Abstract
While physical inactivity is a key risk factor for a range of chronic diseases and conditions associated with aging, a significant proportion of midlife and older adults remain insufficiently active. This is particularly true for ethnic minority populations such as Latino adults for whom few culturally adapted programs have been developed and tested. The major objective of this 12-month cluster-randomized controlled trial is to test the comparative effectiveness of two linguistically and culturally adapted, community-based physical activity interventions with the potential for broad reach and translation. Ten local community centers serving a sizable number of Latino residents were randomized to receive one of two physical activity interventions. The Virtual Advisor program employs a computer-based embodied conversational agent named “Carmen” to deliver interactive, individually tailored physical activity advice and support. A similar intervention program is delivered by trained Peer Advisors. The target population consists of generally healthy, insufficiently active Latino adults ages 50 years and older living within proximity to a designated community center. The major outcomes are changes in walking and other forms of physical activity measured via self-report and accelerometry. Secondary outcomes include physical function and well-being variables. In addition to these outcome analyses, comparative cost analysis of the two programs, potential mediators of intervention success, and baseline moderators of intervention effects will be explored to better determine which subgroups do best with which type of intervention. Here we present the study design and methods, including recruitment strategies and yield as well as study baseline characteristics.
Trial Registration: clinicaltrial.gov Identifier = NCT02111213.
Keywords: Aging, Physical activity, Latino, Clinical trial, Community-based, Information technology
1. Introduction
Physical inactivity is responsible for nearly 10% of major noncommunicable diseases (NCDs) worldwide [1]. In the U.S., population-level data suggest that increasing regular moderate physical activity could reduce annual medical costs by as much as $76.6 billion [2]. While national guidelines for physical activity promotion emphasize the importance of appealing and convenient physical activities such as walking [3], a significant proportion of Americans (33%) remains inactive [4]. This is particularly true for older (45% inactive), low-income (46% inactive), and Latino adults (44% inactive) [4], who have high rates of obesity and other chronic conditions (e.g., Type 2 diabetes) [5] in combination with often reduced access to programs to improve physical and mental health [6].
Few physical activity programs have taken into account the cultural preferences and needs of Latino Americans—among the fastest growing segments of the U.S. population, including aging adults [7]. The major objective of the COMPASS Trial is to systematically compare culturally adapted and individually tailored physical activity counseling for midlife and older Latino adults delivered through two different communication channels: trained peer advisors (called promotores de salud) vs. a virtual advisor (i.e., a computer-based embodied conversational agent named “Carmen”). Peer or lay health advisors, which have been in existence in Latino communities for decades [8], are typically members of the community in which they work, sharing the community's culture, language, and environment [9,10–12]. However, few such programs have specifically targeted physical activity counseling [13]. Similarly, while evidence suggests that aging adults as well as Latinos and other racial/ethnic minorities are increasingly using computer technology and e-Health platforms [14], most people targeted by e-Health programs have been well educated, younger (< 55 years), and White [14–17]. These circumstances increase concerns that e-Health may intensify the “digital divide” and exacerbate health disparities for under-represented communities [14,18,19]. In particular, restricted computer access and lower computer, health, and language literacy levels are significant barriers for underserved populations [14]. Few websites have been designed for persons with less than a high school education [14], and few e-Health programs incorporate cultural factors in health communications [20]. For web-based programs that do offer information in Spanish, content quality often has been substandard [21]. This may help to explain why only 42% of Latino adults ages 55 and older use the Internet, compared with 57% of non-Latinos [19]. In response to these often-cited barriers, the state-of-the-science “virtual advisor” computer technology being employed in COMPASS requires minimal computer skills or literacy, and provides personally and culturally tailored physical activity advice and support in multiple languages [22].
The COMPASS Trial allows for a direct determination of program comparative effectiveness for the Peer vs. Virtual Advisor programs. It also provides the opportunity to explore which Latino adult subgroups may do best with which type of communication channel. Given the dearth of community-based clinical trials in the health promotion area that have specifically targeted low-income aging Latinos, the COMPASS Trial also presents a unique opportunity to evaluate recruitment channels of particular relevance to Latino adults. The study design and procedures, including recruitment, intervention, and assessment procedures, constitute the major focus of this paper.
2. Methods and procedures
The Stanford University School of Medicine Institutional Review Board approved the study protocol for the COMPASS (Computerized Physical Activity Support for Seniors) Trial. All study materials, including informed consent and recruitment, intervention, and assessment forms, were produced in English and underwent thorough translation into Spanish by certified translators. Participants provided written consent upon reviewing the consent form with a bilingual staff member. The trial was registered at Clinicaltrials.gov (#NCT02111213).
2.1. Study design
The primary aim of this randomized trial is to test whether the Virtual Advisor intervention is as efficacious as the Peer Advisor intervention in promoting significant 12-month increases in weekly minutes of walking—a form of moderate-intensity activity that is readily accessible and appealing to substantial numbers of midlife and older adults across the socioeconomic spectrum [3,23]. The study employs a cluster-randomized design of community centers located in neighborhoods with at least 20% midlife and older Latino residents [24]. In addition to location, other factors that were considered in choosing community centers included interest and willingness of center staff to participate in the study, appropriate space to accommodate computer equipment for the Virtual Advisor or Peer Advisor sessions, and a steady flow of Latino midlife and older adults who utilize the center's regular programs and services. Community centers were matched by geographic location and randomized to either the Peer Advisor or Virtual Advisor intervention arm. The comparative effectiveness of these two interventions constitutes the major objective of the study and is the focus of this paper. To take advantage of the study design to begin to explore new dietary intervention strategies in this underserved population, an additional pilot sub-study is also underway. As part of this pilot sub-study, two other similar community centers (one in each county in which the study is located) have been selected to receive culturally adapted dietary information via mail and face-to-face modalities across the one-year study period.
2.2. Study location and participants
The study is located in two San Francisco Bay Area counties—Santa Clara and San Mateo counties. Approximately 26% of the population across these two counties report being of Latino or Hispanic ethnicity [www.census.gov, 2015 American Community Survey]. Latinos in the western U.S. come largely from Mexico and Central America [24]. Of those born outside the US, approximately 50% have lived here for 15 or more years.
The following study eligibility criteria were used to enroll study participants: (a) ages 50 years and older; (b) insufficiently active [3], i.e., engaged in < 100 min/week of moderate intensity activity over the past six months, based on initial study physical activity screening items (see below), followed by a final baseline physical activity determination using the full CHAMPS questionnaire; [25] (c) able to safely engage in moderate forms of physical activities such as walking based on the Physical Activity Readiness Questionnaire; [26] (d) living within close proximity to one of the study-designated community centers to allow regular (e.g., weekly) attendance to the community center-based intervention sessions; (e) able to read and understand English or Spanish sufficiently to provide informed consent and participate in all study procedures; and f) planning to live in the area for the next twelve months. The study screen, typically by phone, to determine physical activity status included the following questions: 1) In the last three months have you regularly participated (at least two times per week) in any physical activity that has increased your breathing, such as aerobics, brisk walking, dancing, swimming, or playing sports? If the participants answered “yes”, they were asked to describe how many days per week they regularly exercised and how many minutes per day. These numbers were multiplied to calculate the total number of minutes per week. If the total number was 100 min or more, the individual was deemed ineligible. If the total number of minutes per week was reported as < 100, then individuals were asked to report, in a typical or normal week over the past four weeks, the total number of minutes per week they engaged in dance, walking or hiking uphill, walking fast or briskly for exercise, and water exercises other than swimming. Individuals were deemed eligible if participation in the above exercises totaled < 100 min per week. A final determination of study eligibility based on physical activity status occurred at baseline using the full CHAMPS questionnaire.
2.3. Study participant recruitment and screening methods
To enhance external validity, three complementary recruitment methods were employed: geographically defined targeted mass mailings, cultural media-based promotion, and community outreach [27–29]. For the geographically defined targeted mass mailings, mailing addresses of residents in geographically defined Census block groups near the community centers were accessed via a private mail service company and selected based on age and Latino ethnicity. Introductory bilingual letters describing the study and business reply cards were sent to households, along with a toll-free number to call to obtain further study information and undergo initial screening for study eligibility. Those individuals judged to be initially eligible based on the telephone screen were invited to attend a group study orientation session at their designated community center, during which time the study objectives and procedures were explained in further detail, all questions were answered, and interested individuals were scheduled for an individual baseline assessment visit also held at the community center. Those individuals found to be eligible and willing to enroll in the study were scheduled for an initial individual intervention session at the community center.
