Abstract
Background: In making the decision to undergo carpal tunnel release (CTR), patients may consider probability of symptom resolution. Prior studies have examined potential preoperative variables that might influence the postoperative outcome. Few studies, however, contain the sample size, prospective design, and high participant completion rate to provide solid data from which to counsel patients. The purpose of this study was to prospectively evaluate factors that have been implicated or dismissed in past studies as sources of outcome variation following CTR surgery and provide patient-relatable facts that the surgeon might use in preoperative patient counseling. Methods: One thousand thirty-one consecutive patients undergoing open CTR were prospectively enrolled. Preoperative frequency of daytime numbness, nighttime awakening, and duration of symptoms were recorded in addition to physical exam, height, weight, sex, history of diabetes, history of thyroid disease, and severity of electrodiagnostic findings. After surgery, patients reported percent resolution of numbness at defined intervals. Results: Age and sex are the only independent factors that predict the degree of resolution of numbness 6 months following surgery. All other studied variables are not independent factors nor are any paired combinations of factors. Below the age of 50, the average reported resolution of daytime numbness by 6 months is 97.3% (men 91.8% and women 99.4%). After age 50, there is a linear 0.77% decline in average resolution of daytime numbness per year. Conclusions: Age and sex but no other studied factors predict resolution of daytime numbness in a multivariate model of patients undergoing CTR.
Keywords: carpal tunnel, carpal tunnel release surgery, preoperative factors, age, sex, PROOF
Introduction
Carpal tunnel syndrome (CTS) is a common peripheral entrapment neuropathy. A recent review of the literature found a wide range of incidence of CTS ranging from 104/100 000 to 496/100 000 persons per year (1.04%-4.96%).5
When patients fail to improve with conservative measures, surgery is frequently performed. The number of patients who undergo carpal tunnel release (CTR) surgery per year is 29/100 000 to 148/100 000 persons per year (0.29%-1.48%).5 Decision-making regarding surgery is an important step that takes into account many factors including symptom level and duration, surgical complication rate, recovery, and likelihood of success in alleviating preoperative symptoms. This final factor has been studied using standardized tools such as the Disabilities of the Arm, Shoulder and Hand (DASH), QuickDASH, the Boston Questionnaire, and the Michigan Hand Outcomes Questionnaire.
Prior studies have found that preoperative variables such as medical comorbidities,3,9,13,15,17,18,21 sex,14 duration of symptoms preoperatively,14 neurophysiologic testing,4,14 physical exam findings,16 and body mass index (BMI)2 do not affect postoperative outcomes. Other studies, however, have found that diabetes,7 neurophysiologic testing,6 and other factors such as mental health, alcohol use, involvement of an attorney, and preoperative function11 do affect outcomes.
With regard to age, several authors have demonstrated poorer outcomes in the elderly.8,14 Hobby et al,8 in a study of 97 patients with 11% lost at follow-up, found that the majority of patients over the age of 70 reported an improvement in symptoms and function but they were less satisfied with their treatment than younger patients. To the contrary, a large study of 756 patients found no correlation with age.16 In this latter study, however, 45.9% of patients were lost to follow-up.
Standardized outcomes assessment tools provide cross-study comparable outcomes data. While valuable to the physician researcher, it may be more difficult for the individual patient to relate to measurement scores that are a composite of multiple questions or factors when making a decision for surgery. The current study aims to provide simple to understand, patient-relatable outcomes data that answer questions potentially posed to the physician preoperatively.
Wilgis20 reported that numbness was the most common symptom in patients undergoing CTR (95% of patients). In addition, a study by Bessette et al1 found that 94% of patients preoperatively felt that relief of numbness was extremely or very important. In our own patient population, daytime numbness and awakening at night with numbness were the most frequently voiced preoperative symptoms and became the basis of our study’s outcome measures.
