Abstract
Objectives
In order to address acetabular defects, porous metal revision acetabular components and augments have been developed, which require fixation to each other. The fixation technique that results in the smallest relative movement between the components, as well as its influence on the primary stability with the host bone, have not previously been determined.
Methods
A total of 18 composite hemipelvises with a Paprosky IIB defect were implanted using a porous titanium 56 mm multihole acetabular component and 1 cm augment. Each acetabular component and augment was affixed to the bone using two screws, while the method of fixation between the acetabular component and augment varied for the three groups of six hemipelvises: group S, screw fixation only; group SC, screw plus cement fixation; group C, cement fixation only. The implanted hemipelvises were cyclically loaded to three different loading maxima (0.5 kN, 0.9 kN, and 1.8 kN).
Results
Screw fixation alone resulted in up to three times more movement (p = 0.006), especially when load was increased to 100% (p < 0.001), than with the other two fixation methods (C and SC). No significant difference was noted when a screw was added to the cement fixation. Increased load resulted in increased relative movement between the interfaces in all fixation methods (p < 0.001).
Conclusion
Cement fixation between a porous titanium acetabular component and augment is associated with less relative movement than screw fixation alone for all implant interfaces, particularly with increasing loads. Adding a screw to the cement fixation did not offer any significant advantage. These results also show that the stability of the tested acetabular component/augment interface affects the stability of the construct that is affixed to the bone.
Cite this article: N. A. Beckmann, R. G. Bitsch, M. Gondan, M. Schonhoff, S. Jaeger. Comparison of the stability of three fixation techniques between porous metal acetabular components and augments. Bone Joint Res 2018;7:282–288. DOI: 10.1302/2046-3758.74.BJR-2017-0198.R1.
Keywords: Revision hip arthroplasty, Hip arthroplasty, Acetabular revision, Primary stability, Porous metal
Article focus
Does fixation between acetabular component and augment affect overall construct stability?
How do fixation methods between acetabular component and augment differ in stability?
Key messages
The stability of the acetabular component/augment interface affects the stability of the entire construct.
Screw fixation is less stable than cement or screw plus cement fixation.
Strengths and limitations
This is an in vitro study with a limited sample size.
Clinical confirmation of the measured results may be necessary.
Introduction
In revision hip arthroplasty, the surgeon is frequently confronted with deficient bone stock, necessitating reconstruction of the acetabular bone. The use of large structural allografts has mixed results,1,2 with loosening and migration rates of up to 70% reported.3 The subsequent introduction of metal cages has reduced the loosening rate to 14% for larger defects (Paprosky IIIA and IIIB) when followed for a mean of 6.3 years.4 More recently, porous metals have been used for the treatment of these defects,5-7 and consist of acetabular components and augments, with either a porous tantalum surface (Trabecular Metal; Zimmer Biomet, Warsaw, Indiana) or a porous titanium surface (Gription; DePuy Synthes, West Chester, Pennsylvania). Trabecular metal (TM) is most often used, and TM components have led to a further decrease in the loosening rate to 2.5% at 3.7 years’ follow-up.4 It is believed that the advantage of porous metals with press-fit implantation is the provision of a stable mechanical interface between the implant surface and native bone in the short term (primary stability) and osseointegration in the mid and long term.7 Optimal primary stability requires minimal relative movement at bone/component interfaces, and previous studies have shown that successful osseointegration occurs at up to 40 µm relative movement, with fibrous attachment occurring at 150 µm relative movement.8,9 Minimal relative movement is a critical factor in success, and with increased numbers of interfaces, there is potential for increased relative movement. Although osseointegration only occurs at bone interfaces, relative movement of the acetabular component/augment interface can potentially affect the stability of the construct as a whole, particularly if it results in progressive particle shedding that is associated with loosening of the prosthesis and failure.6 To minimize this risk, it is important that a stable fixation is achieved between the metal-to-metal surfaces of the acetabular component and augment. There are few studies that evaluate the stability of the acetabular component/augment interface, and we know of only one study that evaluates the stability of the cement/porous metal interface.10 Cement-only, screw-only, and a combination of cement and screw are the fixation methods currently used at the acetabular component/augment interface. The aim of this study is to determine which of the three possible fixation techniques provide the most stable bond between the porous titanium acetabular component and augment, and to assess how the fixation affects the stability of the construct as a whole.