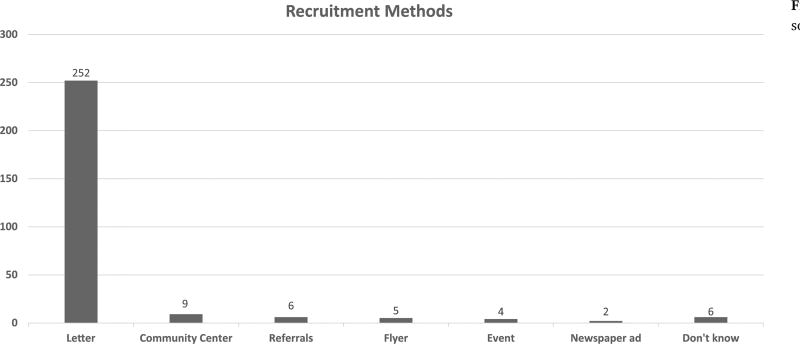
To broaden the types of individuals enrolled in the trial, the targeted mass mailings were augmented with bilingual media-based promotion and community outreach [27–29]. The media promotional methods included study announcements placed in local Latino newspapers. As part of community outreach activities, study information was placed at participating community centers and was made available at local stakeholder events attended by bilingual study staff, such as health and resource fairs, back to school nights, Parent Teacher Association (PTA) meetings, local school council events, and parent group meetings, as well as neighborhood libraries, churches, local health clinics serving Latino adults, and local grocery stores [30]. Study participants and others who expressed interest in the study also were encouraged to refer others or share study information. The subject yield for the different recruitment strategies across the 24-month study recruitment period is summarized in Fig. 2 of the Results section.
Fig. 2.
Total number of enrolled subjects by recruitment sources.
2.4. Study participant retention methods
To promote high levels of participant retention across the 12-month intervention and assessment period, group-based study orientation sessions were employed following the telephone screening process and prior to baseline assessment to ensure that all individuals considering study participation were fully informed about the study objectives, what would be expected of them throughout the study, and what they in turn could expect from the study staff. The interactive group session included the weighing of the pros and cons of participating in the study, along with related motivational interviewing techniques and behavioral strategies, such as structuring of realistic expectations related to study outcomes. This type of pre-enrollment educational session has been associated with high levels of study retention in health behavior change trials across periods lasting up to 18 months [31].
2.5. Peer Advisor recruitment and screening methods
Recruitment of Peer Advisors was accomplished using a variety of strategies. Study interventionists worked with the community center staff to identify activities within the community center through which Peer Advisors might be recruited. In addition, study staff requested referrals of people who attended the community centers regularly and who center staff identified as potentially viable candidates for the Peer Advisor role. In addition to collaborating with the community centers directly, Peer Advisor recruitment was also conducted through collaborating with different agencies external to the community centers. These agencies included local social and civic service agencies along with educational institutions such as schools and libraries. In addition, some recruitment efforts occurred through partnering with local fitness centers and targeting their physically active population as potential study peer advisors.
Peer Advisor eligibility criteria consisted of the following: (a) ages 30 years and older; (b) physically active on a regular basis (i.e., engaged in approximately 150 min/week or more of moderate intensity physical activity over the past 12 months); (c) free of any medical problems that might make it difficult to participate in regular physical activity or serve as a Peer Advisor in the study (e.g., any unstable chronic conditions); (d) willing to participate in the peer advisor 12-hour training program and volunteer an average of 2–3 h per week to advise their participants on physical activity; (e) willing to participate in monthly Peer Advisor supervision meetings; (f) able to read and understand English or Spanish sufficiently to provide informed consent and participate in all study procedures; and (g) planning to live in the area for the next 12 months. Peer Advisor selection and training consisted of screening interested individuals by phone to determine initial eligibility. Eligible individuals then attended an orientation session during which time the study objectives and procedures were explained in further detail, all questions were answered, and interested individuals provided informed consent related to study confidentiality protocols and information sharing. Individuals then completed a 12-hour Peer Advisor training program based on the successful peer-led physical activity training programs conducted previously by the Stanford team [32–34].
2.6. Peer Advisor oversight and quality assurance methods
Ongoing Peer Advisor oversight and quality assurance have been accomplished through monthly Peer Advisor supervision meetings, periodic review of Peer Advisor logs and notes completed after each Peer Advisor-participant advising session, and random check-ins by study staff with study participants. Each monthly study staff-led, group-based Peer Advisor supervision meeting lasts approximately 120 min and focuses on the following activities: (a) sharing among Peer Advisors of their experiences and challenges with their participants, along with receipt of problem-solving advice and ideas from study staff and other Peer Advisors; (b) ongoing physical activity-relevant information and updates; and (c) provision of relevant resources such as tip pages and newsletters that Peer Advisors can use in their meetings with their participants.
2.7. Peer Advisor retention methods
In addition to the monthly supervision meetings, other Peer Advisor retention methods include annual informational and motivational workshops provided by Stanford investigators and staff, modest monetary payment for the general time commitment accompanying Peer Advisor activities (i.e., a $15 local store gift card received upon completion of each participant introductory intervention session; a monthly store gift card commensurate with the number of participant advising sessions completed that month, equaling $5.00 per advising session), intermittent receipt of low-cost project incentives (e.g., project apparel, project mugs and tote bags), and a certificate of completion honoring each Peer Advisor's contributions to the project at the end of his or her study advising period.
2.8. Development and delivery of study interventions
The two physical activity interventions are based on the theoretically derived cognitive-behavioral advice and support strategies used in the evidence-based Active Choices physical activity counseling program and similar behaviorally based interventions in the field [35–38]. The primary behavioral theory utilized in the program is Social Cognitive Theory [39] combined with the contextual framework of the Transtheoretical Model [40]. Social Cognitive Theory (SCT) recognizes the dynamic interplay of cognitive, behavioral, and social factors in influencing behavior change [39]. Among the variables derived from SCT are self-efficacy, the use of self-regulatory skills (e.g., self-monitoring, goal-setting), factors related to the physical activity behavior itself (e.g., format, intensity), and social environmental factors (e.g., modeling, social support, feedback from others), as predictors of physical activity participation [41]. Applications of the Transtheoretical Model to the health promotion area include the use of a range of behavioral and cognitive strategies aimed at an individual's motivational readiness to change a particular behavior (e.g., consciousness raising and other cognitive approaches in the preparation and action phases early in the program; reinforcement management and related behavioral approaches in the later phase of the program) [40].
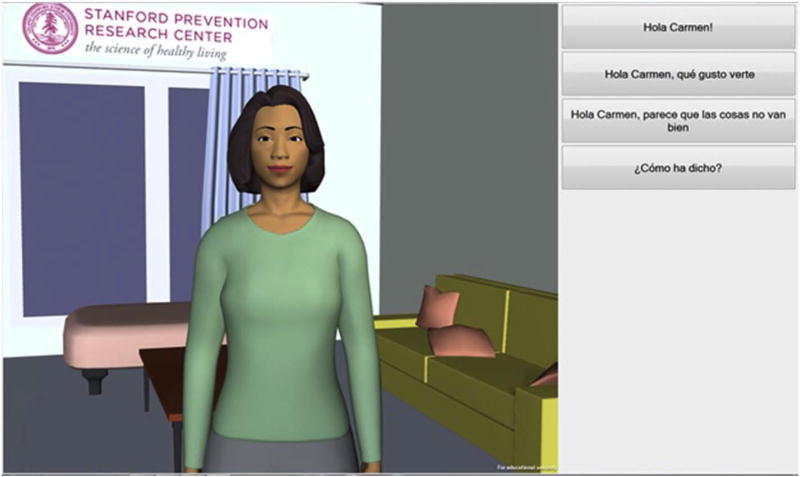
The Virtual Advisor program consists of an embodied conversational agent (ECA)—an interactive, animated computer character that simulates face-to-face counseling and support using simple speech as well as nonverbal behaviors (e.g., facial cues, hand gestures) [42,43] (See Fig. 1). Individuals interact with it through touching one of several simple conversation boxes shown on the screen throughout the interaction, which eliminates the need to utilize a computer mouse, track pad, or keyboard. The conversation boxes are aimed at less than an eighth grade education level [42,44].
Fig. 1.
Screenshot of the Virtual Advisor (“Carmen”).
