Abstract
Background: Approximately 10% of patients with lateral epicondylitis go on to have surgical treatment; however, multiple surgical treatment options exist. The purpose of this study was to review the literature for the clinical outcomes of open, arthroscopic, and percutaneous treatment of lateral epicondylitis. The authors hypothesized that the clinical outcome of all 3 analyzed surgical treatments would be equivalent. Methods: A systematic review was performed using PubMed, Cochrane Central Register of Controlled Trials, and Google Scholar in July 2016 to compare the functional outcome, pain, grip strength, patient satisfaction, and return to work at 1-year follow-up for open, arthroscopic, and percutaneous treatment of lateral epicondylitis. Results: Six studies (2 Level I and 4 Level II) including 179 elbows (83 treated open, 14 arthroscopic, 82 percutaneous) were analyzed. Three outcome measures (Disabilities of the Arm, Shoulder, and Hand [DASH] score, visual analog scale [VAS], and patient satisfaction) were reported for more than one category of surgical technique. Of these, the authors noted no clinically significant differences between the techniques. Conclusions: This is the first systematic review looking at high-level evidence to compare open, percutaneous, and arthroscopic techniques for treating lateral epicondylitis. There are no clinically significant differences between the 3 surgical techniques (open, arthroscopic, and percutaneous) in terms of functional outcome (DASH), pain intensity (VAS), and patient satisfaction at 1-year follow-up.
Keywords: lateral epicondylitis, tennis elbow, elbow arthroscopy, percutaneous, extensor carpi radialis brevis
Introduction
Lateral epicondylitis affects 1% to 3% of the general population but as much as 10% of patient over 40 years old in high-risk occupations.3,19,29 In the majority (80%-90%) of cases, it can be successfully treated nonoperatively with relief within 1 year.16,29 However, 4% to 11% of patients will have symptoms that persist, often leading to surgical intervention that results in “good” or “excellent” outcomes in 80% to 90% of cases.7,16,33
There is considerable controversy regarding the cause of lateral epicondylitis, but the most common theory, popularized by Nirschl and Pettrone,27 attributes it to angiofibroblastic hyperplasia that predominantly affects the extensor carpi radialis brevis (ECRB). Often within the literature, this symptomatology is combined into the term lateral elbow pain, which includes various etiologies such as posterior interosseous nerve (PIN) compression, tightening or contracture of the ECRB, contracture of the annular (or orbicular) ligament, elbow plica (ie, chronic impingement of a redundant synovial fold between the radius and the humerus) or inflamed synovial folds, radiocapitellar cartilage lesions or chondromalacia, radiohumeral bursa, and so forth.5,35 Due to controversy regarding the underlying pathology, there is no consensus regarding the surgical treatment. The most commonly used procedure was initially described by Nirschl and Pettrone27 in 1979, which involves excision of diseased tissue at the origin of the ECRB tendon. However, there are 13 other techniques with approximately 300 modifications described within the literature.7,16,33
Six prior systematic reviews have been published attempting to compare the different treatment methods for lateral epicondylitis (Table 1).4-6,21,36 However, only 3 of these reviews, all written by the same group of authors, looked at high-level evidence (Level I and II), and all 3 did not include arthroscopic treatment.4-6 Instead, they focused on open and percutaneous treatment alone.4-6 Thus this represents the first systematic review looking at high-level evidence to compare the surgical treatment of lateral epicondylitis using all 3 techniques (open, percutaneous, and arthroscopic).
Table 1.
Prior Systematic Reviews for Surgical Treatment of Lateral Epicondylitis.
| Study (year) | Journal | No. of articles included (levels of studies included) | Purpose | Surgical procedures included and compared | Surgical outcome and conclusions |
|---|---|---|---|---|---|
| Buchbinder et al4 (2002, Updated 2009) | Cochrane Database of Systematic Reviews | 3 (I) | Compare outcomes of surgery for lateral epicondylitis for the best: (1) symptom reduction, (2) improvement in function, and (3) improvement in grip strength | 1. Open 2. Percutaneous 3. PIN decompression |
“At this time, there are no published controlled trials of surgery for lateral elbow pain. Without a control group, it is not possible to draw any conclusions about the value of this modality of treatment.” |
| Lo and Safran21 (2007) | Clinical Orthopaedics and Related Research | 33 (I, II, III, IV, V) | Compare outcomes of surgery for lateral epicondylitis for the best: (1) relief of pain, (2) restoration of strength, and (3) return to work | 1. Open 2. Percutaneous 3. Arthroscopic |
“Although there are advantages and disadvantages to each procedure, no technique appears superior by any measure. Therefore, until more randomized, controlled trials are done, it is reasonable to defer to individual surgeons regarding experience and ease of procedure.” |
| Buchbinder et al5 (2008) | Clinical Evidence | 2 (I) | Compare the effects of treatment (both nonsurgical and surgical) for tennis elbow | 1. Open 2. Percutaneous |
“Percutaneous surgery may be more effective (than open surgery) at improving function at 1-year, and at reducing the median time to return to work.” |
| Karkhanis et al16 (2008) | British Medical Bulletin | 45 (I, II, III, IV) | Compare study quality/methodology within literature discussing the surgical treatment of lateral epicondylitis | 1. Open 2. Percutaneous 3. “Endoscopic” (Arthroscopic) |
Not applicable—Looked at study quality, rather than outcomes. |
| Buchbinder et al6 (2011) | Cochrane Database of Systematic Reviews | 5 (I) | Compare outcomes of surgery for lateral epicondylitis for all clinically relevant outcome measures. | 1. Open 2. Percutaneous 3. Radiofrequency microtenotomy 4. PIN decompression |
“We cannot be confident that one type of operation provides more benefit and less harm than another operative procedure. There is a suggestion that percutaneous surgery (vs open surgery) may result in better function and earlier return to work compared. Radiofrequency microtenotomy (vs open surgery) may confer earlier pain relief but longer term outcomes appear similar.” |
| Yeoh et al36 (2012) | Arthroscopy | 10 (III, IV) | Compare outcomes of various procedures utilizing arthroscopic elbow surgery (including lateral epicondylitis) | 1. Open 2. Arthroscopic |
“Arthroscopic treatment of lateral epicondylitis shows similar results when compared with open operations, but no reports compare it to non-operative treatment.” |
Note. PIN = posterior interosseous nerve.
