Abstract
Policy Points:
For more than 3 decades, international development agencies have advocated health system decentralization to improve health system performance in low‐ and middle‐income countries.
We found little rigorous evidence documenting the impact of decentralization processes on health system performance or outcomes in part due to challenges in measuring such far‐reaching and multifaceted system‐level changes.
We propose a renewed research agenda that focuses on discrete definitions of decentralization and how institutional factors and mechanisms affect health system performance and outcomes within the general context of decentralized governance structures.
Context
Despite the widespread adoption of decentralization reforms as a means to improve public service delivery in developing countries since the 1980s, empirical evidence of the role of decentralization on health system improvement is still limited and inconclusive. This study reviewed studies published from 2000 to 2016 with adequate research designs to identify evidence on whether and how decentralization processes have impacted health systems.
Methods
We conducted a systematic review of peer‐reviewed journal articles from the public health and social science literature. We searched for articles within 9 databases using predefined search terms reflecting decentralization and health system constructs. Inclusion criteria were original research articles, low‐ and middle‐income country settings, quantifiable outcome measures, and study designs that use comparisons or statistical adjustments. We excluded studies in high‐income country settings and/or published in a non‐English language.
Findings
Sixteen studies met our prespecified inclusion and exclusion criteria and were grouped based on outcomes measured: health system inputs (n = 3), performance (n = 7), and health outcomes (n = 7). Numerous studies addressing conceptual issues related to decentralization but without any attempt at empirical estimation were excluded. Overall, we found mixed results regarding the effects of decentralization on health system indicators with seemingly beneficial effects on health system performance and health outcomes. Only 10 studies were considered to have relatively low risks of bias.
Conclusions
This study reveals the limited empirical knowledge of the impact of decentralization on health system performance. Mixed empirical findings on the role of decentralization on health system performance and outcomes highlight the complexity of decentralization processes and their systemwide effects. Thus, we propose a renewed research agenda that focuses on discrete definitions of decentralization and how institutional factors and mechanisms affect health system performance and outcomes within the general context of decentralized governance structures.
Keywords: decentralization, health reform, developing countries
Over the past several decades, countries around the world have implemented decentralization reforms for varying reasons and with varying degrees of success. By the 1990s, it was estimated that at least 80% of the world's countries had implemented some form of decentralization.1 Since then, more countries, particularly in Asia and Africa, have also adopted decentralization.2 Broadly defined as the process of transferring responsibilities and resources from the central government to subnational government entities, decentralization has been promoted as a means to improve allocative efficiency of public goods and services delivery,3, 4 facilitate popular participation in decision making,5, 6 improve the accountability and responsiveness of government,2 maintain state legitimacy and stability,7, 8 and contribute to better democratic governance.9 Because of these rationales, decentralization is being implemented virtually everywhere and has become the most important government reform in the past few decades.2
Decentralization in the health sector in most developing countries was originally promoted by major international development agencies in the 1980s and 1990s.10 Researchers have advanced a number of theoretical and normative arguments that support health sector decentralization primarily related to its purported benefits for public administration, local fiscal issues, and social capital.11 From a public administration perspective, decentralized health systems are thought to ensure responsiveness and flexibility in management systems to meet local needs and better align with the key principles of primary health care service provision.10, 12, 13 Local fiscal theory suggests that, through decentralization, subnational governments will provide an optimal level of public goods and services, thereby reducing waste and satisfying citizens’ preferences and needs.4 From a social capital perspective, decentralized health systems are believed to encourage citizen participation in planning and providing health services.14
While decentralization advocates point to its many purported advantages, skeptics note the potential for less desirable outcomes. For instance, some arguments against decentralization suggest it restricts the central government's role, which may increase economic inequality and may facilitate political control and domination of local elites.10
Despite the widespread adoption of decentralization, empirical evidence of whether decentralization brings actual improvement in public goods and services delivery is still lacking.15 Much of the existing empirical evidence is predominantly based on cross‐national studies or a small number of case studies in one or a few countries based on qualitative evidence with mixed outcomes.16 There have been only 2 review studies to date focusing on the impacts of decentralization.17, 18 Neither study was focused on the relationship between decentralization and health system performance or outcomes. Additionally, both studies were more narrative reviews of the literature that made little attempt to assess the quality of studies or to extract information on decentralization's effectiveness in improving outcomes. Thus, a systematic review focusing on empirical research with rigorous study designs is needed to evaluate existing evidence regarding the effects of decentralization on health system functioning.
The complex nature of relationships between decentralization and health system performance and outcomes poses substantial challenges for testing empirically the theoretical arguments in favor of decentralization. Figure 1 illustrates the complex relationships between decentralization and health outcomes. Decentralization provides discretion or “decision space” that describes the range of possible choices of actions available to subnational governments.11 It determines subnational government actors’ decisions over finance, service organization, human resources, access rules, and governance rules in order to create innovations, facilitate directed changes, or take no action.11 The choice of actions determines the inputs to the health system that will result in health system performance and eventually affect health outcomes at the individual or population level. These relationships can be analyzed in 3 outcome domains, presented as 3 dashed‐line boxes in Figure 1: health system actions and inputs (eg, health system budgets and spending); health system performance outcomes (eg, health insurance coverage, availability of appropriate health services/supplies); and, ultimately, health outcomes (eg, maternal or child health indicators). Institutional capacities within health systems act as mediators,19 while institutional, political, and macroeconomic factors may confound the causal links from decentralization to health outcomes. Population health outcomes are not determined solely by health system performance but also by other determinants outside the health system (eg, initial health status and socioeconomic factors).
Figure 1.
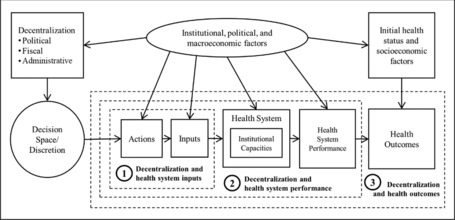
Stylized Causal Link Diagram Between Decentralization and Health Outcomes
In spite of the challenges inherent in classifying and measuring decentralization processes, this study is aimed at contributing to the ongoing efforts for establishing an evidence base regarding whether and how decentralization has contributed to the improvement in health services delivery and outcomes. We conducted a systematic review to identify empirical evidence from studies with adequate research designs on whether decentralization processes have impacted health systems.
Methods
Analytic Overview
This is a systematic review of studies on the effects of decentralization on health system performance and outcomes. We adapted the Institute of Medicine's systematic review guideline to prevent poor reporting in systematic reviews.20 We used the causal link model presented in Figure 1 to organize our data synthesis.