Material and Methods
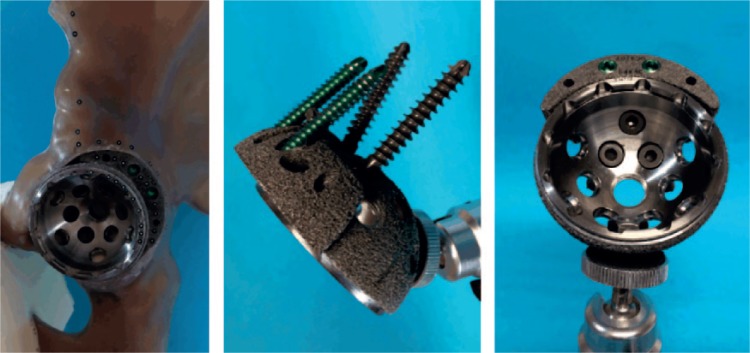
To evaluate the primary stability between a porous metal acetabular component and a porous metal augment, we utilized titanium acetabular components and augments (Pinnacle Multi-Hole Cup with Gription surface plus Gription augment; DePuy Synthes). All acetabular components were size 56 mm, with the corresponding 54/56 × 1 cm augment. A total of 18 large fourth-generation composite left hemipelvises (#3405 Sawbones; Sawbones Europe AB, Malmö, Sweden) were divided into three groups of six after sample size estimation. Sample size estimation was done using G*Power 3.1 Software (Heinrich-Heine-University, Düsseldorf, Germany),11 using a Mann–Whitney U test for two groups with an expected effect size of d = 2.5 and α = 0.05, with power (1-β) = 0.8; these values were based on the high level of standardization of the experiment and laboratory experience, as well as the literature.12 Each group had a different fixation method: C, cement-only fixation between acetabular component and augment (without an additional screw); S, screw-only fixation between acetabular component and augment, utilizing one 6.5 mm × 15 mm screw; SC, screw plus cement fixation between acetabular component and augment, utilizing one 6.5 mm × 15 mm screw plus cement. Prior to component implantation, a grade IIB Paprosky defect (i.e. a segmental defect of less than one-third of the acetabular circumference) of 1 cm thickness was created in a standardized fashion in each of the composite bones at the posterocranial aspect of the acetabulum, with the edge of the defect adjacent to the anterior-inferior iliac spine. To do this, the defect borders were marked on the Sawbone pelvis prior to implantation, then subsequently created by burring and reaming out the defect until it was the appropriate size. The acetabular component/augment constructs were subsequently implanted in a standardized fashion by an experienced orthopaedic surgeon (RGB) according to the manufacturer's instructions, with the augments first fixed to the host composite bone using two 5.5 mm × 30 mm screws. In cases where cement was used, the cement was applied to the surface of the augment adjacent to the acetabular component prior to acetabular component implantation. The acetabular component was attached to the bone using 6.5 mm × 40 mm and 6.5 mm × 30 mm screws, with the screws directed towards the sacroiliac joint (Fig. 1). A press-fit implantation was attempted in all cases, although, given the rim defect, the fit created did not show the same tightness as with a comparable primary implantation without a rim defect.
Fig. 1.
Photographs demonstrating the acetabular component, augment, and screw fixation position.
A medium-viscosity bone cement (Palacos R + G pro; Heraeus Medical GmbH, Wehrheim, Germany) was used to fix groups SC and C. The cement was vacuum-mixed (Optivac Cement Mixing System; Zimmer Biomet, Warsaw, Indiana) and applied 120 seconds after the start of mixing. Cementing was performed under standardized room conditions with a mean room temperature of 20.1°C (sd 0.4) and mean humidity of 38.6% (sd 8.8). Cement was dispensed with a cement gun and modelled by hand onto the augment surface only. Approximately 1.5 cm3 of cement was applied to the surface of the augment adjacent to the acetabular component prior to acetabular component implantation. Care was taken to remove all excess cement from the multi-hole acetabular component. If screws were used, they were inserted before the end of the cement working phase was reached.