The purpose of this systematic review was to determine whether the choice of surgical technique (open, percutaneous, or arthroscopic) would lead to significantly different clinical outcomes in terms of functional outcome score, pain, grip strength, patient satisfaction, and return to work at 1-year follow-up. The authors hypothesized that the clinical outcome of all 3 analyzed surgical treatments would be equivalent.
Materials and Methods
Search Strategy
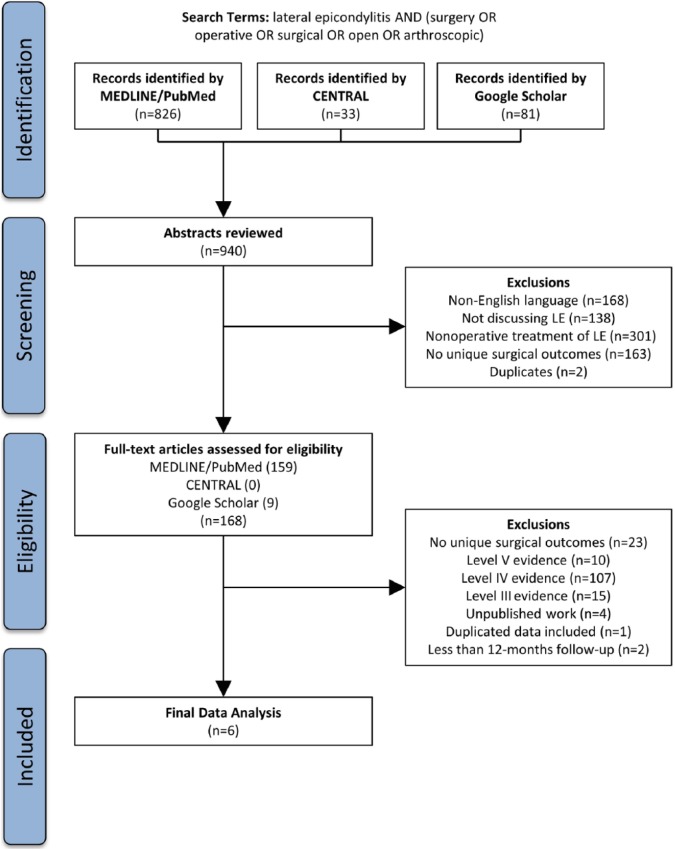
This systematic review was registered with the International Prospective Register of Systematic Reviews (PROSPERO) on June 5, 2015 (Registration number: CRD42015023254). It was conducted and reported using the protocol described by Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA).26,33 Two authors (M.B.B., R.J.M.) performed the search using the PubMed interface (MEDLINE), Cochrane Central Register of Controlled Trials, and Google Scholar between July 1, 2016, and July 20, 2016 (search terms: lateral epicondylitis AND [surgery OR operative OR surgical OR open OR arthroscopic]). All titles and abstracts from the search results were screened, while identifying relevant articles by applying the inclusion and exclusion criteria. If an article met the criteria or if insufficient information was provided from the abstract to make a decision, the full text was obtained. The full text was subsequently reviewed by applying the same criteria. To ensure that no relevant studies were omitted, the references of prior systematic reviews were assessed for additional relevant studies, which yielded no additional studies.4-6,21,36
Screening
Articles included in the final analysis were Level I or Level II evidence studies looking at the therapeutic clinical outcomes of the surgical treatment (open, percutaneous, and/or arthroscopic) of lateral epicondylitis (Figure 1) with a minimum of 12-month follow-up of 12-months. An “open” procedure was defined by a single incision greater than 3 cm in length, while an “arthroscopic” procedure involved the use of arthroscopes for intra-articular visualization. Procedures utilizing an incision 3 cm or less in length and without arthroscopes were defined as “percutaneous.” Levels of evidence were defined as specified by the Journal of Bone & Joint Surgery guidelines, which were revised in 2015.22 Level I evidence included randomized controlled trials, while Level II evidence included prospective cohort (ie, comparing 2 methods of treatment) studies and observational studies with dramatic effect.22 Level III studies were retrospective cohort studies or case-control studies. Level IV studies were case series and historically controlled studies. Level V studies were mechanism-based reasoning, expert opinions, and case reports. However, studies were graded downward or upgraded on the basis of study quality or inconsistencies.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart illustrating application of exclusion criteria to determine the final number of studies analyzed in this systematic review.
Note. LE = lateral epicondylitis.