The goal of this study, therefore, was to enroll a cohort of sufficient size to create a model with sufficient statistical power to quantitate and identify factors that affect the answer to the question “How much will my symptoms improve if I have surgery?” Our hypothesis was that with sufficient sample size, we will have the ability to construct a statistically valid model using preoperatively identified factors that influence the outcome of carpal tunnel surgery.
Methods
Study Design
After obtaining institutional review board (IRB) approval, 1114 consecutive patients undergoing open CTR from May 2009 through October 2014 gave informed consent and were prospectively enrolled in the study, of which, 1031 met inclusion criteria. The patients were asked to complete a written intake questionnaire upon decision to undergo surgery.
The diagnosis of CTS was made on the basis of clinical history of numbness (1023 of 1031) in the median-innervated digits and physical exam. Electrodiagnostic testing was used to confirm the diagnosis in 934 patients who met inclusion. Prior to enrollment, patients were offered conservative treatment with nighttime splints and oral vitamin B6. Cortisone injections were used infrequently preoperatively (126 patients). Patients with more severe or long-standing symptoms were advised that prolonged conservative management might negatively affect their final outcome.
Exclusion criteria included previous CTR in the same extremity and emergent CTR performed in the days following a distal radius fracture. In addition, patients who were undergoing other surgical procedures on the same date on the same extremity were excluded except those undergoing trigger finger release.
Each CTR was performed under intravenous (IV) sedation plus local infiltration at the incision line or local anesthesia alone and utilized an open technique approximately 3.2 cm long by a single fellowship-trained hand surgeon. The longitudinal incision was placed just ulnar to the interthenar depression, and the transverse carpal ligament was divided under direct vision. The distal extent included identification of the midpalmar fat pad, and the proximal extent included the fibers of the forearm fascia up to several centimeters proximal to the wrist crease. Prior to closure, the edges of the ligament were examined from proximal to distal extent to ensure a complete release. The tourniquet was deflated, and hemostasis was obtained prior to closure. The incision was closed with a 4-0 prolene running subcuticular suture and a splint applied. The dressing and suture was removed at 7 to 11 days postoperatively. Patients typically attended one visit of occupational therapy followed by a home program of incision line care and exercises.
Measurements
Data recorded at intake included age, height, weight, sex, history of thyroid disease and diabetes, and duration of symptoms as well as patient-reported preoperative frequency of daytime numbness and nighttime awakening. The written questionnaire asked patients to rate their daytime numbness on a scale from no daytime numbness, <1x/week, weekly, daily, or constant daytime numbness. A similar scale was used for nocturnal symptom frequency. At the 1-week and 6-week postoperative visits, patients were asked to report what percent of their preoperative daytime numbness had resolved. They were also asked to rate how often they were awakened at night with numbness on the same scale as the initial assessment. Additionally, patients were mailed a symptom survey tool at 6 months and asked to report percent resolution of their preoperative symptoms.
Statistical Analysis
All statistical calculations were performed by a biostatistician uninvolved with the data acquisition. Our primary endpoint was patient-reported symptom resolution of numbness 6 months postoperatively. Chi-square tests were used to compare categorical variables, t tests were used to compare continuous variables such as age, and Wilcoxon test was used to compare ordinal or nonnormal data. Nerve conduction latency shift data were categorized into 0.5-ms increments (from 0 ms through 2.5-ms shift) followed by a category of greater than 2.5-ms difference in latency as well as a category including nonresponsive nerves. A P value of less than .05 was considered statistically significant for all calculations.
Multivariate modeling was performed using a least absolute shrinkage and selection operator (LASSO) based model selection in the context of generalized regression modeling. Specifically, multivariate logistic regression was used to analyze the categorical outcomes of 100% resolution, 0% resolution, while linear regression models were selected for continuous outcomes of percent resolution and awakening (scale: never = 0 to every night = 3). All potential predictors and their 2-way interactions were made available to the selection procedure. The Schwarz Bayesian information criterion was used for selecting the final model. Age was similarly considered a continuous variable in the multivariate model. The R-squared value was calculated to estimate the proportion of variability in the outcome that is explained by the predictor (in this case, age). Analysis was completed using SAS Version 9.2 (SAS, Cary, NC).
