Abstract
Adoptive T-cell immunotherapy is a rapidly growing field and is shifting the paradigm of clinical cancer treatment. Axicabtagene ciloleucel (axi-cel) is an anti-CD19 chimeric antigen receptor T-cell therapy that was initially developed at the National Cancer Institute and has recently been commercially approved by the US Food and Drug Administration for relapsed or refractory aggressive non-Hodgkin’s lymphomas including diffuse large B-cell lymphoma and its variants. The ZUMA-1 Phase I and II clinical trials formed the basis of the US Food and Drug Administration approval of this product, and we discuss the particulars of the clinical trials and the pharmacology of axi-cel. In addition, we review the CD19 chimeric antigen receptor T-specific toxicities of cytokine release syndrome and neurotoxicity, which remain the challenges to the safe delivery of this important therapy for aggressive B-cell lymphomas with poor prognosis.
Keywords: axicabtagene ciloleucel, CAR T, non-Hodgkin’s lymphoma, immunotherapy
Epidemiology of aggressive B-cell lymphomas
Aggressive B-cell lymphoma is a subtype of B-cell non-Hodgkin’s lymphomas (NHLs) that encompasses a clinically and molecularly heterogeneous group. In this group, diffuse large B-cell lymphoma (DLBCL) is the most common with ~22,000 cases a year and it represents 30%–35% of all lymphomas.1 Within DLBCL itself, there is additional heterogeneity and this is reflected in the World Health Organization 2016 classification that further subtypes of DLBCL to include high-risk histologies such as high-grade B-cell lymphomas not otherwise specified (NOS) and high-grade B-cell lymphomas with MYC and BCL2 and/or BCL6 rearrangements, known as double (DHL) or triple hit lymphomas (THL).2 Primary mediastinal B-cell lymphoma (PMBCL) and transformed follicular lymphoma (TFL) are less frequent, but important variant subtypes that are also described.
Clinical indicators of prognosis in DLBCL
The prognosis of aggressive B-cell lymphomas is based on clinical, molecular and genetic factors as well as responsiveness to induction chemotherapy. The International Prognostic Index (IPI), based on clinical features found at initial diagnosis (age, stage, extranodal disease, performance status and lactate dehydrogenase elevation) is historically the most widely used and is a powerful prognostic system.3 The revised version of the IPI score extended the predictive value of the IPI into the rituximab era (ie, when the anti-CD20 rituximab became widely added to chemotherapy due to overall survival [OS] benefits).4 An enhanced scoring system, the National Comprehensive Cancer Network-International Pronostic Index (NCCN-IPI) score, stratifies newly diagnosed DLBCL patients in four risk groups based on the same prognostic factors used in the IPI score, but with better discrimination of the low- and high-risk subgroups. Patients in the high-risk subgroup category per the revised version of the IPI score and the NCCN-IPI score have a 5-year OS of 54% and 33%, respectively.5,6 Overall, the prognostic scores highlight that a proportion of patients do not have successful outcomes with standard DLBCL treatment.
Molecular and genetic factors predictive of poor prognosis in DLBCL
Molecular profiling studies and next-generation sequencing have improved the understanding of DLBCL and its heterogeneity, and may prospectively identify cases with high-risk features.7,8 Based on the cell of origin using gene expression profiling studies, DLBCL can be classified as activated B-cell (ABC) subtype and germinal center B-cell (GCB) subtype (with 10% of cases being unclassifiable). ABC and GCB have distinct phenotypes and clinical characteristics, and with upfront chemotherapy, the ABC–DLBCL subtype has inferior outcomes after standard R-CHOP.9–11 Widespread use of gene expression profiling or next-generation sequencing remains limited due to cost and complexity, while immunohistochemistry methods are more practical for most pathology laboratories. By immunohistochemistry, the Hans classifier uses three markers (CD10, BCL6 and MUM1/IRF4) and classifies DLBCL as GCB or non-GCB, and seems to be a useful tool to differentiate DLBCL by the cell of origin.12,13 That said, RNA-based diagnostic testing to discriminate ABC and GCB subtypes appears to have higher accuracy, and recent advances allow testing in standard formalin-fixed paraffin-embedded biopsies rather than requiring fresh or frozen material.14
Another high-risk subgroup of DLBCL patients is char-acterized by the chromosomal translocation of the proto-oncogene c-MYC that promotes uncontrolled cell growth, unregulated cell division and extranodal dissemination of lymphomas.15 IgH-MYC rearrangements detected by fluorescent in situ hybridization or cytogenetics can be present in 3%–17% of all DLBCL cases and have particularly poor outcomes when coupled with BCL2 and/or BCL6 rearrangements (DHL or THL).16–18 Clinically, DHL and THL are char-acterized by advanced disease stage, highly elevated lactate dehydrogenase and central nervous system involvement.19,20 The optimal treatment of DHL has not been well defined, but it appears that frontline intensive regimens (such as dose-adjusted EPOCH-R with central nervous system prophylaxis) are associated with better outcomes.20–22 Given its poor outcomes with standard chemotherapy, DLBCL patients with c-MYC rearrangements represent another unmet need.
Response to therapy as a prognostic indicator
The addition of rituximab to CHOP improved the OS of patients with DLBCL; however, despite this advancement, ~30%–40% of patients relapse or are refractory to this regimen.23 In general, patients with refractory disease (less than partial response [PR] to initial treatment) or early relapse (relapse within a year from diagnosis or 6 months after the end of treatment) or progression within 2 years (event free survival 24) have poorer prognosis than those with late relapses.24,25 The current standard for relapsed DLBCL consists of salvage chemotherapy followed by autologous stem cell transplantation (ASCT) with a proportion of patients achieving cure.24,26 Approximately 50% of these patients who completed ASCT will ultimately relapse with minimal hope of cure despite international efforts at clinical trials and drug development in DLBCL.24,27,28 Indeed, the prognosis of relapsed DLBCL after ASCT relapse is poor with a median OS of 10 months, and is particularly worse for those relapsing within 6 months of transplantation with a median OS of 5.7 months.27,29
A retrospective international multicenter study (SCHOLAR-1) was carried out using data from Phase III randomized clinical trials (the European trial CORAL and the Canadian Clinical Trials Group LY.12 trial) and two observational studies (MD Anderson Cancer Center and University of Iowa/Mayo Clinic) that evaluated patients who achieved stable disease (SD) or progressive disease as the best response at any point during chemotherapy, or if relapse occurred within 12 months of ASCT. The results of this pooled analysis showed an overall response rate of 26% with a median OS of 6.3 months.30 Another large retrospective study of 15 US academic institutions assessed the risk factors of refractory DLBCL. Three subgroups were identified to have poor outcomes: primary progression (progressive disease with or within 6 months of chemoimmunotherapy [CIT]), residual disease (PR or SD after completion of CIT) and early relapse (relapse within 6 months of CIT and having achieved a complete response [CR]), with a 2-year OS of 18.5%, 30.6% and 45.5%, respectively.31 Multivariate analysis demonstrated that ultra-high risk (UHR) features in this cohort were primary progression, the presence of MYC rearrangement and intermediate-high or high NCCN-IPI score at the time of progression. The 2-year OS was very poor at 13.9% if any of these UHR factors were present (versus 57.6% in those without UHR features).31 These poor outcomes represent a significant unmet need in which novel approaches are urgently needed. It is in the landscape of relapsed/refractory and UHR DLBCL that CD19 chimeric antigen receptor (CAR) T cells have been studied to date.
