Abstract
Background: The goal of this study was to compare the biomechanical stability of a 2.4-mm dorsal spanning bridge plate with a volar locking plate (VLP) in a distal radius fracture model, during simulated crutch weight-bearing. Methods: Five paired cadaveric forearms were tested. A 1-cm dorsal wedge osteotomy was created to simulate an unstable distal radius fracture with dorsal comminution. Fractures were fixed with a VLP or a dorsal bridge plate (DBP). Specimens were mounted to a crutch handle, and optical motion-tracking sensors were attached to the proximal and distal segments. Specimens were loaded in compression at 1 mm/s on a servohydraulic test frame until failure, defined as 2 mm of gap site displacement. Results: The VLP construct was significantly more stable to axial load in a crutch weight-bearing model compared with the DBP plate (VLP: 493 N vs DBP: 332 N). Stiffness was higher in the VLP constructs, but this was not statistically significant (VLP: 51.4 N/mm vs DBP: 32.4 N/mm). With the crutch weight-bearing model, DBP failed consistently with wrist flexion and plate bending, whereas VLP failed with axial compression at the fracture site and dorsal collapse. Conclusions: Dorsal spanning bridge plating is effective as an internal spanning fixator in treating highly comminuted intra-articular distal radius fracture and prevents axial collapse at the radiocarpal joint. However, bridge plating may not offer advantages in early weight-bearing or transfer in polytrauma patients, with less axial stability in our crutch weight-bearing model compared with volar plating. A stiffer 3.5-mm DBP or use of a DBP construct without the central holes may be considered for distal radius fractures if the goal is early crutch weight-bearing through the injured extremity.
Keywords: distal radius fracture, dorsal bridge plating, distraction plating, biomechanical study, early weight-bearing
Introduction
Distal radius fractures are common, comprising one-sixth of all fractures treated in the emergency room.15 Among postmenopausal women, there is a 15% lifetime risk of sustaining a distal radius fracture, behind only compression fractures in the spine and hip fractures.2 Severely comminuted distal radius fractures present a major treatment challenge, especially in an elderly patient with osteopenia, as many of the articular fragments are not amenable to direct fixation.
Internal distraction plating across the dorsal radiocarpal joint was first described by Burke and Singer in a case report as an effective treatment method for the treatment of comminuted distal radius fractures.1 The dorsal spanning bridge plate is applied from the radial diaphysis to the second or third metacarpal diaphysis, allowing stabilization of comminuted metadiaphyseal segments as well as distraction and ligamentotaxis across the impacted articular fragments.5 Ruch et al published the first clinical series in 2005, describing the use of a 14- or 16-hole 3.5-mm plate for the treatment of 22 severely comminuted intra-articular distal radius fractures.10 Richard et al demonstrated the effectiveness of distraction plating in comminuted, osteoporotic distal radius fractures in elderly patients.9
Hanel et al described the use of distraction bridge plating for distal radius fractures as a relative indication for the polytrauma patient who requires load-bearing through the injured wrist for mobilization assistance.6 The recommended protocol allows for advancement of patients to crutch weight-bearing with a hand handle 1 month postoperatively. For polytrauma patients with distal radius fractures, the ability to weight bear early through the injured wrist would be of substantial benefit for early mobilization and independence in bed to chair transfers, to minimize the medical complications of prolonged bed rest. In a series of elderly patients with distraction plating of distal radius fractures, Richard et al allowed patients to platform weight bear using the injured forearm postoperatively.9
The load-to-failure strength of various volar locking plates (VLPs) has been well established in the literature and has been demonstrated to support early active motion but not immediate weight-bearing. Previously, Wolf et al compared the biomechanical properties of the 2.4-mm radiocarpal-spanning plate and external fixation in a distal radius model, and found the spanning plate to be stronger than a standard distal radius external fixator.14 However, the model only tested the bending strength of the construct and not axial loading. To our knowledge, there are no biomechanical studies to support the postoperative weight-bearing recommendations for crutch weight-bearing or to quantify the load-to-failure capability of this construct. We hypothesize that internal distraction fixation of distal radius fractures with the radiocarpal-spanning 2.4-mm locking plate will demonstrate sufficient biomechanical strength to withstand forces seen across the radiocarpal joint with axial weight-bearing associated with crutch mobilization.