Formal power analysis was not conducted, as the aim of the study was to explore a large number of possible predictors and perform model selection among them. The model selection was based on 77 predictors (counting multiple levels of categorical predictors, and the interaction terms), providing approximately 10 observations per predictor.
Patient Population
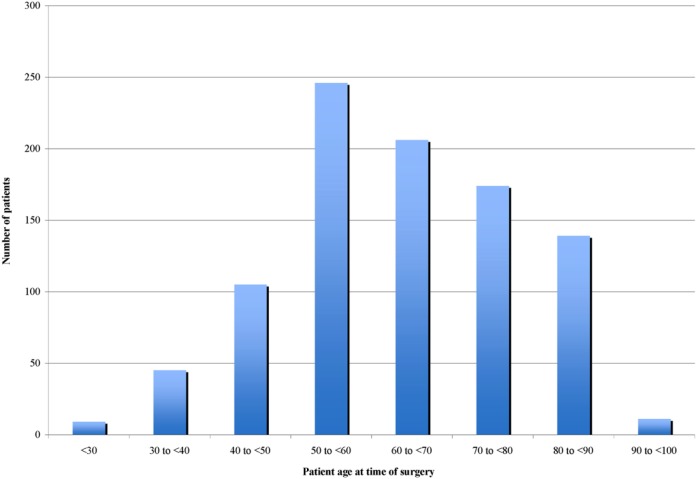
In all, 1114 consecutive patients completed the IRB-approved intake survey. Of these, 83 patients were excluded from outcome analysis based upon our exclusion criteria resulting in an initial cohort of 1031. Of this initial cohort, 936 patients (91%) completed the study through the final follow-up symptom survey at 6 months. Forty-two patients had trigger releases at the time of CTR and were included in the analysis. Six patients underwent simultaneous bilateral CTR, and each hand was included as a separate data element with individual intake assessments and outcome measurements for each hand. The average age of the cohort was 63 years (range 15-96, Figure 1), and the average duration of symptoms prior to surgery was 3.9 years (range 1 month to 20 years). There were 373 males and 658 females. Of the 1031 study participants, 133 (12.9%) had diabetes, 246 (23.9%) had BMIs of 35 or greater, 422 (40.9%) had a positive Tinel sign, and 450 (43.6%) had a positive pressure provocative test (PPT) (Table 1). Nerve conduction testing demonstrated an abnormal latency shift between the median and ulnar nerves of 0.5 ms or greater in 95% of patients and fibrillations in the abductor pollicis brevis muscle in 34% of patients. Of our patients, 9.2% did not respond to the 6-month questionnaire. In addition, we did not have weight on 10 patients nor duration of symptoms reported on 18 patients. Thirteen patients did not report their frequency of nighttime awakening.
Figure 1.
Age distribution of study population.
Table 1.
Characteristics of Cohort.