Pharmacology and mode of action of axicabtagene ciloleucel (axi-cel)
One mechanism by which the immune system is able to recognize and fight cancer cells is through activation of T-lymphocytes that use T-cell receptors to recognize tumor peptides presented on major histocompatibility complexes.32 Once the T cells are activated, proliferation of T cells and cytotoxic granule secretion ensues, which leads to antitumor activity and lysis of tumor cells. However, tumors perform immune evasion by several mechanisms including increased expression of immune checkpoints (that limit T-cell activation and cause T-cell exhaustion) and effects of the tumor microenvironment. The design of CAR T cells is intended to enhance T-cell responses against tumor cells. The CARs are composed of an antibody-derived single-chain variable fragment linked to CD28 and CD3 zeta signaling domains. The combination of the specificity of a monoclonal antibody with the activation domain of T cells allows the CARs to deliver activated T cells with potent cytotoxicity against tumor-specific antigens and to target tumors independently of the major histocompatibility complex. Overall, CAR T engagement of CD19-expressing cancer cells results in T-cell activation, proliferation and secretion of inflammatory cytokines and chemokines resulting in tumor cell lysis.33,34
First-generation CARs utilized a signaling domain composed of CD3 zeta only and demonstrated weak proliferation ability and short survival, with short-lived antitumor activity. Co-stimulatory molecules, such as CD28, were introduced in second-generation CARs, and they proved to significantly improve signaling strength, expansion and persistence of CAR T cells.35 There are other co-stimulatory domains that are effective in improving T-cell signaling; however, CD28 and 4-1BB are currently the most widely used in CAR T-cell clinical trials. The optimal co-stimulatory domain is currently unknown. In general, the CD28-based CAR T-cell construct exhibits a greater peak expansion, whereas CAR T cells using 4-1BB co-stimulation show greater longevity (persistence).36 Further data are needed to confirm these findings and to find out whether the co-stimulatory domain used impacts clinical outcomes.
CD19 is a transmembrane glycoprotein that is expressed at all stages of differentiation of normal B cells. As a target, CD19 is expressed in over 95% of B-cell malignancies including chronic lymphocytic leukemia, B-cell NHL and acute lymphoblastic leukemia. Thus, CD19 is an attractive target for immunotherapeutic approaches with several companies and academic institutions developing pivotal trials with anti-CD19 CAR T cells.37,38
The development of axi-cel began with preclinical and clinical work at the National Cancer Institute (NCI). Initial studies demonstrated the proof of principle that anti-CD19 CAR T cells derived from human T cells can eradicate CD19-expressing malignant B cells, co-stimulation is required for CAR T-cell persistence and efficacy and finally CD19 CAR T cells can be clinically useful.34,39 The NCI CD19 CAR T cells were then developed by Kite Pharma (now owned by Gilead), leading to axi-cel, an US Food and Drug Administration-approved CD19-directed cellular immunotherapy of autologous T cells genetically engineered to express CARs.39
Pharmacokinetics
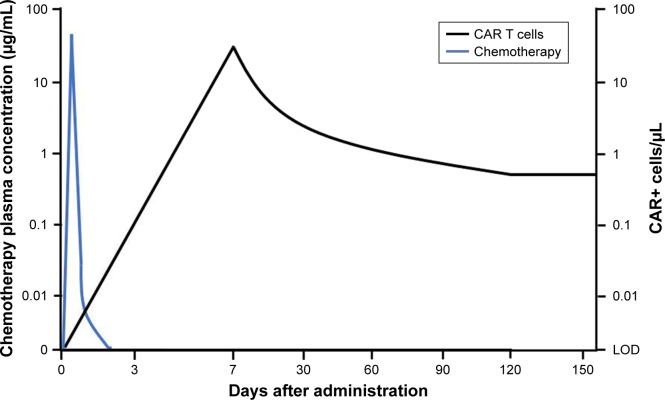
As a cytoreductive agent targeting rapidly dividing cells, chemotherapy has the greatest impact immediately following initiation of therapy. The decrease in tumor burden is initially dramatic, but short-lived, resulting in a return to the pretreatment growth rate and necessitating multiple cycles of chemotherapy to provide a long-term antineoplastic effect.40
Axi-cel offers a unique mechanism of action and pharmacokinetic profile in the treatment of NHL. In contrast to cytoreductive therapy, the decrease in tumor burden is not as rapid, but sustained after a single dose infusion. Although CAR T cells have the potential to cause serious toxicities such as cytokine release syndrome and neurotoxicity, the targeted action of axi-cel against CD19 limits additional adverse effects related to the damage of healthy cells to on-target off-tumor effects. Due to the expression of CD19 on all nonmalignant B-cell lymphocytes, on-target prolonged suppression of B cells (B-cell aplasia) is one of the complications of CD19 CAR T-cell therapy.41
Axi-cel is a single-dose infusion containing a suspension of 2×106 CAR-positive viable T cells per kilogram body weight (maximum of 2×108 CAR-positive viable T cells) iñ68 mL.42 Following administration, axi-cel exhibits a rapid expansion, with peak CAR T-cell levels occurring within 7–14 days. In the pivotal Phase II trial, ZUMA-1, of axi-cel in large B-cell lymphoma, CAR T cells remained detectable in most patients at 180 days. The median CAR T area under the curve (AUC), defined as the cumulative level of CAR-positive cells/µL of blood over the first 28 days following axi-cel, was 462.3 cells/µL (range 5.1–14,329.3). Notably, CAR T expansion and peak cellular concentration within 28 days of infusion demonstrated a positive correlation with objective clinical response. The CAR T AUC was 5.4 times higher in patients with an objective response rate (ORR) versus patients without a response. Of the patients obtaining a CAR T AUC exceeding the median AUC, the ORR was 96%.43,44 These results further emphasize the importance of CAR T expansion post-infusion, as observed in previous studies.45,46 Peak expansion was also associated with grade 3 or higher neurologic events, but was not correlated with cytokine release syndrome43 (Figure 1).
Figure 1.
Comparative serum concentrations of chemotherapy and CAR T-cell expansion.
Notes: Traditional cytoreductive chemotherapy has the greatest impact immediately following initiation; however, it is short-lived, requiring multiple cycles for a long-term antineoplastic effect. In contrast, the pharmacokinetic profile of axi-cel leads to a slower initial decrease in tumor burden, but it is sustained after a single infusion due to potential persistence of CAR T cells in patients’ blood over time.
Abbreviations: CAR, chimeric antigen receptor; LOD, limit of detection.
In contrast to cell expansion, the significance of cell persistence is unclear. CAR T-cell persistence and B-cell aplasia have been reported with axi-cel.47,48 In ZUMA-1, three patients with an ongoing complete remission at 24 months still had detectable blood levels of CAR T cells.43 However, recent data from earlier studies of NCI showed that long-term complete remissions are documented with limited persistence and recovery of normal B cells.48 This is in contrast to patients with acute lymphoblastic leukemia in whom recovery of normal B cells may be associated with poor prognosis.49,50 Long-term persistence allows for continued disease assessment, however, at the cost of long-term B-cell aplasia.51 The effect of CAR T-cell persistence is unknown with limited and conflicting data; determining the role and impact on disease response is an area of ongoing research.
