Abstract
Background: Many surgeons and emergentologists use non–ultrasound-guided wrist nerve blocks. There is little evidence to guide the ideal volume of local anesthesia or how long we should wait after injection before performing pain-free procedures. This pilot study examined time to maximal anesthesia to painful needle stick in 14 volunteer participants receiving bilateral wrist blocks of 6 versus 11 mL of local. Methods: One surgeon performed all 14 bilateral wrist median nerve blocks in participants who remained blinded until after bandages were applied to their wrist. No one could see which wrist received the larger 11-mL volume injection versus the 6-mL block. Blinded sensory assessors then measured perceived maximal numbness time and numbness to needle stick pain in the fingertips of the median nerve distribution. Results: Failure to get a complete median nerve block occurred in seven of fourteen 6-mL wrist blocks versus failure in only one of fourteen 11-mL blocks. Perceived maximal numbness occurred at roughly 40 minutes after injection, but actual numbness to painful needle stick took around 100 minutes. Conclusions: Incomplete median nerve numbness occurred with both 6- and 11-mL non–ultrasound-guided blocks at the wrist. In those with complete blocks, it took a surprisingly long time of 100 minutes for maximal anesthesia to occur to painful needle stick stimuli to the fingertips of the median nerve distribution. Non–ultrasound-guided median nerve blocks at the wrist as described in this article lack reliability and take too long to work.
Keywords: lidocaine, wide awake surgery, time to anesthesia, numbness to pain, median nerve block, local anesthetic, volume of local anesthetic
Introduction
Pure local anesthesia for hand surgery and emergency department procedures is becoming increasingly popular, particularly with the advent of the minimally painful injection technique of local anesthesia.4,6,11 Many surgeons and emergentologists use wrist nerve blocks instead of tumescent lidocaine with epinephrine injection for painful hand interventions. The latter technique has become popular for wide awake local anesthesia no-tourniquet (WALANT) hand surgery.5,7,12 There is very little evidence to guide us in knowing the ideal volume of local anesthesia to perform a non–ultrasound-guided wrist median nerve block. There is also little evidence to tell us how long we should wait after a median nerve block so that we can perform pain-free surgical interventions. The primary aim of this pilot study was to compare the effectiveness of 6 versus 11 mL of 1% lidocaine with 1:100 000 epinephrine in non–ultrasound-guided bilateral wrist blocks in 14 participants. The second goal of this study was to look at the amount of time required to obtain peak numbness to painful needle prick in fingertips after a wrist median nerve block.
Methods
Approval for the study was obtained through the Research Ethics Board of Horizon Health Network. Fourteen first-year medical students (9 male and 5 female) with a mean age of 24.75 (SD = 3.49) years volunteered to participate in the study. All participants were injected in both wrists by a single plastic surgeon, one wrist with 6 mL and the other wrist with 11 mL (Figure 1). Participants were blinded during the bilateral injections with their eyes covered, and remained blinded until after the injecting surgeon wrapped the visibly injected areas with a bandage after injection. No one else but the injecting surgeon saw the injected part of the wrists until after the sensory data were collected and the wrist bandages were removed. All injections were performed in a room separate from other investigators.
Figure 1.
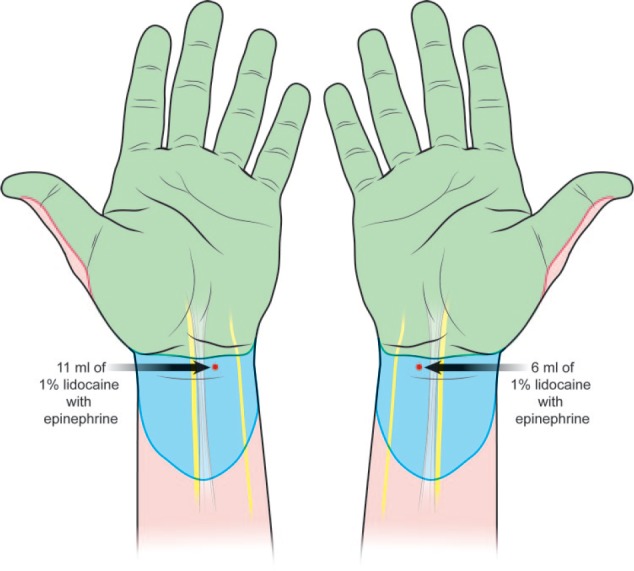
Each of 14 blinded volunteer participants received bilateral median nerve blocks.
