 2.3 | 3.8 ± 1.6 | 6.5 ± 1.9 | 7.1 ± 1.6 | 0.001a | 0.028a | 0.003a | 0.924 | 0.929 | 0.999 | 0a | 0.177 | 0a |
| Buoyant | 5.0 ± 2.8 | 4.7 ± 2.9 | 4.5 ± 2.9 | 3.4 ± 2.3 | 6.0 ± 2.8 | 6.7 ± 2.3 | 0.006a | 0.039a | 0.002a | 0.666 | 0.256 | 0.431 | 0.004a | 0.036a | 0a |
| Gleeful | 4.7 ± 3.2 | 4.6 ± 2.8 | 4.4 ± 2.6 | 2.9 ± 2.2 | 5.4 ± 2.9 | 7.0 ± 2.0 | 0.004a | 0.202 | 0a | 0.694 | 0.396 | 0.674 | 0.001a | 0.002a | 0a |
| Happy | 5.0 ± 3.0 | 5.2 ± 2.6 | 5.0 ± 2.9 | 2.7 ± 2.1 | 6.1 ± 2.8 | 6.9 ± 2.2 | 0a | 0.115 | 0.007a | 0.324 | 0.375 | 0.975 | 0a | 0.047a | 0a |
| Cheerful | 5.9 ± 2.9 | 6.0 ± 3.0 | 6.2 ± 2.6 | 3.8 ± 2.2 | 7.4 ± 2.2 | 7.5 ± 2.3 | 0a | 0.023a | 0.056 | 0.266 | 0.542 | 0.66 | 0a | 0.183 | 0a |
| Optimistic | 6.7 ± 2.9 | 6.7 ± 2.7 | 7.2 ± 2.5 | 6.3 ± 2.4 | 7.4 ± 2.7 | 7.3 ± 1.8 | 0.479 | 0.246 | 0.856 | 0.628 | 0.715 | 0.428 | .241 | 0.584 | 0.062 |
| Relaxation | 6.4 ± 2.2 | 6.3 ± 2.2 | 7.2 ± 2.1 | 4.5 ± 1.5 | 7.6 ± 1.5 | 7.6 ± 1.5 | 0a | 0.004a | 0.362 | 0.78 | 0.072 | 0.12 | 0a | 0.867 | 0a |
| Easygoing | 6.2 ± 3.1 | 6.3 ± 3.0 | 6.8 ± 2.6 | 5.3 ± 2.2 | 7.3 ± 2.6 | 7.6 ± 2.0 | 0.119 | 0.101 | 0.209 | 0.424 | 0.845 | 0.354 | 0.017a | 0.166 | 0a |
| Relaxed | 6.4 ± 3.0 | 6.4 ± 3.1 | 7.3 ± 2.3 | 4.1 ± 2.0 | 7.9 ± 2.2 | 7.9 ± 2.2 | 0a | 0.015a | 0.247 | 0.294 | 0.712 | 0.176 | 0a | 0.163 | 0a |
| Well-balanced | 6.2 ± 2.8 | 5.6 ± 2.9 | 7.1 ± 2.3 | 4.5 ± 1.9 | 7.1 ± 2.1 | 7.5 ± 1.8 | 0.002a | 0.012a | 0.446 | 0.943 | 0.152 | 0.145 | 0.002a | 0.037a | 0a |
| In a chilled manner | 6.0 ± 2.9 | 6.1 ± 2.8 | 7.0 ± 2.8 | 3.7 ± 2.0 | 7.7 ± 1.9 | 7.9 ± 1.9 | 0a | 0.005a | 0.168 | 0.136 | 0.805 | 0.133 | 0a | 0.076 | 0a |
| Calm | 7.3 ± 2.5 | 7.0 ± 2.7 | 7.8 ± 2.1 | 4.9 ± 2.6 | 7.9 ± 2.1 | 7.2 ± 2.1 | 0a | 0.142 | 0.288 | 0.817 | 0.449 | 0.324 | 0a | 0.773 | 0a |
| Activation | 4.8 ± 2.1 | 4.5 ± 1.8 | 5.0 ± 2.1 | 4.2 ± 1.6 | 5.7 ± 1.8 | 6.2 ± 1.6 | 0.128 | 0.005a | 0.02a | 0.377 | 0.227 | 0.716 | 0.001a | 0.255 | 0a |
