Abstract
Background: In 1957, Dr Geoffrey Osborne described a structure between the medial epicondyle and the olecranon that placed excessive pressure on the ulnar nerve. Three terms associated with such structures have emerged: Osborne’s band, Osborne’s ligament, and Osborne’s fascia. As anatomical language moves away from eponymous terminology for descriptive, consistent nomenclature, we find discrepancies in the use of anatomic terms. This review clarifies the definitions of the above 3 terms. Methods: We conducted an extensive electronic search via PubMed and Google Scholar to identify key anatomical and surgical texts that describe ulnar nerve compression at the elbow. We searched the following terms separately and in combination: “Osborne’s band,” “Osborne’s ligament,” and “Osborne’s fascia.” A total of 36 papers were included from 1957 to 2016. Results: Osborne’s band, Osborne’s ligament, and Osborne’s fascia were found to inconsistently describe the etiology of ulnar neuritis, referring either to the connective tissue between the 2 heads of the flexor carpi ulnaris muscle as described by Dr Osborne or to the anatomically distinct fibrous tissue between the olecranon process of the ulna and the medial epicondyle of the humerus. Conclusions: The use of eponymous terms to describe ulnar pathology of the elbow remains common, and although these terms allude to the rich history of surgical anatomy, these nonspecific descriptions lead to inconsistencies. As Osborne’s band, Osborne’s ligament, and Osborne’s fascia are not used consistently across the literature, this research demonstrates the need for improved terminology to provide reliable interpretation of these terms among surgeons.
Keywords: ulnar neuritis, anatomical history, Osborne’s band, Osborne’s ligament, Osborne’s fascia, eponymous terminology, medial epicondyle and olecranon, ulnar nerve compression
Introduction
Compression of the ulnar nerve can lead to pain, numbness, weakness, and disability. Surgical and nonsurgical interventions to decompress the neural elements have been developed to alleviate these symptoms.34 In 1957, Dr Geoffrey V. Osborne described a particular etiology for ulnar neuritis in which fibrous tissue spanning the 2 heads of the flexor carpi ulnaris (FCU) muscle placed excessive pressure on the nerve and decompression of this tissue alleviated the symptoms.29 In 1959, Osborne further characterized this fibrous tissue.30 Since these original papers, 3 eponymous names have emerged: Osborne’s band, Osborne’s ligament, and Osborne’s fascia. As anatomical language is changing from eponymous terminology toward descriptive, consistent scientific nomenclature,10,18 we seek to clarify the definitions of these 3 terms in the present article. We review how each of the terms has been used in the anatomical and surgical literature, and investigate whether the 3 terms are used consistently to describe structures associated with ulnar nerve compression at the elbow.
Materials and Methods
To survey the relevant literature, we conducted an exhaustive online search via Google Scholar and PubMed databases to identify key anatomical and surgical texts that describe these 3 eponymous terms. We searched the following terms separately and in combination: “Osborne’s band,” “Osborne’s ligament,” and “Osborne’s fascia.” Papers were excluded from Google Scholar if they were published prior to 2010 with fewer than 15 citations. Papers were included in this review if the authors provided an anatomical definition of at least one of the eponymous terms we investigated. A total of 36 papers were identified from 1957 to 2016 (Figure 1).
Figure 1.
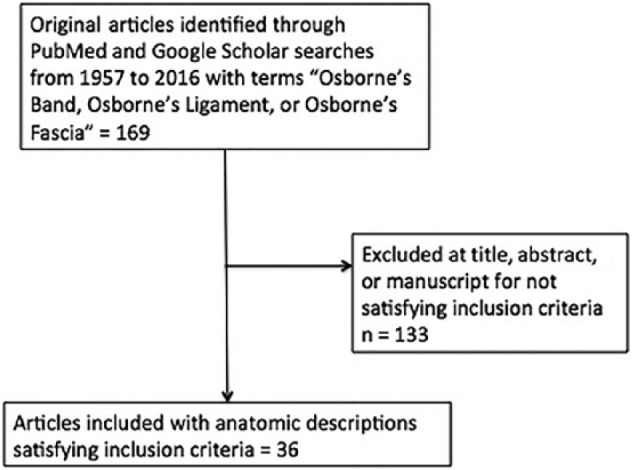
Flow diagram demonstrating selection of articles included in our analysis.
Results
Osborne’s Original Description
Dr Osborne wrote 2 key papers in 1957 and 1959 that describe the fibrous tissue compressing the ulnar nerve at the elbow. He discusses a “band of fibrous tissue bridging the two heads of the flexor carpi ulnaris [that] lay directly over the nerve.”