Note. One hand received 6 mL, and the other hand was injected with 11 mL in each participant. The red dot indicates the point of injection. Blue indicates the area of visible or palpable local anesthesia. Green indicates the areas of local anesthesia obtained by complete median (and ulnar) nerve blocks.
The volumes of lidocaine and which side to be injected first for both hands were randomly assigned and enclosed in an unmarked envelope by an independent investigator who gave the envelopes to the injector. Only the injector knew which hand got the higher volume.
All injections were performed over 5 minutes. In each volunteer, one wrist got 1 mL under the skin and 10 mL under the forearm fascia for a total of 11 mL. The other wrist got 1 mL under the skin and 5 mL under the forearm fascia for a total of 6 mL. All blocks were performed with 27-gauge needles and 10-mL syringes. The injection site was consistently 5 mm proximal to the wrist crease and 3 mm medial (ulnar) to the midline of the wrist. All injections contained 1% lidocaine with 1:100 000 epinephrine buffered with 8.4% bicarbonate in a ratio of 10 mL of lidocaine to 1 mL of bicarbonate. All anesthetic solutions were maintained at room temperature.
The injector left the facility once all injections were complete to prevent unblinding the data collection. Sensory assessment investigators asked participants whether they felt the level of anesthesia had increased over the last 5 minutes at 5-minute intervals beginning 5 minutes after injection. The data collectors continued asking in 5-minute intervals until there were 3 consecutive negative responses (15 minutes) in which the participants felt that the level of anesthesia had not increased. After each reported negative responses (no increase in perceived anesthesia in the last 5 minutes), or if the participant was unable to determine whether the level of anesthesia had increased, the data collector used a sterile 30-gauge needle to assess and map the area of loss of needle pain sensation with a marking pen. When numbness to painful needle prick ceased to increase in the area of anesthesia at 5-minute intervals, sensory assessment ceased.
Nerve blocks were labeled as complete if the all the median nerve innervated fingertips achieved complete numbness to painful needle stick. Nerve blocks were determined to be incomplete if the participants retained sensibility to painful needle stick of the fingertips of the median nerve distribution when their numbness had maximized.
Exclusion criteria included daily pain medication use, any contraindication to local anesthetic injection, prior surgery of the wrist, and pregnancy or lactation.
Results
Every one of the 14 participants received both a 6-mL injection in one wrist and an 11-mL injection in the other wrist. Seven of the 14 participants experienced an incomplete median nerve block in the hand with the 6-mL injection of local anesthesia, whereas only 1 of 14 participants experienced an incomplete nerve block in the hand with the 11-mL injection. An exact McNemar test determined that there was a statistically significant difference in the proportion of incomplete nerve blocks for 6- and 11-mL injections of anesthesia (P = .03).
Of the participants who achieved complete nerve blocks after 11-mL injections, participant perception of achievement of maximal numbness occurred at a mean of 42.3 minutes (SD = 12.18), while peak numbness as determined by painful needle stick testing occurred at a mean of 103.5 minutes (SD = 18.2 minutes). In other words, numbness to painful stimulus took an average of 61.2 minutes longer to achieve than perceived numbness.
After a 6-mL injection, perception of achievement of maximal numbness occurred at a mean of 37.1 minutes (SD = 10.7 minutes), while peak numbness as determined by painful needle stick testing occurred at a mean of 95.7 minutes (SD = 14.3 minutes). In other words, numbness to painful stimulus took 58.6 minutes longer to achieve than volunteer perceived numbness.
Note that 7 participants did not achieve complete nerve blocks with 6-mL injections. As a result, the means for perception of maximal numbness and achievement of peak numbness by needle stick after a 6-mL injection are based on data from only 7 participants. Similarly, as 1 participant did not achieve a complete nerve block after an 11-mL injection, the means for perception of maximal numbness and achievement of peak numbness by needle stick after an 11-mL injection are based on data from 13 participants.