| High-spirited | 5.8 ± 2.8 | 5.2 ± 2.8 | 6.1 ± 3.1 | 5.1 ± 2.4 | 6.4 ± 2.6 | 7.0 ± 2.2 | 0.274 | 0.051 | 0.167 | 0.913 | 0.607 | 0.676 | 0.346 | 0.042a | 0.002a |
| Active | 5.0 ± 2.9 | 4.2 ± 2.5 | 5.3 ± 2.9 | 3.7 ± 2.3 | 5.4 ± 2.9 | 6.1 ± 2.4 | 0.029a | 0.037a | 0.218 | 0.655 | 0.398 | 0.667 | 0.085 | 0.035a | 0a |
| Powerful | 5.0 ± 3.0 | 4.3 ± 2.4 | 5.0 ± 2.5 | 4.0 ± 2.4 | 5.6 ± 2.8 | 6.6 ± 1.9 | 0.13 | 0.034a | 0.008a | 0.835 | 0.769 | 0.936 | 0.174 | 0.004a | 0a |
| Overexcited | 2.8 ± 2.2 | 2.9 ± 2.3 | 3.1 ± 2.5 | 3.3 ± 2.5 | 3.9 ± 3.1 | 4.4 ± 3.2 | 0.387 | 0.113 | 0.104 | 0.346 | 0.755 | 0.581 | 0.95 | 0.168 | 0.136 |
| Talkative | 5.6 ± 2.8 | 5.8 ± 2.8 | 5.6 ± 3.0 | 4.8 ± 2.8 | 7.1 ± 2.3 | 6.6 ± 2.5 | 0.178 | 0.03a | 0.151 | 0.19 | 0.225 | 0.956 | 0.015a | 0.685 | 0.008a |
| Sedation | 2.7 ± 1.3 | 3.7 ± 1.7 | 3.1 ± 1.7 | 2.5 ± 1.5 | 3.0 ± 1.8 | 3.1 ± 1.7 | 0.557 | 0.108 | 0.921 | 0.003a | 0.191 | 0.183 | 0.197 | 0.862 | 0.144 |
| Muddled | 1.8 ± 1.6 | 3.5 ± 2.8 | 2.6 ± 2.3 | 1.6 ± 1.2 | 3.1 ± 2.6 | 2.9 ± 2.3 | 0.612 | 0.421 | 0.62 | 0.001a | 0.192 | 0.072 | 0.001a | 0.464 | 0.007a |
| Woozy | 1.8 ± 1.8 | 3.3 ± 2.4 | 2.7 ± 2.2 | 2.1 ± 2.2 | 2.6 ± 2.2 | 3.1 ± 2.1 | 0.571 | 0.198 | 0.458 | 0.012a | 0.604 | 0.069 | 0.11 | 0.801 | 0.067 |
| Limp | 4.6 ± 3.1 | 4.9 ± 2.9 | 3.6 ± 2.4 | 3.4 ± 2.5 | 3.2 ± 2.1 | 2.7 ± 1.8 | 0.075 | 0.004a | 0.09 | 0.532 | 0.35 | 0.154 | 0.216 | 0.014a | 0.191 |
| Inattentive | 2.6 ± 2.1 | 3.1 ± 2.3 | 3.4 ± 2.4 | 3.0 ± 2.8 | 2.6 ± 2.5 | 3.1 ± 2.3 | 0.425 | 0.349 | 0.666 | 0.514 | 0.346 | 0.107 | 0.839 | 0.672 | 0.844 |
| Slowed down | 2.7 ± 2.2 | 3.5 ± 2.5 | 3.4 ± 2.4 | 2.4 ± 2.1 | 3.6 ± 3.3 | 3.7 ± 2.5 | 0.551 | 0.775 | 0.665 | 0.107 | 0.872 | 0.148 | 0.054 | 0.796 | 0.025a |
| Anxiety | 2.7 ± 2.0 | 2.7 ± 2.0 | 2.4 ± 2.1 | 4.2 ± 2.0 | 1.9 ± 1.3 | 2.0 ± 1.1 | 0.002a | 0.033a | 0.356 | 1 | 0.481 | 0.482 | 0a | 0.771 | 0a |
