Sir,
A 25-year-old male presented with persistent fever for 2 months which was low grade with evening rise. On general examination, the patient was febrile with moderate pallor. Systemic examination revealed hepatosplenomegaly (HSM). There was no evidence of peripheral lymphadenopathy/bleeding or any other significant findings. Chest X-ray showed focal haziness in lower lobes. Peripheral smear showed mild anemia and thrombocytopenia with absence of any hemoparasite. Urine routine and microscopy were within normal limits. Widal test and serological status were also negative. Sputum examination does not show any acid-fast bacilli.
Hence, based on clinical presentation of long-standing fever with evening rise, weight loss, and haziness on chest X-ray, a provisional diagnosis of tuberculosis was suspected, and the patient was started on antitubercular treatment. The patient returned after 1 month with absence of any significant response. In view of persistent thrombocytopenia, fever, and HSM, the diagnosis was reconsidered and bone marrow (BM) aspiration was performed to rule out other causes such as lymphoma/leukemia, metastasis, Kala Azar, and other hematological causes.
BM was mildly hypercellular with mild erythroid hyperplasia and normoblastic maturation. Megakaryocytes were adequate. Myeloid series show orderly maturation. Few eosinophils and plasma cells are also seen. Many intracellular round inclusion like structures in the cytoplasm of macrophages were seen resembling histoplasma [Figure 1]. There was absence of separate nucleus and kinetoplast of Leishmania. Thus, based on morphology, a diagnosis of histoplasma was considered and special stain for fungus was asked for which confirmed the diagnosis [Figure 2]. Diagnosis of disseminated histoplasmosis (DH) was rendered to the patient in view of the presence of lung lesion, HSM, and BM involvement and was started on antifungal treatment. The patient responded well to the treatment and was lost to follow-up after 1 month of treatment.
Figure 1.
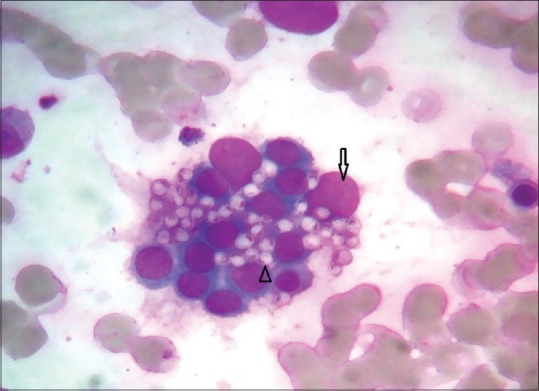
Leishman-stained smears show erythroid Island with macrophage (arrow) showing multiple intracellular histoplasma organisms (arrowhead) (×1000)
Figure 2.
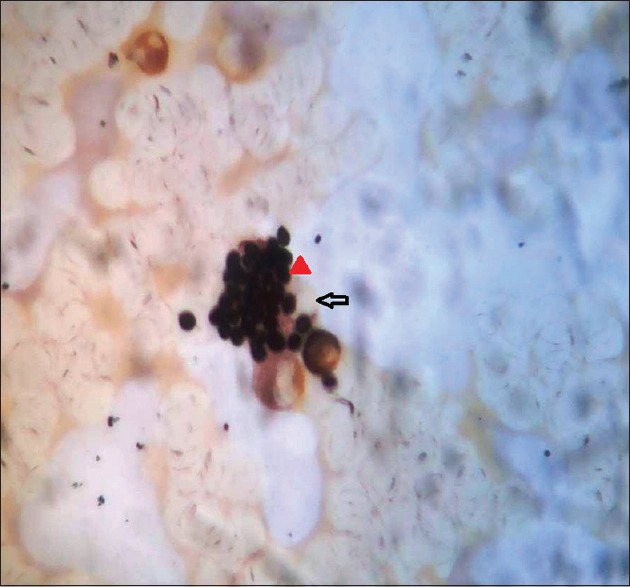
Grocott's methenamine silver stain highlighting the fungal organism (arrowhead) inside the macrophage (arrow) (×1000)
Histoplasmosis is a systemic fungal infection, and the disease spectrum ranges from asymptomatic primary infection to disseminated disease in immunocompromised patients.[1] DH is defined as a condition where fungus is present in more than one location. Most common signs and symptoms are fever, HSM, lymphadenopathy, ulceration of mucosa, and BM involvement.[2] It is endemic in great river valleys in the American and African countries but is still rare in India. In India, most cases have been reported from eastern region of India, especially in West Bengal and Gangetic plains. Approximately 10% patients infected may develop progressive DH [3] and is mostly seen in patients who are immunocompromised, transplant patients, and patients with hematological malignancy.[4] DH in immunocompetent patients is rare but can be seen as described in various case reports.[5] Histoplasma has to be differentiated from Leishmania which shows nucleus and kinetoplast of amastigote forms. We report here a case of an immunocompetent patient developing DH presenting as fever with bicytopenia and diagnosed on BM examination.
Thus, BM can be helpful in cases of pyrexia of unknown origin with hematological abnormality and histoplasma should be considered and to be looked for even in nonendemic areas.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sane SY, Patel MG, Patel BM, Kokal K. Disseminated histoplasmosis (a case report) J Postgrad Med. 1983;29:270–3. [PubMed] [Google Scholar]
- 2.Fortaleza SC, Lopes SK, Bandeira TJ, Nogueira TN, Holanda MA. Acute disseminated histoplasmosis in an immunocompetent patient. J Bras Pneumol. 2004;30:1–6. [Google Scholar]
- 3.Kauffman CA. Histoplasmosis. In: Goldman L, Schafer AI, editors. Cecil Medicine. 24th ed. Philadelphia, PA: Saunders Elsevier; 2011. Ch. 340. [Google Scholar]
- 4.Srikrishna A, Sitalakshmi S, Shantala Devi AM, Damodar P, D'Souza GA. Disseminated histoplasmosis in an AIDS patient diagnosed on bone marrow. Indian J Pathol Microbiol. 2002;45:333–4. [PubMed] [Google Scholar]
- 5.Mukherjee A, Tangri R, Verma N, Gautam D. Chronic disseminated histoplasmosis bone marrow involvement in an immunocompetent patient. Indian J Hematol Blood Transfus. 2010;26:65–7. doi: 10.1007/s12288-010-0022-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