The ECA communication interface has been shown to be effective in changing behavior in individuals with little to no computer experience and low levels of health literacy [44]. The initial adaptation of the Virtual Advisor program to the Latino population being targeted was accomplished through a smaller intervention study that preceded the current trial [22] that was based on earlier work with embodied conversational agents (i.e., virtual advisors) conducted by Dr. Bickmore [43]. This work was augmented with information from Dr. King et al.'s Active Choices physical activity intervention program [36]. The formative testing and pilot work that was conducted also suggested that “Carmen”, the virtual advisor, could be acceptable to other midlife and older ethnic minority groups as well, including Asian, Filipino, and African-American adults. The intervention protocol derived from this prior work was applied, in conjunction with similar intervention work with peer advisors [45], in establishing a parallel physical activity counseling program delivered in the trained Peer Advisor arm [45].
Both individually adapted programs are delivered at each participant's designated community center and focus in particular on walking and similar forms of moderate-intensity physical activity. Both interventions begin with an introductory session that covers the following information: [36] (a) review of the participant's physical activity history, long-term goals, and anticipated barriers to and facilitators of regular physical activity; (b) provision of information on the physical activity national guidelines, safety tips, and community center resources; (c) co-creation of a weekly physical activity plan; (d) training in the regular use of a pedometer and a project calendar to log steps and walking minutes; and (e) scheduling of the next intervention appointment.
Following the introductory session, each session follows a standard counseling protocol that is similar across the two interventions and which generally consists of the following elements: greetings and introductory social dialogue, checking for important health changes, review of pedometer-measured steps and minutes walked since the last advising session, acknowledgement of successes, problem-solving around barriers to physical activity, provision of relevant information to continue with physical activity or to overcome barriers, goal-setting for the period between the current and the next advising session, scheduling of the next advising session, and summary and wrap up. The typical advising session for each intervention was developed to average approximately 10–15 min, and the general schedule of advising sessions for both arms over the one-year intervention period, based on previous research [32,36], is as follows: weekly sessions for the first two months; and twice-per-month sessions for the remaining 10 months.
In the Peer Advisor arm, peer advisors meet with their individual participants in a location within the community center that affords privacy. The Virtual Advisor, meanwhile, is housed on a dedicated computer (supplied by the study) located in a private, secure area at each designated community center receiving that intervention. Participants are trained in a brief introductory session with project staff and are provided with a private log-in to initiate sessions with the advisor. Similar to the Peer Advising arm, participants are taught to use an Omron pedometer (Omron Healthcare, Inc., model HJ-720ITC, Lake Forest, Ill, 60045, USA), which provides a valid, reliable daily step count under prescribed and self-paced walking conditions in normal-weight and overweight adults [46]. Participants are instructed to wear the pedometer on a daily basis, and download it on the Virtual Advisor computer via USB port at each session. The Omron can reliably store data for up to 41 days. Participants also complete a brief survey of personalized information at enrollment (e.g., favorite entertainment, names of supportive relatives/friends) that is programmed into the computer to personalize Virtual Advisor dialogue. Participants are encouraged to wear headphones during Virtual Advisor sessions to ensure privacy. As described earlier, Virtual Advisor and Peer Advisor sessions include individualized social interaction, progress review based on downloaded pedometer information, personalized feedback and problem solving, and goal setting based on current progress [47]. Educational information can be received if desired in both arms.
2.9. Intervention fidelity and quality assurance
To maintain intervention fidelity and quality assurance in the Peer Advisor arm, trained staff members conduct regular quality control checks and activities as described above [32,48]. Virtual Advisor quality assurance includes regular monitoring of system performance and backup along with participant log-in activity, and ongoing availability of a study helpline for participants and center staff to call for assistance in correcting any problems. A designated Stanford staff member is in regular contact (twice a month or more frequently as needed) with the Virtual Advisor programming and oversight team at Northeastern University to ensure that any problems that occur can be resolved in a timely manner.
2.10. Assessment: primary outcome measures
The primary outcome is change in walking activity across the 12-month intervention period. Walking is assessed at three time points (baseline, six months, 12 months) using the four walking items from the validated CHAMPS questionnaire (interview format) for older adults, which is available in English and Spanish [25,49,50]. The CHAMPS questionnaire assesses usual weekly minutes of walking over the previous 4 weeks. Such validated self-report instruments represent the most direct and reliable means for assessing walking patterns, given that device-based assessment tools (pedometers, accelerometers) typically capture more general movement levels beyond walking behavior. The CHAMPS walking items have been significantly associated with pedometer steps in previous studies, and were sensitive to change in the earlier conducted Virtual Advisor physical activity intervention study in a similar group of midlife and older Latino adults [22]. The CHAMPS total activity as well as moderate and more vigorous physical activity (MVPA) variables have been consistently associated with objective physical activity measures in prior studies and therefore will be evaluated as secondary measures of physical activity in the COMPASS Trial [52,53]. We will also describe the proportion of each arm meeting the national physical activity recommendations of at least 150 min/week of MVPA [3].
Physical activity measurement using the CHAMPS is accompanied by the validated Actigraph® accelerometer (model wGT3X) at each of the three assessment time points [54]. The accelerometer provides objective information related to overall physical activity amounts and intensity (though not the types of activities engaged in). The accelerometry protocol from a large study of 860 older adults is being applied [55]. The activity monitor is worn on the hip during waking hours for seven consecutive days at each time point, ensuring a sufficient number of days of physical activity data (at least five days is considered as complete data) commensurate with current physical activity studies in older adults [56]. Participants are instructed to wear the accelerometer for at least 8 h per day during their waking hours. Wear-time validity will be determined through applying the wear and non-wear time analysis and classification algorithms reported by Choi et al. [57], and analysis and interpretation of the accelerometry data will be based on our prior investigations and those of other older adult populations [58].
2.11. Secondary outcome measures
Secondary outcome variables of particular importance to aging Latino populations include the following: sedentary behavior, measured using a validated one-week recall survey responsive to change in older adults; [59] body mass index (BMI), derived using standard clinical assessment protocols for height and weight; [50] resting blood pressure and heart rate, using standard protocols; [50] physical function, assessed with the validated two-minute step test from the Senior Fitness Test protocol; [60] and quality of life and well-being, measured with the 10-item Vitality Plus Scale assessing well-being constructs associated with regular physical activity in aging adults, including sleep quality, energy, mood, and pain [61].
In addition to the above outcomes, program safety and adverse events are being tracked in both intervention arms using standardized forms and protocols used in prior physical activity intervention trials [32,37]. Also, overall participant acceptability ratings of the novel Virtual Advisor intervention are being assessed at the end of the 12-month intervention period via a 19-item computer program acceptability scale [62], a 4-item cultural congruity scale [63], and the Working Alliance Inventory's 12-item bonding subscale [22,64]. Similar program acceptability questionnaires are being collected in the Peer Advisor arm at 12 months [32].
2.12. Baseline moderators of intervention effects
Based on the human-computer interactions literature and our own work [65–68], we plan to evaluate several baseline moderators of intervention effects that are of particular relevance to the Peer vs. Virtual Advisor comparison and the social aspects of Latino culture [69]. Four such potential moderators are social anxiety, comfort with computers, perceived neighborhood social cohesion, and acculturation and health literacy levels. Social anxiety, drawn from Interpersonal Theory [70], refers to persons with increased social discomfort and anxiety. This subgroup has been shown to perform better with computers relative to humans across an array of educational tasks [67,71,72]. Descriptive analysis from a prior trial of ours comparing human vs. automated physical activity advisers also indicated that those with more social anxiety assigned to human advice had poorer physical activity levels compared to similar persons assigned to automated advice [73]. This construct is being measured via Fenigstein et al.'s scale [74].
Comfort with computers is another potential moderator that will be evaluated. Prior physical activity intervention work in this age group has shown that persons expressing less general comfort with and trust in computers had stronger preferences for non-automated (human) advisors relative to their peers [22,36]. This construct is being measured via the Computer Attitudes scale [75].
Perceived neighborhood social cohesion is a third potential moderator that will be evaluated. In addition to the psychosocial characteristics described above, the nature of the neighborhood environments in which walking typically occurs can affect physical activity levels [55]. For older Latinos, living in neighborhoods that enhance social contact and cohesion has been associated with greater physical activity and physical function [76,77]. It follows that those with higher neighborhood social cohesion may do well irrespective of program assignment, whereas those lower in social cohesion might require the additional personalized “touch” possible with the Peer Advisor. This construct is being measured via the Neighborhood Social Cohesion scale [78].
Acculturation and health literacy levels represent additional potential moderators that will be evaluated. Given that baseline levels of acculturation and health literacy may impact subsequent engagement with the two interventions, these constructs are being assessed using standard measures [79–81].