| Worried | 2.7 ± 2.6 | 3.2 ± 2.8 | 2.3 ± 2.1 | 3.8 ± 2.4 | 1.9 ± 2.3 | 1.6 ± 1.1 | 0.075 | 0.031a | 0.117 | 0.849 | 0.609 | 0.477 | 0.068 | 0.069 | 0a |
| Concerned | 3.1 ± 2.6 | 3.3 ± 2.8 | 2.7 ± 2.6 | 4.2 ± 2.6 | 2.0 ± 1.9 | 2.1 ± 1.8 | 0.067 | 0.027a | 0.33 | 0.439 | 0.999 | 0.489 | 0.017a | 0.31 | 0.001a |
| Anxious | 2.6 ± 2.3 | 2.5 ± 2.2 | 2.2 ± 2.1 | 3.4 ± 2.3 | 1.7 ± 2.1 | 1.4 ± 0.7 | 0.119 | 0.083 | 0.087 | 0.308 | 0.977 | 0.335 | 0.019a | 0.091 | 0a |
| Excited | 2.7 ± 2.2 | 2.5 ± 2.2 | 2.4 ± 2.0 | 5.2 ± 2.4 | 2.0 ± 1.8 | 2.5 ± 2.0 | 0a | 0.269 | 0.809 | 0.367 | 0.794 | 0.572 | 0a | 0.626 | 0a |
| Nervous | 2.6 ± 2.2 | 2.3 ± 1.8 | 2.5 ± 2.4 | 4.4 ± 2.6 | 1.9 ± 2.1 | 2.3 ± 1.8 | 0.001a | 0.462 | 0.739 | 0.312 | 0.48 | 0.856 | 0a | 0.727 | 0.001a |
In CERP patients, cheerfulness, relaxation and activation increase and anxiety decreases significantly, while sedation remains unchanged. On the other hand, in CURP patients, sedation increases significantly, while the other dimensions remain broadly unchanged.
CURP: cluster of uneasy reaction pattern; CERP: cluster of euphoric reaction pattern; t1: time immediately before gastrointestinal endoscopy; t2: time immediately after gastrointestinal endoscopy; t3: time seven days after gastrointestinal endoscopy. a: t test
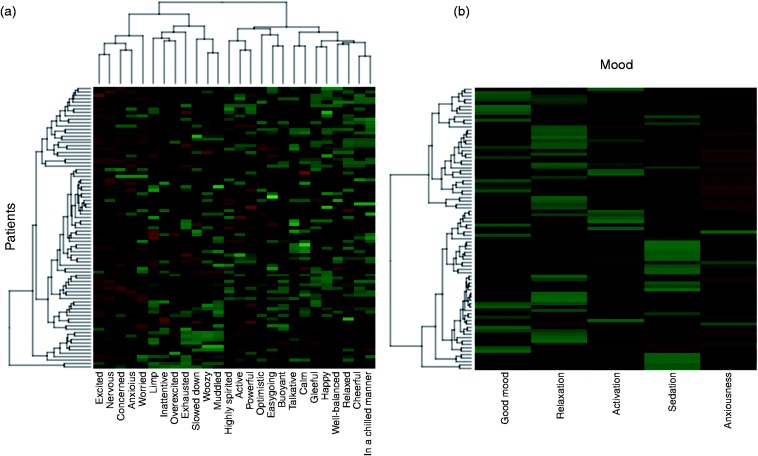
Two different behavioral clusters can be distinguished by means of a latent factorial analysis (see Figure 2). Cluster 1 is characterized by less activation, partially worse mood and less relaxation with increased sedation and is, therefore, called the cluster of uneasy reaction pattern (CURP, 46 patients, 56.1%). Thirty-six patients (43.9%) belong to cluster 2, which is characterized by improved mood and deeper relaxation with less sedation and anxiety and is, therefore, called the cluster of euphoric reaction pattern (CERP).