The implanted hemipelvises were secured along the sacral side of the ilium (Fig. 2) in a containment device using polyurethane foam (RenCast FC 53 A/B; Goessl + Pfaff GmbH, Karlskron, Germany). Separately, the symphysis was secured to a two-component casting resin block with an attached stainless-steel ball on the undersurface, which was placed on a metal plate (Fig. 3). This provides a two-point pelvic fixation, whereby the symphysis is only fixed in one degree of freedom to allow for multiplanar movement and rotation of the symphysis, in order to mimic a more physiological fixation, as has been described in previous studies (Fig. 3).13,14 Optical markers (uncoded passive white markers with a diameter of 0.8 mm, GOM Item Number: 21874; GOM Gmbh, Braunschweig, Germany) were placed along the rim of the acetabular component, augment, and composite bone in adjacent rows to allow for 3D discrimination and recording of relative movement between the components during loading (Fig. 4). These markers were detected in greyscale by a stereo camera system, and a 3D point triangulation was done to calculate the 3D marker position in the defined coordinate system. The 3D micromovements in x-, y-, and z-axes were measured simultaneously between acetabular component and bone, acetabular component and augment, and augment and bone using an optical measuring system (PONTOS; GOM GmbH), and resultant movements of the component augment, acetabular component, and bone were calculated using the formula . We tested each group (S, SC, and C) using a materials testing machine (MTS Mini Bionix 359; MTS Systems Corporation, Eden Prairie, Minnesota), with the load applied in the direction of greatest load occurring during normal gait, as identified by Bergmann et al.15,16 The maximum load during normal walking was shown to equate to 233% of the individual’s body weight at 31° of rotation around the x-axis and 5° around the z-axis relative to the acetabular component coordinate system described by Bergmann et al.17 We assumed a body weight of 80 kg for each specimen, which translates to 1.8 kN at 100% load. A total of 1000 cycles were applied in a sinusoidal waveform at 1 Hz at each of three load levels: 3% to 30% load (the equivalent of 0.5 kN); then 5% to 50% load (the equivalent of 0.9 kN); and, finally, at 10% to 100% load (1.8 kN). To ensure a good force closure between the force plate and the sample, 0.2 kN was applied prior to testing. For each loading level, a total of 3000 cycles were applied. The dependent variable was the relative movement between the components (measured in μm), measured at cycles 1 to 50, 51 to 200, 201 to 500, 501 to 800, and 801 to 995 (average and variance).
Fig. 2.
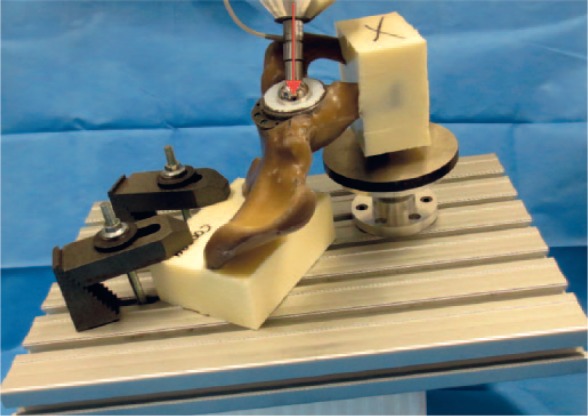
Photograph showing an example of test set-up. Fixation of the pubic and sacral sides of the hemipelvis using a casting resin, with the sacral side being held in a containment device during testing to allow for 3D fixation. The load was applied in the direction of maximal load, represented by the red arrow.
Fig. 3.
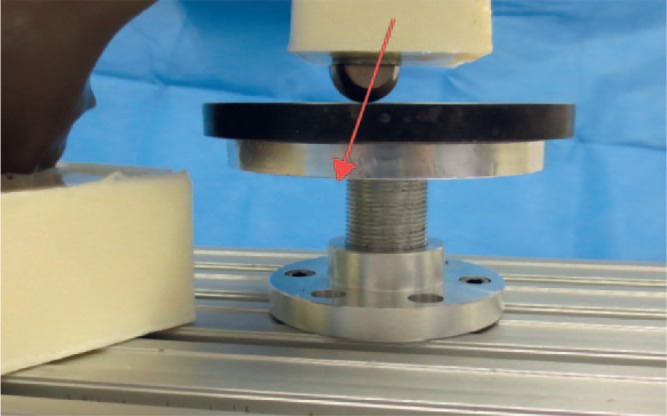
Photograph of the pubic fixation with a hemispherical ball attached. The symphysis was only fixed in one degree of freedom to allow for multiplanar movement and rotation of the symphysis, in order to mimic a more physiological fixation than a rigid fixation of the symphysis in all planes allows. The load direction is represented by the red arrow.
Fig. 4.