2.13. Potential mediators of intervention effects
To evaluate the pathways through which the two interventions may exert their effects, putative mediators of intervention success are being collected at the three measurement time points. Several mediational pathways of particular relevance to the Virtual Advisor vs. Peer Advisor comparison are advisor-based and social network-based support, access, and accountability. With respect to perceived advisor physical activity support, it has been suggested that the more neutral, less implicitly evaluative environment created by an automated or virtual advisor may be less socially threatening than that created by human advisors [67]. However, in one of our previous physical activity trials [36], we found that while the human and automated advisor programs showed similar significant increases in rated advisor support during the initial 6-month period, these increases were not sustained through 12 months in the automated advisor arm relative to the human advisor arm. This construct is being measured via the adapted Support for Exercise scale [82].
Social Cognitive Theory and the Transtheoretical Model underscore the importance of learning ways of enlisting support for ongoing behavior change from one's social network or environment, and this skill is emphasized in both the Peer and Virtual Advisor programs. In a previous physical activity trial involving a primarily Caucasian sample [36], both the human and automated advisor arms reported significant increases in this variable relative to control at 6 and 12 months. However, in our preliminary study of the COMPASS Virtual Advisor with a small Latino sample, this variable did not change significantly across the 4-month intervention period relative to control [22]. This construct is being measured via the Motivational Processes of Change Inventory [83].
Perceived access to and actual use of the advisor are additional putative mediators of intervention effects that will be explored. For example, the Virtual Advisor essentially “lives” at the community center and could conceivably be accessed by participants more often and more readily than the Peer Advisors. This in turn could affect physical activity participation. This construct is being evaluated using a brief scale from our prior research [36]. The actual amount of time participants interact with their assigned advisor across the intervention period also is being captured automatically by the Virtual Advisor program and through advising session logs kept by the trained Peer Advisors.
With respect to perceived accountability to the advisor, the more neutral, less implicitly evaluative environment created by an automated advisor, while potentially less socially threatening than that created by human advisors, may also engender less accountability to the advisor [67]. This could in turn result in a reduced likelihood of following the advisor's suggestions, which could negatively impact physical activity participation. We are measuring this construct via an adapted version of the Perceived Accountability scale [84], which assesses perceived accountability for both task (i.e., physical activity) performance and interpersonal facilitation.
2.14. Randomization of community centers to study arms
Block randomization by county locale was used to assign ten community centers to the two major study arms. Allocation concealment was in place for each block of centers during the randomization process to minimize selection bias with respect to subsequent blocks. Assessment staff members are blinded to randomization assignment.
2.15. Sample size calculation and data analysis plan
Sample size estimates have been developed to test the study's primary question related to whether the Virtual Advisor intervention is no worse than the intervention delivered by trained human advisors, i.e., a test of non-inferiority [85]. Using a two-tailed 95% confidence interval on the effect size (Cohen's d), the threshold of clinical significance between the two treatments, Δ, has been developed to demonstrate clinical non-inferiority of the new intervention (Virtual Advisor) if the confidence interval lay completely above −Δ, while clinical non-inferiority of the Peer Advisor intervention will be demonstrated if the confidence interval lay completely below +Δ. In this trial, the effect size (Cohen's d) is the standardized difference between the change in walking minutes/week over the 12-month intervention period. The critical value of Δ is based on a clinically meaningful difference between arms of 30 min of walking per week [3], and a within-arm standard deviation of 90, accounting for clustering within centers [86]. We calculated that a sample of 112 per arm (224 total) would provide 80% power to demonstrate non-inferiority between the two interventions using a simple pre-post analysis. We plan to use a mixed-effects linear regression model (linear on ln(t +1), where t is time from entry to the study, to model the usual rapid early change in physical activity with later stabilization, and use an autoregressive covariance structure (assuming that weeks that are closer together will be more highly correlated within subjects than those further apart). Mixed-effects linear regression effectively addresses both missing data and early dropout in “intent-to-treat” analysis [87,88]. In addition, the multiple assessment time points in the trial (at baseline, 6 months, and 12 months) will serve to provide more detailed information on changes over time relative to studies using pre-post assessment only [89]. Twenty-one additional participants were recruited to protect against loss to follow-up.
Similar mixed-effects linear regression techniques will be used to address the secondary outcomes of interest, e.g., intervention impacts on physical function and well-being variables across the study period.
2.16. Comparative cost analysis of the two programs
Given the dearth of cost analyses for e-Health and lay (peer) advisor programs generally as well as in the physical activity field, collecting such data is strongly recommended [90,91]. The analysis procedures that will be used are informed by the cost determinations used by other investigators in the physical activity arena [92,93]. Study methods have included the assessment of the costs of program administration so that analysis of the relation between costs and study outcomes can be conducted [90,93]. Costs that have been tracked in each intervention, based on prior literature [92–94], include costs of administering the programs and costs of participant compliance. Tracked participant compliance costs include length of the advising sessions and related contacts and costs associated with travel to community centers. The time participants spend engaging in physical activity is an outcome and will not be counted among program costs. Program costs will be compared to outcomes data (e.g., weekly minutes of walking) [95]. Among program costs included are the advisor training and supervision costs incurred in the Peer Advisor program, and the initial personalization and ongoing tech support costs incurred in the Virtual Advisor program. Given that tech support personnel are often more highly paid than community staff overseeing volunteers, the economic trade-offs for the two are currently unclear. (That is, the increased convenience and greater potential use of the Virtual Advisor may be offset by higher program maintenance costs.)
With respect to statistical power, cost analysis studies involving peer and automated physical activity advisors are lacking. However, a prior physical activity study that had sufficient power to successfully compare the cost-effectiveness of two active center-based physical activity programs had a combined sample size for the two active intervention arms (n = 235) that is comparable to the sample size in the current study [93]. Mixed-effects linear regression noninferiority and superiority methods will be employed.
2.17. Baseline moderator analysis
In addition to the above analyses, we plan to conduct exploratory moderator analyses following the procedures described by Kraemer et al. [96] and using mixed-effects linear regression models. The previously described moderator variables of interest will be centered and an interaction term calculated between the moderator variable and study arm assignment. Alpha will be set at 0.05 using a two-tailed test of significance for all interactions. Effect sizes will be calculated for moderation effects using Cohen's d formula [97]. Results from these analyses will inform future studies aimed specifically at a priori testing of specific moderators in this population to improve intervention response for non-responder groups.
2.18. Exploratory mediator analysis
As per prior mediation work [83,98], mediator analysis will follow the general procedures first described by Baron and Kenny [99] and informed by MacKinnon [100]. After confirming intervention success in changing physical activity, mixed effects linear regression will be used to evaluate if the interventions produced significant changes in the proposed mediators, described earlier, and if the proposed mediators were associated with significant increases in physical activity. Variables meeting these criteria will be included in formal tests of mediation, which will employ mixed effects linear regression modeling to assess whether treatment effect was attenuated after accounting for its indirect effects via the mediators. Complete mediation occurs when the direct effect of treatment in achieving improvements in physical activity vanishes when controlling for the putative mediator. The single mediator approach can be generalized to multiple-mediation scenarios provided that in step two of the Baron and Kenny approach, the putative mediators are regressed simultaneously on intervention group via a multivariate normal regression model, as per Preacher and Hayes [101].
3. Results
3.1. Selection and description of study community centers
Ten community centers located in Santa Clara and San Mateo Counties, California with at least 20% Latino households (range = 21–55% Latino households) living within a one- to five-mile radius from the center were identified and expressed interest in serving as a study intervention site. These sites were block-randomized by locale to either the Peer or Virtual Advisor arms. Soon after recruitment, one center experienced unforeseen changes in its administration that disrupted center operations and precluded center participation in the study. To ensure comparable participant enrollment in each study arm, additional participants were enrolled at the remaining four community centers assigned to that intervention arm.
In each center, there were center staff who were willing to support the research team in reserving meeting space for clinical assessments, recruitment meetings, and, when relevant, Peer Advisor meetings. For the sites that received the Virtual Advisor, designated staff members were instructed on how to maintain the computer kiosk (i.e., refilling printer paper, providing minor technical support related to the computer such as making sure that it was switched on and that the touch screen remained clean, and contacting a member of the research team if needed.)
All participating community centers offered, as part of their usual activities, a nutrition program for older adults as well as non-physical activity oriented classes and activities, such as bingo, karaoke, and arts and crafts. Additionally, 89% offered weekly physical activity classes and had at least one general computer available for older adults visiting their center.
3.2. Study participants enrolled and recruitment sources
Participant study enrollment occurred between July 2014 and July 2016. A total of 245 participants are enrolled in the primary trial (Peer Advisor arm: n= 122; Virtual Advisor arm: n =123). Participant baseline demographic and health characteristics are summarized in Table 1. The study participants range in age from 50 to 87 years, and 79% are women, with about half of participants reporting being married or living with a partner. The predominance of women is common in such health promotion intervention studies, as is the reluctance of participants, especially from such lower-income communities, to report their household incomes. Forty-four percent of participants have high school or lower levels of education.