Discussion
Non–ultrasound-guided wrist blocks as performed in this study take too long to work and may not be as effective as many surgeons and emergentologists may think they are, even when larger volumes of 11 mL are injected.
After non–ultrasound-guided wrist bilateral median nerve blocks in our 14 participants, 7 of 14 hands obtained incomplete median nerve blocks with injections of 6 mL of lidocaine and epinephrine. Only one of 14 hands did not get a complete median nerve block with an 11-mL injection. Therefore, 6 mL appeared to be less effective than 11 mL in producing complete median nerve blocks in this pilot study. Our findings support the intuitive reasoning that if we inject more molecules of lidocaine around the nerve, more will get into the nerve. It is possible that the optimal volume of local anesthetic in non–ultrasound-guided nerve blocks is higher than 11 mL.
There is little high-level evidence to indicate how much local anesthesia we should inject to properly numb painful hand procedures when we provide non–ultrasound-guided wrist median nerve block anesthesia. A search of anesthesia textbook literature revealed recommended lidocaine volumes of 2 to 4 mL9 and 3 mL1 for median nerve anesthesia. Our clinical experience and the results of this article suggest that this 4 mL may not be generous enough for non–ultrasound-guided nerve blocks. Another study of 11 mL median nerve injections of 2% lidocaine and 0.6% bupivacaine without nerve stimulation found that 9% of participants required reinjection of the median nerve prior to endoscopic carpal tunnel release surgery.3 The same study also reported a 34% reinjection rate of ulnar nerve blocks; however, the authors attributed this to suboptimal ulnar nerve injection technique.3
Plastic surgery textbooks recommend lidocaine volumes as low as 5 mL13 and up to volumes of 10 mL10 for carpal tunnel release surgery. Endoscopic carpal tunnel release procedures using 4 to 6 mL of 1% lidocaine without epinephrine8 and open carpal tunnel release using 11 mL of 1% lidocaine without epinephrine2 have also been recommended.
We were surprised to find that the level of anesthesia to needle stick takes so long to peak at about 100 minutes. Most patients and doctors would not be willing to wait that long. Our clinical experience and previously published studies5,7,12 show that minimally painfully injected tumescent local anesthesia where a surgeon is going to cut in the hand will provide much faster and more reliable anesthesia than what we observed in this study. Thirty minutes of waiting after tumescent local anesthesia has reliably provided excellent pain-free surgery. This may be because the nerves in the hand and fingers are much smaller in diameter than the median nerve at the wrist. Smaller nerves may be penetrated more quickly and effectively by lidocaine. Non–ultrasound-guided nerve blocks as performed in this study are clearly inferior to the usual tumescent local anesthesia injection we routinely perform in WALANT hand surgery.
Why did some of the hands get an incomplete block when injected with the same technique when the others got a complete block? It may not only be the volume. Anatomical variation may be one reason. Another may be subfascial versus suprafascial injection. We have observed that even as much as 20 mL of 1% lidocaine with epinephrine may not produce a complete median nerve block if it is only injected subcutaneously and not under the forearm fascia. This structure appears to be able to be a relative barrier to local anesthetic diffusion in some patients. A limitation of not using ultrasound is that we cannot be certain that our needle tip is below the forearm fascia and that our local anesthesia actually bathed the median nerve. However, most hand surgeons and emergentologists still do not use ultrasound at this time to perform median nerve blocks in daily clinical practice. Maybe we should be routinely using ultrasound for large nerve blocks.
We chose the median nerve block injection site usually used by the senior author. He chooses this site between the median and ulnar nerves to ensure that neither the median nor the ulnar nerve suffer an intraneural injection injury. Although the goal of this study was to examine median nerve blocks, this median nerve block technique also happens to block the ulnar nerve in most cases. This can be helpful if there is crossover between the 2 nerves in the hand. We used 6 mL, so the initial 1 mL could be injected under the skin to numb the needle penetration site, while the remaining 5 mL could be delivered under the forearm fascia without pain in the skin. Similarly, we used 11 mL, so the initial 1 mL could be injected under the skin to numb the needle penetration site, while the remaining 10 mL could be delivered under the forearm fascia without pain in the skin.