Search Strategy
The following databases were searched for journal articles published from 2000 to 2016: Medline with Full Text, ScienceDirect, Business Source Complete, EconLit with Full Text, Social Sciences Full Text (H.W. Wilson), JSTOR, Scopus, Social Sciences Citation Index, and Public Administration Abstracts. These databases were chosen based on the consideration that they covered literature whose topics fit with this study objective.
“Decentralization” is a broad term that encompasses a number of institutional changes that potentially impact health system performance. For this study, we were interested specifically in devolution, a form of decentralization that entails devolving responsibility, authority, and accountability to lower levels of government units with some degree of political autonomy.21, 22 Devolution has become a global trend since the 2000s, as more countries have adopted devolution compared to the previous period, which was dominated by deconcentration or delegation systems, less ambitious forms of decentralization.21, 23 Under devolution, some responsibilities and resources for health care service provision, particularly for delivering essential health services, are transferred from the central to the subnational governments. These responsibilities may include ensuring the availability of primary health facilities, managing health workers, maintaining continuous stocks of essential medical supplies, and mobilizing funds for the operation and maintenance of health facilities and programs.
Due to possible variations in how the term is used in different fields, we used different related constructs of decentralization as the search terms to include “decentralization,” “deconcentration,” “delegation,” “devolution,” and “decision space” with any possible wording variations. For the health indicators, we used “output,” “outcome,” “performance,” “effect,” “impact,” “equity,” “quality,” “effectiveness,” “efficiency,” and “accountability.” These terms were also combined with health‐specific terms: “health outcomes,” “health status,” “life expectancy,” “immunization,” “mortality,” and “health care/service utilization.” We used Boolean operators to improve precision in the literature search process.
Review Process
Articles were eligible for the review process if they met our prespecified inclusion and exclusion criteria (Table 1). The inclusion criteria were decentralization type (ie, devolution), peer‐reviewed and original research article, time horizon (studies published from 2000 to 2016), quantifiable health indicators as outcome variables (ie, health system inputs, performance, and health outcomes), study design, and low‐ and middle‐income countries as listed in the World Bank's classification of low‐ and middle‐income countries.24 Our decision to include only studies published from 2000 onward was based on consideration of the historical timelines of when decentralization had become widespread among developing countries. Countries in Latin America, Africa, Asia, and Eastern Europe began decentralizing during the late 1980s and 1990s. The World Bank also reported that most of the countries it was assisting were not undergoing some form of decentralization until the late 1990s.21 We decided that searching studies published from 2000 onward would yield good‐quality studies on decentralization, considering the time needed for policy implementation or institutional reform to be fully operational and for sufficient data related to decentralization to be available.
Table 1.
Inclusion and Exclusion Criteria
| Criteria | Definition, Explanation, or Examples |
|---|---|
| Inclusion Criteria | |
| Decentralization type | Decentralization is defined as the transfer of government's responsibility from the upper to lower tier of government through various types of fiscal, political, and administrative instruments43 and implies the strengthening of subnational levels of governments to exercise a degree of autonomy from central government with respect to a defined set of functions12 |
| Peer‐reviewed and original research article |
|
| Time horizon | Articles published from 2000 to 2016 |
| Quantifiable health indicators |
|
| Study design |
|
| Low‐ or middle‐income country setting | Countries categorized as low and middle income by the World Bank |
| Exclusion Criteria | |
| Decentralization type | Deconcentration, delegation, and privatization |
| High‐income country setting |
|
| Non‐English language | Studies published in Spanish, French, Portuguese, Chinese, etc |
In terms of study design, we focused only on “large‐N” studies: those that use a sufficiently large number of subjects or observations that were randomly selected or distributed, and use inferential statistical methods for analyses. The exclusion criteria were other types of decentralization (ie, deconcentration, delegation, and privatization), high‐income country setting, qualitative assessments of outcomes, and non‐English language. (See Figure 2 for a flow diagram.)
Figure 2.
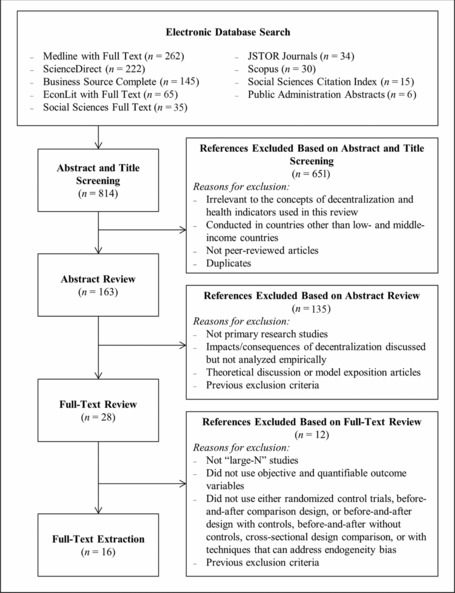
Literature Review Flow Diagram
Data Extraction
From the selected articles, we extracted the following information for analysis: research question, study design (data years, location, unit of analysis, analytic methods, population, sampling method, and data sources), health indicators/outcomes, decentralization constructs, decentralization context (implementation year, level of decentralization, and summary of decentralization policies), and research findings.
Data Synthesis
The final selected studies were grouped following the 3 domains for analyzing the effects of decentralization on health indicators presented in Figure 1: health system inputs, health system performance, and population health outcomes. We did not conduct meta‐analysis because of the variation in outcome measures, key predictors, and study designs. Research findings were synthesized qualitatively in each group in terms of whether the effects of decentralization on health indicators were beneficial, harmful, mixed, or no effect. Each article was assessed for the risks of selection bias and confounding, selective outcome and analysis biases, and other sources of bias. We adapted the quality assessment instrument by Waddington and colleagues25 to assess consistent internal validity of the reviewed studies. We used this instrument because it covers study designs that are commonly used in international development settings (eg, regression discontinuity design, instrumental variable estimation, difference‐in‐difference, matching). Each study was scored in terms of its overall risk of bias as “low risk,” “medium risk,” or “high risk.” (See Online Appendix for the quality assessment instrument and criteria for assessing overall risks of bias.)
Results
Overview of the Studies
Figure 2 presents the flow diagram of the process of identifying and including articles for this review. We initially retrieved 814 titles and abstracts from the database search. We screened out 651 articles that were irrelevant based on our concepts of decentralization and health indicators, were conducted in countries other than low‐ and middle‐income countries, were not peer‐reviewed articles, or were duplicates. From the remaining 163 articles, we excluded 135 articles through abstract review and selected 16 articles after full‐text review for data extraction. The primary reasons for exclusion during abstract review were that the study did not measure quantitative or empirical outcomes or used different concepts of decentralization.