| Parameter | Number of patients (n = 1031) |
|---|---|
| Average age | 63 years (range 15-96) |
| sex | 373 male (36%), 658 female (64%) |
| Average symptom duration | 3.9 years (1 month-20 years) |
| Diabetes | 133 (12.9%) |
| Body mass index ≥ 35 | 246 (23.9%) |
| Positive Tinel sign | 422 (40.9%) |
| Positive pressure provocative sign | 450 (43.6%) |
Results
Daytime Numbness
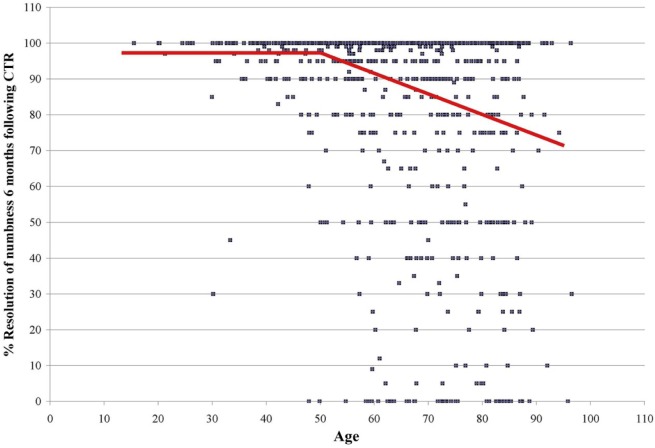
In patients up to age 50, the average reported resolution of daytime numbness at 6 months is independent of age and averages 97.3% (men 91.8% and women 99.4%, range 0%-100%, P < .05). After age 50, there is a linear decline in resolution of daytime numbness of 0.77% per year of age (95% CI, −0.86 to −0.59, P < .05) with an R2 value of 11% (Figure 2). Although bivariate analysis demonstrates several potentially significant factors (Table 2), multivariate analysis of BMI, diabetes, hypothyroidism, preoperative symptom duration, Tinel sign, PPT, and slowing on nerve conduction studies shows that these factors are not statistically predictive of numbness resolution. Multivariate analysis identifies age and sex as the independent variables.
Figure 2.
Scatter plot demonstrating percent resolution of numbness for each study participant at 6 months. Line represents statistical model of the data (P < .0001).
Note. CTR = carpal tunnel release.
Table 2.
Preoperative Factor and Bivariate Statistical Significance.
| Preoperative factor | P value |
|---|---|
| Age | <.05 |
| sex | <.05 |
| Body mass index | .49* |
| Diabetes | <.05* |
| Tinel sign | .35* |
| Pressure provocative test | <.05* |
| Nocturnal awakening with numbness | <.05* |
| Median to ulnar latency >0.5 ms | <.05* |
| Fibrillations in abductor pollicis brevis | <.05* |
Note. * = not statistically significiant upon multivariate analysis.
Patient-reported complete resolution of daytime numbness at 6 months follows a similar statistically significant (P < .05) relationship to age. In the population less than 40 years (54 patients), 71% saw complete resolution; in 40- to 79-year-olds (731 patients), there is a 60% rate of complete resolution; and in those 80 years and older (150 patients), a 43% rate of complete resolution.
Failure to achieve any improvement (0% resolution of daytime numbness) following CTR surgery was also statistically age-related (P < .05). Before age 80 (785 patients), there is a less than 3% failure rate of the operation to give any resolution of daytime numbness. In patients 80 years and older (150 patients), this increases to 14%.
Although data on speed of symptom resolution were not a primary goal of our data collection and analysis, we did perform raw data tabulation of symptom resolution at the first postoperative visit (7-11 days) and found that 56% of patients reported 90% or greater resolution at that early time point.
Nighttime Awakening
Awakening with numbness is a common symptom in CTS with 89% of patients in our population reporting this at least 1 night a week preoperatively. Persistence of this symptom postoperatively is uncommon in all age groups. In patients less than 40 years, 8% report any awakening with numbness at 6 months. In patients ages 40 to 79, 10% report any awakening, and in patients age 80 and greater, 15% report awakening.
Complications
There were no postoperative infections and no recognized nerve or vascular injuries. No patient returned to the operating room for postoperative hematoma treatment, secondary wound management, or other complication. One patient underwent repeat CTR for persistent symptoms during the study period. The results of the first surgery were included in the data analysis; however, the second surgery was excluded based upon our exclusion criteria.