Manufacturing
The general manufacturing processes of CAR T cells consist of T-cell collection (harvesting), T-cell selection (through magnetic beads) and activation (with an anti-CD3 antibody in the presence of interleukin [IL]-2), introduction of the CAR gene into the activated T cell through a vector (lentivirus or retrovirus), CAR T-cell expansion and CAR T-cell product formulation.52,53 In order to streamline the process and improve the support for large global trials (or even widespread clinical use), some key steps were taken for the manufacturing of axi-cel, such as removal of human serum from the culture media, thus reducing the infection risk, and excluding the use of magnetic beads for T-cell selection. In addition, there was a decrease in the duration of ex vivo expansion, thus minimizing the risk of T-cell exhaustion.52,54 This process led to the production of predominantly CD3+ T cells with CD8+ T cells in 57% and CD4+ T cells in 43%, with the majority being effector T cells and central memory T cells (TCM).54 The process was highly successful and the expected time of axi-cel production was <2 weeks.43,54
Efficacy of axi-cel
Lymphoma response criteria and trial design
Results of axi-cel in DLBCL and variants have mainly been reported in terms of patients who received infusion of the CAR T cells, although an intent-to-treat analysis is also reported.43,44 Although the lymphoma response criteria have been updated, in ZUMA-1, the Cheson 2007 criteria were used, which allows a comparison with prior clinical trials.55,56 By these criteria, the ORR is defined as the rate of patients attaining a CR (disappearance of measurable disease on computed tomography scan or residual masses that are positron emission tomography negative) or a PR (50% decrease in tumor burden with ongoing positron emission tomography avidity). However, for the purposes of clinical outcome in aggressive lymphoma, attaining CR is the most important and it is further important that these CRs are durable and that relapse does not occur.
Axi-cell was initially tested outside of the NCI in the Phase I ZUMA-1 study; this was the first multicenter study of CAR T-cell therapy in refractory aggressive NHL including DLBCL, TFL and PMBCL. This study included seven patients and showed durable responses with axi-cel with an ORR and CR rate of 71% and 57%, respectively.47 These encouraging results led to the multicenter Phase II portion of ZUMA-1. Key eligibility criteria for this study were aggressive B-cell lymphomas (DLBCL, PMBCL and TFL), refractory disease with no response to last therapy or relapse within 12 months of autologous hematopoietic stem cell transplantation, prior anti-CD20 monoclonal antibody and anthracycline and an Eastern Cooperative Oncology Group (ECOG) of 0–1. The primary endpoint was ORR in patients with >6 months follow-up post-axi-cel infusion. The secondary endpoints were duration of response, OS, safety and levels of CAR T cells and cytokines. The CAR manufacturing success was 99%. The conditioning regimen consisted of cyclophosphamide 500 mg/m2 and fludarabine 30 mg/m2 ×3 days followed by infusion of KTE-C19 or axi-cel at a dose of 1–2×106 CART cells/kg. The conditioning regimen and doses were determined in previous studies.57
Efficacy of axi-cel on ZUMA-1
Administration of axi-cel was highly efficacious in 101 patients with refractory/relapsed DLBCL, who were considered to have a poor prognosis with a median OS of ~6 months and no available standard therapies.30 The median time to response was 1 month, which is the timing of the first response assessment in the trial protocol of ZUMA-1. However, the range was 0.8–6.0 months, which indicates that patients not showing response at the 1-month assessment could convert and be seen to respond in subsequent months. Indeed, 11 of 35 patients in PR and 12 of 25 patients with SD at 1 month subsequently converted to CR. That said, patients who never attained CR (maximum response of PR) had a median duration of response of 1.9 months only, consistent with the usual situation in aggressive lymphoma where PR is not an adequate depth of response44 (Table 1).
Table 1.
Highlights of the ZUMA-1 trial of axicabtagene ciloleucel, a CD19 CAR T-cell product, in DLBCL and variants
| Highlights of the Zuma-1 clinical trial with axicabtagene ciloleucel (Yescarta) in DLBCL and variants | |
|---|---|
| Product | Autologous T cells expressing a CAR: |
| • Antibody fragment to target CD19 | |
| • Intracellular domains of CD3 zeta (to activate T-cell receptor signaling) and CD28 (for co-stimulation and persistence) | |
| Inclusion/exclusion highlights | • DLBCL, TFL and PMBCL all allowed. Richter transformation from CLL, indolent lymphoma and mantle cell lymphoma was not included |
| • Chemorefractory disease: stable disease or progressive disease as the best response to the most recent regimen (second line or greater), or progression within 12 months of autologous stem cell transplant | |
| • No history of CNS lymphoma or current involvement | |
| Manufacturing | • Median time from leukapheresis to delivery 17 days |
| • Successful CAR T production in 99% of patients | |
| Conditioning and dose | • Days −5 to −3: Fludarabine 30 mg/m2 and cyclophosphamide 500 mg/m2 daily |
| • Day 0: 2×106 CAR T cells/kg | |
| Bridging while awaiting cell infusion | • Chemotherapy not allowed |
| • Ten of 111 patients with successful manufacturing did not proceed to CAR T-cell infusion. Seven were due to adverse events or death prior to infusion | |
| Efficacy | • Median time to response 1 month (range 0.8–6.0 months) |
| • ORR 82%, CR 54%, 6-month PFS 49%. Relapses appear to be infrequent after 6 months | |
| • TFL and PMBCL have a higher CR rate than de novo DLBCL (71% versus 49%) | |
| • Historical cohort (SCHOLAR-1) ORR 26%, median OS of 6.3 months | |
| Deaths | Of 101 patients receiving CAR T cells: |
| • 37 died of disease progression | |
| • 2 died of CRS-associated events (cardiac arrest, HLH) | |
| • 1 died of pulmonary embolus | |
| Toxicity | • CRS grade 3 or higher: 13% |
| • Neurologic events grade 3 or higher: 28% | |
| • Toxicity management with tocilizumab or steroids did not appear to affect CAR T-cell efficacy | |
| Biomarkers | • CAR T-cell efficacy was not affected by classic prognostic markers in DLBCL, such as IPI, cell of origin (ABC versus GCB) or number of prior lines of therapy |
| • Expansion (peak CAR T-cell levels in the blood) was correlated not only with response, but also with neurologic events | |
| • Cytokine release was associated with CRS and neurologic events | |
Abbreviations: ABC, activated B-cell subtype of DLBCL; CAR, chimeric antigen receptor; CLL, chronic lymphocytic leukemia; CR, complete response rate; CRS, cytokine release syndrome; DLBCL, diffuse large B-cell lymphoma; GCB, germinal center B-cell subtype of DLBCL; HLH, hemophagocytic lymphohistiocytosis; IPI, International Prognostic Index; ORR, objective response rate (includes complete and partial responses); OS, overall survival; PFS, progression-free survival; PMBCL, primary mediastinal B-cell lymphoma; TFL, transformed follicular lymphoma; CNS, central nervous system; ABC, activated B-cell subtype of DLBCL.