We included only those studies that fit our definition of decentralization: the devolution of responsibility, authority, and accountability to lower levels of government units with some degree of political autonomy.21, 22 This more intensive form of decentralization is not as well studied as other forms of decentralization. We excluded a substantial number of studies that used “decentralization” in terms of relocation or expansion of the physical location of service provisions. These studies often focused on efforts to move disease prevention, diagnosis, and medical treatment from hospitals to health centers with the aim to improve access and reduce patients’ travel distance to health care service providers. We excluded these because they were not measuring the decentralization of decision‐making authority but rather represented a top‐down service delivery intervention. We also excluded studies that used “delegation” because they referred to “task‐shifting,” which means the extension of the scopes of practice of nonphysicians or community health workers to assume some tasks previously undertaken by professional health workers.
Table 2 reports the characteristics of the articles selected for review. Sixteen different studies were identified, with the earliest one published in 2003 and the most recent one published in 2016.16, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40 The selected studies were situated in Latin America (n = 8), Asia (n = 5), Africa (n = 2), and multiple countries (n = 1). The unit of analysis varied and included country (n = 1), state/province (n = 4), district/municipality (n = 7), household (n = 2), and individual level (n = 2). In terms of the study design, we did not find any randomized controlled trials (RCTs), and therefore all selected studies relied on quasi‐experimental designs. The studies used cross‐sectional analysis (n = 3) or longitudinal analysis (n = 13); of the latter, 11 were based on panel data and 2 were based on repeated cross‐sectional. Among all studies, only 4 employed individual‐level analysis using individual or household data from survey data,30, 32, 34, 39 whereas the remaining studies used the ecological analysis approach. The analytical methods that were used in the studies varied from fixed effects, modified difference‐in‐difference, instrumental variable estimation, multilevel modeling, and regression‐based analyses. For ease of reporting, we classified articles by the 3 domains of relationships presented in Figure 1: health system inputs, performance, and population health outcomes.
Table 2.
Characteristics of Studies
| Characteristics | N |
|---|---|
| Study location | |
| • Multiple countries | 1 |
| • Asia | 5 |
| • Africa | 2 |
| • Latin America | 8 |
| Unit of analysis | |
| • Country | 1 |
| • State/province | 4 |
| • District/municipality | 7 |
| • Household | 2 |
| • Individual | 2 |
| Study design | |
| • Panel study | 11 |
| • Repeated cross‐sectional | 2 |
| • Cross‐sectional | 3 |
| Analytical approach | |
| • Individual‐level analysis | 4 |
| • Ecological analysis | 12 |
The Overall Effects of Decentralization on Health Indicators
In general, we uncovered mixed findings about the effects of decentralization on health system inputs, performance, and outcomes. Tables 3, 4, and 5 report the summary of reviewed articles examining the effects of decentralization on health system inputs, health system performance, and health outcomes, respectively.
Table 3.
Summary of Findings on the Effects of Decentralization on Health System Inputs
| Author(s), (Year), Country | Study Design, Unit of Analysis, Data Year | Implementation of Decentralization | Decentralization Variables | Health Indicators | Effects, Magnitude |
|---|---|---|---|---|---|
|
|
|
Fiscal resource control: The percentage of local government budget financed by local sources | Budget shares for health sector and other sectors | No significant effect |
| Decentralization maturity: Years since receipt of the unconditional grant | Harmful effect: Districts receiving unconditional grant for more than 3 years allocated 0.16% to 0.20% less in all public goods spending | ||||
|
|
Fiscal, administrative, and political administration were implemented starting in 2001 in all provinces and districts | Fiscal resource control: District's per capita revenue | District's per capita public health spending |
|
|
|
Decentralization of the health care provision was implemented in 1988; anticorruption program started in 2003 | Fiscal resource control: The percentage of total health expenditure financed locally | Number of financial transaction irregularities classified as corruption | No significant effect |
| Administrative control: The percentage of production of outpatient services under local management | No significant effect |
Table 4.
Summary of Findings on the Effects of Decentralization on Health System Performance
| Author(s), (Year), Country | Study Design, Unit of Analysis, Data Year | Implementation of Decentralization | Decentralization Variables | Health Indicators | Effects, Magnitude |
|---|---|---|---|---|---|
|
|
|
Fiscal resource control: Local own revenue (local taxes and charges) as a share of total expenditure | Change in the poor population covered by public health insurance | Beneficial effect: An increase of health expenditure by 1 standard deviation is associated with the expansion of health insurance coverage by 2.33%‐14.07% |
| Provincial/central control: A dummy variable indicating if a municipality is certified to receive transfers directly from central government | Beneficial effect: A municipality that has certification is more likely to expand its health insurance coverage by 8.4%‐12.6% | ||||
|
|
Fiscal, administrative, and political administration were implemented starting in 2001 in all provinces and districts | The timing of decentralization: A dummy variable indicating if a birth delivery took place after the implementation of decentralization (2001) | Facility‐based delivery (a dummy variable indicating if a birth delivery took place in a medical facility) |
|
|
|
|
The timing of decentralization: A set of dummy variables indicating if observation belongs to one of the decentralization periods | A dummy variable of whether a respondent utilized a skilled birth attendant |
|
|
|
Varied from one country to another | The adoption of decentralization framework: A dummy variable indicating if a country adopted decentralization policy |
|
|
|
|
Fiscal, administrative, and political administration were implemented starting in 2001 in all provinces and districts | Fiscal commitment to health sector: The ratio of local public expenditure on health to total local public expenditure |
|
No significant effect |
|
|
|
The adoption of decentralization: A dummy variable indicating if the household is served by decentralized health providers (health care services providers managed by the state government) | Utilization of preventive services |
|
| Out‐of‐pocket health expenditures |
|
||||
|
|
Fiscal, administrative, and political administration were implemented starting in 2001 in all provinces and districts | Fiscal commitment to health sector: District per capita public health spending | Outpatient health care utilization rates |
|
| Household out‐of‐pocket health spending | No significant effect |
Table 5.