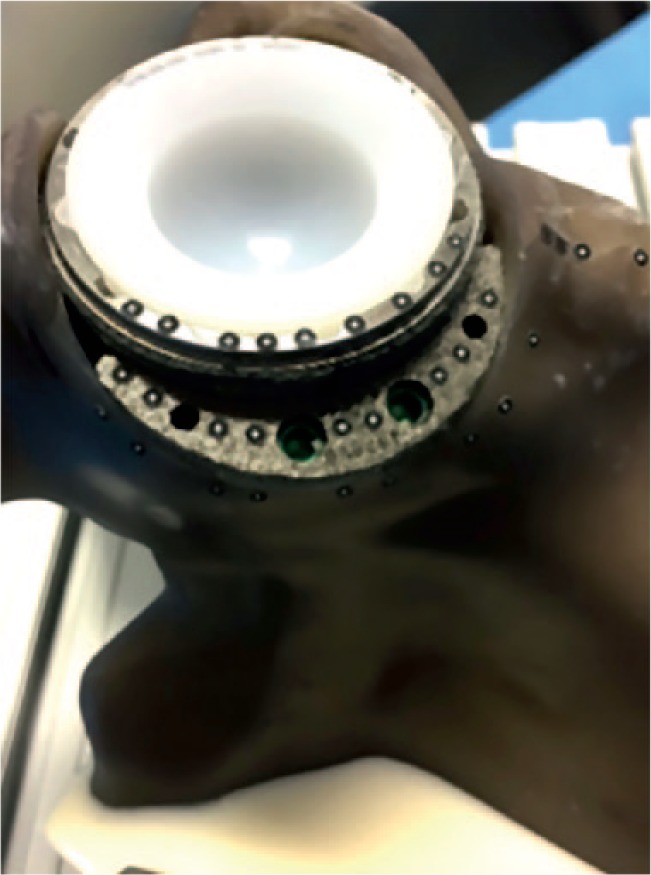
Photograph showing an example of optical marker placement on the adjacent surfaces of the respective components; all markers were placed in rows so that each marker had a corresponding marker on the adjacent component to allow for superior discrimination of movement.
Statistical analysis
The primary variable of interest was the relative movement between the components during loading (measured in µm). Separate analyses were carried out for the augment/acetabular component, bone/augment, and bone/acetabular component interface. The data were evaluated descriptively using the arithmetic mean, standard deviation, and range. We calculated a linear mixed model for the transformed relative movement (averaged over cycles, as described above, and weighted by the inverse variance of these samples). The Kenward–Roger approximation was used to correct the degrees of freedom in the unknown covariance matrix. Covariates were the fixation techniques (S, C, SC), force (30%, 50%, and 100% maximal load), and their interaction. Hemipelvis ID served as a random intercept, and post hoc comparisons between S/C, S/SC, and C/SC were performed using differences of ‘least-squares’ means.18 A two-tailed p-value ⩽ 0.05 was considered statistically significant. Statistical evaluation was performed using the R statistical programming language (R foundation for statistical computing, Vienna, Austria).
Results
Table I displays relative movement occurring at the three interfaces with increasing loads. For the augment/acetabular component interface, the least relative movement, and therefore the most stable fixation, was achieved with cement (around 11 µm, on average, independent of load). When cement and screws were used together, relative movement was only minimally increased compared with cement alone (around 12 µm, independent of load). However, screw fixation alone resulted in significantly more relative movement (F(2, 13.8) = 7.69, p = 0.006), especially when loading was increased to 100%, compared with other fixation methods, with average movement up to 31.4 µm at 100% load (F(4, 105.6) = 45.4, p < 0.001) (Fig. 5a).
Table I.
Augment/acetabular component, augment/bone, and acetabular component/bone relative movement (mean and standard deviation) in µm relative to fixation technique
| Fixation | Load (%) | Augment/acetabular component |
Augment/bone |
Acetabular component/bone |
|---|---|---|---|---|
| Mean relative movement, μm (sd, range) | Mean relative movement, μm (sd, range) | Mean relative movement, μm (sd, range) | ||
| Cement | 30 | 11.0 (1.9, 7.4 to 15.0) | 20.2 (7.3, 11.4 to 36.8) | 27.9 (8.1, 15.5 to 48.2) |
| 50 | 10.9 (2.2, 8.0 to 16.1) | 38.7 (19.2, 11.9 to 88.4) | 50.2 (21.0, 22.8 to 107.4) | |
| 100 | 11.3 (4.0, 6.8 to 20.9) | 84.3 (37.8, 26.9 to 142.0) | 107.2 (41.6, 47.7 to 173.7) | |
| Screw plus cement | 30 | 11.0 (3.2, 5.5 to 18.2) | 22.4 (10.6, 11.2 to 43.9) | 27.3 (15.1, 1.7 to 54.8) |
| 50 | 11.7 (3.5, 6.1 to 20.7) | 41.9 (22.2, 15.9 to 87.1) | 48.7 (30.8, 2.9 to 108.7) | |
| 100 | 12.6 (4.0, 7.8 to 21.5) | 79.9 (38.9, 24.2 to 135.1) | 91.9 (53.3, 14.1 to 165.4) | |
| Screw | 30 | 11.1 (2.3, 7.6 to 16.2) | 26.2 (18.0, 9.8 to 70.1) | 28.0 (12.6, 17.1 to 73.9) |