Articles were excluded if they: (1) were not written in the English language, (2) did not discuss lateral epicondylitis, (3) did not discuss the surgical treatment of lateral epicondylitis, (4) discussed the surgical treatment of lateral epicondylitis but did not contain unique surgical outcome data (ie, cadaver studies, review articles), (5) were duplicates of other already included studies, (6) represented Level III, IV, or V evidence, (7) represented unpublished work (ie, description of a future clinical trial,23 poster presentations), (8) included the same data set as another already included study,24 and (9) had less than 12 months of follow-up.1,18
Quality Assessment and Data Extraction
Each included article was independently assessed by 2 authors (M.B.B., R.J.M.) without blinding for each article’s identifiers, such as authors, institution, and/or journal names. Each reviewer computed an individual Jadad Scale14 (Supplementary Table 1, online only), Consolidated Standards of Reporting Trials (CONSORT)2 (Supplementary Table 2, online only), and Cochrane Bone, Joint and Muscle Trauma Group Quality Assessment Tool8 (Supplementary Table 3, online only) scores for each article using each system’s respective criteria. Disagreements were resolved by consensus. In addition, data were extracted from each article including journal, publication date, title, authors, conflict of interest reporting, study design, blinding, randomization, power, alpha error, study purpose, time period of data collection, country of origin, inclusion criteria, exclusion criteria, number of patients eligible, number of patients enrolled, number of elbows that underwent surgery, sex, average age, laterality of symptoms (including whether or not it was the dominant upper extremity), duration of symptoms, duration of active nonoperative treatment, type of occupation, intervention type and description (eg, open, percutaneous, arthroscopic), outcome scores (ie, Disabilities of the Arm, Shoulder, and Hand [DASH], Mayo Elbow Performance Score [MEPS], etc), patient self-ratings (ie, pain by visual analog scale [VAS], pain relief, satisfaction, etc), objective measures (ie, grip strength, wrist strength, etc), and return to work.
Data Analysis
In a single study with cohorts of 2 or more surgical techniques (ie, cohort of patients with open surgical technique vs a cohort of patients with percutaneous surgical technique), the available elbows were split and considered to represent separate studies. All means were weighted for sample size. Descriptive statistics were calculated. Proportions were compared using either a 1- or 2-proportion Z-test. Patient satisfaction categories varied between the included studies but were always limited to 3 levels of satisfaction. To allow for comparison, categories were standardized by changing (1) “Satisfied”17 and “Pleased”28 to “Very Pleased,”11 (2) “Moderately Satisfied”17 to “Satisfied,”11,28 and (3) “Not Satisfied”11 to “Dissatisfied.”17,28 Due to significant heterogeneity in the outcome measures and data collection time points utilized by the included studies, a formal complete meta-analysis was not possible. Thus, the Best Evidence Synthesis technique was performed as described by Slavin,32 Letzel,20 and van Tulder et al.34 This involved a qualitative analysis of available studies by defining the available evidence into: (1) “strong evidence” when demonstrated consistently (greater than 75% agreement) by 2 or more high-quality studies, (2) “moderate evidence” when demonstrated consistently (greater than 75% agreement) by 1 high-quality study and/or 2 or more low-quality studies, (3) “limited evidence” when demonstrated in only 1 low-quality study, (4) “conflicting evidence” when less than 75% of studies showed consistent findings, and (5) “no evidence” when no studies could be found.
Results
Study Characteristics
Using the 3 databases, 940 abstracts were found and reviewed; 934 of these studies were excluded, which left 6 studies2,23-27 to be included in final analysis.11,17,19,25,28,30 Of these included studies, 2 (33%) were Level I11,25 and 4 (66%) were Level II.17,19,28,30 The quality scores for the available studies were calculated as (1) Jadad 46% ± 19%, (2) CONSORT 57% ± 9%, and (3) Cochrane 50% ± 9%. Five (83%) of the studies were randomized,11,17,19,25,30 but none of the studies mentioned blinding. Only 2 (33%) of the studies reported any financial conflicts of interest.11,25 Four of the studies were from Europe, specifically 2 from Scandinavia19,25 (Norway, Finland), 1 from the Netherlands,17 and 1 from the United Kingdom.11 The remaining 2 studies were from Egypt.28,30
Demographics of the Patients
One hundred seventy-nine elbows were treated within the included studies (Table 2), with 83 (46%) treated open,11,17,19,25 14 (8%) arthroscopically,28 and 82 (46%) percutaneously.11,25,28,30 Dates of subject enrollment were reported in 4 studies with subjects enrolled between 1987 and 2010.17,19,28,30 Age was reported in all 6 studies,11,17,19,25,28,30 with a weighted mean of 44 years old overall (range, 22-72), 43 years old for open (range, 25-72), 42 years old for arthroscopic (range, 28-54), and 44 years old for percutaneous (range, 22-64). Sex was reported in all 6 studies11,17,19,25,28,30 with a weighted mean of 53% men overall, 49% for open, 57% for arthroscopic, and 58% for percutaneous. This represented an equal proportion of men and women overall (P = .056; Z = −1.9), for open (P = .557; Z = .6), and arthroscopic (P = .283; Z = −1.1) groups. Although there was significantly higher proportion of men within the percutaneous group (P = .002; Z = −3.2), the proportion was not significantly different when compared with the open (P = .177; Z = −1.4) or arthroscopic (P = .943; Z = −0.1) groups. Four studies11,17,19,25 (66%) reported the duration of symptoms prior to evaluation with a weighted mean of 19.6 months (range, 5-60). The duration of nonoperative treatment prior to surgical intervention was: (1) greater than 12 months (2 studies,11,25 33%), (2) greater than 6 months (2 studies,28,30 33%), and (3) not reported (2 studies,17,19 33%). The laterality of disease involvement was only reported in 2 studies,17,19 both in the open group, with the dominant extremity being involved in a weighted mean of 75% (range, 65%-86%). Three studies11,19,25 (50%) reported whether patients’ occupation involved “manual labor” or was “physically demanding,” which was true for weighted mean of 70% overall (range, 61%-92%), 76% for open (range, 66%-92%), and 60% for percutaneous (range, 61%-77%). There was a significantly higher proportion of these “manual labor” occupations overall (P < .001; Z = −8.8), in the open group (P < .001; Z = −9.6), and in the percutaneous group (P = .001; Z = −2.6). However, the proportion was not significantly different between the open and percutaneous groups (P = .09; Z = 1.7).