Summary of Findings on the Effects of Decentralization on Health Outcomes
| Author(s), (Year), Country | Study Design, Unit of Analysis, Data Year | Implementation of Decentralization | Decentralization Variables | Health Indicators | Effects, Magnitude |
|---|---|---|---|---|---|
|
|
Expenditure decentralization reform in health sector was announced in 1997 as part of the Health Sector Reform Program, 1995‐2000 |
|
Infant mortality rate | No significant effect |
| The timing of decentralization: A dummy variable indicating if the observation takes place in the period before or after the decentralization reform | |||||
|
|
The Family Health and Community Health Agents programs were expanded in 1996; responsibilities for managing primary care clinics, health centers, and health posts were transferred to municipal government control | Administrative control: The proportion of ambulatory care facilities directly under control of the municipal government | Postneonatal mortality |
|
|
|
|
Fiscal resource control: The ratio of provincially controlled resources to total provincial resources | Infant mortality rate |
|
|
Fiscal resource control: The ratio of provincial taxes to total provincially controlled resources |
|
|||
|
|
The systematic change to a decentralized fiscal system from a centralized one was started in 1994 by the passage of the 1994 Tax Sharing System (TSS) | Fiscal resource control: The ratio of per capita provincial budgetary expenditures to the sum of per capita central budgetary expenditures and per capita provincial budgetary expenditures | Infant mortality rate |
|
| Timing of decentralization: A dummy variable indicating if the observation was in the period after the 1994 TSS reform |
|
||||
|
|
|
Fiscal resource control: The share of overall health expenditures financed by municipalities’ own resources | Infant mortality rates up to the age of 1 year and up to the age of 5 years | No significant effect |
|
|
The reassignment of government functions and responsibilities for providing health services across different levels of government began in 1993 | Fiscal resource control: Locally controlled health expenditure as a proportion of total health expenditure | Infant mortality rate |
|
|
|
The systematic change to a decentralized fiscal system from a centralized one was started in 1994 by the passage of the 1994 Tax Sharing System (TSS); fiscal transfer has played a substantial role in bridging fiscal gaps since then | Fiscal resource control: The ratio of total counties’ expenditure to total counties’ revenue within the province (vertical balance) | Infant mortality rate |
|
| Fiscal resource control: The ratio of counties’ expenditure to total provincial expenditure (fiscal capacity relative to other counties) |
|
In terms of the effects of decentralization on health system inputs, 2 of the 3 studies showed adverse effects of decentralization,26, 40 and 1 study did not find significant effects of decentralization on corruption.35 The impact of decentralization on health system performance was investigated in 7 studies and showed mixed findings.16, 30, 32, 33, 34, 39, 40 Two studies showed beneficial effects,16, 40 3 studies showed mixed results,30, 32, 33 1 study showed harmful effects,39 and 1 study showed no significant effects.34
The impact of decentralization on health outcomes seemed to show consistently beneficial effects. There were 7 studies whose outcome variables were classified in the health outcomes domain.27, 28, 29, 31, 36, 37, 38 More than half of the studies reported beneficial effects of decentralization in reducing infant and postneonatal mortality.28, 29, 37, 38 Two studies did not find significant associations.27, 36 Interestingly, 2 studies from Brazil28, 36 and another 2 studies from China31, 38 reported contradicting results between them.
Effects of Decentralization on Health System Inputs
Among the purported benefits of decentralization is that it improves the efficiency of resource allocation and increases overall health care spending in low‐ and middle‐income countries. However, 2 of 3 studies examining the effects of decentralization on health system inputs (ie, resource allocations; Figure 1, box 1) seemed to show consistently harmful effects despite differences in the decentralization constructs and the outcome variables used. Although Akin, Hutchinson, and Strumpf did not find significant effect of the fiscal autonomy on health spending in Uganda,26 they found that as the districts progressed further into the decentralization process, they allocated less money for public goods and primary health care. A study by Kruse, Pradhan, and Sparrow found that each additional 1% increase in local revenue was associated with a 0.88% increase in total public health spending.40 This finding suggests that an increase in local revenue does not translate into an equal rate of increase in public health spending.
Effects of Decentralization on Health System Performance
Health system decentralization is believed to increase the provision of basic services, thereby improving health system performance. However, studies on the effects of decentralization on health system performance (Figure 1, box 2) showed mixed findings (Table 4). This may be attributed to variations among studies in outcome variables, decentralization constructs, and study designs used. In terms of outcome variables, measures of health system performance varied across studies and included the change in the population of low‐income individuals covered by public health insurance,16 delivery in health facilities,30 utilization of skilled birth attendants,32 coverage rates of immunization and complete immunization status among children,33, 34 utilization of preventive and outpatient services,39, 40 and out‐of‐pocket health expenditures.39, 40 The decentralization variables used in these studies also reflect the different ways in which decentralization reforms are conceptualized: from the degree of control over fiscal resources16 and the degree of control by higher levels of government,16 to the timing of decentralization,30, 32 to the adoption of a decentralization framework33, 39 and the degree of mobilized health resources.34, 40
Studies categorized in the health system performance domain used different study designs and analytic methods. Studies reporting beneficial effects of decentralization used longitudinal study designs at various levels of aggregation. Faguet and Sánchez used panel data on budgets and financial flows linked with cross‐sectional data on demographic, infrastructural, institutional, and social variables.16 This allowed them to employ panel estimation and exploit the gradual nature of decentralization reforms in Colombia. Kengia, Igarashi, and Kawabuchi used individual‐level data from the 4 waves of the Tanzanian Demographic Health Survey to reflect the timing of decentralization reforms and found that the health system reforms accompanied by full‐scale implementation of decentralization have increased the utilization of skilled birth attendants among poor women and reduced disparity in the utilization of skilled birth attendants across socioeconomic groups.32
Studies that reported negative effects of decentralization also used different health system performance measures and units of analysis. Hodge, Firth, Jimenez‐Soto, and Trisnantoro used repeated cross‐sectional data that were constructed from 5 waves of the Indonesia Demographic and Health Survey to reflect periods before and after the implementation of decentralization policy in 2001.30 They found that the disparity of facility‐based birth delivery between Java/Bali region, the most developed region in Indonesia, and all other island groups has worsened following decentralization. Bustamante used cross‐sectional data from a 2003 household survey and compared 2 different population groups: households served by the state‐controlled health care providers and households served by the centrally managed health care providers.39 The study found that households reached by health providers managed in the decentralized system paid higher out‐of‐pocket costs compared to those served by health providers under the centralized regime.39
A cross‐country analysis by Khaleghian used panel data on 57 low‐income and 81 middle‐income countries from 1980 to 1997.33 The study exploited the variation in adoption timing of decentralization policies among low‐ and middle‐income countries to compare outcomes between decentralized and centralized countries over time. Khaleghian found that decentralization is associated with higher immunization coverage rates in low‐income countries but lower coverage rates in middle‐income countries. Maharani and Tampubolon used cross‐sectional survey data to predict complete immunization status of children aged 12–23 months using multilevel modeling and did not find significant effects of fiscal decentralization on outcome.34
Effects of Decentralization on Health Outcomes
Studies focused on the effects of decentralization on health outcomes (Figure 1, box 3) showed relatively consistent beneficial effects, with some studies showing contradictory findings and insignificant effects (Table 5). The majority of studies used infant mortality rate as the outcome measure and used fiscal autonomy variables as the main decentralization constructs.