Discussion
For the factors examined, age and sex are the independent variables in predicting percent resolution of daytime numbness in patients 6 months following CTR. Our study demonstrates that even these factors only accounts for a low portion of the variability in the outcome of CTR surgery. The study size and high study completion rate allowed age-stratified multivariate analysis of factors including diabetes, thyroid disease, BMI, sex, Tinel sign, PPT, electrophysiological findings, and duration of symptoms. Although bivariate analysis demonstrated several statistically significant preoperative factors such as diabetes, nocturnal awakening, fibrillations in the abductor polices brevis on nerve testing, and PPT, upon multivariate analysis, only age and sex were significant. In addition, no model combining multiple factors was statistically significant in predicting percent resolution of numbness. The data suggest that many of the studied factors vary by decade of life and are themselves more frequent in older individuals; however, these other factors lose outcome significance once age is included in the analysis. By not stratifying for age, previous studies have come to varying conclusions regarding the importance of risk factors investigated.7,16-18 Our study population is comparable with prior studies with regard to age, BMI, and diabetic incidence.2,3,10 Similar to prior studies,8,14,20 our data demonstrate that older individuals improve following CTR, however, to a lesser degree than their younger counterparts. Most prior studies have used a predefined age cutoff comparing young and old groups. Our study, by contrast, treats age as a continuum so that a statistical model could be created that would be useful to the counseling clinician for a patient of any age. Similar to drug studies which prove efficacy through a dose-response curve, our data demonstrate a linear relationship between advancing age and reduction in symptom resolution in patients 50 years and older.
Previous studies2,7,8,16,20 have used standardized and validated outcomes tools such as DASH, QuickDash, Boston Questionnaire, and the Michigan Hand Outcomes Questionnaire which provide a means to compare results between studies and add to a consistent base of scientific knowledge. The current study design instead aims to provide outcomes data that patients can relate to during the time of preoperative decision making. When answering the basic question, “Will this surgery help my symptoms?” we use the acronym PROOF (patient-relatable operative outcomes facts) to describe the evidence-based patient-understandable facts that we offer to help in their decision making. This study provides 5 such outcomes facts:
Average daytime resolution: Age matters with 97.3% (men 91.8% and women 99.4%) average resolution of daytime numbness for patients up to age 50 and 0.77% average reduction per year thereafter.
100% resolution: Complete resolution of daytime numbness follows a similar age relationship. In the population less than 40 years, 71% see complete resolution; in 40- to 79-year-olds, there is a 60% rate of complete resolution; and those 80 years and older, a 43% rate of complete resolution.
0% resolution: There is a less than 3% chance of no improvement in daytime numbness following CTR in those younger than age 80 and a 14% chance of no improvement for patients 80 years and older.
Nocturnal awakening: Awakening is a common symptom in CTS (89% in this study), and persistence of this symptom is infrequent (8% ages <40, 10% ages 40 to <80, and 15% ages 80 and greater).
Variability: There is a wide range of outcomes in every age group and even age only explains 11% of the variability of daytime symptom resolution (R2 = 11%).
Unlike most outcome tools that measure symptoms at the time of tool administration, this study’s outcome measures include questions that incorporate patient recall bias. The participants were asked what percent resolution they felt the operation provided them compared with their preoperative symptoms. Although this might be considered a methodological flaw, we chose this measurement as it represents the patient’s lasting opinion of the success of the operation and what they might tell a neighbor, coworker, or family member.
Although previous studies have not been able to demonstrate a linear association between age and outcome,8 small sample size may have prevented the demonstration of such a relationship. The current study shows equal outcomes in patients under age 50 and then a statistically validated and linear decline from age 50 through the oldest age range that included patients in their nineties. Our data demonstrate that all age groups experience on average overall improvement.
Our data demonstrate that older individuals have more severe electromyography (EMG) findings with a correlation coefficient .14 (P < .05). Other studies have similarly found that older individuals have more advanced EMG findings on presentation.5,12,16 Multivariate analysis, however, does not show this as a factor in resolution of daytime numbness.