Table 2.
Demographics of Surgical Candidates.
| Study (year) | Surgical technique | No. of elbows | Mean age, y | Male ratio (to female) | Job type (manual labor/physically demanding), % | Symptom duration, mo | Duration of non-operative treatment, mo | Average number of corticosteroid injections | Dominant hand affected, % | Mean follow-up, mo |
|---|---|---|---|---|---|---|---|---|---|---|
| Open | ||||||||||
| Leppilahti et al19 (2001) | N, O2 | 14, 14 | 42, 41 | 0.9, 1.0 | 92, 79 | 23a | — | — | 86, 79 | 31a |
| Keizer et al17 (2002) | O1 | 20 | 43a | 1.0a | — | 11a | — | — | 65 | 24a |
| Dunkow et al11 (2004) | O1D | 24 | 43 | 0.9 | 66 | — | ≥12a | — | — | 12a |
| Meknas et al25 (2008) | O1 | 11 | 49 | 1.2a | 73 | 28 | ≥12a | ≥3a | — | 10-18a |
| Arthroscopic | ||||||||||
| Othman28 (2011) | A | 14 | 42 | 1.3 | — | — | ≥6a | 2a | — | 12a |
| Percutaneous | ||||||||||
| Dunkow et al11 (2004) | P1 | 23 | 46 | 0.9 | 61 | — | ≥12a | — | — | 12a |
| Meknas et al25 (2008) | P2 | 13 | 47 | 1.2a | 77 | 22 | ≥12a | ≥3a | — | 10-18a |
| Radwan et al30 (2008) | P1 | 27 | 39 | 2.0 | — | 18 | ≥6a | — | — | 12a |
| Othman28 (2011) | P1 | 19 | 48 | 1.7 | — | — | ≥6a | 2a | — | 12a |
Note. “—” denotes information not reported; N = neurolysis of the posterior interosseous nerve (PIN); O2 = ECRB tendon z-lengthening in the mid-to-distal forearm; O1 = open (~4-cm incision) debridement of the damaged portions of the ECRB or release of the ECRB origin at the lateral epicondyle with additional “D” to denote drilling of the lateral epicondyle (when performed); A = arthroscopic ECRB debridement; P1 = percutaneous (~1- to 2-cm incision) division of the common extensor tendon; P2 = radiofrequency microtenotomy of the ECRB; ECRB = extensor carpi radialis brevis.
Value was reported for all patients, but not individually for each subgroup receiving an intervention.
Definition of Surgical Procedures in Included Studies
Open procedures were used in 4 studies11,17,19,25 (66%) on 83 elbows (46%). Dunkow et al11 used a 7-cm incision centered over the common extensor origin (as described by Nirschl and Pettrone27). The extensor carpi radialis longus (ECRL) was reflected to expose the origin of the ECRB, and the damaged portion of the tendon was removed. Three small drill holes were made in the lateral epicondyle. The radiocapitellar joint was explored to check for degenerative changes or synovitis. Keizer et al17 and Meknas et al25 both used a 3- to 4-cm incision starting over the tip of the lateral epicondyle and extending distally over the ECRB origin. However, Keizer et al17 went on to incise the ECRB origin transversely just ventral to the lateral epicondyle (Hohmann procedure) to a depth where the synovium of the radiohumeral joint was visible. The synovium was incised to allow inspection of the joint for intra-articular lesions. In contrast, while Meknas et al25 detached the ECRB, they avoided entering the elbow joint and proceeded to decorticate the lateral epicondyle and repair the tendon. Leppilathi et al19 included 2 open surgical groups, which were both included in the “open” category in this study. The first group received a PIN decompression, which involved an “anterolateral” incision and exposure of the radial nerve in the groove between the brachioradialis and the brachialis. The nerve was traced distally as the PIN, where it was decompressed at the arcade of Frohse by incising 1 to 2 cm of the supinator muscle. The second group received an ECRB Z-lengthening in the mid-forearm (so-called Garden Procedure13,31). A 4-cm incision was made over the dorsolateral forearm just proximal to where the thumb extensors cross the radius obliquely. The tendon of the ECRB was isolated, a Z-shaped tenotomy was performed, and the ends were reattached loosely with suture.