Including all variants of DLBCL enrolled, the ORR of axi-cel was 82% with a CR rate of 54%. The expected ORR of conditioning doses of fludarabine and cyclophosphamide alone without CAR T cells is not known. In general, fludarabine-based regimes are not considered to have significant antitumor activity in aggressive lymphomas.58–60 Therefore, these results suggest that axi-cel was active in the majority of patients due to the anti-lymphoma effects of the cellular product.
Although no statistical test was applied, the CR rate of the variants of DLBCL (TFL and PMBCL) was numerically higher than that for de novo DLBCL (DLBCL, CR rate 49%; TFL/PMBCL, CR rate 71%).43,44 Beyond this, the subgroup analysis did not identify clinical or disease-related risk factors that predicted response. The caveat of the subgroup analysis is that it is underpowered and may not identify true differences. Nonetheless, typical DLBCL risk factors such as age, stage, IPI risk score or bulky disease >10 cm did not obviously predict CAR T failure per multivariate analysis.43
The earliest patients treated with the CD19 CAR T construct at the NCI (the same construct as axi-cel) have attained long-term durable CRs up to 56 months.48 In ZUMA-1, the updated analysis was conducted after a minimum follow-up of 1 year, with 42% of patients still in CR. In general, very few relapsed occurred if patients remained in CR at 6 months post-CAR T infusion, but long-term follow-up will be required to determine the curative potential of this therapy.
Efficacy comparison of axi-cel to other CD19 CAR T products in DLBCL
When comparing the efficacy of axi-cel to other CD19 CAR T-cell products including tisagenleucel (tis-gen) and lisocabtagene maraceucel (liso-cel), it is important to note some key differences in trial design. For example, tis-gen was tested in both DLBCL and follicular lymphoma, and not all DLBCL patients (12 patients – 86%) met the criteria for refractory disease.61 Conversely, the variants TFL and PMBCL (with high CR rates for axi-cel) were not included. The efficacy results of tis-gen were similar to those of axi-cel with 6 out of 14 DLBCL patients (43%) attaining CR.61 Similarly, liso-cel (at the optimized dose level) showed a 6-month CR rate of 50%, in 14 patients with DLBCL or TFL only.62 While cross-trial comparisons should be viewed with great caution for methodological reasons, overall, it seems that the efficacy of axi-cel is similar to that of the other two CD19 CAR T-cell products. This is despite substantial design and manufacturing differences among the three products (reviewed in Jain and Davila63).
Biomarkers of efficacy
After infusion into the patient, CAR T cells duplicate inside the patient. On ZUMA-1, CAR T-cell numbers rapidly increased, peaking at day +7 after the infusion.64 The peak number of cells (known as peak expansion) was fourfold higher in responding patients compared to that in patients who did not respond (p=0.002), highlighting that expansion is important to obtain a response. An identified determinant of CAR T expansion was the composition of the T-cell subsets that made up the manufactured axi-cel product.65 Axi-cel product that had a higher proportion of naïve and TCM led to superior expansion after infusion compared to the product that had more effector and effector memory T cells. It is not well understood which clinical, biologic or manufacturing factors promote naïve and TCM retention in manufactured CAR T-cell products.
Safety and tolerability
While anti-CD19 CAR T-cell therapy offers a new therapeutic strategy for aggressive B-cell lymphomas, its growing use requires further education/training and prompt recognition and management of these unique toxicities. In the primary analysis of ZUMA-1, all 101 patients who received axi-cel encountered adverse events, with 95% having grade 3 or higher related adverse events.43 Two of the most common toxicities observed are cytokine release syndrome (CRS) and CAR T-cell–related encephalopathy syndrome (CRES). Close monitoring parameters, early identification and intensive supportive management minimize the life-threatening risks caused by this potentially curative therapy.
Cytokine release syndrome
CRS is the most common and well-described toxicity associated with CAR T-cell therapy, occurring in over 90% of patients at any grade, as reported in the ZUMA-1 clinical trial.43 The activation of T cells upon recognition of tumor antigens by CARs results in the release of inflammatory cytokines and chemokines including IL-6, soluble IL-6R, IL-2, soluble IL-2Rα, interferon-γ, tumor necrosis factor α, IL-8, and IL-10, granulocyte-macrophage colony-stimulating factor and activated immune effector cells.66
Given the nature of the systemic inflammatory response, any organ system can be affected, including cardiovascular, pulmonary, gastrointestinal, hepatic, renal, nervous, integumentary, musculoskeletal and hematologic systems. The most common symptoms of CRS include pyrexia, hypoxia and hypotension, and the onset of CRS symptoms typically occurs within the first week after CAR T-cell infusion with a median onset at 2 days in the ZUMA-1 trial. However, CRS sometimes persists, with symptoms resolving by a median time of 8 days.41,43 As the use of CAR T-cell therapy becomes widespread, more experience and knowledge with clinical use will lead to more detailed assessment systems, algorithms, preventive measures and supportive interventions.
Lee et al proposed the current consensus criteria for CRS grading as seen in Table 2, and organ toxicity assessment was graded as per the Common Terminology Criteria for Adverse Events (v4.0).67 For management of grade 1 and 2 CRS, there should be assessment for infection and vigilant supportive care including intravenous fluids, antipyretics and analgesics as needed, with a close monitoring of cardiac complications and other organ function. Tocilizumab is an anti-IL-6 monoclonal antibody that can be considered in patients with identified CRS, and tocilizumab can result in rapid resolution of CRS toxicities without loss of CAR T-cell expansion or efficacy. The timing for tocilizumab administration has evolved in the last few years, especially since more experience has been gained with high-risk immunotherapy trials. It was initially recommended for grade 3 CRS, but the current consensus recommendation is to use it with grade 2 CRS and higher.43,44 Tocilizumab doses of 4–8 mg/kg (maximum dose 800 mg) can be repeated as needed for patients with persistent signs/symptoms of CRS. However, if there is no improvement despite anti-IL-6 therapy with ongoing severe CRS grade 3 or higher, high-dose corticosteroids could be considered. The role of steroids is fundamental in the treatment of CRS (and neurotoxicity) and should be considered for severe cases after tocilizumab therapy failure or even concomitantly to anti-IL-6 therapy in special situations.66,67 Although there is a theoretical risk of subsequent lymphotoxic effect and CAR T-cell suppression with steroid therapy, this has not been demonstrated in the ZUMA-1 study.43,68 In the ZUMA-1 trial, tocilizumab and steroids (at various doses) were administered to 43% and 27% of patients, respectively, for the treatment of CRS and/or neurotoxicity43 (Table 1).
Table 2.
Grading of CRS
| Grade 1 | Grade 2 | Grade 3 | Grade 4 |
|---|---|---|---|
| Fever (≥38.3°C) | Hypotension responsive to fluids or one low-dose vasopressor | Hypotension requiring multiple or high-dose vasopressors | Requiring mechanical ventilation |
| Constitutional symptoms | Hypoxia responsive to <40% FiO2 Organ toxicity grade 2 |
Hypoxia requiring ≥40% FiO2 Organ toxicity grade 3 Grade 4 transaminitis |
Organ toxicity grade 4 excluding transaminitis |
Abbreviation: CRS, cytokine release syndrome.