Table 1.
Descriptive statistics for the sample and by randomization arm.
| All | Virtual Advisor | Peer Mentor | Between group p value |
||||
|---|---|---|---|---|---|---|---|
| Variable (categorical) | N | % | N | % | N | % | |
| Sex | |||||||
| Women | 193 | 78.8 | 98 | 79.7 | 95 | 77.9 | 0.73 |
| Men | 52 | 21.2 | 25 | 20.3 | 27 | 22.1 | |
| Race/ethnicity | |||||||
| Hispanic | 241 | 98.4 | 120 | 97.6 | 121 | 99.2 | 0.71 |
| Asian | 3 | 1.2 | 3 | 2.4 | 0 | 0.0 | |
| White | 1 | 0.4 | 0 | 0.0 | 1 | 0.8 | |
| Country of birth | |||||||
| United States | 100 | 40.8 | 53 | 43.1 | 47 | 38.5 | 0.01 |
| Mexico, Central, South America | 139 | 56.7 | 65 | 52.8 | 74 | 60.7 | |
| Other | 3 | 1.2 | 2 | 1.6 | 1 | 0.8 | |
| Missing | 3 | 1.2 | 3 | 2.4 | 0 | 0.0 | |
| Marital status | |||||||
| Married or living with partner | 125 | 51.0 | 59 | 48.0 | 66 | 54.1 | 0.11 |
| Not married or living with partner | 118 | 48.2 | 63 | 51.2 | 55 | 45.1 | |
| Refused | 2 | 0.8 | 1 | 0.8 | 1 | 0.8 | |
| Education | |||||||
| Less than High School | 62 | 25.3 | 27 | 21.9 | 35 | 28.7 | 0.42 |
| High school | 45 | 18.4 | 28 | 22.8 | 17 | 13.9 | |
| Some college | 80 | 32.7 | 39 | 31.7 | 41 | 33.6 | |
| College | 27 | 11.0 | 15 | 12.2 | 12 | 9.8 | |
| Postgraduate | 28 | 11.4 | 12 | 9.8 | 16 | 13.1 | |
| Missing | 3 | 1.2 | 2 | 1.6 | 1 | 0.8 | |
| Household income | |||||||
| < $5000 to $34,999 | 32 | 13.1 | 17 | 13.8 | 15 | 12.3 | 0.97 |
| $35,000 to $49,999 | 23 | 9.4 | 11 | 8.9 | 12 | 9.8 | |
| $50,000 to $74,999 | 30 | 12.2 | 16 | 13.0 | 14 | 11.5 | |
| $75,000 or greater | 45 | 18.4 | 21 | 17.1 | 24 | 19.7 | |
| Don't know, refused, missing | 115 | 46.9 | 58 | 47.2 | 57 | 46.7 | |
| Variable (continuous) | Mean | SD | Mean | SD | Mean | SD | |
| Age (yr.) | 62.3 | 8.4 | 63.1 | 8.3 | 62.4 | 8.5 | 0.82 |
| Years in US | 47.4 | 17.0 | 47.7 | 17.2 | 47.1 | 16.8 | 0.80 |
| Number in household | 3.5 | 2.2 | 3.7 | 2.5 | 3.3 | 1.8 | 0.16 |
| CHAMPS Q - baseline (min/wk.): | |||||||
| Walking for exercise & leisure | 45.9 | 91.6 | 48.0 | 98.1 | 43.6 | 81.4 | 0.71 |
| Walking briskly | 3.7 | 16.1 | 5.1 | 19.7 | 2.3 | 11.4 | 0.18 |
| Moderate, vigorous activities | 23.5 | 69.2 | 22.4 | 62.8 | 24.6 | 75.1 | 0.81 |
In addition, 39 participants are enrolled from the additional two non-physical activity center comparison sites that are participating in the dietary intervention pilot substudy that will be used to explore secondary questions of interest (e.g., examination of physical activity intervention effect size estimates relative to no physical activity intervention).
Sources of recruitment for the total sample of enrolled participants are summarized in Fig. 2. The highest recruitment yield (88.7% of enrolled subjects) was obtained from the geographically defined and demographically targeted bilingual mass mailings aimed at the Census blocks surrounding the community centers. The total number of targeted letters mailed describing the study and inviting individuals to contact the study team for more information was 107,930. The total cost of the targeted mailing recruitment strategy equaled approximately $69,900.00.
3.3. Results related to recruitment and enrollment of Peer Advisors
During the recruitment process for Peer Advisors, 230 individuals expressed initial interest, and 119 individuals were found to be eligible based on the study's Peer Advisor eligibility criteria. Of these individuals, 56 completed the Peer Advisor training requirement, and 36 initiated Peer Advisor activities with at least one participant. Over the course of the intervention period, six Peer Advisors had to relinquish their peer advisor activities due to a move out of the area, medical illness, or the initiation of a new job which put constraints on their time. Their study participants were transferred successfully to other Peer Advisors with minimal difficulties.
4. Discussion
The COMPASS Trial is among the first studies to systematically compare the effectiveness of physical activity advice delivered by humans versus automated advisors in aging Latino adults. Insufficiently active Latino adults are at elevated risk for a variety of chronic diseases and conditions, yet have rarely been targeted for tailored physical activity advice and support using communication sources (i.e., trained peer advisors, virtual advisors) that have great potential for population transferability and reach. The use of community centers for intervention delivery provides a readily available intervention access point in many communities across the U.S., and the one-year intervention period will provide insights related to initial physical activity adoption and more sustained behavioral maintenance. The multi-faceted recruitment plan allows for a more diverse and potentially generalizable sample, and the particularly high yield of the targeted mass mailings is notable, given its less frequent use in a number of community-based research studies. At least one study has shown that personalized direct mailings can increase response rates for Latino adults relative to nontargeted approaches [28]. The planned comparative cost analysis will provide additional information concerning the potential implementation of the two interventions in real-world contexts. This analysis will be essential for informing future dissemination of the novel Virtual Advisor intervention method. While community-based promotores de salud (i.e., lay or peer advisors) are a known and effective mechanism for health promotion in Latino populations, the method has been limited by the ability to scale. If the technology-enabled Virtual Advisor proves comparable and cost-sensitive relative to the Peer Advisor arm, it represents a scalable and replicable solution that could be readily integrated into current community and senior center infrastructures.
While the primary aim of this trial is to compare the 12-month effectiveness of the Virtual Advisor relative to Peer Advisors, a similarly compelling goal is to explore, through the planned moderator analyses, which participant subgroups may do best with which type of intervention. Referred to as “the whiches conundrum” [102–104], ascertaining how best to target different interventions to different subgroups of people represents among the most important challenges currently facing the behavioral health and precision medicine fields [102]. Similarly, the planned mediator analyses will provide initial information on which types of variables may be of particular importance for achieving intervention-related impacts on physical activity levels.
5. Conclusion
If the promising preliminary Virtual Advisor evidence obtained from the original pilot study [22] is confirmed in this comparative effectiveness trial, this intervention will represent a potentially low-cost, readily accessible option that could be broadly disseminated across a range of community settings (e.g., clinics, pharmacies, libraries, residential settings). As such, it has substantial potential to reduce the health disparities gap by influencing a key health behavior in underserved populations [105].
Acknowledgments
This investigation was supported by Public Health Service Grant 5R01HL116448 from the National Heart, Lung, and Blood Institute awarded to Dr. King. Dr. King also received partial support from US Public Health Service Grant 1U54EB020405 supporting the National Center for Mobility Data Integration and Insight (PI: S Delp). Dr. Hauser received support from National Institutes of Health training grant 5T32HL007034-39 (PI: C. Gardner).
We gratefully acknowledge the assistance and support of the study peer advisors, the participants, staff, and volunteers of participating community centers in Santa Clara and San Mateo Counties, CA, and the following individuals in project activities or methods input: Betsy Barrera, Gustavo Chavez, Ana Cortes, Michele Escobar, Darlyne Esparza, Lidya Esparza-Rivera, Martha Gabaray, Ruby Gonzalez, John Ioannidis, MD, PhD, Alan Moreno, Cain Murguía, Randall Stafford, MD, PhD, Selene Virgen, and Sandra Winter, PhD from Stanford University School of Medicine; and Ha Trinh and Langxuan (James) Yin from Northeastern University.