Figure 2.
Cluster analysis.
The mood changes after propofol sedation are displayed as scoring in a heat map. Patients are plotted in rows, and the difference of the specific psychotropic rating in columns. Green indicates higher rating at t2, red a lower rating at t2 and black an equal rating (up to ±1 point) at t2. This overall heat map (a) does not clearly indicate the patients’ clustering (lines): two outpatients (lowest lines) show strong, a small cluster (second from below), modest deterioration, a large cluster (middle area) reacts with rising mood, a medium cluster with apparent improvement of temper. Instead, the questions’ clustering (columns) obviously presents two different blocks of positive and negative adjectives; default categories can largely be reproduced. The heat map, therefore, proposes two clusters (b): CURP is characterized by improved mood and deeper relaxation with less sedation and anxiety; CERP is characterized by less activation, partially worse mood and less relaxation with increased sedation.
t2: time after gastrointestinal endoscopy; CURP: cluster of uneasy reaction pattern; CERP: cluster of euphoric reaction pattern.
Basic characteristics, such as center recruitment, gender, kind of endoscopy, overall comorbidities, ASA scoring, indication for endoscopy and its findings (see Table S-2, supplementary material) and all sedation parameters were equally distributed between the clusters (see Table 1).
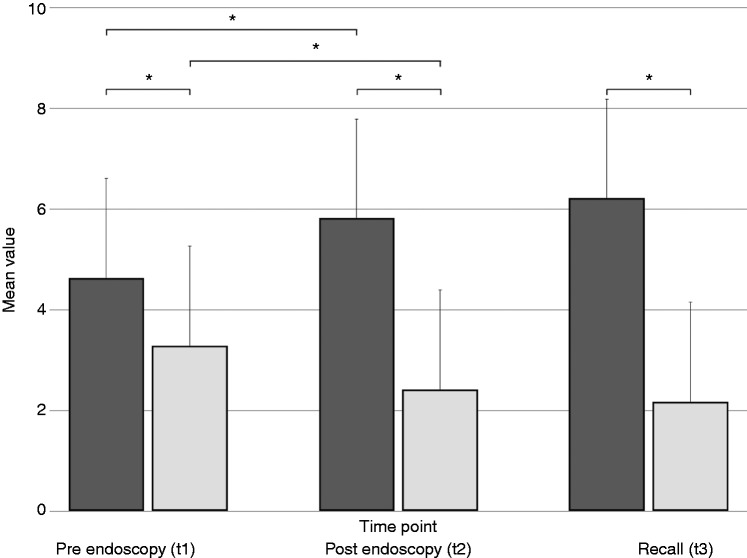
Marked differences occurred in relation to short-term changes (t1 to t2) of mood and feelings. The CURP patients showed equal values regarding cheerfulness, relaxation and anxiety, while relaxation decreased and sedation increased slightly due to endoscopy under propofol sedation (see Table 3 and Figure 3). On the other hand, CERP patients were characterized by markedly increased cheerfulness, relaxation and somewhat less activation, while, simultaneously, the degree of anxiety decreased substantially. The degree of relaxation in CURP patients one week later was rated even higher and the level of sedation slightly lower. The CERP patients rated the degree of cheerfulness and activation even higher than directly after endoscopy, while the level of relaxation, sedation and anxiety was appraised nearly the same.
Figure 3.
Development of the emotional dimensions of the moods anxiety and relaxation.
Mean values determined by visual analog scales are displayed for two of the five dimensions of mood (*p < 0.05).