Percutaneous procedures were used in 4 studies11,25,28,30 (66%) on 82 (46%) elbows. Dunkow et al11 and Othman28 used a 1-cm incision over the midpoint of the lateral epicondyle to reveal the common extensor origin, while Radwan et al30 used a 1- to 2-cm incision just distal to the lateral epicondyle. The elbow is flexed to protect the radial nerve. A small pair of artery forceps is maneuvered under the common extensor origin, which is divided. The wrist is flexed to complete the defect and allow a 1-cm gap to be created at the common extensor origin, which is palpated to confirm successful release. Meknas et al25 used a 3-cm incision over the lateral epicondyle to expose the extensor tendon. Next, rather than using a scalpel, a Topaz Microdebrider electrode (ArthroCare, Austin, Texas) was inserted and used to create a microtenotomy with radiofrequency energy.
Arthroscopic procedures were used in only 1 study28 (17%) on 14 (8%) elbows.28 Othman28 used a 30° arthroscope to perform diagnostic arthroscopy to assess the elbow joint for intra-articular pathology from medial portal. Using a 3.5-mm mechanical shaver or an electrothermal device, the lateral joint capsule was resected to visual the ECRB tendon origin, which is extra-articular. Othman28 stated that commonly the ECRB attachment site is already torn, but if not the common extensor origin is released. The resection is deemed sufficient in depth when the ECRL is visualized, while limited it to the ventral half of the radial head to avoid damage to the lateral ulnar collateral ligament (LUCL). Next, the ECRB ridge is decorticated with a shaver and burr or a hand-held rasp.
Outcomes Reported in Included Studies
Overall, 11 clinically applicable outcome measures were utilized in these 6 studies.11,17,19 Of these, only 5 (of 11, 45%) were used in more than 1 surgical category (open, arthroscopic, and percutaneous), including: (1) the DASH score, (2) pain by VAS, (3) subjective patient satisfaction with surgery, (4) return to work, and (5) grip strength. Due to this heterogeneity, a formal meta-analysis was not possible, and the Best Evidence Synthesis technique (as described in the Methods) was used.
The results of these 5 clinical measures (for each study) were tabulated to allow for easier comparison (Table 3). Studies in all 3 surgical categories reported DASH scores,11,28 VAS,17,25,28,30 and patient satisfaction.11,17,28 Only the open and percutaneous categories utilized return to work11,19 and grip strength.17,19,30 The variations in reporting method (ie, reporting percentage improvement rather than actual postoperative value) and lack of reported standard deviations (only ranges or interquartile ranges were reported) limit statistical comparison of DASH scores, VAS, grip strength, and return to work.
Table 3.
Outcome Results at 12-Month Follow-up in Identified Studies.
| Outcome instrument (worst-best possible score) | Average scores |
||||
|---|---|---|---|---|---|
| Open |
Arthroscopic |
Percutaneous |
|||
| Mean/median (range, number of elbows, follow-up in months) | Mean/median (range, number of elbows, follow-up in months) | Mean/median (range, number of elbows, follow-up in months) | |||
| Preoperative scores | |||||
| DASH (100-0) Dunkow et al11—Md, IQRa Othman28—Md, Rg |
70 (64-75, 24e)11 | 72 (67-86, 14e)28 | 70 (65-80, 23e)11
70 (64-85, 19e)28 |
||
| VAS (0-10) Othman28—Mn, Rg Meknas et al25—Mn, Rg Keizer17—Mn, Rg Radwan et al30—Md, IQR |
6.5 (4-8, 11e, 10-18)25
7.4 (4-10, 20e)17 |
9.1 (8-10, 14e)28 | 9.0 (8-10, 19e)28
2.5 (1.5-4, 27e)30 7.1 (5-10, 13e, 10-18)25 |
||
| Grip strength Keizer et al17—Mn Leppilahti et al19—NR Radwan et al30—b |
26 kg (NR, 20e)17 | Radwan et al30b | |||
| Postoperative scores | |||||
| DASH (100-0) Dunkow et al11—Md, IQR Othman28—Md, Rg |
53 (48-57, 24e)11 | 48 (44-57, 14e)28 | 49 (46-51, 23e)11
50 (46-58, 19e)28 |
||
| VAS (0-10) Othman28—Mn, Rg Meknas et al25—Mn, Rg Keizer17—c Radwan et al30—Md, IQR |
1.8 (0-6, 11e, 10-18m)25
Keizer et al17d |
2.0 (NR, 14e)28 | 2.1 (NR, 19e)28
0.3 (0-1, 27e)30 2.0 (0-7, 13e, 10-18m)25 |
||
| Grip strengthd
Leppilahti et al19—Mn Keizer17—Mn Radwan et al30—Mn, Rg |
39 kg (NR, 18e)17
0.49 kp/cm2 (0-1, 28e, 31m)19 |
Radwan et al30b | |||
| Patient satisfaction | |||||
| Categoriese: | Dunkow et al11 (24e) | Keizer17 (18e) | Othman28 (14e) | Dunkow et al11
(23e) |
Othman28
(19e) |
| Very pleased | 25% | 94% | 50% | 61% | 37% |
| Satisfied | 67% | 6% | 43% | 39% | 53% |
| Dissatisfied | 8% | 0% | 7% | 0% | 11% |
| Return to workf
Leppilahti et al19—Mn, Rg Dunkow11—Md, IQR |
5 wk (4-6 wk, 24e)11
3 wk (2-5 wk, 28e, 31)19 |
2 wk (2-3 wk, 23e)11 | |||
| Change in instrument scores (pre- to postoperative) | |||||
| DASH (100-0) Dunkow et al11—Md, IQR Othman28—Md, Rg |
17 (11-19, 24e)11 | 24 (18-30, 14e)28 | 20 (18-26, 23e)11
20 (18-26, 19e)28 |
||
| VAS (0-10) Meknas et al25—Mn, Rg Radwan et al30—Md, IQR Othman28—Mn |
4.7 (NR, 11e, 10-18m)25 | 7.1 (NR, 14e)28 | 6.9 (NR, 19e)28
2.2 (NR, 27e)30 5.1 (NR, 13e, 10-18m)25 |
||
Note. Results were only reported in this table if the same outcome score was available for more than one category (open, arthroscopic, and percutaneous). If outcomes were reported longer than 12 months, they were noted in the table. Radwan et al30 reports VAS pain for multiple different daily activities (ie, resting pain, night pain, pressure pain, pain during Thomsen test, pain during chair test). For this table, we have only included the result for resting pain. NR = not reported; DASH = Disabilities of the Arm, Shoulder and Hand score; VAS = visual analogue scale.