The above funding sources had no involvement in the described research, including research development, execution, analysis, interpretation of results, and write-up and submission of this paper's content and results.
Footnotes
Competing interests
The authors report no competing or conflicts of interest.
Authors' contributions
AK: Conceived of study investigation and design, obtained funding to support the research, contributed to study methods development and implementation, provided general study oversight, contributed to analysis and interpretation of results, and took the lead in writing the manuscript.
IC: Contributed to study methods development and implementation, data collection, project management and quality assurance, study-related community outreach, data management and interpretation of results, edited the manuscript and approved the final version of the manuscript.
JS: Contributed to study methods development and implementation, study-related community outreach and recruitment, data collection and interpretation of results, edited the manuscript and approved the final version of the manuscript.
CCS: Contributed to conception of study design, collaborated in obtaining funding to support the research, contributed to study methods development, management, and implementation, edited the manuscript and approved final version of the manuscript.
DG: Contributed to study methods development, implementation, data collection and quality control, edited the manuscript and approved the final version of the manuscript.
AC: Contributed to study methods development, implementation, and data collection, study-related community outreach and intervention management, edited the manuscript and approved the final version of the manuscript.
GB: Contributed to study methods development, implementation, and data collection, study-related community outreach and intervention management, edited the manuscript and approved final version of the manuscript.
MH: Contributed to study methods implementation and data collection, including medical oversight, and approved the final version of the manuscript.
FF: Contributed to study methods implementation and data collection, provided edits to the manuscript, and approved the final version of the manuscript.
DA: Data management, statistical analysis and interpretation, and approved the final manuscript.
JD: Contributed to study methods implementation and data collection, and approved the final version of the manuscript.
MD: Contributed to study methods implementation and data collection, and approved the final version of the manuscript.
JF: Contributed to study methods implementation and data collection, and approved final version of the manuscript.
TB: Contributed to conception of study investigation and design, contributed to study methods development and implementation, collaborated in obtaining funding to support the research, provided oversight of portions of data collection, edited the manuscript and approved the final version of the manuscript.
References
- 1.Lee IM, Shiroma EJ, Lobelo F et al. Effect of physical inactivity on major noncommunicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380(9838):219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pratt M, Macera CA, Wang G. Higher direct medical costs associated with physical inactivity. Phys. Sportsmed. 2000;28:63–70. doi: 10.3810/psm.2000.10.1237. [DOI] [PubMed] [Google Scholar]
- 3.Physical Activity Guidelines Advisory Committee. Report of the Physical Activity Guidelines Advisory Committee, 2008. U.S. Department of Health and Human Services; Washington, DC: 2008. [Google Scholar]
- 4.Pleis JR, Ward BW, Lucas JW. Summary Health Statistics for U.S. Adults: National Health Interview Survey, 2009. CDC; Atlanta, CA: 2010. [PubMed] [Google Scholar]
- 5.Livingston G, Minushkin S, Cohn D. Hispanics and Health Care in the United States: Access, Information and Knowledge. Pew Hispanic Center. 2008 [Google Scholar]
- 6.Silvia CA. Barriers to physical activity in the Hispanic community. J. Public Health Policy. 2003;24(1):41–58. [PubMed] [Google Scholar]
- 7.Vincent GK, Velkoff AK. The Older Population in the United States: 2010 to 2050. U.S. Census Bureau; Washington, DC: 2010. The Next Four Decades. [Google Scholar]
- 8.World Health Organization. The Community Health Worker, Office of Publications. World Health Organization; Geneva, Switzerland: 1990. [Google Scholar]
- 9.Eng E, Parker E, Harlan C. Health advisor interventions strategies: a continuum from natural helping to paraprofessional helping. Health Educ. Behav. 1997;24(4):510–522. doi: 10.1177/109019819702400402. [DOI] [PubMed] [Google Scholar]
- 10.Love MB, Gardner K, Legion V. Community health workers: who they are and what they do. Health Educ. Behav. 1997;24(4):510–522. doi: 10.1177/109019819702400409. [DOI] [PubMed] [Google Scholar]
- 11.Ayala GX, Vaz L, Earp JA, Elder JP, Cherrington A. Outcome effectiveness of the lay health advisor model among Latinos in the United States: an examination by role. Health Educ. Res. 2010;25(5):815–840. doi: 10.1093/her/cyq035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Viswanathan M, Kraschnewski J, Nishikawa B, et al. Outcomes of Community Health Work Interventions. Evidence Report. Agency for Healthcare Research and Quality; Rockville, MD: Jun, 2009. (Technology Assessment No. 181) [Google Scholar]
- 13.Vega WA, González HM. Latinos “aging in place”: issues and potential solutions. In: Angel JL, Torres-Gil F, Markides K, editors. Aging, Health, and Longevity in the Mexican-Origin Population. Springer; New York, NY: 2012. pp. 193–205. [Google Scholar]
- 14.Viswanath K, Kreuter MW. Health disparities, communication inequalities, and eHealth. Am. J. Prev. Med. 2007;32(5 Suppl):S131–133. doi: 10.1016/j.amepre.2007.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glasgow RE. eHealth evaluation and dissemination research. Am. J. Prev. Med. 2007;32(5 Suppl):S119–126. doi: 10.1016/j.amepre.2007.01.023. [DOI] [PubMed] [Google Scholar]
- 16.Norman CD, Skinner HA. eHealth Literacy: essential skills for consumer health in a networked world. J. Med. Internet Res. 2006;8(2):e9. doi: 10.2196/jmir.8.2.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Norman GJ, Zabinski MF, Adams MA, Rosenberg DE, Yaroch AL, Atienza AA. A review of eHealth interventions for physical activity and dietary behavior change. Am. J. Prev. Med. 2007;33(4):336–345. doi: 10.1016/j.amepre.2007.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Curry SJ. eHealth research and healthcare delivery beyond intervention effectiveness. Am. J. Prev. Med. 2007;32(5 Suppl):S127–130. doi: 10.1016/j.amepre.2007.01.026. [DOI] [PubMed] [Google Scholar]
- 19.Livingston G. The Latino Digital Divide: The Native Born Versus the Foreign Born. Pew Research Center; Washington, DC: Jul 28, 2010. [Google Scholar]
- 20.Kreuter MW, McClure SM. The role of culture in health communication. Annu. Rev. Public Health. 2004;25:439–455. doi: 10.1146/annurev.publhealth.25.101802.123000. [DOI] [PubMed] [Google Scholar]
- 21.Cardelle AJF, Rodriguez EG. The quality of Spanish health information websites: an emerging disparity. J. Prev. Interv. Community. 2005;29:85–102. [Google Scholar]
- 22.King AC, Bickmore TW, Campero MI, Pruitt LA, Yin JL. Employing “virtual advisors” in preventive care for underserved communities: results from the COMPASS study. J. Health Commun. Int. Perspect. 2013;18(12):1449–1464. doi: 10.1080/10810730.2013.798374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murphy MH, Nevill AM, Murtagh EM, Holder RL. The effect of walking on fitness, fatness and resting blood pressure: a meta-analysis of randomised, controlled trials. Prev. Med. 2007;44(5):377–385. doi: 10.1016/j.ypmed.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 24.U.S. Census Bureau, U.S. 2010 Census Data. [Accessed December 3, 2011];Census Summary File 1. 2011 Available at http://2010.census.gov/2010census/data/
- 25.Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS Physical Activity Questionnaire for older adults: outcomes for interventions. Med. Sci. Sports Exerc. 2001;33(7):1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Thomas S, Reading J, Shephard RJ. Revision of the Physical Activity Readiness Questionnaire (PAR-Q) Can. J. Sports Sci. 1992;17:338–345. [PubMed] [Google Scholar]