Most CURP patients were worried before endoscopy (70% vs. 30%) with a slight but statistical difference during recall (75% vs. 25%, p = 0.048, χ2 test); however, most CERP patients rated themselves as not worried before endoscopy (66% vs. 34%; p = 0.002, χ2 test) and during recall (68% vs. 32%; p > 0.05, χ2 test). At the same time, most CURP patients felt more confident/cheerful (71%), while most CERP patients felt depressed/anxious (66%, p = 0.001, χ2 test). Again, this perception changed slightly during recall in CURP, but not in CERP patients (see Table S-7, supplementary material). Both clusters converged after endoscopy, resulting in smaller, nonsignificant differences; at t2, fewer CURP patients rated themselves as more confident/cheerful (48 %; p = 0.116 related to t1) and fewer CERP patients as more depressed/anxious (33%, p = 0.054 related to t1; p > 0.05, χ2 test related to CURP patients). This rating did not change during recall.
Although the findings of endoscopy did not differ significantly (p = 0.821, χ2 test, see Table S-5, supplementary material), the perception of the diagnosis at t2 varied widely; thus, a total of 90% of CERP patients rated the result to be positive, while only 47% CURP patients did so (p = 0.013, χ2 test).
Relationship of basic characteristics and psychological outcome
There were no differences regarding smoking habits, alcohol consumption, medication use and previous short anesthesia, depression and panic disorders between the two clusters (see Table 1, and Tables S-2 and S-3). Neither did personality traits differ (see Table 2); only the medium score of agreeableness showed a tendency to be more frequent in CURP patients (86% vs. 70%, p = 0.083). On the other hand, slight differences appeared regarding the distribution of the intensity of characteristics (see Table 2); none of the CURP patients showed conscientiousness above average, while 15% of CERP patients did so (p = 0.025, χ2 test).
Discussion
Propofol is recommended for sedation during gastrointestinal endoscopy, but evidence of its addictive potentials increases. As already suggested in a small crossover study in healthy volunteers,8 we could clearly distinguish two different clusters of reaction by means of a factor analysis in patients undergoing elective gastrointestinal endoscopy (see Figure 1). A total of 56% belonged to Cluster 1, characterized by less activation, partially worse mood and less relaxation with an increased level of sedation; it was, therefore, called the cluster of uneasy reaction pattern (CURP). Cluster 2, called cluster of euphoric reaction pattern (CERP), is characterized by improved mood, deeper relaxation and less sedation and anxiety. This euphoric reaction pattern, which is one of the criteria for the relative addictive risk of hypnotics,9 appears unexpectedly often in 44% of patients.
Appropriately, one week later, CERP patients remembered their positive affective state, as reported immediately after endoscopy. Moreover, the dimensions cheerfulness and activation were rated even higher (see Table 3), while relaxation and anxiety were remembered similarly (see Figure 2). Furthermore, the CERP patients rated the diagnosis after endoscopy more favorably and advantageously, although there was no difference objectively regarding the severity of diagnosis (see Table S-2, supplementary material). This strong reminiscence of a euphoric propofol effect thereafter is remarkable.
According to present theories, drug addiction develops in several steps:17,18,27–31 At first there is the experience of a reinforcing effect of a drug, e.g. a positive hedonic effect like euphoria or the reduction of an aversive affective state, such as anxiety. In particular, a positive hedonic effect is related to the increased activity of the dopaminergic reward system triggered by the respective drug. In the next step a regular use is established that in turn induces via biological changes, e.g. in the reward system, changes in mental functioning, e.g. attention bias to drug-related stimuli, decreased ability to inhibit drug use behavior. Eventually, addictive use of a drug is established that is characterized by a strong urge to use a drug even if it is damaging to the social and health situation (“wanting”) instead of the initial experience of a positive drug effect (“liking”31). The risk of transition from “liking” to “wanting” is difficult to estimate for an individual and a respective drug, because there are several factors influencing this risk, e.g. genetics of the reward system, availability of a drug, individual reaction to the drug. For certain, the reminiscence of a positive effect of propofol as found in the present cohort is a basic risk factor in the development of drug addiction. In addition, it is known that propofol manipulates the dopaminergic reward system, which is a basic common property of drugs able to induce the development of an addiction.5–7
Patients experiencing a positive effect after a drug administration who simultaneously exhibit higher levels of specific personality traits, such as neuroticism or impulsivity, are thought to be at a higher risk of developing drug addiction.32,33 However, we could not prove any risk factor for a euphoric propofol reaction. On the other hand, we identified slight differences regarding personality: None of the CURP patients showed above average conscientiousness, while 15% of the CERP patients did so. By contrast, about 21% of CURP patients exhibited above average agreeableness, while only 12% CERP patients did so. Below average neuroticism was apparent in 16% of patients in CURP and in 9% in CERP. However, the mean rating of all personality traits did not differ; further studies with larger cohorts might clarify these psychological relations.