| 50 | 15.1 (4.6, 9.5 to 27.2) | 59.3 (41.0, 23.5 to 172.6) | 63.1 (37.2, 34.6 to 211.4) | |
| 100 | 31.4 (16.6, 12.4 to 55.3) | 151.1 (82.1, 60.0 to 297.3) | 170.3 (72.2, 99.6 to 325.3) |
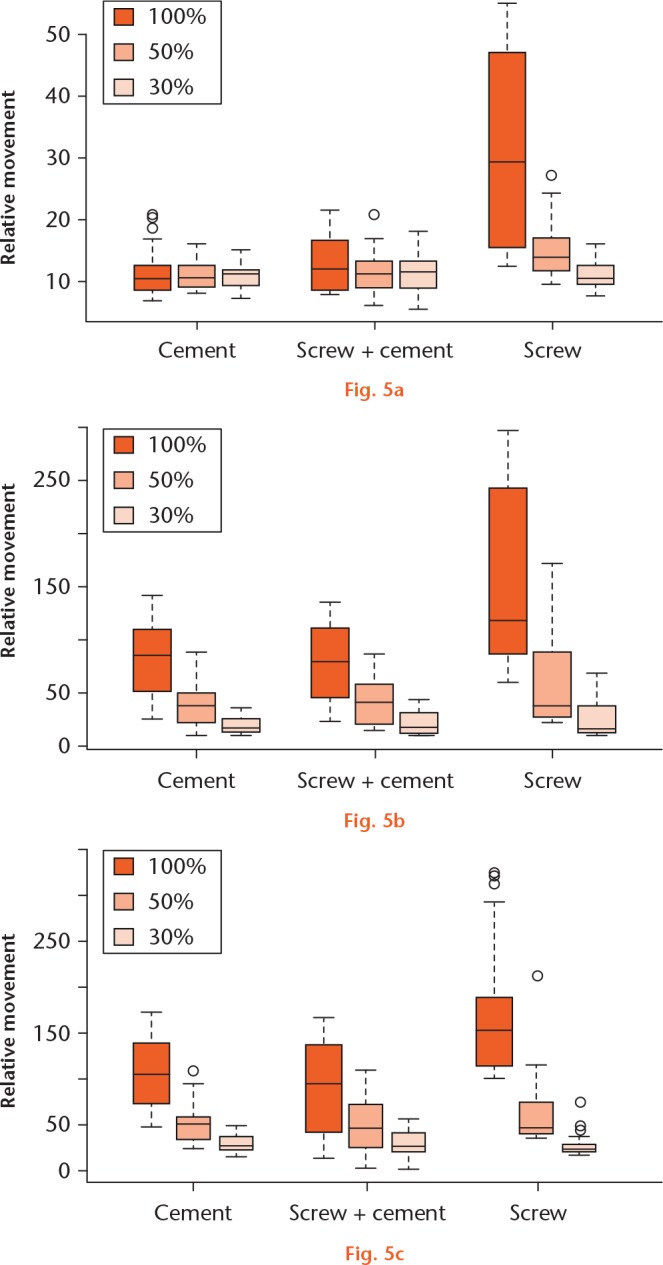
a) Graph showing relative movement in µm at the augment/acetabular component interface under different loads and fixations. Screw fixation alone resulted in significantly more relative movement under 100% load. b) Graph showing relative movement in µm at the bone/augment interface under different loads and fixations. Under full load, screw fixation alone resulted in significantly more relative movement. c) Graph showing relative movement in µm at the bone/component interface under different loads and fixations.
For the other two interfaces (augment/bone, acetabular component/bone; Table I, Figs 5b and 5c), relative movement was related to load for all fixation techniques (p < 0.001 for both interfaces). Overall, the fixation types were similar in stability (F < 1 for both interfaces), but under 100% load, screw fixations showed a substantial increase in relative movement (interaction F(4, 398) = 5.70, p < 0.001 for augment/bone, and F(4, 42) = 13.07, p < 0.001 for acetabular component/bone).
In summary, samples with screw fixation alone showed more relative movement than other samples at all interfaces, and relative movement increased with increasing load.
Discussion
The degree of relative movement occurring at all interfaces is an important element in determining the integrity of the primary stability and ultimately the successful osseointegration of the construct. Prior in vivo animal studies post-implant, and studies on human autopsy bones several months to years after implantation, have indicated that successful osseointegration occurs at up to 40 µm relative movement, with 150 µm relative movement resulting in fibrous attachment.8,9 Although these studies do not replicate the immediate postoperative scenario, these values for degree of relative movement have been widely quoted as significant because they underpin the importance of achieving minimal relative movement between bone and implant for osseointegration and surgical success. With an increasing number of bone and/or component interfaces, as occurs with the use of augments, it is reasonable to hypothesize that there is a correspondingly greater potential for increased relative movement. Therefore, the identification of the most stable method of fixation at this interface is important and contributes to the overall stability of the construct. In addition, increased relative movement is associated with the potential for progressive particulate debris that can result in loosening of the prosthesis and failure.6 To minimize this risk and to promote successful osseointegration, it is important to achieve stable fixation of acetabular component to the augment in addition to fixation of implant to bone. There have been a number of studies evaluating the stability of the acetabular component/bone interface, but we are aware of only one study that has evaluated the acetabular component/augment interface.10 Potential fixation methods between acetabular component and augment include screw, cement, or a combination of the two; the efficacy of these methods, to our knowledge, has not previously been reported.