- 27.King AC, Harris RB, Haskell WL. Effect of recruitment strategy on types of subjects entered into a primary prevention clinical trial. Ann. Epidemiol. 1994;4:312–320. doi: 10.1016/1047-2797(94)90087-6. [DOI] [PubMed] [Google Scholar]
- 28.Kiernan M, Phillips K, Fair JM, King AC. Using direct mail to recruit Hispanic adults into a dietary intervention: an experimental study. Ann. Behav. Med. 2000;22(1):89–93. doi: 10.1007/BF02895172. [DOI] [PubMed] [Google Scholar]
- 29.Brown SD, Lee K, Schoffman DE, King AC, Crawley LM, Kiernan M. Minority recruitment into clinical trials: experimental findings and practical implications. Contemp. Clin. Trials. 2012;33(4):620–623. doi: 10.1016/j.cct.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Soto J, Campero MI, Castro CM, King AC. Lessons from recruiting Latino older adults into the LIFE trial; Society of Behavioral Medicine 33rd Annual Meeting and Scientific Sessions: Rapid Communications; April 13, 2012; New Orleans, LA. [Google Scholar]
- 31.Goldberg JH, Kiernan M. Innovative techniques to address retention in a behavioral weight-loss trial. Health Educ. Res. 2005;20(4):439–447. doi: 10.1093/her/cyg139. [DOI] [PubMed] [Google Scholar]
- 32.Castro CM, Pruitt LA, Buman MP, King AC. Physical activity program delivery by professionals versus volunteers: the TEAM randomized trial. Health Psychol. 2011;30(3):285–294. doi: 10.1037/a0021980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wilcox S, Dowda M, Griffin SF, et al. Results of the first year of active for life: translation of two evidence-based physical activity programs for older adults into community settings. Am. J. Public Health. 2006;96:1201–1209. doi: 10.2105/AJPH.2005.074690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Griffin SF, Wilcox S, Ory MG, et al. Results from the active for life process evaluation: program delivery fidelity and adaptations. Health Educ. Res. 2010;25(2):325–342. doi: 10.1093/her/cyp017. [DOI] [PubMed] [Google Scholar]
- 35.King AC, Haskell WL, Taylor CB, Kraemer HC, DeBusk RF. Group- vs home-based exercise training in healthy older men and women. A community-based clinical trial. JAMA. 1991;266(11):1535–1542. [PubMed] [Google Scholar]
- 36.King AC, Friedman RM, Marcus BH et al. Ongoing physical activity advice by humans versus computers: the Community Health Advice by Telephone (CHAT) Trial. Health Psychol. 2007;26:718–727. doi: 10.1037/0278-6133.26.6.718. [DOI] [PubMed] [Google Scholar]
- 37.King AC, Castro CM, Buman MP, Hekler EB, Urizar G, Ahn DG. Behavioral impacts of sequentially versus simultaneously delivered dietary plus physical activity interventions: the CALM Trial. Ann. Behav. Med. 2013;46(2):157–168. doi: 10.1007/s12160-013-9501-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wilcox S, Dowda M, Leviton LC, et al. Active for Life: final results from the translation of two physical activity programs. Am. J. Prev. Med. 2008;35(4):340–351. doi: 10.1016/j.amepre.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 39.Bandura A. Social cognitive theory: an agentic perspective. Annu. Rev. Psychol. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 40.Marshall SJ, Biddle SJH. The transtheoretical model of behavior change: a meta-analysis of applications to physical activity and exercise. Ann. Behav. Med. 2001;23:229–246. doi: 10.1207/S15324796ABM2304_2. [DOI] [PubMed] [Google Scholar]
- 41.King AC. Interventions to promote physical activity in older adults. J. Gerontol. Biol. Sci. Med. Sci. 2001;56A(Special Issue II):36–46. doi: 10.1093/gerona/56.suppl_2.36. [DOI] [PubMed] [Google Scholar]
- 42.Bickmore T, Caruso L, Clough-Gorr K, Heeren T. ‘It's just like you talk to a friend’ - relational agents for older adults. Interact. Comput. 2005;17:711–735. [Google Scholar]
- 43.Bickmore T, Gruber A, Picard R. Establishing the computer-patient working alliance in automated health behavior change interventions. Patient Educ. Couns. 2005;59:21–30. doi: 10.1016/j.pec.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 44.Bickmore T, Pfeifer LM, Byron D, et al. Usability of conversational agents by patients with inadequate health literacy: evidence from two clinical trials. J. Health Commun. 2010;15(Suppl. 2):197–210. doi: 10.1080/10810730.2010.499991. [DOI] [PubMed] [Google Scholar]
- 45.Castro CM, Pruitt LA, French SH, Cassayre CL, King AC. Successful peer mentoring for physical activity: 12-month results of the TEAM trial. Ann. Behav. Med. 2008;35:S081. [Google Scholar]
- 46.Holbrook EA, Barreira TV, Kang M. Validity and reliability of Omron pedometers for prescribed and self-paced walking. Med. Sci. Sports Exerc. 2009;41(3):669–673. doi: 10.1249/MSS.0b013e3181886095. [DOI] [PubMed] [Google Scholar]
- 47.Umstattd MR, Wilcox S, Saunders R, Watkins K, Dowda M. Self-regulation and physical activity: the relationship in older adults. Am. J. Health Behav. 2008;32(2):115–124. doi: 10.5555/ajhb.2008.32.2.115. [DOI] [PubMed] [Google Scholar]
- 48.King AC, Sallis JF, Dunn AL, et al. Overview of the Activity Counseling Trial (ACT) intervention for promoting physical activity in primary care settings. Med. Sci. Sports Exerc. 1998;30:1086–1096. doi: 10.1097/00005768-199807000-00011. [DOI] [PubMed] [Google Scholar]
- 49.Hekler EB, Buman MP, Dunton GF, Atienza AA, King AC. Are daily fluctuations in perceived environment associated with walking after controlling for implementation intentions? Psychol. Health. 2012;27(9):1009–1020. doi: 10.1080/08870446.2011.645213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pahor M, Guralnik JM, Ambrosius WT, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE Study Randomized Clinical Trial. JAMA. 2014;311(23):2387–2396. doi: 10.1001/jama.2014.5616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Harada ND, Chiu V, King AC, Stewart AL. An evaluation of three self-report physical activity instruments for older adults. Med. Sci. Sports Exerc. 2001;33:962–970. doi: 10.1097/00005768-200106000-00016. [DOI] [PubMed] [Google Scholar]
- 53.Hekler EB, Buman MP, Haskell WL, et al. Reliability and validity of CHAMPS self-reported sedentary to vigorous intensity physical activity in older adults. J. Phys. Act. Health. 2012;9:225–236. doi: 10.1123/jpah.9.2.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Feito Y, Bassett DR, Thompson DL. Evaluation of activity monitors in controlled and free-living environments. Med. Sci. Sports Exerc. 2011;44(4):733–741. doi: 10.1249/MSS.0b013e3182351913. [DOI] [PubMed] [Google Scholar]
- 55.King AC, Sallis JF, Frank LD, et al. Aging in neighborhoods differing in walkability and income: associations with physical activity and obesity in older adults. Soc. Sci. Med. 2011;73:1525–1533. doi: 10.1016/j.socscimed.2011.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hart TL, Swartz AM, Cashin SE, Strath SJ. How many days of monitoring predict physical activity and sedentary behaviour in older adults? Int. J. Behav. Nutr. Phys. Act. 2011;8:62–68. doi: 10.1186/1479-5868-8-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Choi L, Liu Z, Matthews CE, Buchowski MS. Validation of accelerometer wear and nonwear time classification algorithm. Med. Sci. Sports Exerc. 2011;43(2):357–364. doi: 10.1249/MSS.0b013e3181ed61a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rejeski WJ, Marsh AP, Brubaker PH, et al. Analysis and interpretation of accelerometry data in older adults: the LIFE Study. J. Gerontol. A Biol. Sci. Med. Sci. 2016;71(4):521–528. doi: 10.1093/gerona/glv204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gardiner PA, Clark BK, Healy GN, Eakin EG, Winkler EAH, Owen N. Measuring older adults' sedentary time: reliability, validity, and responsiveness. Med. Sci. Sports Exerc. 2017;43(11):2127–2133. doi: 10.1249/MSS.0b013e31821b94f7. [DOI] [PubMed] [Google Scholar]
- 60.Rikli RE, Jones CJ. Development and validation of a functional fitness test for community-residing older adults. J. Aging Phys. Act. 1999;7:129–161. [Google Scholar]
- 61.Myers AM, Malott OW, Gray E, et al. Measuring accumulated health-related benefits of exercise participation for older adults: the Vitality Plus Scale. J. Gerontol. Ser. A Biol. Med. Sci. 1999;54A:M456–M466. doi: 10.1093/gerona/54.9.m456. [DOI] [PubMed] [Google Scholar]
- 62.Delcourt MAB, Kinzie MB. Attitudes Toward Computer Technologies (ACT) and Self-efficacy for Computer Technologies (SCT) McGill University; Montreal, Quebec, Canada: 1990. [Google Scholar]