Limitations
All 25 adjectives that have been used to describe the dimensions of mood (cheerfulness, relaxation, activation, sedation, anxiety; five adjectives for each dimension) had been gathered from well-established questionnaires.22,23 However, this specific assembly of adjectives was not evaluated in a larger population. In addition, the study population was not large enough to establish an internal validation. For the differentiation of particular reaction patterns, adjectives that clearly characterize euphoria (overexcited, relaxed, happy, in a chilled manner, cheerful, buoyant, optimistic, gleeful for CERP) and unease (anxious, concerned, worried, nervous CURP) were arranged. We applied a well-established and conservative clustering approach, but, of course, all classification methods are more or less prone to produce artificial results. However, our results are highly comparable between methods of distance measuring (Euclidian vs. Manhattan) or aggregation methods (maximum linkage vs. ward vs. neighbor-joining, data not shown).
We included only patients who underwent gastrointestinal endoscopy under mono sedation with propofol. Since our study design lacks a control group that underwent endoscopy without sedation, the psychotropic effects documented probably, but not reliably, are attributed to propofol. The virtue of propofol to induce euphoria has already been shown in animal models and healthy volunteers5–8 and a growing number of propofol addiction cases have been documented.10–13 On the other hand, a linkage between endoscopy and psychotropic effects has not been proven and the results of endoscopy did not influence the reaction pattern. However, since about 90% of gastrointestinal endoscopies are performed under sedation,34 gaining a proper control group is markedly challenging and would, as individuals who abandon sedation presumably exhibit particular personality traits and psychological reaction patterns, probably result in a selection bias.
Conclusion
In conclusion, our data show that patients react psychologically in different ways to propofol administration. The group of patients who showed a euphoric reaction pattern comprised almost half of all patients investigated. Most patients remembered these specific patterns even a week later. It is difficult to estimate how many patients experiencing a euphoric reaction pattern bear a relevant risk of developing propofol addiction. Presumably, the high-risk group consists of those patients who experienced a euphoric effect and showed psychological and anamnestic risk factors for addiction. Further studies should focus on these traits. Endoscopists and anesthesiologists should be aware of the psychotropic effects of propofol especially in patients who request examinations that are only questionably indicated.
Supplementary Material
Acknowledgements
We gratefully thank Jules Huber for her linguistic assistance in translating emotion- and mood-describing idioms (Supplementary material, Table 1).
Writing assistance: Jules Huber has graciously assisted to translate emotion- and mood-describing idioms (Supplementary material, Table 1) from German into English. The manuscript has been proofread by a language editing service (Phillip Saunders, Language Support Services, Jablonskistr. 4a, D-10405 Berlin).
Specific author contributions: Christoph Maier: Conception and design of the study, data analysis and interpretation, supervision, reviewing the manuscript; approval of the final manuscript.
Andrea Riphaus: Conception and design of the study, data acquisition and interpretation, drafting the manuscript; approval of the final manuscript.
Thorsten Brechmann: Conception and design of the study, data acquisition, analysis and interpretation, drafting the manuscript; approval of the final manuscript.
Fred Rist: Conception and design of the study, data interpretation, reviewing the manuscript; approval of the final manuscript.
Jan Vollert: Data analysis and interpretation; reviewing the manuscript; approval of the final manuscript.
Miriam Kaisler: Data acquisition, analysis and interpretation, drafting the manuscript; approval of the final manuscript.
Norbert Scherbaum: Conception and design of the study, data analysis and interpretation, reviewing the manuscript; approval of the final manuscript.
Wolff Schmiegel: Supervision, reviewing the manuscript; approval of the final manuscript.