There are several limitations to our study. This is a single-surgeon study using an open carpal tunnel technique with results that may not be generalizable to other surgical methods. Another limitation is that this is a single arm study without comparison with nonsurgical treatment options. By design, our study asked subjective outcome questions; however, this limits comparison of the study data to other studies which use standardized outcomes tools. Our study used frequency of daytime numbness and nighttime awakening as markers of symptom severity but did not ascertain other subjective information about severity such as the degree of patient numbness or loss of function through the intake questionnaire. In addition, we used EMG evidence of thenar muscle denervation as a studied factor but did not include visible thenar atrophy in the data collection. The electrodiagnostic analysis included latency difference between median and ulnar nerve at 140-mm distance but did not study absolute latencies or other conduction variables. Although we chose to study latency shift based upon prior studies,19 other conduction factors not studied or studying latency as a continuous rather than a categorical variable may have shown relevance.
Another potential limitation is that our outcome endpoint was selected to be 6 months without prestudy analysis of whether this endpoint was adequate to assess final symptom resolution. This endpoint was based upon prior studies that have chosen a similar endpoint.1,8,20 Measurements at a later point in time may have yielded different results. Our study included 6 patients (12 procedures) done bilaterally on the same date. These surgeries may represent events with outcomes dependent upon one another and should have represented an exclusion criterion. We specifically evaluated the bilateral data and found them similar to the larger dataset outcomes. Despite limitations, the current study overcomes shortcomings of prior research on this topic including lack of adequate age stratification, limited sample size, high loss to follow-up rate, and retrospective design.
It is important to decide whether a .77% decline in results per year is significant enough to become part of the preoperative discussion for the individual patient. For the patient in their 50s or early 60s, this may not be the case compared with an octogenarian; however, we feel it begins the discussion of incomplete symptom resolution.
In conclusion, there is a linear relationship of age to outcome in patients older than 50 years on a background of outcome variability that may be useful in the preoperative counseling of patients with CTS considering surgery. Other factors such as BMI, diabetes, hypothyroidism, preoperative symptom duration, Tinel sign, PPT, and slowing on nerve conduction studies are not predictive of resolution of daytime numbness at 6 months.
Acknowledgments
The authors thank Randy Dahl, OTR, CHT, for help with data acquisition and input. Statistical analysis was provided by Aniko Szabo, PhD, and Alexis Visotcky, MS, Medical College of Wisconsin, Department of Biostatistics.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all patients for being included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Bessette L, Keller RB, Liang MH, et al. Patients’ preferences and their relationship with satisfaction following carpal tunnel release. J Hand Surg Am. 1997;22:613-620. [DOI] [PubMed] [Google Scholar]
- 2. Bodavula VK, Burke FD, Dubin NH, et al. A prospective, longitudinal outcome study of patients with carpal tunnel surgery and the relationship of body mass index. Hand. 2007;2:27-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cagle PJ, Jr, Reams M, Agel J, et al. An outcomes protocol for carpal tunnel release: a comparison of outcomes in patients with and without medical comorbidities. J Hand Surg Am. 2014;39:2175-2180. [DOI] [PubMed] [Google Scholar]