CAR T-cell–related neurotoxicity
Grading scales for neurologic events in the ZUMA-1 trial followed the NCI Common Terminology Criteria for Adverse Events, version 4.03, and the grading of common neurotoxicities seen is displayed in Table 3. In this trial, 64% of patients experienced a neurologic event at any grade, with 28% having grade 3 or higher neurotoxicity.43,44 The best described is CRES, which occurred in 34% of patients to any grade and 21% of patients at grade 3. Other grade 3 neurologic events frequently observed were confusional state, aphasia and somnolence, and early neurologic signs included word-finding difficulties, inattention, disorientation, agitation or seizures. Median onset of neurotoxicity occurred at day 5 post-CAR T-cell infusion, with the median time of resolution of neurologic symptoms being day 17. All patients who developed neurologic symptoms had complete resolution, except for four patients who died from either progressive disease or unrelated adverse events43 (Table 1).
Table 3.
Grading of the common neurotoxicity symptoms
| Neurotoxicity grading assessment (CTCAE 4.03) | Grade 1 | Grade 2 | Grade 3 | Grade 4 |
|---|---|---|---|---|
| Encephalopathy | Mild limiting of ADL | Limiting instrumental ADL | Limiting self-care ADLs | Life-threatening consequences |
| Confusion | Mild disorientation | Moderate disorientation; limiting instrumental ADL | Severe disorientation; limiting self-care ADL | Life-threatening consequences; urgent intervention indicated |
| Dysphasia | Awareness of receptive or expressive characteristics; impaired ability to communicate | Moderate receptive/expressive characteristics; impaired ability to communicate spontaneously | Severe receptive/expressive characteristics; impaired ability to read, write or communicate intelligibly | N/A |
| Seizure | Brief partial seizure; no loss of consciousness | Brief generalized seizure | Multiple seizures despite medical intervention | Life-threatening; prolonged repetitive seizures |
| Somnolence | Mild, but more than usual drowsiness or sleepiness | Moderate sedation; limiting instrumental ADL | Obtundation or stupor | Life-threatening; urgent intervention indicated |
Note: Neurotoxicity grading assessment of common adverse events from CAR T-cell therapy.
Abbreviations: ADL, activities of daily living; CAR, chimeric antigen receptor; CTCAE, Common Terminology Criteria for Adverse Events; N/A, not applicable.
In a review of 133 adults who received lymphodepletion chemotherapy followed by infusion of CD19 CAR T cells, 53 (40%) developed one or more grade 1 or higher neurologic adverse events. Grade ≥3 neurotoxicity was associated with more severe CRS, disseminated intravascular coagulation with subsequent coagulopathy, earlier peak of IL-6 concentration and evidence of endothelial activation with capillary leak.69 Patients who developed severe neurotoxicity also showed increased cerebrospinal fluid protein levels, increased cells including CAR T cells, and inflammatory cytokines such as IL-6, interferon-γ and tumor necrosis factor α in the cerebrospinal fluid.66,69 This suggests increased blood–brain barrier permeability associated with the pathophysiology of neurotoxicity after CAR T-cell infusion.
Monitoring and grading of CRES involves close neuro-logic assessments with ongoing evaluation for signs or symptoms of further complications including increased intracranial pressure and seizures. Grade 1 CRES involves supportive care with consideration of electroencephalogram, magnetic resonance imaging, funduscopic exam and neurology consultation, and grade 2 CRES adds to this management with anti-IL6 therapy, particularly if concurrent CRS occurs. More severe CRES grades 3 and 4 require intensive care unit admission, corticosteroids for symptoms not responding to anti-IL-6 and medical management of status epilepticus and increased intracranial pressure with consideration of neurosurgical evaluation if indicated.66
Other safety and supportive care considerations
Other commonly encountered and potential risks include cytopenias, B-cell aplasia, consumptive coagulopathies, neutropenic fever, infections and tumor lysis syndrome. Patients enduring B-cell aplasia may require intravenous immunoglobulin infusions for prolonged period of time.66 Ongoing investigations are looking into preventive measures to limit toxicity experienced by patients receiving CAR T-cell therapy. Efforts include identifying baseline and treatment-related risk factors for development of CRS, which have been associated with higher marrow tumor burden, fludarabine/cyclophosphamide lymphodepletion and higher CAR T-cell dose.70
Prophylactic supportive care considerations have previously consisted of seizure prophylaxis with levetiracetam 750 mg orally every 12 hours for 30 days starting on the day of CAR T infusion, tumor lysis precautions per institutional guidelines and other institution-dependent algorithms for monitoring and symptom management.66,67 As clinical utilization and experience grows, further standardized assessments, grading and adverse event management protocols can be developed for improved early recognition and expedited treatment.
Patient-focused perspectives
The results of ZUMA-1 (and other multicenter studies in CAR T-cell therapy for refractory lymphomas) met the primary endpoint of improving objective responses in a patient population with refractory aggressive B-cell lymphomas with otherwise no options of cure.30,43,48 Thus, these data suggest that there is a significant patient benefit with CAR T-cell therapy. It is most likely to be accepted as a viable alternative for the disease with an otherwise very poor prognosis, despite the potential associated toxicity.
The toxicities of CAR T-cell therapy are unique; thus, strategies for recognition and management of CRS and CRES are of paramount importance in order to minimize and/or speed up the recovery of patients receiving this type of high-risk immunotherapy. Conversely, patient education will become essential not only for understanding the efficacy and toxicity of CAR T-cell therapy, but also for the recognition of early toxicity signs. The development of guidelines and harmonization of the management of CAR T-cell therapy–related toxicities have been the focus of investigators recently.66,67 In addition, the development of institutional guidelines and specialized immunotherapy centers with multidisciplinary support from different specialties and allied health providers may ensure the success of utilizing this therapy in a large scale for further benefiting patients.71
With the approval of axi-cel for the treatment of refractory DLBCL and since its clinical benefit will likely outweigh the risk associated with this therapy, a Risk Evaluation and Mitigation Strategies program has been established in order to mitigate the side effects related to CAR T-cell therapy. The Risk Evaluation and Mitigation Strategies program ensures that hospitals or cancer centers are adequately trained for the management of the toxicity and have the essential elements to treat toxicity (ie, availability of tocilizumab).
As this therapy will become widely available as the standard of care for refractory aggressive B-cell lymphomas, it is important to recognize that not all patients will have a favorable clinical condition/comorbidities that will make them candidates to receive this therapy. Honest discussion of the pros and cons of CAR T-cell therapy should occur and alternatives should be offered, including quality of life recommendations.
Conclusion
The development of CAR T-cell therapy represents the paradigm of personalized medicine and cancer immunotherapy. With the imminent widespread use (given the US Food and Drug Administration approval), one of the main focuses has been the optimization of CAR T-cell construct technology and improving the manufacturing process in order to increase its efficiency without affecting its activity and potency.72 The understanding and management of CAR T-related toxicities represent another challenge and focus of research.
The dramatic responses seen with CAR T-cell therapy in B-cell lymphomas (and other hematologic malignancies) will likely shift the treatment paradigm of these conditions. This may include the use of this therapy in earlier stage of the disease or even as frontline therapy. However, the expected widespread availability CAR T-cell therapy will also come with a significant economic burden due to the high cost of the therapy and the care of patients developing related toxicities.