Methods
Specimen Preparation
Five matched pairs of cadaveric midarm specimens (from elbow to fingertips) with mean age of 67 years (3 females, 2 males), received from the Institution’s Willed Body Program, were tested in this study. Prior to testing, all specimens were screened using fluoroscopy to ensure that all were free of prior fracture, deformity, or fixation in the distal radius. Proximally, soft tissue was removed 5 cm distal to the elbow from the proximal radius and ulna, followed by potting with casting resin (Smooth-Cast 300; Smooth-On, Easton, Pennsylvania), with the long axis of the radius perpendicular to the base of the potting fixture.
One sample from each pair received a 2.4 mm × 170 mm dorsal radiocarpal-spanning locking compression plate (LCP) (Synthes, West Chester, Pennsylvania), while the contralateral specimen received a 2.4-mm, 6-hole variable angle volar plate (VA-LCP 2-CLMN VLR HD/3H; Synthes). Left versus right was randomly selected for the first pair and then alternated for subsequent pairs. For all specimens, the skin was circumferentially dissected for ease of plate application and access for the dorsal wedge osteotomy. Care was taken to preserve the dorsal and volar radiocarpal ligaments.
Surgical Techniques
Dorsal spanning bridge plate
Ten pounds of traction was applied with the use of finger traps on the index and long fingers. The dorsal spanning plate was placed along the index metacarpal distally and passed proximally under the second dorsal extensor compartment. With traction in place, the distal most screw hole over the index metacarpal shaft was filled with a 2.4-mm cortical screw and the proximal most screw hole on the radius was filled with a 2.7-mm cortical screw. The plate and screws were removed for the osteotomy. The location of the osteotomy was marked with two 0.062 Kirschner wires (K-wires), with the first one at the proximal base of Lister’s tubercle which correlated with the metadiaphyseal junction of the distal radius and a second K-wire placed 1 cm proximal to this point. Fluoroscopic imaging was used to verify that the trajectories of the K-wires intersected volarly to create a wedge osteotomy. An oscillating saw (Stryker, Kalamazoo, Michigan) was used to create the 10-mm dorsal wedge osteotomy to simulate an AO 23-A3 multifragmentary fracture. The dorsal spanning plate was reapplied with placement of the previous distal and proximal most cortical screws. Two additional 2.4-mm locking screws were placed distally into the index metacarpal shaft. Proximally, fixation was performed with an additional 2.7-mm cortical screw placed 3 holes distal to the first cortical screw, followed by a 2.7-mm locking screw adjacent to the first cortical screw.
Volar locked plate
A standard flexor carpi radialis (FCR) approach was used to expose the distal radius. The pronator quadratus was subperiosteally elevated off the volar aspect of the distal radius. A Synthes variable angle narrow distal radius plate was applied on the volar cortex, just proximal to the watershed line in the pronator fossa. Plate placement was verified with fluoroscopy. The plate was secured proximally with three 2.7-mm cortical screws and distally with four 2.4-mm locking screws. The dorsal wedge osteotomy was performed as described for the dorsal bridge plate (DBP) specimen with the plate in situ.
Biomechanical Testing
Specimens were mounted to a servohydraulic test frame (858 Mini Bionix; MTS Systems Corporation, Eden Prairie, Minnesota). The proximal potted end with the proximal radius and ulna shaft was attached to the MTS actuator, and the hand was mounted to a crutch handle (Figure 1). The standard crutch handle was attached to the base plate. The frame holding the crutch handle constrained the fingers at the metacarpals to eliminate slipping of the hand during testing. The hands were oriented on the crutch handle to maximize contact with the thenar eminence. Load was applied through the long axis of the radius to simulate crutch weight-bearing. Optical motion-tracking sensors (Optotrak Certus; Northern Digital Inc, Waterloo, Ontario, Canada) were attached to the proximal and distal segments, adjacent to the osteotomy. Points on the proximal and distal edges of the fracture gap were digitized to measure gap site displacement throughout the test. Each specimen was preloaded to 10 N. All specimens were then loaded in compression at 1 mm/s until failure. Failure was defined as 2 mm of gap displacement at the osteotomy.
Figure 1.

Biomechanical testing setup: The proximal was potted in resin and was attached to the MTS actuator and the hand was mounted to a crutch handle. Optical motion-tracking sensors were attached to the proximal and distal segments adjacent to the fracture site.