- 63.Yin L, Bickmore T, Cortes D. The impact of linguistic and cultural congruity on persuasion by conversational agents; Proceedings of the 10th Intelligent Virtual Agents Conference (IVA); 2010; Philadelphia, PA. [Google Scholar]
- 64.Horvath A, Greenberg L. Development and validation of the Working Alliance Inventory. J. Couns. Psychol. 1989;36(2):223–233. [Google Scholar]
- 65.Anderson-Bill ES, Winett RA, Wojcik JR. Social cognitive determinants of nutrition and physical activity among web-health users enrolling in an online intervention: the influence of social support, self-efficacy, outcome expectations, and self-regulation. J. Med. Internet Res. 2011;13(1):e28. doi: 10.2196/jmir.1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hekler E, Buman M, Otten J, et al. Who responds better to computer-delivered vs. human-delivered physical activity intervention? Ann. Behav. Med. 2011;40 (abstract) [Google Scholar]
- 67.Kluger AN, Adler S. Person- versus computer-mediated feedback. Comput. Hum. Behav. 1993;9:1–16. [Google Scholar]
- 68.Murphy JW, Pardeck JT. Technology and language use: implications for computer mediated therapy. J. Humanist. Psychol. 1988;28:120–134. [Google Scholar]
- 69.Varela RE, Vernberg EM, Sanchez-Sosa JJ, Riveros A, Mitchell M, Mashunkashey J. Anxiety reporting and culturally associated interpretation biases and cognitive schemas: a comparison of Mexican, Mexican American, and European American families. J. Clin. Child Adolesc. Psychol. 2004;33(2):237–247. doi: 10.1207/s15374424jccp3302_4. [DOI] [PubMed] [Google Scholar]
- 70.Nass C, Moon Y. Machines and mindlessness: Social responses to computers. J. Soc. Issues. 2000;56:81–103. [Google Scholar]
- 71.Karabenick SA, Knapp JR. Effects of computer privacy on help seeking. J. Appl. Soc. Psychol. 1988;16:461–472. [Google Scholar]
- 72.King AC, Satariano WA, Marti J, Zhu W. Multilevel modeling of walking behavior: advances in understanding the interactions of people, place, and time. Med. Sci. Sports Exerc. 2008;40(7 Suppl):S584–593. doi: 10.1249/MSS.0b013e31817c66b7. [DOI] [PubMed] [Google Scholar]
- 73.King AC. The Individual and Physical Activity Promotion: Harnessing the Social and Built Environments. OBSSR, NIH; Bethesda, MD: Jun 21, 2006. [Google Scholar]
- 74.Fenigstein A, Scheier MF, Buss AH. Public and private self-consciousness: assessment and theory. J. Consult. Clin. Psychol. 1975;43:522–527. [Google Scholar]
- 75.Rainer RK, Miller MD. An assessment of the psychometric properties of the Computer Attitude Scale. Comput. Hum. Behav. 1996;12(1):93–105. [Google Scholar]
- 76.Brown SC, Mason CA, Perrino T, et al. Built environment and physical functioning in Hispanic elders: the role of “Eyes on the Street”. Environ. Health Perspect. 2008;116:1300–1307. doi: 10.1289/ehp.11160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Martinez SM, Ayala GX, Patrick K, Arredondo EM, Roesch S, Elder J. Associated pathways between neighborhood environment, community resource factors, and leisure-time physical activity among Mexican-American adults in San Diego, California. Am. J. Health Promot. 2012;26(5):281–288. doi: 10.4278/ajhp.100722-QUAN-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 79.Marin G, Sabogal F, Marin B, Otero-Sabogal R, Perez-Stable E. Development of a short acculturation scale for Hispanics. Hisp. J. Behav. Sci. 1987;9:183–205. [Google Scholar]
- 80.Lee SYD, Bender DE, Ruiz RE, Choi YI. Development of an easy-to-use Spanish health literacy test. Health Serv. Res. 2006;41:1392–1412. doi: 10.1111/j.1475-6773.2006.00532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam. Med. 1993;25(6):391–395. [PubMed] [Google Scholar]
- 82.Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev. Med. 1987;16:825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 83.Napolitano MA, Papandonatos GD, Lewis BA, et al. Mediators of physical activity behavior change: a multivariate approach. Health Psychol. 2008;27(4):409–418. doi: 10.1037/0278-6133.27.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mero NP, Guidice RM, Werner S. A field study of the antecedents and performance consequences of perceived accountability. J. Manag. 2012 [Google Scholar]
- 85.Kaul S, Diamond GA. Good enough: a primer on the analysis and interpretation of noninferiority trials. Ann. Intern. Med. 2006;145(1):62–69. doi: 10.7326/0003-4819-145-1-200607040-00011. [DOI] [PubMed] [Google Scholar]
- 86.Albright CL, Pruitt L, Castro C, Gonzalez A, Woo S, King AC. Modifying physical activity in a multiethnic sample of low-income women: one-year results from the IMPACT (Increasing Motivation for Physical ACTivity) project. Ann. Behav. Med. 2005;30(3):191–200. doi: 10.1207/s15324796abm3003_3. [DOI] [PubMed] [Google Scholar]
- 87.Gibbons RD, Hedeker D, Waternaux C, Kraemer HC, Greenhouse JB. Some conceptual and statistical issues in the analysis of longitudinal psychiatric data. Arch. Gen. Psychiatry. 1993;50:739–750. doi: 10.1001/archpsyc.1993.01820210073009. [DOI] [PubMed] [Google Scholar]
- 88.Laird N, Lange N, Stram D. Maximum likelihood computations with repeated measures: application. J. Am. Stat. Assoc. 1987;82:97–105. [Google Scholar]
- 89.Kraemer HC, Blasey C. Statistical Power Analysis in Research. 2. Sage Publications, Inc; Los Angeles: 2016. How Many Subjects? [Google Scholar]
- 90.Tate DF, Finkelstein EA, Khavjou O, Gustafson A. Cost effectiveness of internet interventions: review and recommendations. Ann. Behav. Med. 2009;38:40–45. doi: 10.1007/s12160-009-9131-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.U.S. Department of Health and Human Services. HHS Action Plan to Reduce Racial and Ethnic Disparities: A Nation Free of Disparities in Health and Health Care. USDHHS; Washington, DC: Apr, 2011. [Google Scholar]
- 92.Roux L, Pratt M, Tengs TO, et al. Cost effectiveness of community-based physical activity interventions. Am. J. Prev. Med. 2008;35(6):578–588. doi: 10.1016/j.amepre.2008.06.040. [DOI] [PubMed] [Google Scholar]
- 93.Sevick MA, Dunn AL, Morrow MS, Marcus BH, Chen GJ, Blair SN. Cost-effectiveness of lifestyle and structured exercise interventions in sedentary adults: results of project ACTIVE. Am. J. Prev. Med. 2000;19(1):1–8. doi: 10.1016/s0749-3797(00)00154-9. [DOI] [PubMed] [Google Scholar]
- 94.Thomas KS, Miller P, Doherty M, Muir KR, Jones AC, O'Reilly SC. Costeffectiveness of a two-year home exercise program for the treatment of knee pain. Arthritis Rheum. 2005;53(3):388–394. doi: 10.1002/art.21173. [DOI] [PubMed] [Google Scholar]
- 95.Warner KE, Luce BR. Practice, and Potential. Health Administration Press; Ann Arbor: 1982. Cost-benefit and Cost-effectiveness Analyses in Health Care: Principles. [Google Scholar]
- 96.Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch. Gen. Psychiatry. 2002;59:887–893. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 97.Rosenthal R, Rosnow RL. Essentials of Behavioral Research: Methods and Data Analysis. 2. McGraw-Hill; New York: 1991. [Google Scholar]
- 98.Buman MP, Hekler EB, Bliwise DL, King AC. Moderators and mediators of exercise-induced objective sleep improvements in midlife and older adults with sleep complaints. Health Psychol. 2011;30(5):579–587. doi: 10.1037/a0024293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 100.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu. Rev. Psychol. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Preacher K, Hayes A. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 102.King AC. Behavioral medicine in the 21st century: transforming “The Road Less Traveled” into the “American Way of Life”. Ann. Behav. Med. 2014;47(1):71–78. doi: 10.1007/s12160-013-9530-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.King AC, Ahn DF, Atienza AA, Kraemer HC. Exploring refinements in targeted behavioral medicine intervention to advance public health. Ann. Behav. Med. 2008;35(3):251–260. doi: 10.1007/s12160-008-9032-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hekler EB, Buman MP, Otten J, et al. Determining who responds better to a computer- vs. human-delivered physical activity intervention: results from the community health advice by telephone (CHAT) trial. Int. J. Behav. Nutr. Phys. Act. 2013;10:109–118. doi: 10.1186/1479-5868-10-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Munoz RF. Using evidence-based internet interventions to reduce health disparities worldwide. J. Med. Internet Res. 2010;12(5):e60. doi: 10.2196/jmir.1463. [DOI] [PMC free article] [PubMed] [Google Scholar]