Denotes the statistical value represented: Median (Md) versus mean (Mn), range (Rg) versus interquartile range (IQR).
Radwan et al30 (27e, 12 mo) did not report values for the grip strength. Instead, they reported the grip strength in the affected arm relative to that in the contralateral (unaffected) arm. This was reported as (1) equal to the contralateral, (2) reduced by up to 25%, (3) reduced by up to 50%, and (4) reduced by up to 75%.
Keizer et al17 (20e, 12 mo/24 mo) reported postoperative VAS as decreased by 50% (3), 50% to 80% (0), 100% (15).
The grip strength in Leppilahti et al19 was reported in kilopond per square centimeter and was only reported postoperatively.
For comparison, categories were standardized by changing (1) “Satisfied”17 and “Pleased”28 to “Very pleased,”11 (2) “Moderately Satisfied”17 to “Satisfied,”11,28 and (3) “Not Satisfied”11 to “Dissatisfied.”17,28 Also, each number was converted to percentages based on the number of elbows in each category.
Return to work for Leppilahti et al19 was turned into a weighted mean as both treatment groups included in their study fell into the “open” category in this study.
The weighted mean for patient satisfaction for each technique were: (1) “very pleased” in 55%, 50%, and 50%, (2) “satisfied” in 40%, 43%, and 45%, and (3) “dissatisfied” in 5%, 7%, and 5%, for open, arthroscopic, and percutaneous techniques, respectively. There was no significant difference in patient satisfaction between open and arthroscopic (“very pleased,” P = .746, Z = 0.324; “satisfied,” P = .844, Z = −0.197; “dissatisfied,” P = .793, Z = −0.263), open and percutaneous (“very pleased,” P = .646, Z = 0.459; “satisfied,” P = .643, Z = −0.464; “dissatisfied,” P > .999, Z = 0), and arthroscopic and percutaneous (“very pleased,” P > .999, Z = 0; “satisfied,” P = .896, Z = 0.131; “dissatisfied,” P = .793, Z = 263) technique.
Only 1 (17%) of the studies25 reported the surgical time necessary to complete the procedure. Meknas et al25 reported 18 minutes (range, 10-23) for percutaneous release versus 30 minutes (range, 22-40) for open ECRB release/repair. Only 2 (33%) of the studies reported whether any complications resulted from treatment, but both reported no complications (minor or major) from open,19 arthroscopic,28 or percutaneous28 techniques.
Discussion
The authors’ hypothesis was that there would not be a significant clinical difference between the 3 techniques in terms of functional outcome scores, pain, grip strength, patient satisfaction, and/or return to work at 1-year follow-up. Two studies11,28 including all 3 surgical categories and utilized the DASH score as a measure of functional outcome both pre- and postoperatively, which has been shown to be a valid measure of function for lateral epicondylitis with a clinically significant difference defined by a 10-point change.12,15 All studies had a significant improvement from pre- to postoperatively, but the difference between techniques was not clinically significant. All 4 studies17,25,28,30 that reported VAS postoperatively showed a clinically significant decrease in VAS postoperatively, which was equivalent between the 3 techniques. Three studies11,17,28 in all 3 surgical categories reported patient satisfaction with their treatment postoperatively. Comparison between these studies was limited by the differing scales used; however, overall the patient satisfaction appears equivalent between the surgical techniques with approximately 90% of patients either “very pleased” or “satisfied” with their procedure (compared with “dissatisfied”). Based on this review, there is moderate evidence that there is no clinically significant difference between the 3 techniques in terms of DASH, VAS, or patient satisfaction. Reporting of grip strength and return to work was only available for open and percutaneous techniques. The method of reporting the grip strength varied between studies negating comparison. Percutaneous techniques appeared to have a more rapid return to work when compared with the open techniques.