The increased incidence of revision hip surgery has been accompanied by an increase in the use of porous metal acetabular components and augments that are implanted with a press-fit technique, and that are believed to improve primary stability and to promote rapid osseointegration. The porous metals that are currently most commonly used are tantalum (TM; Zimmer Biomet) and titanium (Gription; DePuy Synthes). The manufacturer of TM components has recommended the use of cement fixation between acetabular component and augment, but, as far as we are aware, there is no scientific data to support this. Other manufacturers have not recommended a particular fixation technique, and leave the choice to the surgeon.
Recent reports of revision surgeries using porous metals have overwhelmingly used porous tantalum components with cement fixation between acetabular component and augment, with good medium- and long-term results. Meneghini et al7 utilized porous tantalum acetabular components and porous tantalum buttress augments in eight patients with Paprosky IIIA and IIIB bone defects, and utilized cement fixation between acetabular component and augment. At a mean follow-up of 16.5 months (10 to 28), there was no loosening or reoperation. Abolghasemian et al6 reported on 38 patients with porous tantalum (TM) acetabular components and augments who were followed for a mean of 64.5 months. Cement fixation was used between acetabular component and augment. Three patients developed aseptic loosening, of whom two had prior Paprosky type IIIB defects (pelvic discontinuity). One patient died and two required re-revision surgery. Metal debris shedding was noted in early postoperative radiographs in eight patients, but was only progressive in two cases that ultimately failed.
Whitehouse et al5 reported on a series of 56 acetabular component/augment procedures, of which 53 were revisions; slightly more than two-thirds of the patients were Paprosky types IIIA or IIIB. The authors utilized TM shells and augments with only cement fixation in an unspecified number of cases that was less than the total number of cases on which they operated. They achieved a ten-year survival rate of the augments of 92%.
We have found only one study that utilized porous titanium acetabular components and augments in revision arthroplasty19. In 16 revision surgeries, 16 hemispherical modules (HM) of porous trabecular titanium were screwed to the acetabular bone and also screwed to the porous titanium acetabular component. Cement was not used for fixation. One of the 16 patients required re-revision surgery secondary to a fracture of the HM augment that occurred in the line of the screw holes. All implanted HM augments showed osseointegration.
Little information has been published on the negative aspects of porous implants. Porous implants are modular and combining the acetabular component with an augment will result in a further interface that may enable various types of implant failure. Minimal movement between the components, such as the augment and acetabular component, or between the screws and acetabular component or augment, may result in the production of metal debris. Adverse reactions to metal debris (ARMD) have not only been described in metal-on-metal (MoM) bearings, but also in non-MoM hip arthroplasties, often requiring revision arthroplasty.20,21 Fretting between the various construct components, corrosion, and polyethylene wear particles may also result and may accelerate failure, as has been described with other modular implants.22,23 Improved stability and minimized movement between the components may reduce these effects.
Our in vitro biomechanical study was designed specifically to examine and compare different methods of fixation at the interface between the porous metal acetabular component and the augment. We examined three methods of fixation of this interface, and measured the resultant relative movement occurring at the interface and relative movement of the acetabular component/bone and augment/bone, with different applied loads of 30%, 50%, and 100% of the normal weight-bearing sustained during the gait cycle, as described by Bergmann et al.15,16 Our study differs from previous studies in two aspects: the use of titanium components rather than the more widely used tantalum ones; and the examination and comparison of relative movement at the acetabular component/augment interface as an indicator of stability associated with three different methods of fixation.
Our results show that screws alone led to substantially more relative movement at all interfaces, particularly when load was increased from 30% to 100%. The screw/cement combination displayed slightly better results at the augment/bone and acetabular component/bone interfaces than cement alone, but only at 100% load; the difference was not statistically significant. Cement fixation alone performed better than screw/cement fixation at the acetabular component/augment interface, and showed very little change with increasing load; the difference was not statistically significant. Our results also demonstrated that the stability of the acetabular component/augment interface directly influenced the degree of relative movement recorded at the other interfaces, and therefore influenced the stability of the entire construct.