Statistical Analysis
Paired t tests were performed comparing ultimate load to failure and stiffness of the constructs (Excel 2010; Microsoft, Redmond, Washington) with P < .05 set as the threshold for statistical significance.
Results
The VLP construct was significantly more stable to axial load in a crutch weight-bearing model than a 2.4-mm dorsal spanning bridge plate. The failure load to displace the fracture by 2 mm was 493 ± 123 N for the VLP constructs compared with 332 ± 138 N for the DBP constructs (P < .01; Figure 2). The stiffness was also higher in the VLP constructs (51.4 ± 26.0 N/mm) compared with DBP (32.4 ± 17.2 N/mm), but this was not statistically significant (P = .07; Figure 3). Consistent failure mechanisms were observed in the 2 groups. In the DBPs, the wrist flexed with progressive axial loading, causing the plate to bend (Figure 4). For the volar plate specimens, failure occurred with axial compression of the fracture site and dorsal collapse (Figure 5).
Figure 2.

Load to failure to displace the fracture by 2 mm for the dorsal bridge plate versus volar locking plate.
Figure 3.
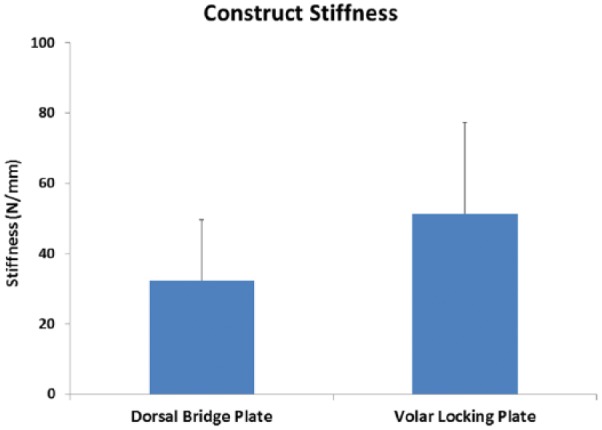
Construct stiffness for the dorsal bridge plate versus volar locking plate.
Figure 4.
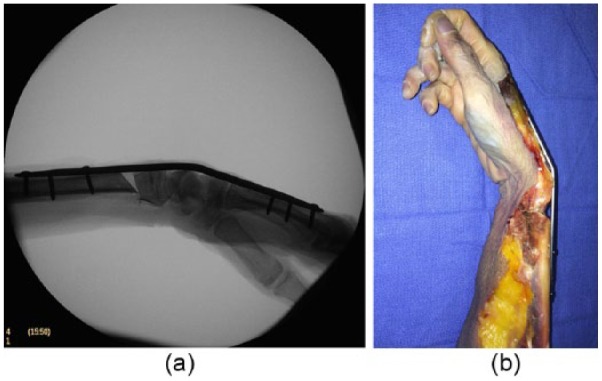
Failure of the dorsal bridge plate demonstrating consistent failure in plate bending: (a) radiographs and (b) specimen.
Figure 5.

Failure of the volar locking plate demonstrating consistent failure with axial compression and dorsal collapse at the osteotomy: (a) before loading and (b) after loading.
Discussion
The dorsal spanning bridge plate construct was less stable to axial load than the volar distal radius locking plate construct in our crutch weight-bearing model. Although not statistically significant, stiffness also trended toward being lower in the DBP constructs. Loads on the wrist required for crutch walking are estimated to be between 22% and 50% of body weight.11 For a patient of average body weight (80 kg), 50% weight-bearing translates to loads of 350 to 400 N on the wrist, exceeding the average failure load of 332 N in our DBP constructs. Based on our results, the 2.4-mm DBP may not offer advantages in early crutch weight-bearing or bed to chair transfers in polytrauma patients.
The volar plating was more stable to axial loads with a mean load to failure of 493 N. In similar distal radius models with an extra-articular osteotomy, studies by Wall et al and Liu et al reported axial loads to failure of 460 and 591 N, respectively.8,13 Dahl et al analyzed the ultimate yield strength of 8 different VLPs and reported mean strengths between 900 and 1950 N.3 Testing in the aforementioned studies was performed through direct axial loading of the distal radius articular surface, which does not simulate physiologic loading of the wrist. Our crutch weight-bearing model is unique in that it simulated physiologic weight-bearing through crutch handles, with axial loading of the radiocarpal joint.