All prior systematic reviews looking at clinical outcomes after surgery for lateral epicondylitis either reported having “insufficient evidence” to compare techniques or reported equivalent outcomes between techniques; however, additional studies have since been published.4-6,21,36 Of the 6 prior literature reviews looking at the surgical treatment of lateral epicondylitis, all included open techniques, which are the most commonly used, and 5 included percutaneous techniques. However, only 3 studies16,21,36 included the arthroscopic technique, with 1 study16 solely looking at the quality of evidence (rather than clinical outcomes) and another36 looking at only 2 of the 3 techniques (ie, open vs arthroscopic). Yeoh et al36 looked at 2 Level III studies and 8 Level IV studies comparing open versus arthroscopic techniques and found “similar results” between them. Lo and Safran21 compared all 3 techniques by looking at all levels of evidence (2, 1, 1, 28, and 1 studies for Level I, II, III, IV, and V evidence, respectively). They interpreted the evidence to show a faster return to work with arthroscopic and percutaneous (vs open procedures) with an equivalent decrease in grip strength (to 90% of the unaffected side) and an equivalent “success rate” (including multiple outcome measures: pain, function, return to activities) for all 3 techniques.21
Outside of patient preference and surgeon familiarity with each technique, 3 commonly discussed factors affecting the choice of treatment are: (1) the ability to visualize the elbow joint (to rule out other pathology), (2) the complication rate, and (3) the length of the surgical procedure. Proponents of the open and arthroscopic techniques often cite a theoretical benefit of intra-articular visualization allowing the identification of other potential intra-articular pathology causing lateral elbow pain (either coexisting with or masquerading as ECRB tendinosis), thus limiting the number of refractory cases.29 The open technique can be modified with a capsulotomy to allow partial visualization of the elbow joint, while the arthroscopic technique allows visualization of the entire elbow joint and avoids division of the overlying common extensor origin, which may or may not be involved in the disease process.9,27 Elbow arthroscopy is thought to have a high learning curve with potentially devastating complications (ie, peripheral nerve injury), while both open and percutaneous techniques require minimal technical aptitude in the hands of most surgeons with a detailed knowledge of elbow anatomy.10 However, 2 prior studies have shown the complication rate for arthroscopic treatment of lateral epicondylitis to be less than that of open and percutaneous techniques.16,29 Pomerantz29 found an overall complication rate for the surgical treatment of lateral epicondylitis of 3.3% with a rate of 4.3%, 1.9%, and 1.1% for open, percutaneous, and arthroscopic surgery, respectively. Karkhanis et al16 found slightly higher complication rates overall with 10.6%, 6.3% and 0% for open, percutaneous, and arthroscopic surgery, respectively. Only 2 of the studies included in this review reported their complications, which were nonexistent in both.19,28 Only 1 study commented on the surgery time for open and percutaneous procedures, which was approximately 2 times longer for the open procedure.25 No study reported the surgical time for the arthroscopic technique. The results of this study show equivalent clinical outcomes regardless of the technique used (with or without intra-articular visualization), complication rates, or the length of the surgical procedure.
The majority of limitations are related to the studies included in this review. Study design bias is limited as only levels of evidence I-II were included, and all but one of the studies was randomized. Selection bias is present as we limited studies to those with a minimum of 1-year follow-up. Only 2 (33%) of the included studies reported their conflicts of interest contributing to selection bias. Publication bias is present due to the exclusion of medical conference abstracts, non-English language studies, and unpublished English language studies. Performance bias is present as the surgical interventions and postoperative protocols were not identical for all studies, even within the treatment groups. Detection bias may be present as none of the studies mentioned blinding of outcome assessment. Last, there was a wide heterogeneity in surgical procedures and outcome measures used in the included studies. However, comparison was only done for outcome measures found for more than 1 surgical technique. The authors can only compare outcomes at 1-year follow-up as this was most commonly used in the included studies.
Conclusions
All surgical techniques for the treatment of lateral epicondylitis demonstrate excellent results. There is moderate evidence that there are no clinically significant differences between the 3 surgical techniques (open, arthroscopic, and percutaneous) in terms of functional outcome (DASH), pain intensity (VAS), and patient satisfaction at 1-year follow-up.
Supplementary Material
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: Not applicable.
Statement of Informed Consent: Not applicable.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Albrecht S, Kleihues H, Cordis R, et al. Diagnostic and therapeutic strategies for the operative treatment of radiohumeral epicondylopathy. Arch Orthop Trauma Surg. 1997;116(3):164-172. [DOI] [PubMed] [Google Scholar]
- 2. Begg C, Cho M, Eastwood S, et al. Improving the quality of reporting of randomized controlled trials. The CONSORT statement. JAMA. 1996;276(8):637-639. [DOI] [PubMed] [Google Scholar]
- 3. Bisset L, Paungmali A, Vicenzino B, et al. A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. Br J Sports Med. 2005;39(7):411-422; discussion 411-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Buchbinder R, Green S, Bell S, et al. Surgery for lateral elbow pain. Cochrane Database Syst Rev. 2002;(1):CD003525. [DOI] [PubMed] [Google Scholar]
- 5. Buchbinder R, Green SE, Struijs P. Tennis elbow. BMJ Clin Evid. 2008;2008:1117-1119. [PMC free article] [PubMed] [Google Scholar]
- 6. Buchbinder R, Johnston RV, Barnsley L, et al. Surgery for lateral elbow pain. Cochrane Database Syst Rev. 2011;(3):CD003525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Calfee RP, Patel A, DaSilva MF, et al. Management of lateral epicondylitis: current concepts. J Am Acad Orthop Surg. 2008;16(1):19-29. [DOI] [PubMed] [Google Scholar]
- 8. Cochrane Collaboration. Resources for developing a review. http://bjmt.cochrane.org/resources-developing-review. Accessed June 5, 2015.