He continues to add that the band of compression had an “attachment to the medial epicondyle and . . . to the olecranon.”29 While this description would appear to refer to only the connective tissue between the 2 heads of the FCU muscle, the additional description referring to the medial epicondyle and the olecranon became a source of confusion. The connective tissue between the 2 heads of the FCU muscle extends to the medial epicondyle and the olecranon; however, there is additional connective tissue between the medial epicondyle and the olecranon that can also result in ulnar nerve compression (Figure 2). This structure is more proximal to 2 heads of the FCU muscle (Figure 3). These anatomically distinct sites of compression are inconsistently given eponymous terminology across the literature.
Figure 2.
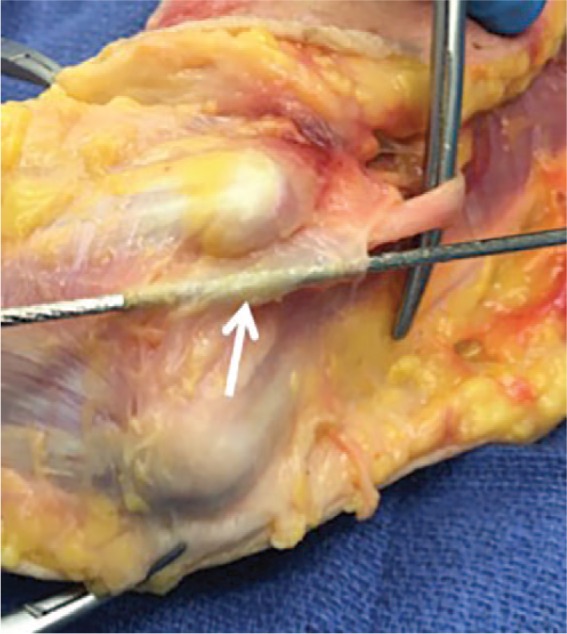
Cadaveric right upper extremity.
Note. Note that the ulnar nerve passes between the medial epicondyle of the humerus and the olecranon. The arrow demonstrates potential site of ulnar nerve compression by the connective tissue between the olecranon and the medial epicondyle. This site of potential compression is proximal to the connective tissue between the 2 heads of the flexor carpi ulnaris muscle.
Figure 3.
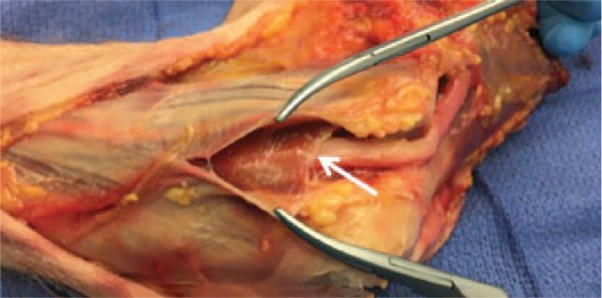
Deeper dissection of the same cadaveric right upper extremity.
Note. The arrow demarcates another potential site for ulnar nerve compression between the 2 heads of the flexor carpi ulnaris muscle. Note that this location is distal to the connective tissue spanning the medial epicondyle and the olecranon.
In 1959, Osborne wrote further on this site of compression describing “a band of fibrous tissue bridging the two heads of flexor carpi ulnaris . . . superficial to the nerve, . . . a definite condensation of transversely arranged fibres in the base of the aponeurosis, filling the triangular gap between the two heads of the muscle.”30 In 1970, he wrote a third paper again emphasizing “a transverse band between the heads of the flexor carpi ulnaris” as the source of ulnar nerve compression at the elbow.28 He did not name the structure after himself in any of these papers, and although he focused his descriptions on compression between the 2 heads of the FCU muscle, he also identified a possible second location of compression by the connective tissue between the medial epicondyle and the olecranon.
The results demonstrating the inconsistencies across “Osborne’s band,” “Osborne’s ligament,” and “Osborne’s fascia” with regard to either the connective tissue between the medial epicondyle and the olecranon or the connective tissue between the 2 heads of the FCU muscle can be summarized in Table 1. The history and the development of these terms are described below.
Table 1.