Two studies from Brazil and 2 studies from China showed different results between them. In the Brazilian studies, the most recent study did not find a significant effect,36 while the older one found a significant beneficial effect.28 The 2 Chinese studies also reported different findings, with the most recent one reporting harmful effects of decentralization, noting that expanded provincial fiscal autonomy was associated with an increase in infant mortality.31, 38
Both Brazilian studies used similar study design, a longitudinal ecological analysis using panel data at the municipal level. Both studies also used a fixed‐effects model, but only Rocha, Orellano, and Nishijima used an instrumental variable approach for panel data to correct for potential endogeneity bias.36 These studies also used different decentralization constructs as key predictors. Guanais and Macinko used the proportion of ambulatory care facilities directly under control of the municipal government, which reflects the degree of administrative control,28 whereas Rocha, Orellano, and Nishijima used the share of overall health expenditures financed by municipalities’ own resources, which reflects the degree of fiscal control over resources.36
Studies on China's decentralization used the same unit of analysis (province) but different analytic approaches. Uchimura and Jütting accounted for total counties’ expenditure within the province to construct the vertical fiscal balance and ratio of county expenditure to total provincial expenditure.38 Jin and Sun, conversely, used the ratio of per capita provincial budgetary expenditures to the sum of per capita central budgetary expenditures and per capita provincial budgetary expenditures.31 Unlike the other study, Jin and Sun used data points that cover observations before and after the 1994 Tax Sharing System reform and implemented instrument variable estimation to deal with potential omitted variable biases.
Quality Assessment
We assessed each study's quality based on the study's efforts in identifying and mitigating potential risks of endogeneity bias. Table 6 presents the summary of quality assessment of studies being reviewed (see Online Appendix Table A for the complete results of quality assessment). Only 10 studies were considered to have relatively low risks of bias.16, 27, 30, 31, 33, 34, 37, 38, 39, 40 These studies showed mixed results: 3 studies showed beneficial effects,16, 37, 38 3 studies showed mixed effects,30, 33, 40 2 studies showed harmful effects,31, 39 and 2 studies showed an insignificant effect of decentralization.27, 34
Table 6.
Summary of Study Quality Assessment Resultsa
| Author(s) | Study Design (Analysis Method) | Selection Bias and Confounding Addressed? | Selective Reporting Bias Addressed? | Other Sources of Bias Addressed? | Overall Risk of Bias Assessment | Effects |
|---|---|---|---|---|---|---|
| Akin, Hutchinson, and Strumpf26 | Longitudinal ecological analysis (Ordinary least squares with year dummy) | Unclear | Yes | Unclear | High risk | Mixed |
| Bustamante39 | Cross‐sectional, individual‐level analysis (Log‐linear and probit regression) | Yes | Yes | Unclear | Low risk | Harmful |
| Faguet and Sánchez16 | Longitudinal ecological analysis (Instrumental variable estimation) | Yes | Yes | Yes | Low risk | Beneficial |
| Fritscher and Zamora27 | Longitudinal ecological analysis (Fixed effects/modified difference‐in‐difference) | Yes | Yes | Unclear | Low risk | No effect |
| Guanais and Macinko28 | Longitudinal ecological analysis (Fixed effects) | Yes | Unclear | Unclear | Medium risk | Beneficial |
| Habibi and colleagues29 | Longitudinal ecological analysis (Fixed effects) | Unclear | Yes | Unclear | High risk | Beneficial |
| Hodge, Firth, Jimenez‐Soto, and Trisnantoro30 | Repeated cross‐sectional, individual‐level analysis (Multilevel modeling) | Yes | Yes | Unclear | Low risk | Mixed |
| Jin and Sun31 | Longitudinal ecological analysis (Fixed effects) | Yes | Yes | Unclear | Low risk | Harmful |
| Kengia, Igarashi, and Kawabuchi32 | Repeated cross‐sectional, individual‐level analysis (Regression) | Unclear | Unclear | Unclear | High risk | Mixed |
| Khaleghian33 | Longitudinal ecological analysis (Fixed effects) | Yes | Yes | Yes | Low risk | Mixed |
| Kruse, Pradhan, and Sparrow40 | Longitudinal ecological analysis (Fixed effects) | Yes | Yes | Yes | Low risk | Mixed |
| Maharani and Tampubolon34 | Cross‐sectional, individual analysis (Multilevel modeling) | Yes | Yes | Unclear | Low risk | No effect |
| Peixoto, Rocha, Nishijima, and Postali35 | Cross‐sectional ecological analysis (Regression) | Unclear | Unclear | Unclear | High risk | No effect |
| Rocha, Orellano, and Nishijima36 | Longitudinal ecological analysis (Fixed effects and instrumental variable estimation) | Yes | Unclear | Unclear | Medium risk | No effect |
| Soto, Farfan, and Lorant37 | Longitudinal ecological analysis (Fixed effects) | Yes | Yes | Unclear | Low risk | Beneficial |
| Uchimura and Jütting38 | Longitudinal ecological analysis (Fixed effects) | Yes | Yes | Unclear | Low risk | Beneficial |
The quality assessment instrument was adapted from Waddington and colleagues25 and is available in the Online Appendix. A full report of quality assessment is available in Online Appendix Table A.
Discussion
We conducted a systematic review to evaluate empirical evidence of the effects of decentralization on health indicators. Sixteen studies met our inclusion criteria and represent the empirical research published since 2000 analyzing the effects of decentralization on health indicators in low‐ and middle‐income countries. We classified the selected articles in 3 domains of health indicators following the framework presented in Figure 1: inputs, performance, and health outcomes. In general, the studies showed mixed results with seemingly beneficial effects of decentralization on health system performance and health outcomes on average. However, the findings of these studies were not comparable because they focused on different aspects of decentralization and used different outcome measures.