We used hypodermic needle stick pain to determine whether we had complete or incomplete median nerve blocks. The reason is that surgeons and emergentologists who perform median nerve blocks do so in order to perform painful procedures. Numbness to pain is therefore more clinically relevant than numbness to touch. If a nerve block is incomplete, patients will feel pain and will require a further injection of local anesthetic. This is why our end point was complete or incomplete nerve block to painful stimuli instead of touch or pressure measurements.
Another main limitation of this study is that it is a pilot study with only 14 participants. Further analysis with larger numbers would be helpful.
Conclusion
This pilot study suggests that 6 mL is inferior to 11 mL of local anesthesia in obtaining complete median nerve anesthesia to fingertip painful needle stick in non–ultrasound-guided wrist median nerve blocks. It also suggests that it may take as long as approximately 100 minutes to reach maximal anesthesia to painful fingertip needle stick with a wrist median nerve block. Our clinical experience with tumescent local anesthesia injected in the area of painful dissection in the hand suggests that it is much faster and more reliable than non–ultrasound-guided median nerve blocks in the wrist as performed in this study.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Barash P, Cullen B, Stoelting R, et al. Peripheral nerve blockade. In: Clinical Anesthesia. 6th ed. Philadelphia, PA: Wolters Kluwer; 2009:979. [Google Scholar]
- 2. Cooney W. Carpal tunnel syndrome. In: Cooney W., III ed.Wrist: Diagnosis and Operative Treatment. 2nd ed. Philadelphia,PA: Wolters Kluwer; 2012:1117. [Google Scholar]
- 3. Delaunay L, Chelly JE. Blocks at the wrist provide effective anesthesia for carpal tunnel release. Can J Anaesth. 2001;48:666-660. [DOI] [PubMed] [Google Scholar]
- 4. Farhangkhoee H, Lalonde J, Lalonde DH. Teaching medical students and residents how to inject local anesthesia almost painlessly. Can J Plast Surg. 2012;20(3):169-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gibson M. Outpatient carpal tunnel decompression without tourniquet: a simple local anaesthetic technique. Ann R Coll Surg Engl. 1990;72:408-409. [PMC free article] [PubMed] [Google Scholar]
- 6. Lalonde DH. Minimally invasive anesthesia in wide awake hand surgery. Hand Clin. 2014;30:1-6. [DOI] [PubMed] [Google Scholar]
- 7. Lalonde DH, Wong A. Dosage of local anesthesia in wide awake hand surgery. J Hand Surg Am. 2013;38:2026-2028. [DOI] [PubMed] [Google Scholar]
- 8. Luchetti R, Amadio P. Endoscopic carpal tunnel release. In: Carpal Tunnel Syndrome. 1st ed New York, NY: Springer; 2011:166-169. [Google Scholar]
- 9. Pardo M, Miller R. Anesthesia management. In: Miller R, ed. Miller’s Anesthesia. 7th ed. Vol 2 Philadelphia, PA: Elsevier Churchill Livingstone; 2011:1647. [Google Scholar]
- 10. Sammer DM, Chung KC. Rheumatologic conditions of the hand and wrist. In: Chung J, Neligan P, eds. Plastic Surgery Hand and Upper Extremity. 3rd ed. Vol 6 Stanford, CA: Elsevier Saunders; 2013:401-402. [Google Scholar]
- 11. Strazar AR, Leynes PG, Lalonde DH. Minimizing the pain of local anesthesia injection. Plast Reconstr Surg. 2013;132(3):675-684. [DOI] [PubMed] [Google Scholar]
- 12. Teo I, Lam W, Muthayya P, et al. Patients’ perspective of wide-awake hand surgery—110 consecutive cases. J Hand Surg Eur Vol. 2013;38(9):992-999. [DOI] [PubMed] [Google Scholar]
- 13. Wolfe S, Hotchkiss S, Pederson R, et al. Basic principles: anesthesia for hand surgery. In: Green’s Operative Hand Surgery. 6th ed. Vol 1 Philadelphia, PA: Elsevier Churchill Livingstone; 2011:31-32. [Google Scholar]