Summary of Findings.
| Connective tissue between the 2 heads of the FCU muscle | Connective tissue between the medial epicondyle and the olecranon | |
|---|---|---|
| “Osborne’s band” or a “band” of tissue causing compression | Apfelberg and Larson2
Brown et al4 Clark6 Dellon9 Feindel and Stratford11 Levy and Apfelberg21 Macnicol22 Mahan et al23 O’Driscoll et al26 O’Hara and Stone27 Vanderpool et al37 |
Blonna et al3
Fulkerson12 Gervasio and Zaccone13 |
| Osborne’s ligament | Alcid et al1
Gervasio and Zaccone13 Gonzalez et al15 Karatas et al19 Mazurek and Shin25 Palmer and Hughes32 |
Damert et al7
Henry16 Hoffmann and Siemionow17 Kleinman20 Polatsch et al33 Wilson et al38 Yamada et al39 |
| Osborne’s fascia | Catalano and Barron5
Damert et al7 Henry16 Osterman and Spiess31 Polatsch et al33 Poujade et al35 |
Goldfarb et al14
Martinoli et al24 Shahabpour et al36 |
Note. FCU = flexor carpi ulnaris.
Osborne’s Band
Fourteen papers describing “Osborne’s band” or a “band” of tissue causing ulnar nerve compression at the elbow while citing Osborne’s original article were recovered from the literature. Feindel and Stratford’s paper first cites Osborne’s work describing a “band of fibrous tissue” bridging the 2 heads of the FCU but reports confusion as to which structure Osborne was referencing.11 Several authors2,4,6,9,21-23,27,37 would continue to cite Osborne’s description of compression by the heads of the FCU muscle. Macnicol22 in 1979 provided the first eponymous term—“Osborne’s lesion.” Dellon9 in 1986 provided the first use of the term “Osborne’s band” by defining the structure as the aforementioned band bridging the heads of the FCU.
On the other hand, Fulkerson et al12 coined the terms “Osborne’s canal” and “Osborne’s tunnel” for the space in which the ulnar nerve courses between the connective tissue between the medial epicondyle and the olecranon. In 1991, O’Driscoll et al26 suggested a new terminology for ulnar neuritis, proposing the term “cubital tunnel retinaculum” (CTR) to denote the structure bridging the medial epicondyle and the olecranon and emphasized that this structure is anatomically distinct from the aponeurosis between the 2 heads of the FCU. Gervasio and Zaccone13 and Blonna et al3 described Osborne’s band as the CTR, and Gervasio and Zaccone specified that this structure was distinct from the connective tissue between the 2 heads of the FCU muscle. It is evident that 2 distinct genealogies of eponymous terms formed, the first describing the band between the FCU muscle and the second describing the connective tissue between the medial epicondyle and the olecranon.
Osborne’s Ligament
Thirteen papers were identified describing “Osborne’s ligament.” The study by Kleinman20 was the earliest reference found to have used this terminology, defining “Osborne’s ligament” as the roof of the bony retrocondylar groove at the elbow between the medial epicondyle and the olecranon rather than the 2 heads of the FCU muscle. However, several authors1,8,13,15,19,25,32 each used “Osborne’s ligament” to denote the thickened band between the humeral and ulnar heads of the FCU. Gervasio and Zaccone equated Osborne’s ligament to Osborne’s band, while emphasizing that the CTR was anatomically distinct.13 In contradiction, Karatas et al described Osborne’s ligament as the CTR defined as the connective tissue between the 2 heads of the FCU muscle.19 Other authors7,16,17,33,38,39 described Osborne’s ligament as a connective tissue between the medial epicondyle and the olecranon. In particular, 3 authors7,16,33 emphasized that Osborne’s ligament was distinct from Osborne’s fascia, in which Osborne’s fascia was the structure between the 2 heads of the FCU muscle. These papers further demonstrate that 2 distinct anatomical structures, the connective tissue between the 2 heads of the FCU muscle and the tissue between the olecranon and the medial epicondyle, are both referred to inconsistently across the literature as Osborne’s ligament.
Osborne’s Fascia
Nine papers were identified describing “Osborne’s fascia.” Three authors14,24,36 each defined Osborne’s fascia as synonymous with the term CTR defined by O’Driscoll et al26—the connective tissue between the medial epicondyle and the olecranon. On the contrary, 2 authors5,31 described Osborne’s fascia as the connective tissue between the 2 heads of the FCU. As mentioned above, 3 authors7,16,33 each described Osborne’s fascia as distinct from Osborne’s ligament; however, Osborne’s fascia was consistently described as the distal ligament extending between the 2 heads of the FCU. Poujade et al35 distinguished Osborne’s fascia as not only the fascial structure connecting the humeral and ulnar heads of the FCU but also a distinct extension of the CTR. Within these 9 citations, “Osborne’s fascia” is used to denote 2 distinct structures: either the connective tissue formed by the olecranon and the medial epicondyle, or the anatomically distinct fibrous tissue between the 2 heads of the FCU.