Several hurdles and setbacks have marked the path of CAR T-cell therapy from its initial preclinical and case reports to multicenter studies with promising results.73 There is still much to do in the field, and it will depend on the collaboration, hope and vision of investigators, patients and supporters.
Footnotes
Disclosure
Julio C Chavez received fees from Kite Pharma (advisory board, speakers’ bureau) and Novartis (advisory board). The other authors report no conflicts of interest in this work.
References
- 1.Howlader N, Noone A, Krapcho M. SEER Cancer Statistics Review, 1975–2012, Based On November 2014 SEER Data Submission, Posted to the SEER Web Site, April 2015. Bethesda, MD, USA: National Cancer Institute; 2015. [Accessed November 1, 2017]. Forrás: Available from: http://seercancergov/csr/1975_2010/(2015 június 10 17: 41) [Google Scholar]
- 2.Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127(20):2375–2390. doi: 10.1182/blood-2016-01-643569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.International Non-Hodgkin’s Lymphoma Prognostic Factors Project A predictive model for aggressive non-Hodgkin’s lymphoma. N Engl J Med. 1993;329(14):987–994. doi: 10.1056/NEJM199309303291402. [DOI] [PubMed] [Google Scholar]
- 4.Sehn LH, Berry B, Chhanabhai M, et al. The revised International Prognostic Index (R-IPI) is a better predictor of outcome than the standard IPI for patients with diffuse large B-cell lymphoma treated with R-CHOP. Blood. 2007;109(5):1857–1861. doi: 10.1182/blood-2006-08-038257. [DOI] [PubMed] [Google Scholar]
- 5.Zhou Z, Sehn LH, Rademaker AW, et al. An enhanced International Prognostic Index (NCCN-IPI) for patients with diffuse large B-cell lymphoma treated in the rituximab era. Blood. 2014;123(6):837–842. doi: 10.1182/blood-2013-09-524108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El-Galaly TC, Villa D, Alzahrani M, et al. Outcome prediction by extranodal involvement, IPI, R-IPI, and NCCN-IPI in the PET/CT and rituximab era: a Danish-Canadian study of 443 patients with diffuse-large B-cell lymphoma. Am J Hematol. 2015;90(11):1041–1046. doi: 10.1002/ajh.24169. [DOI] [PubMed] [Google Scholar]
- 7.Pasqualucci L, Trifonov V, Fabbri G, et al. Analysis of the coding genome of diffuse large B-cell lymphoma. Nat Genet. 2011;43(9):830–837. doi: 10.1038/ng.892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang J, Grubor V, Love CL, et al. Genetic heterogeneity of diffuse large B-cell lymphoma. Proc Natl Acad Sci U S A. 2013;110(4):1398–1403. doi: 10.1073/pnas.1205299110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenwald A, Wright G, Chan WC, et al. Leukemia Molecular Profiling Project The use of molecular profiling to predict survival after chemotherapy for diffuse large-B-cell lymphoma. N Engl J Med. 2002;346(25):1937–1947. doi: 10.1056/NEJMoa012914. [DOI] [PubMed] [Google Scholar]
- 10.Alizadeh AA, Eisen MB, Davis RE, et al. Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature. 2000;403(6769):503–511. doi: 10.1038/35000501. [DOI] [PubMed] [Google Scholar]
- 11.Lenz G, Wright G, Dave SS, et al. Lymphoma/Leukemia Molecular Profiling Project Stromal gene signatures in large-B-cell lymphomas. N Engl J Med. 2008;359(22):2313–2323. doi: 10.1056/NEJMoa0802885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hans CP, Weisenburger DD, Greiner TC, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004;103(1):275–282. doi: 10.1182/blood-2003-05-1545. [DOI] [PubMed] [Google Scholar]
- 13.Visco C, Li Y, Xu-Monette ZY, et al. Comprehensive gene expression profiling and immunohistochemical studies support application of immunophenotypic algorithm for molecular subtype classification in diffuse large B-cell lymphoma: a report from the International DLBCL Rituximab-CHOP Consortium Program Study. Leukemia. 2012;26(9):2103–2113. doi: 10.1038/leu.2012.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scott DW, Mottok A, Ennishi D, et al. Prognostic significance of diffuse large B-cell lymphoma cell of origin determined by digital gene expression in formalin-fixed paraffin-embedded tissue biopsies. J Clin Oncol. 2015;33(26):2848–2856. doi: 10.1200/JCO.2014.60.2383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adhikary S, Eilers M. Transcriptional regulation and transformation by Myc proteins. Nat Rev Mol Cell Biol. 2005;6(8):635–645. doi: 10.1038/nrm1703. [DOI] [PubMed] [Google Scholar]
- 16.Savage KJ, Johnson NA, Ben-Neriah S, et al. MYC gene rearrangements are associated with a poor prognosis in diffuse large B-cell lymphoma patients treated with R-CHOP chemotherapy. Blood. 2009;114(17):3533–3537. doi: 10.1182/blood-2009-05-220095. [DOI] [PubMed] [Google Scholar]
- 17.Barrans S, Crouch S, Smith A, et al. Rearrangement of MYC is associated with poor prognosis in patients with diffuse large B-cell lymphoma treated in the era of rituximab. J Clin Oncol. 2010;28(20):3360–3365. doi: 10.1200/JCO.2009.26.3947. [DOI] [PubMed] [Google Scholar]
- 18.Horn H, Ziepert M, Becher C, et al. German High-Grade Non-Hodgkin Lymphoma Study Group MYC status in concert with BCL2 and BCL6 expression predicts outcome in diffuse large B-cell lymphoma. Blood. 2013;121(12):2253–2263. doi: 10.1182/blood-2012-06-435842. [DOI] [PubMed] [Google Scholar]
- 19.Johnson NA, Slack GW, Savage KJ, et al. Concurrent expression of MYC and BCL2 in diffuse large B-cell lymphoma treated with rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone. J Clin Oncol. 2012;30(28):3452–3459. doi: 10.1200/JCO.2011.41.0985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Petrich AM, Gandhi M, Jovanovic B, et al. Impact of induction regimen and stem cell transplantation on outcomes in double-hit lymphoma: a multicenter retrospective analysis. Blood. 2014;124(15):2354–2361. doi: 10.1182/blood-2014-05-578963. [DOI] [PubMed] [Google Scholar]
- 21.Oki Y, Noorani M, Lin P, et al. Double hit lymphoma: the MD Anderson Cancer Center clinical experience. Br J Haematol. 2014;166(6):891–901. doi: 10.1111/bjh.12982. [DOI] [PubMed] [Google Scholar]
- 22.Howlett C, Snedecor SJ, Landsburg DJ, et al. Front-line, dose-escalated immunochemotherapy is associated with a significant progression-free survival advantage in patients with double-hit lymphomas: a systematic review and meta-analysis. Br J Haematol. 2015;170(4):504–514. doi: 10.1111/bjh.13463. [DOI] [PubMed] [Google Scholar]