The majority of studies in the health system inputs domain found harmful effects of decentralization on resource allocation for the health sector through budget allocation.26, 40 The findings contradict allocative efficiency arguments advanced in the decentralization literature, which suggest that, in decentralized systems, local governments are better able to match the provision of local public goods with local preferences.4 For instance, the Uganda26 and Indonesia40 cases, which exhibited similar processes of decentralization in which decision making in budget allocation was transferred to the local level, showed that decentralization had somewhat harmful effects on local health spending. One of the possible explanations is that transferring discretionary power of fiscal decisions to local governments may be insufficient without improving local accountability. In Brazil, expanded discretion to include citizens’ views on public resource allocation seemed to be associated with beneficial effects.41 Brazilian municipalities that adopted participatory budgeting processes allocated more resources for the health sector compared with municipalities that did not adopt participatory budgeting.41 In Indonesia, despite the mandate to incorporate citizen participation into the budget decision‐making process, the participatory mechanisms failed to provide meaningful channels for citizens to influence budget decisions.42 Potentially beneficial effects of decentralization on health system inputs seem to be substantially conditioned by the presence of effective governance mechanisms that enable responsiveness to local needs and values.18
The mixed findings, particularly among studies focusing on the effects of decentralization on health system performance, may be attributed to the different ways decentralization concepts and outcome measures were operationalized. This finding underscores the fact that the decentralization concept encompasses multiple meanings and dimensions (eg, political, administrative, and fiscal).43 For instance, some studies used fiscal autonomy measures to reflect the level of fiscal discretion that the subnational governments need to finance programs and interventions contributing to improvements in health system performance. Some studies used per capita health spending or the ratio of health expenditure to total expenditure as measures of subnational governments’ commitments to allocate health resources. Other studies used the percentage of outpatient services produced by local authorities to reflect the level of administrative responsibility in providing health services. These measures may not capture equally well the effect of decentralization processes. Each makes the tacit assumption that the observed variation in these exposures is due exclusively to decentralization. In addition to varying “exposure” measures, outcome measures used in the studies also differed substantially. Performance measures ranged from the immunization status of children, to the utilization of preventive services, to individual and household out‐of‐pocket spending. These variations impede efforts to assess overall impacts of decentralization.
Due to the complex nature of the decentralization process, rigorous study designs are needed to determine the true effects of decentralization on the improvement of health systems. We did not find RCT studies in this review. However, studies that use quasi‐experimental techniques can also produce valid causal inferences when well implemented.44 Ten studies that were considered to have relatively low risks of bias used various analytical methods, such as fixed effects, difference‐in‐difference, instrumental variables, and multilevel modeling. These studies showed mixed findings. One study focused on the effects of decentralization on health system inputs,40 6 studies focused on health system performance,16, 30, 33, 34, 39, 40 and 4 studies focused on health outcomes.27, 31, 37, 38 In terms of the effects of decentralization on health system performance, only 1 study showed beneficial effects,16 while the rest of the studies showed mixed, harmful, or insignificant effects. The effects of decentralization on health outcomes were inconclusive due to the opposing findings among the studies.
Mixed findings among these studies might be attributed to various factors. Variations in countries’ specific conditions and decentralization designs may explain these differences. For instance, the decentralization process in Colombia took place in a phased manner from the 1970s to the 2000s,16 whereas decentralization in Indonesia was implemented as a sudden policy change in 2001.30 Therefore, measured effects in these studies were only relevant to the corresponding countries being studied. Another explanation is that model specifications implemented in these studies may not capture the complex nature of relationships. In particular, studies focusing on the relationships between decentralization and health outcomes are more vulnerable to confounders than studies that focus on more proximal variables such as health system inputs and performance. Moreover, variations in data quality and methods of measurement may also affect the estimation results. For instance, all of the reviewed studies on the effects of decentralization on health outcomes used infant and postneonatal mortality rates as outcome variables. These rates are calculated using civil registration, national census, or population‐based surveys. However, many developing countries do not have well‐functioning civil registry systems and must use mortality estimates derived from survey data, which may affect the validity and reliability of the measurements.
This systematic review reveals some gaps in the literature on decentralization and health system outcomes. Our knowledge of the role of decentralization in the improvement of health systems is still severely limited. Only 3 studies focused on health system inputs and only 1 of them was considered to have low risk of bias. Other aspects of health system inputs have not been studied sufficiently, such as the effects of decentralization on health workforces, infrastructure and technology, and medical supplies. Numerous studies have looked at different aspects of health system performance and health outcomes, but only a few were considered rigorous. More robust evidence from rigorous empirical studies is still needed. The mixed findings across studies suggest that the effects of decentralization on health systems are conditioned by countries’ specific contexts and decentralization designs. Beneficial effects from one country may not be generalizable to another country because of the differences in historical trajectories, social and political contexts, and decentralization designs. It is also worth noting that the mixed findings from this review do not necessarily imply that health system decentralization reforms are not worth pursuing in practice. Decentralization is a complex process (or set of processes) and our understanding of it is still limited; more rigorous empirical research is warranted to inform decentralization reforms.
Future Research
Future research is still needed to build our understanding of how decentralization can deliver beneficial results. The findings of this review support the call for developing a more discrete definition of decentralization that focuses on specific processes that are being decentralized and their interactions as opposed to generalized definitions of decentralization.45 Bossert's “decision space” approach can provide a framework for analyzing decentralization in terms of the range of choice or discretion owned by the local officials over various government functions.11 This framework can assist researchers to determine key aspects of decentralization that may contribute to changes in performance and outcomes under decentralization. Future research also needs to build understanding about various institutional and governance conditions that are essential for decentralization to deliver beneficial results. Some recent conceptual and empirical studies have paved the way in this direction. For instance, studies by Rocha, Orellano, and Nishijima36 and Bossert and Mitchell19 highlight the importance of institutional capacity and quality in decentralized systems to deliver beneficial results. Since decentralization has been adopted in virtually every country in the world, future research may view it as an important background context and focus on how institutional designs and changes following decentralization may contribute to outcomes. Faguet, Fox, and Pöschl argue that decentralization designs that allow for participatory decision making, in which citizens can affect outcomes meaningfully, are important conditions to ensure the effectiveness of decentralized systems.46 An empirical study from Brazil showed that participatory budgeting, a participatory decision‐making instrument in Brazil's decentralization system, has facilitated an allocation of local public expenditures that matched popular preferences for larger shares of health services and contributed to improvement in community health outcomes.41
Limitations
There were some limitations to this systematic review. This review relies on only peer‐reviewed and English‐language journal publications. It excluded potential empirical studies published as “gray literature.” Because decentralization reforms in developing countries have been mostly sponsored by international development aid agencies, much of the research on decentralization may have been published by these institutions through their publication outlets. The exclusion of non‐English‐language publications also excluded potential empirical studies published in non‐English‐speaking countries that have long histories of decentralization such as those in Latin America. The use of quantifiable outcome measures and specific study designs in the inclusion and exclusion criteria also excluded other types of studies that commonly fall under the qualitative research tradition, which might also provide valuable information about decentralization processes. Because this review focused on decentralized systems only, we cannot make an assessment of the relative performance of centralized versus decentralized systems in improving health system delivery.