Clinical rates of hardware failure and fracture displacement are low in patients with dorsal spanning bridge plating. Ruch et al published a clinical series of 22 patients and demonstrated congruent radiocarpal joint with articular stepoff less than 2 mm in 21 patients (95%).10 There were no cases of implant failure, re-fracture, tendon rupture, or loss of reduction. All patients had 3.5-mm plates. Using lower profile 2.4-mm mandibular plates and 2.7-mm custom stainless steel locking plates, Hanel et al demonstrated fracture healing in 100% of patients and no articular stepoff or gapping more than 2 mm.6 There was only 1 case of plate failure that occurred at 16 months postoperatively. The patient did not have the plate removed at the recommended time, as he did not want to take time off work.
More recently, Hanel et al reviewed complications associated with bridge plate fixation of distal radius fractures in 144 consecutive patients.7 A 2.4-mm mandibular plate was used in the first 59 fractures, whereas a custom 2.7-mm stainless steel plate was used in the remaining fractures. There were 5 cases of hardware failure. In 3 patients, the plate fractured at the radiocarpal articulation through an empty screw hole. In the other 2 patients, there was a fracture in the metacarpal through the most distal screw hole. The authors felt that the fracture at the level of the radiocarpal joint would have been avoided if a larger 3.5-mm plate was used or if the empty screw holes at the level of the joint were removed in the plate design. Moreover, the use of 2.7-mm screws in the metacarpal was recommended to decrease the risk of screw breakage. The current 2.4-mm dorsal spanning bridge plate is lower profile, which decreases the risk of extensor tendon irritation and also allows for placement of the plate through a minimally invasive technique by sliding it underneath the extensor tendons. However, the results of our current study corroborate with the recommendations of Hanel et al that a thicker plate should be considered in polytrauma patients in whom early crutch weight-bearing is considered. Increasing plate thickness corresponds with increasing plate stiffness. Garrigues et al demonstrated that the bending strength of the 2.7-mm locking plate was approximately one-third as stiff as the 3.5-mm nonlocking plate (P < .02).4 Uhl et al reported average yield strengths of 1167 N for 3.5-mm LCP plates and 1291 N for 3.5-mm limited-contact dynamic compression plates (LCDCPs) in axial loading.12 There are currently several commercially available spanning plates for the distal radius, both in thicker options than the plate tested in this study and options with the middle screw holes removed.
There were some limitations to our study. Although we preserved the dorsal and volar radiocarpal ligaments, soft tissue stripping of the dorsal muscles and periosteum had to be performed for the osteotomy. In a patient with a closed injury, the surrounding soft tissue contributes to fracture stability. The age and demographics of the specimens used (mean, 67 ± 14 years; 40% male) may not match the demographics of the polytrauma population, with typically young males with better bone density. However, the mechanism of failure in this study was not bone failure or screw pullout as is often seen with osteoporotic bone but was consistently bending of the 2.4-mm dorsal spanning plate at the radiocarpal joint. The characteristics of the specimens do, however, provide a worst case scenario in terms of osteoporotic bone quality in an elderly patient. As this study simulated an extra-articular distal radius fracture with dorsal comminution, the results cannot be directly applied to intra-articular fractures or other distal radius fracture types. Moreover, the simulated model in our study represents the immediate postoperative construct, with no interval bone healing. Hanel et al recommended initiation of axial weight-bearing through hand grip crutches at 1 month postoperatively.6 At 1 month, there is generally evidence of trabecular healing and increased strength of the constructs, which may explain why hardware failure rates are low clinically. Moreover, patients will generally self-protect against weight-bearing of the injured extremity in the early postoperative period. We initially had intended on cyclic testing of our constructs at 50% weight-bearing which would be approximately 400 N for an average 80-kg male. However, as our dorsal spanning plate had ultimate failure loads lower than this, we were not able to perform cycling loading but instead tested the constructs to ultimate load to failure with our crutch weight-bearing model.