- 23.Coiffier B, Thieblemont C, Van Den Neste E, et al. Long-term outcome of patients in the LNH-98.5 trial, the first randomized study comparing rituximab-CHOP to standard CHOP chemotherapy in DLBCL patients: a study by the Groupe d’Etudes des Lymphomes de l’Adulte. Blood. 2010;116(12):2040–2045. doi: 10.1182/blood-2010-03-276246. French. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gisselbrecht C, Glass B, Mounier N, et al. Salvage regimens with autologous transplantation for relapsed large B-cell lymphoma in the rituximab era. J Clin Oncol. 2010;28(27):4184–4190. doi: 10.1200/JCO.2010.28.1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maurer MJ, Ghesquieres H, Jais JP, et al. Event-free survival at 24 months is a robust end point for disease-related outcome in diffuse large B-cell lymphoma treated with immunochemotherapy. J Clin Oncol. 2014;32(10):1066–1073. doi: 10.1200/JCO.2013.51.5866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Crump M, Kuruvilla J, Couban S, et al. Randomized comparison of gemcitabine, dexamethasone, and cisplatin versus dexamethasone, cytarabine, and cisplatin chemotherapy before autologous stem-cell transplantation for relapsed and refractory aggressive lymphomas: NCIC-CTG LY.12. J Clin Oncol. 2014;32(31):3490–3496. doi: 10.1200/JCO.2013.53.9593. [DOI] [PubMed] [Google Scholar]
- 27.Van Den Neste E, Schmitz N, Mounier N, et al. Outcomes of diffuse large B-cell lymphoma patients relapsing after autologous stem cell transplantation: an analysis of patients included in the CORAL study. Bone Marrow Transplant. 2017;52(2):216–221. doi: 10.1038/bmt.2016.213. [DOI] [PubMed] [Google Scholar]
- 28.Van Den Neste E, Schmitz N, Mounier N, et al. Outcome of patients with relapsed diffuse large B-cell lymphoma who fail second-line salvage regimens in the International CORAL study. Bone Marrow Transplant. 2016;51(1):51–57. doi: 10.1038/bmt.2015.213. [DOI] [PubMed] [Google Scholar]
- 29.Nagle SJ, Woo K, Schuster SJ, et al. Outcomes of patients with relapsed/refractory diffuse large B-cell lymphoma with progression of lymphoma after autologous stem cell transplantation in the rituximab era. Am J Hematol. 2013;88(10):890–894. doi: 10.1002/ajh.23524. [DOI] [PubMed] [Google Scholar]
- 30.Crump M, Neelapu SS, Farooq U, et al. Outcomes in refractory diffuse large B-cell lymphoma: results from the international SCHOLAR-1 study. Blood. 2017;130(16):1800–1808. doi: 10.1182/blood-2017-03-769620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Costa LJ, Maddocks K, Epperla N, et al. Diffuse large B-cell lymphoma with primary treatment failure: ultra-high risk features and benchmarking for experimental therapies. Am J Hematol. 2017;92(2):161–170. doi: 10.1002/ajh.24615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang Y. Cancer immunotherapy: harnessing the immune system to battle cancer. J Clin Invest. 2015;125(9):3335–3337. doi: 10.1172/JCI83871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kochenderfer JN, Wilson WH, Janik JE, et al. Eradication of B-lineage cells and regression of lymphoma in a patient treated with autologous T cells genetically engineered to recognize CD19. Blood. 2010;116(20):4099–4102. doi: 10.1182/blood-2010-04-281931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kochenderfer JN, Feldman SA, Zhao Y, et al. Construction and preclinical evaluation of an anti-CD19 chimeric antigen receptor. J Immunother. 2009;32(7):689–702. doi: 10.1097/CJI.0b013e3181ac6138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Savoldo B, Ramos CA, Liu E, et al. CD28 costimulation improves expansion and persistence of chimeric antigen receptor-modified T cells in lymphoma patients. J Clin Invest. 2011;121(5):1822–1826. doi: 10.1172/JCI46110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van der Stegen SJ, Hamieh M, Sadelain M. The pharmacology of second-generation chimeric antigen receptors. Nat Rev Drug Discov. 2015;14(7):499–509. doi: 10.1038/nrd4597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Scheuermann RH, Racila E. CD19 antigen in leukemia and lymphoma diagnosis and immunotherapy. Leuk Lymphoma. 1995;18(5–6):385–397. doi: 10.3109/10428199509059636. [DOI] [PubMed] [Google Scholar]
- 38.Brentjens RJ, Latouche JB, Santos E, et al. Eradication of systemic B-cell tumors by genetically targeted human T lymphocytes co-stimulated by CD80 and interleukin-15. Nat Med. 2003;9(3):279–286. doi: 10.1038/nm827. [DOI] [PubMed] [Google Scholar]
- 39.Kochenderfer JN, Yu Z, Frasheri D, Restifo NP, Rosenberg SA. Adoptive transfer of syngeneic T cells transduced with a chimeric antigen receptor that recognizes murine CD19 can eradicate lymphoma and normal B cells. Blood. 2010;116(19):3875–3886. doi: 10.1182/blood-2010-01-265041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Madan RA, Gulley JL, Fojo T, Dahut WL. Therapeutic cancer vaccines in prostate cancer: the paradox of improved survival without changes in time to progression. Oncologist. 2010;15(9):969–975. doi: 10.1634/theoncologist.2010-0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brudno JN, Kochenderfer JN. Toxicities of chimeric antigen receptor T cells: recognition and management. Blood. 2016;127(26):3321–3330. doi: 10.1182/blood-2016-04-703751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yescarta (axicabtagene ciloleucel) [package insert] Santa Monica, CA, USA: Kite Pharma, Inc;; 2017. [Google Scholar]
- 43.Neelapu SS, Locke FL, Bartlett NL, et al. Axicabtagene Ciloleucel CAR T-cell therapy in refractory large B-cell lymphoma. N Engl J Med. 2017;377(26):2531–2544. doi: 10.1056/NEJMoa1707447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Neelapu SS, Locke FL, Bartlett NL, et al. Long-term follow-up ZUMA-1: a pivotal trial of Axicabtagene Ciloleucel (Axi-Cel; KTE-C19) in patients with refractory aggressive Non-Hodgkin Lymphoma (NHL) Blood. 2017;130(Suppl 1):578. [Google Scholar]