This systematic review also highlights some challenges of conducting rigorous quantitative research on the impact of decentralization. RCTs, typically regarded as the “gold standard” of impact evaluation, are often infeasible for evaluating the impact of decentralization due to the nature of reforms that often involve large‐scale institutional and regulatory changes across sectors and administrative levels. Such changes inhibit random assignment to treatment and control groups—the cornerstone of the RCT design. Other technical statistical analyses are also available, but they require more restrictive assumptions than the RCT design.47, 48 For instance, instrumental variable estimation method relies on good instrumental variables, which are not often readily available.47 Panel data analysis methods, which may allow for making inferences about the dynamic of change from reforms over time,49 require good panel data, which might not be readily available in many developing countries. Alternatively, good qualitative evaluation studies may also provide important insights into how or why certain decentralization reforms can or cannot deliver changes in the outcomes of interest. Although qualitative studies have been traditionally excluded from systematic reviews,50 systematic and rigorous efforts for searching, appraising, and synthesizing findings from qualitative studies on decentralization in health systems must also be undertaken to contribute better understanding of how and why decentralization in health systems works.
This systematic review highlights the fact that despite the widespread adoption of decentralization in low‐ and middle‐income countries since the 1990s, our understanding of the role of decentralization in the effectiveness of public goods and services delivery is still limited. Because the global movement toward decentralization has often been motivated on political and ideological grounds, empirical studies on decentralization need to inform gradual changes of decentralization systems to ensure beneficial results. However, the findings of this review reveal that we are still far from understanding which decentralization arrangements deliver better health system performance and outcomes. The best available research measures different aspects and processes of decentralization, which makes findings incomparable across studies. This review also highlights the complexity of decentralization processes and their systemwide effects. Thus, we propose a renewed research agenda that focuses on discrete definitions of decentralization and on how institutional factors and mechanisms affect health system performance and outcomes within the general context of decentralized governance structures.
Supporting information
Appendix: Study's Quality Assessment Instrument
Appendix Table A: Quality Assessment Results of the Reviewed Studies
Funding/Support
Adenantera Dwicaksono received support from the Fulbright‐DIKTI Scholarship.
Conflict of Interest Disclosures: Both authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. No conflicts were reported.
Acknowledgments: The authors are grateful to Erika Martin and Gang Chen from the University at Albany for comments on an early draft.
References
- 1. Manor J. The Political Economy of Democratic Decentralization. Washington, DC: The World Bank; 1999. [Google Scholar]
- 2. Faguet J‐P. Decentralization and governance. World Dev. 2014;53:2‐13. [Google Scholar]
- 3. Musgrave RA. Who should tax, where, and what? In: McLure C, ed. Tax Assignment in Federal Countries. Canberra, Australia: Centre for Research on Federal Financial Relations, Australian National University; 1983. [Google Scholar]
- 4. Tiebout CM. A pure theory of local expenditures In: Fischel WA, ed. The Tiebout Model at Fifty: Essays in Public Economics in Honor of Wallace Oates. Cambridge, MA: Lincoln Institute of Land Policy; 1956:xi‐xxi. [Google Scholar]
- 5. Blair H. Participation and accountability at the periphery: democratic‐local governance in six countries. World Dev. 2000;28(1):21‐39. [Google Scholar]
- 6. Crook RC. Decentralisation and poverty alleviation in developing countries: a comparative analysis or, is West Bengal unique?. IDS working paper 130. http://www.accountabilityindia.in/sites/default/files/documentlibrary/92_1236960610.pdf. Published February 2001. Accessed March 2, 2018.
- 7. Crook RC. Decentralisation and poverty reduction in Africa: the politics of local‐central relations. Public Adm Dev. 2003;23(1):77‐88. [Google Scholar]
- 8. Devas N, Delay S. Local democracy and the challenges of decentralising the state: an international perspective. Local Gov Stud. 2006;32(5):677‐695. [Google Scholar]
- 9. Selee A. Exploring the link between decentralization and democratic governance. In: Tulchin JS, Selee A, eds. Decentralization and Democratic Governance in Latin America. Washington, DC: Woodrow Wilson International Center for Scholars; 2004. [Google Scholar]
- 10. Collins C, Green A. Decentralization and primary health care: some negative implications in developing countries. Int J Health Serv. 1994;24(3):459‐475. [DOI] [PubMed] [Google Scholar]
- 11. Bossert TJ. Analyzing the decentralization of health systems in developing countries: decision space, innovation and performance. Soc Sci Med. 1998;47(10):1513‐1527. [DOI] [PubMed] [Google Scholar]
- 12. Mills A, Vaughan JP, Smith DL, Tabibzadeh I. Health System Decentralization: Concept, Issues and Country Experience. Geneva, Switzerland: World Health Organization; 1990. [Google Scholar]
- 13. Atkinson S. Restructuring health care: tracking the decentralization debate. Prog Hum Geogr. 1995;19(4):486‐503. [Google Scholar]
- 14. Putnam RD. Making Democracy Work: Civic Traditions in Modern Italy. Princeton, NJ: Princeton University Press; 1993. [Google Scholar]
- 15. Atkinson S, Haran D. Back to basics: does decentralization improve health system performance? Evidence from Ceará in north‐east Brazil. Bull World Health Organ. 2004;82(11):822‐827. [PMC free article] [PubMed] [Google Scholar]
- 16. Faguet J‐P, Sánchez F. Decentralization and access to social services in Colombia. Public Choice. 2014;160(1/2):227‐249. [Google Scholar]
- 17. Ghuman BS, Singh R. Decentralization and delivery of public services in Asia. Policy Soc. 2013;32(1):7‐21. [Google Scholar]
- 18. Ciccone DK, T Vian, Maurer L, Bradley EH. Linking governance mechanisms to health outcomes: a review of the literature in low‐ and middle‐income countries. Soc Sci Med. 2014;117:86‐95. [DOI] [PubMed] [Google Scholar]
- 19. Bossert TJ, Mitchell AD. Health sector decentralization and local decision‐making: decision space, institutional capacities and accountability in Pakistan. Soc Sci Med. 2011;72(1):39‐48. [DOI] [PubMed] [Google Scholar]
- 20. Institute of Medicine Finding What Works in Health Care: Standards for Systematic Reviews. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 21. Independent Evaluation Group . Decentralization in Client Countries: An Evaluation of World Bank Support, 1990–2007. Washington, DC: The World Bank; 2008. [Google Scholar]
- 22. Prud'homme R. On the Dangers of Decentralization . World Bank Policy Research working paper 1252. http://documents.worldbank.org/curated/en/218141468739288067/pdf/multi-page.pdf. Published July 2010. Accessed February 12, 2018.