Results of this study suggest that the standard 2.4-mm dorsal spanning bridge plate may not support early axial weight-bearing in polytrauma patients with comminuted distal radius fractures. A 3.5-mm dorsal spanning plate or a thicker spanning bridge plate design may be considered if the goal is early crutch weight-bearing through the injured extremity in a polytrauma patient. Alternatively, a plate design without the middle screw holes should be considered. Our simulated crutch weight-bearing model can be used for further biomechanical studies evaluating the axial load of failure of stronger plate constructs in a similar dorsal distal radius osteotomy model as well as studies evaluating similar loading in an intra-articular distal radius fracture model.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was obtained when necessary.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a DePuy Synthes research grant #A82171.
References
- 1. Burke EF, Singer RM. Treatment of comminuted distal radius with the use of an internal distraction plate. Tech Hand Up Extrem Surg. 1998;2:248-252. [DOI] [PubMed] [Google Scholar]
- 2. Cummings SR, Kelsey JL, Nevitt MC, et al. Epidemiology of osteoporosis and osteoporotic fractures. Epidemiol Rev. 1985;7:178-208. [DOI] [PubMed] [Google Scholar]
- 3. Dahl WJ, Nassab PF, Burgess KM, et al. Biomechanical properties of fixed-angle volar distal radius plates under dynamic loading. J Hand Surg Am. 2012;37(7):1381-1387. [DOI] [PubMed] [Google Scholar]
- 4. Garrigues GE, Glisson RR, Garrigues NW, et al. Can locking screws allow smaller, low-profile plates to achieve comparable stability to larger, standard plates? J Orthop Trauma. 2011;25(6):347-354. [DOI] [PubMed] [Google Scholar]
- 5. Ginn TA, Ruch DS, Yang CC, et al. Use of a distraction plate for distal radial fractures with metaphyseal and diaphyseal comminution. J Bone Joint Surg. 2006;88A(suppl 1, Pt 1):29-36. [DOI] [PubMed] [Google Scholar]
- 6. Hanel DP, Lu TS, Weil WM. Bridge plating of distal radius fractures: the Harborview method. Clin Orthop Relat Res. 2006;445:91-99. [DOI] [PubMed] [Google Scholar]
- 7. Hanel DP, Ruhlman SD, Katolik LI, et al. Complications associated with distraction plate fixation of wrist fractures. Hand Clin. 2010;26(2):237-243. [DOI] [PubMed] [Google Scholar]
- 8. Liu X, Wu WD, Fang YF, et al. Biomechanical comparison of osteoporotic distal radius fractures fixed by distal locking screws with different length. PLoS ONE. 2014;9(7):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Richard MJ, Katolik LI, Hanel DP, et al. Distraction plating for the treatment of highly comminuted distal radius fractures in elderly patients. J Hand Surg Am. 2012;37(5):948-956. [DOI] [PubMed] [Google Scholar]
- 10. Ruch DS, Ginn TA, Yang CC, et al. Use of a distraction plate for distal radial fractures with metaphyseal and diaphyseal comminution. J Bone Joint Surg Am. 2005;87(5):945-954. [DOI] [PubMed] [Google Scholar]
- 11. Slavens B, Harris G. Biomechanics. In: Abu-Faraj ZO. ed. Handbook of Research on Biomedical Engineering Education and Advanced Bioengineering Learning: Interdisciplinary Concepts, Vol. 2 Hershey, PA: IGI Global; 2012:318-337. [Google Scholar]
- 12. Uhl JM, Seguin B, Kapatkin AS, et al. Mechanical comparison of 3.5 mm broad dynamic compression plate, broad limited-contact dynamic compression plate, and narrow locking compression plate systems using interfragmentary gap models. Vet Surg. 2008;37(7):663-673. [DOI] [PubMed] [Google Scholar]
- 13. Wall LB, Brodt MD, Silva MJ, et al. The effects of screw length on stability of simulated osteoporotic distal radius fractures fixed with volar locking plates. J Hand Surg Am. 2012;37(3):446-453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wolf JC, Weil WM, Hanel DP, et al. A biomechanic comparison of an internal radiocarpal-spanning 2.4-mm locking plate and external fixation in a model of distal radius fractures. J Hand Surg Am. 2006;31(10):1578-1586. [DOI] [PubMed] [Google Scholar]
- 15. Zabinski SJ, Weiland AJ. Fracture of the distal radius. In: Levine AM, ed. Orthopaedic Knowledge Update: Trauma. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1996:67-82. [Google Scholar]