- 45.Turtle CJ, Hanafi LA, Berger C, et al. Immunotherapy of non-Hodgkin’s lymphoma with a defined ratio of CD8+ and CD4+ CD19-specific chimeric antigen receptor-modified T cells. Sci Transl Med. 2016;8(355):355ra116. doi: 10.1126/scitranslmed.aaf8621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kochenderfer JN, Somerville RPT, Lu T, et al. Lymphoma remissions caused by Anti-CD19 chimeric antigen receptor T cells are associated with high serum interleukin-15 levels. J Clin Oncol. 2017;35(16):1803–1813. doi: 10.1200/JCO.2016.71.3024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Locke FL, Neelapu SS, Bartlett NL, et al. Phase 1 results of ZUMA-1: a Multicenter Study of KTE-C19 Anti-CD19 CAR T cell therapy in refractory aggressive lymphoma. Mol Ther. 2017;25(1):285–295. doi: 10.1016/j.ymthe.2016.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kochenderfer JN, Somerville RPT, Lu T, et al. Long-duration complete remissions of diffuse large B cell lymphoma after Anti-CD19 chimeric antigen receptor T cell therapy. Mol Ther. 2017;25(10):2245–2253. doi: 10.1016/j.ymthe.2017.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee DW, Kochenderfer JN, Stetler-Stevenson M, et al. T cells expressing CD19 chimeric antigen receptors for acute lymphoblastic leukaemia in children and young adults: a phase 1 dose-escalation trial. Lancet. 2015;385(9967):517–528. doi: 10.1016/S0140-6736(14)61403-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maude SL, Frey N, Shaw PA, et al. Chimeric antigen receptor T cells for sustained remissions in leukemia. N Engl J Med. 2014;371(16):1507–1517. doi: 10.1056/NEJMoa1407222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Maus MV, June CH. Making better chimeric antigen receptors for adoptive T-cell therapy. Clin Cancer Res. 2016;22(8):1875–1884. doi: 10.1158/1078-0432.CCR-15-1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Roberts ZJ, Better M, Bot A, Roberts MR, Ribas A. Axicabtagene ciloleucel, a first-in-class CAR T cell therapy for aggressive NHL. Leuk Lymphoma. 2017 Oct 23; doi: 10.1080/10428194.2017.1387905. Epub. [DOI] [PubMed] [Google Scholar]
- 53.Wang X, Riviere I. Clinical manufacturing of CAR T cells: foundation of a promising therapy. Mol Ther Oncolytics. 2016;3:16015. doi: 10.1038/mto.2016.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Better M, Chiruvolu V, Oliver J, et al. 287. Production of KTE-C19 (Anti-CD19 CAR T Cells) for ZUMA-1: a Phase 1/2 Multi-Center Study evaluating safety and efficacy in subjects with refractory aggressive Non-Hodgkin Lymphoma (NHL) Mol Ther. 2016;24(Suppl 1):S115. [Google Scholar]
- 55.Cheson BD. The International Harmonization Project for response criteria in lymphoma clinical trials. Hematol Oncol Clin North Am. 2007;21(5):841–854. doi: 10.1016/j.hoc.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 56.Cheson BD, Fisher RI, Barrington SF, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014;32(27):3059–3068. doi: 10.1200/JCO.2013.54.8800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kochenderfer JN, Dudley ME, Kassim SH, et al. Chemotherapy-refractory diffuse large B-cell lymphoma and indolent B-cell malignancies can be effectively treated with autologous T cells expressing an anti-CD19 chimeric antigen receptor. J Clin Oncol. 2015;33(6):540–549. doi: 10.1200/JCO.2014.56.2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lossos IS, Paltiel O, Polliack A. Salvage chemotherapy using a combination of fludarabine and cyclophosphamide for refractory or relapsing indolent and aggressive non-Hodgkin’s lymphomas. Leuk Lymphoma. 1999;33(1–2):155–160. doi: 10.3109/10428199909093737. [DOI] [PubMed] [Google Scholar]
- 59.Zaja F, Rogato A, Russo D, Marin L, Silvestri F, Baccarani M. Combined therapy with Fludarabine and cyclophosphamide in relapsed/resistant patients with B-cell chronic lymphocytic leukaemia and non-Hodgkin’s lymphomas. Eur J Haematol. 1997;59(5):327–328. doi: 10.1111/j.1600-0609.1997.tb01694.x. [DOI] [PubMed] [Google Scholar]
- 60.Redman JR, Cabanillas F, Velasquez WS, et al. Phase II trial of fludarabine phosphate in lymphoma: an effective new agent in low-grade lymphoma. J Clin Oncol. 1992;10(5):790–794. doi: 10.1200/JCO.1992.10.5.790. [DOI] [PubMed] [Google Scholar]
- 61.Schuster SJ, Svoboda J, Chong EA, et al. Chimeric antigen receptor T cells in refractory B-cell lymphomas. N Engl J Med. 2017;377(26):2545–2554. doi: 10.1056/NEJMoa1708566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Abramson JS, Palomba ML, Gordon LI, et al. High durable CR rates in Relapsed/Refractory (R/R) aggressive B-NHL treated with the CD19-directed CAR T cell product JCAR017 (TRANSCEND NHL 001): defined composition allows for dose-finding and definition of pivotal cohort. Blood. 2017;130:581. [Google Scholar]
- 63.Jain MD, Davila ML. Concise review: emerging principles from the clinical application of chimeric antigen receptor T cell therapies for B cell malignancies. Stem Cells. 2018;36(1):36–44. doi: 10.1002/stem.2715. [DOI] [PubMed] [Google Scholar]
- 64.Neelapu SS, Locke FL, Bartlett NL, et al. Axicabtagene ciloleucel CAR T-cell therapy in refractory large B-cell lymphoma. N Engl J Med. 2017;377(26):2531–2544. doi: 10.1056/NEJMoa1707447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Locke FL, Rossi J, Neelapu SS, et al. Product characteristics associated with in vivo expansion of anti-CD19 CAR T cells in patients treated with axicabtagene ciloleucel (axi-cel) J Clin Oncol. 2017;35(15 Suppl):3023. [Google Scholar]
- 66.Neelapu SS, Tummala S, Kebriaei P, et al. Chimeric antigen receptor T-cell therapy – assessment and management of toxicities. Nat Rev Clin Oncol. 2018;15(1):47–62. doi: 10.1038/nrclinonc.2017.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lee DW, Gardner R, Porter DL, et al. Current concepts in the diagnosis and management of cytokine release syndrome. Blood. 2014;124(2):188–195. doi: 10.1182/blood-2014-05-552729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Davila ML, Riviere I, Wang X, et al. Efficacy and toxicity management of 19-28z CAR T cell therapy in B cell acute lymphoblastic leukemia. Sci Transl Med. 2014;6(224):224ra225. doi: 10.1126/scitranslmed.3008226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gust J, Hay KA, Hanafi LA, et al. Endothelial activation and blood-brain barrier disruption in neurotoxicity after adoptive immunotherapy with CD19 CAR-T cells. Cancer Discov. 2017;7(12):1404–1419. doi: 10.1158/2159-8290.CD-17-0698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hay KA, Hanafi LA, Li D, et al. Kinetics and biomarkers of severe cytokine release syndrome after CD19 chimeric antigen receptor-modified T-cell therapy. Blood. 2017;130(21):2295–2306. doi: 10.1182/blood-2017-06-793141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Locke FL, Anasetti C, Moffitt Immunotherapy Working Group and the Immune Cell Therapy (ICE-T) Program Transplanters drive CARs to the clinic by brewing ICE-T: the Moffitt roadmap. J Immunother Cancer. 2017;5(1):59. doi: 10.1186/s40425-017-0265-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Levine BL, Miskin J, Wonnacott K, Keir C. Global manufacturing of CAR T cell therapy. Mol Ther Methods Clin Dev. 2017;4:92–101. doi: 10.1016/j.omtm.2016.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rosenbaum L. Tragedy, perseverance, and chance – The story of CAR-T therapy. N Engl J Med. 2017;377(14):1313–1315. doi: 10.1056/NEJMp1711886. [DOI] [PubMed] [Google Scholar]