Our study has several limitations. The use of composite polyethylene blocks rather than cadaveric bone for acetabular component/augment implantation has the advantage of decreasing inter-specimen variability, but it is less physiological; Zech et al24 showed that synthetic bone has different biomechanical properties than cadaveric bone. We chose, however, not to use cadaveric bone because the specimens will vary substantially in bone density, not only from one donor to another, but also due to individual asymmetry. In addition, it has been shown that fixation is affected by the bone mineral density,25 and it is difficult to compensate for this in a three series setup.
Loads were applied to the specimens from 30% to 50% to 100% of the normal weight-bearing load during gait, but only in the direction of the greatest load that was identified by Bergmann et al,15,16 and therefore did not replicate the entire cyclical pattern of normal walking with loading on different areas of the acetabulum in differing degrees.
This study cannot provide any information as to the advantage of a porous implant over other implant types with other surface characteristics or fixation methods such as cementation.
The defects we created in the acetabular margin were at consistent position and of a uniform size, and were classified as a Paprosky IIB defect, in contrast to the variability of defects occurring in the clinical situation.
Finally, only one type of porous metal was tested (titanium), and we therefore strongly recommend additional studies using other porous metals under similar conditions. Different implants and implant materials may lead to alternative results, although we anticipate that the type of fixation between augment and acetabular component will have a similar impact on the stability of the implant construct irrespective of the type of porous metal.
Our study utilizing porous titanium components clearly demonstrates that cement fixation between acetabular component and augment resulted in less relative movement and is more stable than screw fixation. The combination of cement and screws does not provide any additional advantage. Differences in relative movement with the three fixation methods are most pronounced at the acetabular component/bone and augment/bone interfaces, and also with increasing load. These results indicate that stability of the acetabular component/augment interface affects the stability of the construct as a whole. The increased relative movement noted at the acetabular component/bone and augment/bone interfaces associated with increasing load is additional evidence of the need for limited weight-bearing in the early stages of postoperative recovery, as suggested by others in earlier studies.8,26
Footnotes
Author Contributions: N. A. Beckmann: Conception of the study, Collecting the data, Statistical analysis, Writing the manuscript.
R. G. Bitsch: Supervising the study, Writing and reviewing the manuscript.
M. Gondan: Statistical analysis, Writing the manuscript.
M. Schonhoff: Collecting and evaluating the data, Writing the manuscript.
S. Jaeger: Conception of the study, Collecting the data, Supervising the study, Writing and reviewing the manuscript.
Conflicts of Interest Statement: N. A. Beckmann reports grants from DePuy Synthes that are not related to the current study. R. G. Bitsch and S. Jaeger report grants from B Braun Aesculap, DePuy Synthes, Heraeus, Waldemar Link, and Zimmer Biomet that are not related to the current study.
Follow us @BoneJointRes
Funding Statement
Funding for this project was kindly provided by a research grant from the German Arthrosis Aid (Deutsche Arthrose-Hilfe e.V., Frankfurt/Main, Germany). We also acknowledge financial support by the Deutsche Forschungsgemeinschaft within the funding programme Open Access Publishing, by the Baden-Württemberg Ministry of Science, Research and the Arts, and by Ruprecht-Karls-Universität Heidelberg.
References
- 1. Garbuz D, Morsi E, Gross AE. Revision of the acetabular component of a total hip arthroplasty with a massive structural allograft. Study with a minimum five-year follow-up. J Bone Joint Surg [Am] 1996;78-A:693-697. [DOI] [PubMed] [Google Scholar]
- 2. Sporer SM, O'Rourke M, Chong P, Paprosky WG. The use of structural distal femoral allografts for acetabular reconstruction. Average ten-year follow-up. J Bone Joint Surg [Am] 2005;87-A:760-765. [DOI] [PubMed] [Google Scholar]
- 3. Pollock FH, Whiteside LA. The fate of massive allografts in total hip acetabular revision surgery. J Arthroplasty 1992;7:271-276. [DOI] [PubMed] [Google Scholar]