Svetlana Pak: Data acquisition, reviewing the manuscript; approval of the final manuscript.
Declaration of conflicting interests
None declared.
Ethics approval
This study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki, and has been approved by the ethical review board of the Ruhr-University Bochum (November 15, 2013, registry number 4817-2013) and registered in the German Clinical Trial Registry (DRKS00011202),
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Informed consent
Written, informed consent was obtained from each patient.
References
- 1.Luginbühl M, Vuilleumier P, Schumacher P, et al. Anesthesia or sedation for gastroenterologic endoscopies. Curr Opin Anaesthesiol 2009; 22: 524–531. [DOI] [PubMed] [Google Scholar]
- 2.Dumonceau JM, Riphaus A, Schreiber F, et al. Non-anesthesiologist administration of propofol for gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates Guideline—Updated June 2015. Endoscopy 2015; 47: 1175–1189. [DOI] [PubMed] [Google Scholar]
- 3.Riphaus A, Wehrmann T, Hausmann J, et al. Update S3-guideline: “Sedation for gastrointestinal endoscopy” 2014 (AWMF-register-no. 021/014). Z Gastroenterol 2016; 54: 58–95. [DOI] [PubMed] [Google Scholar]
- 4.Rex DK, Deenadayalu VP, Eid E, et al. Endoscopist-directed administration of propofol: A worldwide safety experience. Gastroenterology 2009; 137: 1229–1237. [DOI] [PubMed] [Google Scholar]
- 5.Li KY, Xiao C, Xiong M, et al. Nanomolar propofol stimulates glutamate transmission to dopamine neurons: A possible mechanism of abuse potential? J Pharmacol Exp Therapeutics 2008; 325: 165–174. [DOI] [PubMed] [Google Scholar]
- 6.Bonnet U. Assessment of the addictive risk of propofol [article in German]. Fortschr Neurol Psychiatr 2011; 79: 442–452. [DOI] [PubMed] [Google Scholar]
- 7.Pain L, Oberling P, Sandner G, et al. Effect of propofol on affective state as assessed by place conditioning paradigm in rats. Anesthesiology 1996; 85: 121–128. [DOI] [PubMed] [Google Scholar]
- 8.Zacny JP, Lichtor JL, Thompson W, et al. Propofol at a subanesthetic dose may have abuse potential in healthy volunteers. Anesth Analg 1993; 77: 544–552. [DOI] [PubMed] [Google Scholar]
- 9.US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research. Assessment of abuse potential of drugs: Guidance for industry. Silver Spring, MD: FDA, 2010.
- 10.Monroe T, Hamza H, Stocks G, et al. The misuse and abuse of propofol. Subst Use Misuse 2011; 46: 1199–1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kranioti EF, Mavroforou A, Mylonakis P, et al. Lethal self administration of propofol (Diprivan). A case report and review of the literature. Forensic Sci Int 2007; 167: 56–58. [DOI] [PubMed] [Google Scholar]
- 12.Bonnet U, Scherbaum N. Craving dominates propofol addiction of an affected physician. J Psychoactive Drugs 2012; 44: 186–190. [DOI] [PubMed] [Google Scholar]
- 13.Maier C, Iwunna J, Tsokos M, et al. Deaths by propofol abuse. Results of questioning in legal-medical institutes in Germany, Austria and Switzerland [article in German]. Anaesthesist 2017; 66: 109–114. [DOI] [PubMed] [Google Scholar]
- 14.Roh S, Park JM, Kim DJ. A case of propofol dependence after repeated use for endoscopy. Endoscopy 2011; 43(Suppl 2 UCTN): E362–E362. [DOI] [PubMed] [Google Scholar]
- 15.Koopmann A, von der Goltz C, Hermann D, et al. Propofol addiction initiated by anesthetic use. Am J Psychiatry 2011; 168: 211–212. [DOI] [PubMed] [Google Scholar]
- 16.Maier C, Leclerc-Springer J. Life-threatening fentanyl and propofol addiction: Interview with a survivor [article in German]. Anaesthesist 2012; 61: 601–607. [DOI] [PubMed] [Google Scholar]