- 23. Rodríguez‐Pose A, Gill N. The global trend towards devolution and its implications. Environ Plann C Gov Policy. 2003;21(3):333‐351. [Google Scholar]
- 24. How does the World Bank classify countries? The World Bank website. https://datahelpdesk.worldbank.org/knowledgebase/articles/378834-how-does-the-world-bank-classify-countries. Accessed August 4, 2016.
- 25. Waddington H, White H, Snilstveit B, et al. How to do a good systematic review of effects in international development: a tool kit. J Dev Effect. 2012;4(3):359‐387. [Google Scholar]
- 26. Akin J, Hutchinson P, Strumpf K. Decentralisation and government provision of public goods: the public health sector in Uganda. J Dev Stud. 2005;41(8):1417‐1443. [Google Scholar]
- 27. Fritscher AM, Zamora CR. An evaluation of the 1997 expenditure decentralization reform in Mexico. Public Finance Rev. 2016;44(5):563‐588. [Google Scholar]
- 28. Guanais FC, Macinko J. The health effects of decentralizing primary care in Brazil. Health Aff (Milwood). 2009;28(4):1127‐1135. [DOI] [PubMed] [Google Scholar]
- 29. Habibi N, Huang C, Miranda D, et al. Decentralization and human development in Argentina. J Hum Dev. 2003;4(1):73‐101. [Google Scholar]
- 30. Hodge A, Firth S, Jimenez‐Soto E, Trisnantoro L. Linkages between decentralisation and inequalities in neonatal health: evidence from Indonesia. J Dev Stud. 2015;51(12):1634‐1652. [Google Scholar]
- 31. Jin Y, Sun R. Does fiscal decentralization improve healthcare outcomes? Empirical evidence from China. Public Finance and Management. 2011;11(3):234‐261. [Google Scholar]
- 32. Kengia JT, Igarashi I, Kawabuchi K. Effectiveness of health sector reforms in reducing disparities in utilization of skilled birth attendants in Tanzania. Tohoku J Exp Med. 2013;230(4):241‐253. [DOI] [PubMed] [Google Scholar]
- 33. Khaleghian P. Decentralization and public services: the case of immunization. Soc Sci Med. 2004;59:163‐183. [DOI] [PubMed] [Google Scholar]
- 34. Maharani A, Tampubolon G. Has decentralisation affected child immunisation status in Indonesia? Global Health Action. 2015;8(1). https://doi.org/10.3402/gha.v7.24913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Peixoto SGD, Rocha F, Nishijima M, Postali FAS. Decentralization and corruption: evidence from primary health‐care programmes. Appl Econ Lett. 2012;19(18):1885‐1888. [Google Scholar]
- 36. Rocha F, Orellano VF, Nishijima M. Health spending autonomy and infant mortality rates: a matter of local administrative capacity? J Dev Areas. 2016;50(2):293‐309. [Google Scholar]
- 37. Soto VE, Farfan MI, Lorant V. Fiscal decentralisation and infant mortality rate: the Colombian case. Soc Sci Med. 2012;74:1426‐1434. [DOI] [PubMed] [Google Scholar]
- 38. Uchimura H, Jütting JP. Fiscal decentralization, Chinese style: good for health outcomes? World Dev. 2009;37:1926‐1934. [Google Scholar]
- 39. Bustamante AV. The tradeoff between centralized and decentralized health services: evidence from rural areas in Mexico. Soc Sci Med. 2010;71:925‐934. [DOI] [PubMed] [Google Scholar]
- 40. Kruse I, Pradhan M, Sparrow R. Marginal benefit incidence of public health spending: evidence from Indonesian sub‐national data. J Health Econ. 2012;31:147‐157. [DOI] [PubMed] [Google Scholar]
- 41. Gonçalves S. The effects of participatory budgeting on municipal expenditures and infant mortality in Brazil. World Dev. 2014;53:94‐110. [Google Scholar]
- 42. Blair H. Participatory budgeting and local governance. Swedish International Center for Local Democracy working paper 10. https://icld.se/static/files/forskningspublikationer/icld-workingpaper-10-tryck-low.pdf. Published 2012. Accessed March 2, 2018.
- 43. Litvack J, Ahmad J, Bird R. Rethinking Decentralization in Developing Countries. Washington, DC: The World Bank; 1998. [Google Scholar]
- 44. Duvendack M, Hombrados JG, Palmer‐Jones R, Waddington H. Assessing ‘what works’ in international development: meta‐analysis for sophisticated dummies. J Dev Effect. 2012;4(3):456‐471. [Google Scholar]
- 45. Bossert TJ. Empirical studies of an approach to decentralization: “decision space” in decentralized health systems In: Faguet J‐P, Pöschl C, eds. Is Decentralization Good for Development? Perspective from Academics and Policy Makers. Oxford, England: Oxford University Press; 2015. [Google Scholar]
- 46. Faguet J‐P, Fox AM, Pöschl C. Decentralizing for a deeper, more supple democracy. J Democr. 2015;26(4):60‐74. [Google Scholar]
- 47. Deaton A. Instruments, randomization, and learning about development. J Econ Lit. 2010;48(2):424‐55. [Google Scholar]
- 48. Duflo E, Kremer M. Use of randomization in the evaluation of development effectiveness In: Pitman GK, Feinstein ON, Ingram GK, eds. Evaluating Development Effectiveness. New Brunswick, NJ: Transaction Publishers; 2005. [Google Scholar]
- 49. Hsiao C. Analysis of Panel Data. Cambridge, UK: Cambridge University Press; 2003. [Google Scholar]
- 50. Dixon‐Woods M, Bonas S, Booth A, et al. How can systematic reviews incorporate qualitative research? A critical perspective. Qual Res. 2006;6(1):27‐44. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix: Study's Quality Assessment Instrument
Appendix Table A: Quality Assessment Results of the Reviewed Studies