- 4. Beckmann NA, Weiss S, Klotz MC, et al. Loosening after acetabular revision: comparison of trabecular metal and reinforcement rings. A systematic review. J Arthroplasty 2014;29:229-235. [DOI] [PubMed] [Google Scholar]
- 5. Whitehouse MR, Masri BA, Duncan CP, Garbuz DS. Continued good results with modular trabecular metal augments for acetabular defects in hip arthroplasty at 7 to 11 years. Clin Orthop Relat Res 2015;473:521-527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Abolghasemian M, Tangsataporn S, Sternheim A, et al. Combined trabecular metal acetabular shell and augment for acetabular revision with substantial bone loss: a mid-term review. Bone Joint J 2013;95-B:166-172. [DOI] [PubMed] [Google Scholar]
- 7. Meneghini RM, Hull JR, Russo GS, Lieberman JR, Jiranek WA. Porous tantalum buttress augments for severe acetabular posterior column deficiency. Surg Technol Int 2015;27:240-244. [PubMed] [Google Scholar]
- 8. Pilliar RM, Lee JM, Maniatopoulos C. Observations on the effect of movement on bone ingrowth into porous-surfaced implants. Clin Orthop Relat Res 1986;208:108-113. [PubMed] [Google Scholar]
- 9. Engh CA, O'Connor D, Jasty M, et al. Quantification of implant micromotion, strain shielding, and bone resorption with porous-coated anatomic medullary locking femoral prostheses. Clin Orthop Relat Res 1992;285:13-29. [PubMed] [Google Scholar]
- 10. Beckmann NA, Bitsch RG, Seeger JB, et al. Mechanical properties of a cemented porous implant interface. Acta Orthop 2014;85:531-537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 2009;41:1149-1160. [DOI] [PubMed] [Google Scholar]
- 12. Stiehl JB, MacMillan E, Skrade DA. Mechanical stability of porous-coated acetabular components in total hip arthroplasty. J Arthroplasty 1991;6:295-300. [DOI] [PubMed] [Google Scholar]
- 13. Nie Y, Pei F, Li Z. Effect of high hip center on stress for dysplastic hip. Orthopedics 2014;37:e637-e643. [DOI] [PubMed] [Google Scholar]
- 14. Martin CT, Heiner AD, Baer TE, Pugely AJ, Noiseux NO. Protrusio after medial acetabular wall breach in total hip arthroplasty. Iowa Orthop J 2015;35:99-107. [PMC free article] [PubMed] [Google Scholar]
- 15. Bergmann G, Deuretzbacher G, Heller M, et al. Hip contact forces and gait patterns from routine activities. J Biomech 2001;34:859-871. [DOI] [PubMed] [Google Scholar]
- 16. Bergmann G, Graichen F, Rohlmann A, et al. Realistic loads for testing hip implants. Biomed Mater Eng 2010;20:65-75. [DOI] [PubMed] [Google Scholar]
- 17. Bergmann G, Bender A, Dymke J, Duda G, Damm P. Standardized loads acting in hip implants. PLoS One 2016;11:e0155612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kuznetsova A, Brockhoff PB, Christensen RHB. 1merTest package: tests in linear mixed effects models. J Stat Softw 2017;82:1-26. [Google Scholar]
- 19. Steno B, Kokavec M, Necas L. Acetabular revision arthroplasty using trabecular titanium implants. Int Orthop 2015;39:389-395. [DOI] [PubMed] [Google Scholar]
- 20. Matharu GS, Judge A, Murray DW, Pandit HG. Outcomes following revision surgery performed for adverse reactions to metal debris in non-metal-on-metal hip arthroplasty patients: analysis of 185 revisions from the National Joint Registry for England and Wales. Bone Joint Res 2017;6:405-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Matharu GS, Judge A, Pandit HG, Murray DW. Which factors influence the rate of failure following metal-on-metal hip arthroplasty revision surgery performed for adverse reactions to metal debris? an analysis from the National Joint Registry for England and Wales. Bone Joint J 2017;99-B:1020-1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Collier JP, Mayor MB, Jensen RE, et al. Mechanisms of failure of modular prostheses. Clin Orthop Relat Res 1992;285:129-139. [PubMed] [Google Scholar]
- 23. Huk OL, Bansal M, Betts F, et al. Polyethylene and metal debris generated by non-articulating surfaces of modular acetabular components. J Bone Joint Surg [Br] 1994;76-B:568-574. [PubMed] [Google Scholar]
- 24. Zech S, Goesling T, Hankemeier S, et al. Differences in the mechanical properties of calcaneal artificial specimens, fresh frozen specimens, and embalmed specimens in experimental testing. Foot Ankle Int 2006;27:1126-1136. [DOI] [PubMed] [Google Scholar]
- 25. Beckmann NA, Jaeger S, Janoszka MB, et al. Comparison of the primary stability of a porous coated acetabular revision cup with a standard cup. J Arthroplasty 2018;33:580-585. [DOI] [PubMed] [Google Scholar]
- 26. Perona PG, Lawrence J, Paprosky WG, Patwardhan AG, Sartori M. Acetabular micromotion as a measure of initial implant stability in primary hip arthroplasty. An in vitro comparison of different methods of initial acetabular component fixation. J Arthroplasty 1992;7:537-547. [DOI] [PubMed] [Google Scholar]