- 4. Choi SJ, Ahn DS. Correlation of clinical history and electrodiagnostic abnormalities with outcome after surgery for carpal tunnel syndrome. Plast Reconstr Surg. 1998;102:2374-2380. [DOI] [PubMed] [Google Scholar]
- 5. English JH, Gwyne-Jones DP. Incidence of carpal tunnel syndrome requiring surgical decompression: a 10.5-year review of 2,309 patients. J Hand Surg Am. 2015;40:2427-2434. [DOI] [PubMed] [Google Scholar]
- 6. Fowler JR, Munsch M, Huang Y, et al. Pre-operative electrodiagnostic testing predicts time to resolution of symptoms after carpal tunnel release. J Hand Surg Eur Vol. 2016;41:137-142. [DOI] [PubMed] [Google Scholar]
- 7. Gulabi D, Cecen G, Guclu B, et al. Carpal tunnel release in patients with diabetes result in poorer outcome in long-term study. Eur J Orthop Surg Traumatol. 2014;24:1181-1184. [DOI] [PubMed] [Google Scholar]
- 8. Hobby JL, Venkatesh R, Motkur P. The effect of age and gender upon symptoms and surgical outcomes in carpal tunnel syndrome. J Hand Surg Br. 2005;30:599-604. [DOI] [PubMed] [Google Scholar]
- 9. Jenkins PJ, Duckworth AD, Watts AC, et al. The outcome of carpal tunnel decompression in patients with diabetes mellitus. J Bone Joint Surg Br. 2012;94:811-814. [DOI] [PubMed] [Google Scholar]
- 10. Karpitskaya Y, Novak CB, Mackinnon SE. Prevalence of smoking, obesity, diabetes mellitus, and thyroid disease in patients with carpal tunnel syndrome. Ann Plast Surg. 2002;48:269-273. [DOI] [PubMed] [Google Scholar]
- 11. Katz JN, Losina E, Amick BC, III, et al. Predictors of outcomes of carpal tunnel release. Arthritis Rheum. 2001;44:1184-1193. [DOI] [PubMed] [Google Scholar]
- 12. Kronlage SC, Menendez ME. The benefit of carpal tunnel release in patients with electrophysiologically moderate and severe disease. J Hand Surg Am. 2015;40:438-444. [DOI] [PubMed] [Google Scholar]
- 13. Mondelli M, Padua L, Reale F, et al. Outcome of surgical release among diabetics with carpal tunnel syndrome. Arch Phys Med Rehabil. 2004;85:7-13. [DOI] [PubMed] [Google Scholar]
- 14. Porter P, Venkateswaran B, Stephenson H, et al. The influence of age on outcome after operation for the carpal tunnel syndrome. A prospective study. J Bone Joint Surg Br. 2002;84:688-691. [DOI] [PubMed] [Google Scholar]
- 15. Roh YH, Lee BK, Noh JH, et al. Effects of metabolic syndrome on the outcome of carpal tunnel release: a matched case-control study. J Hand Surg Am. 2015;40:1303-1309. [DOI] [PubMed] [Google Scholar]
- 16. Stone O, Clement N, Duckworth AD, et al. Carpal tunnel decompression in the super-elderly: functional outcome and patient satisfaction are equal to those of their younger counterparts. Bone Joint J. 2014;96-B:1234-1238. [DOI] [PubMed] [Google Scholar]
- 17. Thomsen NO, Cederlund RI, Andersson GS, et al. Carpal tunnel release in patients with diabetes: a 5-year follow-up with matched controls. J Hand Surg Am. 2014;39:713-720. [DOI] [PubMed] [Google Scholar]
- 18. Thomsen NO, Cederlund R, Rosén I, et al. Clinical outcomes of surgical release among diabetic patients with carpal tunnel syndrome: prospective follow-up with matched controls. J Hand Surg Am. 2009;34:1177-1187. [DOI] [PubMed] [Google Scholar]
- 19. Uncini A, Lange DJ, Solomon M, et al. Ring finger testing in carpal tunnel syndrome: a comparative study of diagnostic utility. Muscle Nerve. 2004;12:735-741. [DOI] [PubMed] [Google Scholar]
- 20. Wilgis EF, Burke FD, Dubin NH, et al. A prospective assessment of carpal tunnel surgery with respect to age. J Hand Surg Br. 2006;31:401-406. [DOI] [PubMed] [Google Scholar]
- 21. Zyluk A, Puchalski P. A comparison of outcomes of carpal tunnel release in diabetic and non-diabetic patients. J Hand Surg Eur Vol. 2013;38:485-488. [DOI] [PubMed] [Google Scholar]