- 9. Cohen MS, Romeo AA. Open and arthroscopic management of lateral epicondylitis in the athlete. Hand Clin. 2009;25(3):331-338. [DOI] [PubMed] [Google Scholar]
- 10. Dodson CC, Nho SJ, Williams RJ, III, et al. Elbow arthroscopy. J Am Acad Orthop Surg. 2008;16(10):574-585. [DOI] [PubMed] [Google Scholar]
- 11. Dunkow PD, Jatti M, Muddu BN. A comparison of open and percutaneous techniques in the surgical treatment of tennis elbow. J Bone Joint Surg Br. 2004;86(5):701-704. [DOI] [PubMed] [Google Scholar]
- 12. Franchignoni F, Vercelli S, Giordano A, et al. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). J Orthop Sports Phys Ther. 2014;44(1):30-39. [DOI] [PubMed] [Google Scholar]
- 13. Garden RS. Tennis elbow. J Bone Joint Surg Br. 1961;43B(1): 100-106. [Google Scholar]
- 14. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1-12. [DOI] [PubMed] [Google Scholar]
- 15. Janssen S, De Smet L. Responsiveness of the DASH questionnaire for surgically treated tennis elbow. Acta Chir Belg. 2008;108(5):583-585. [DOI] [PubMed] [Google Scholar]
- 16. Karkhanis S, Frost A, Maffulli N. Operative management of tennis elbow: a quantitative review. Br Med Bull. 2008;88(1):171-188. [DOI] [PubMed] [Google Scholar]
- 17. Keizer SB, Rutten HP, Pilot P, et al. Botulinum toxin injection versus surgical treatment for tennis elbow: a randomized pilot study. Clin Orthop Relat Res. 2002(401):125-131. [DOI] [PubMed] [Google Scholar]
- 18. Khashaba A. Nirschl tennis elbow release with or without drilling. Br J Sports Med. 2001;35(3):200-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Leppilahti J, Raatikainen T, Pienimaki T, et al. Surgical treatment of resistant tennis elbow. A prospective, randomised study comparing decompression of the posterior interosseous nerve and lengthening of the tendon of the extensor carpi radialis brevis muscle. Arch Orthop Trauma Surg. 2001;121(6):329-332. [DOI] [PubMed] [Google Scholar]
- 20. Letzel H. “Best-evidence synthesis: an intelligent alternative to meta-analysis”: discussion. A case of “either-or” or “as well.” J Clin Epidemiol. 1995;48(1):19-21. [DOI] [PubMed] [Google Scholar]
- 21. Lo MY, Safran MR. Surgical treatment of lateral epicondylitis: a systematic review. Clin Orthop Relat Res. 2007;463:98-106. [DOI] [PubMed] [Google Scholar]
- 22. Marx RG, Wilson SM, Swiontkowski MF. Updating the assignment of levels of evidence. J Bone Joint Surg Am. 2015;97(1):1-2. [DOI] [PubMed] [Google Scholar]
- 23. Matache BA, Berdusco R, Momoli F, et al. A randomized, double-blind sham-controlled trial on the efficacy of arthroscopic tennis elbow release for the management of chronic lateral epicondylitis. BMC Musculoskelet Disord. 2016;17:239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Meknas K, Al Hassoni TN, Odden-Miland A, et al. Medium-term results after treatment of recalcitrant lateral epicondylitis: a prospective, randomized study comparing open release and radiofrequency microtenotomy. Orthop J Sports Med. 2013;1(4):2325967113505433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Meknas K, Odden-Miland A, Mercer JB, et al. Radiofrequency microtenotomy: a promising method for treatment of recalcitrant lateral epicondylitis. Am J Sports Med. 2008;36(10):1960-1965. [DOI] [PubMed] [Google Scholar]
- 26. Moher D, Liberati A, Tetzlaff J, et al. ; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336-341. [DOI] [PubMed] [Google Scholar]
- 27. Nirschl RP, Pettrone FA. Tennis elbow. The surgical treatment of lateral epicondylitis. J Bone Joint Surg Am. 1979;61(6A):832-839. [PubMed] [Google Scholar]
- 28. Othman AM. Arthroscopic versus percutaneous release of common extensor origin for treatment of chronic tennis elbow. Arch Orthop Trauma Surg. 2011;131(3):383-388. [DOI] [PubMed] [Google Scholar]
- 29. Pomerantz ML. Complications of lateral epicondylar release. Orthop Clin North Am. 2016;47(2):445-469. [DOI] [PubMed] [Google Scholar]
- 30. Radwan YA, ElSobhi G, Badawy WS, et al. Resistant tennis elbow: shock-wave therapy versus percutaneous tenotomy. Int Orthop. 2008;32(5):671-677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Savastano AA, Corvese L. Experiences with the Garden operation in resistant tennis elbow. R I Med J. 1977;60(2):78-79, 112. [PubMed] [Google Scholar]
- 32. Slavin RE. Best evidence synthesis: an intelligent alternative to meta-analysis. J Clin Epidemiol. 1995;48(1):9-18. [DOI] [PubMed] [Google Scholar]
- 33. van Hofwegen C, Baker CL, III, Baker CL., Jr. Epicondylitis in the athlete’s elbow. Clin Sports Med. 2010;29(4):577-597. [DOI] [PubMed] [Google Scholar]
- 34. van Tulder M, Furlan A, Bombardier C, et al. Updated method guidelines for systematic reviews in the Cochrane collaboration back review group. Spine (Phila Pa 1976). 2003;28(12):1290-1299. [DOI] [PubMed] [Google Scholar]
- 35. Wilhelm A. Tennis elbow: treatment of resistant cases by denervation. J Hand Surg Br. 1996;21(4):523-533. [DOI] [PubMed] [Google Scholar]
- 36. Yeoh KM, King GJ, Faber KJ, et al. Evidence-based indications for elbow arthroscopy. Arthroscopy. 2012;28(2):272-282. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.