- 17.Fergusson DM, Horwood LJ, Lynskey MT, et al. Early reactions to cannabis predict later dependence. Arch Gen Psychiatry 2003; 60: 1033–1039. [DOI] [PubMed] [Google Scholar]
- 18.Stevens S, Rist F, Gerlach A. A review of experimental findings concerning the effect of alcohol on clinically relevant anxiety [article in German]. Z Klin Psychol Psychother 2008; 37: 95–102. [Google Scholar]
- 19.Löwe B, Spitzer RL, Zipfel S, et al. Gesundheitsfragebogen für Patienten (PHQ D). 2, Auflage. Karlsruhe: Pfizer, 2002. [Google Scholar]
- 20.Rist F, Scheuren B, Demmel R, et al. Alcohol Use Disorders Identification Test (AUDIT-G-M). In: Glöckner-Rist A, Rist F, Küfner H. (eds). Electronic manual on surveillance instruments in the area of addiction (EHES) [manual in German]. Version 3.00, Mannheim: Zentrum für Umfragen, Methoden und Analysen, 2003. [Google Scholar]
- 21.Chabrol H, Niezborala M, Chastan E, et al. A study of the psychometric properties of the Fagestrom Test for Nicotine Dependence. Addict Behav 2003; 28: 1441–1445. [DOI] [PubMed] [Google Scholar]
- 22.Steyer R, Schwenkmezger P, Notz P, et al. The Multidimensional Sensitivity Questionnaire (MDBF) [original in German], Göttingen: Hogrefe, 1997. [Google Scholar]
- 23.Rueger SY, King AC. Validation of the brief Biphasic Alcohol Effects Scale (B-BAES). Alcohol Clin Exp Res 2013; 37: 470–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krohne HW, de Bruin JT, Mohiyeddini C, et al. Specific dimensions of anxiety in surgical patients. Development of a questionnaire and empirical results [article in German]. Psychother Psychosom Med Psychol 2000; 50: 72–80. [DOI] [PubMed] [Google Scholar]
- 25.Gerlitz JY and Schupp J. To survey the Big Five-based personality traits in the SOEP [original in German]. DIW Research Notes 4/2005. Berlin: Deutsches Institut für Wirtschaftsforschung, 2005.
- 26.Standards of Practice Committee of the American Society for Gastrointestinal Endoscopy, Lichtenstein DR, Jagannath S, et al; Sedation and anesthesia in GI endoscopy. Gastrointest Endosc 2008; 68: 815–826. [DOI] [PubMed]
- 27.Schuckit MA. Treatment of opioid-use disorders. N Engl J Med 2016; 375: 357–368. [DOI] [PubMed] [Google Scholar]
- 28.Wise RA, Koob GF. The development and maintenance of drug addiction. Neuropsychopharmacology 2014; 39: 254–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Koob GF. The dark side of emotion: The addiction perspective. Eur J Pharmacol 2015; 753: 73–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nutt D, King LA, Saulsbury W, et al. Development of a rational scale to assess the harm of drugs of potential misuse. Lancet 2007; 369: 1047–1053. [DOI] [PubMed] [Google Scholar]
- 31.Berrigde KC, Robinson TE. Liking, wanting, and the incentive-sensitization theory of addiction. Am Psychol 2016; 71: 670–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Few LR, Grant JD, Trull TJ, et al. Genetic variation in personality traits explains genetic overlap between borderline personality features and substance use disorders. Addiction 2014; 109: 2118–2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kreek MJ, Nielsen DA, Butelman ER, et al. Genetic influences on impulsivity, risk taking, stress responsivity and vulnerability to drug abuse and addiction. Nat Neurosci 2005; 8: 1450–1457. [DOI] [PubMed] [Google Scholar]
- 34.Riphaus A, Geist F, Wehrmann T. Endoscopic sedation and monitoring practice in Germany: Re-evaluation from the first nationwide survey 3 years after the implementation of an evidence and consent based national guideline. Z Gastroenterol 2013; 51: 1082–1088. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.