Discussion
This review of the anatomic literature demonstrates that the terms “Osborne’s band,” “Osborne’s ligament,” and “Osborne’s fascia” are not used consistently. It is clear that the original pathology described by Osborne in his 1957, 1959, and 1970 papers referred to the transverse band of tissue between the 2 heads of the FCU, but his original 1957 paper also indicates the possibility of another structure, the connective tissue between the olecranon and the medial epicondyle. Both these connective tissue bands, the structure between the 2 heads of the FCU and the anatomically distinct structure between the olecranon and the medial epicondyle, have been referred to as Osborne’s band, Osborne’s ligament, and Osborne’s fascia.
Despite the rich history eponymous terms provide, this review demonstrates the potential for confusion when eponymous terminology is used in preference to clear, anatomically defined terms.10,18 Moreover, the surgical consequences of imprecise communication about the anatomical basis of pathology may result in failure to treat symptomatology appropriately.
To clarify these structures for future use, we suggest moving beyond the use of eponymous terms to describe ulnar nerve compression at the elbow. Instead, clear descriptions of either the connective tissue between the 2 heads of the FCU muscle or the connective tissue between the medial epicondyle and the olecranon should be used. If eponymous terminology must be used, we recommend that Osborne’s band, Osborne’s ligament, or Osborne’s fascia only be used to denote the tissue between the 2 heads of the FCU given that his 3 original papers predominantly describe compression at this location. Moreover, the authors recommend that Osborne’s band be the preferred term given the direct language used in the1957 paper.29 This clarification will help maintain the functional and anatomical distinction of the connective tissue between the 2 heads of the FCU muscle and the connective tissue between the medial epicondyle and the olecranon.
Conclusions
The terms Osborne’s band, Osborne’s ligament, and Osborne’s fascia were not consistently used across the literature and referred to 2 distinct structures: the connective tissue between the 2 heads of the FCU muscle and the connective tissue between the medial epicondyle and the olecranon. This analysis demonstrates the need for more reliable terminology to describe ulnar compression at the elbow.
Acknowledgments
The authors thank individuals who donate their bodies and tissues for the advancement of education and research.
Footnotes
Authors’ Note: This research was presented in the form of an abstract at the American Society for Peripheral Nerve 2017 annual meeting.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was obtained when necessary
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institutes of Health (NIH), grant number #TL1TR001443. A.R.W. is supported by NIH TL1 predoctoral grant #TL1TR001443.
References
- 1. Alcid JG, Ahmad CS, Lee TQ. Elbow anatomy and structural biomechanics. Clin Sports Med. 2004;23(4):503-517, vii. [DOI] [PubMed] [Google Scholar]
- 2. Apfelberg DB, Larson SJ. Dynamic anatomy of the ulnar nerve at the elbow. Plast Reconstr Surg. 1973;51(1):79-81. [PubMed] [Google Scholar]
- 3. Blonna D, Huffmann GR, O’Driscoll SW. Delayed-onset ulnar neuritis after release of elbow contractures: clinical presentation, pathological findings, and treatment. Am J Sports Med. 2014;42(9):2113-2121. [DOI] [PubMed] [Google Scholar]
- 4. Brown JM, Mokhtee D, Evangelista MS, et al. Scratch collapse test localizes Osborne’s band as the point of maximal nerve compression in cubital tunnel syndrome. Hand (N Y). 2010;5(2):141-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Catalano LW, III, Barron OA. Anterior subcutaneous transposition of the ulnar nerve. Hand Clin. 2007;23(3):339-344, vi. [DOI] [PubMed] [Google Scholar]
- 6. Clark CB. Cubital tunnel syndrome. JAMA. 1979;241(8):801-802. [PubMed] [Google Scholar]
- 7. Damert HG, Altmann S, Infanger M, et al. Operative decisions for endoscopic treatment of cubital tunnel syndrome. Orthopedics. 2013;36(5):354-359. [DOI] [PubMed] [Google Scholar]
- 8. Degeorges R, Masquelet AC. The cubital tunnel: anatomical study of its distal part. Surg Radiol Anat. 2002;24(3-4):169-176. [DOI] [PubMed] [Google Scholar]
- 9. Dellon AL. Musculotendinous variations about the medial humeral epicondyle. J Hand Surg Br. 1986;11(2):175-181. [DOI] [PubMed] [Google Scholar]
- 10. Duque-Parra JE, Llano-Idarraga JO, Duque-Parra CA. Reflections on eponyms in neuroscience terminology. Anat Rec B New Anat. 2006;289(6):219-224. [DOI] [PubMed] [Google Scholar]
- 11. Feindel W, Stratford J. Cubital tunnel compression in tardy ulnar palsy. Can Med Assoc J. 1958;78(5):351-353. [PMC free article] [PubMed] [Google Scholar]
- 12. Fulkerson JP. Transient ulnar neuropathy from Nordic skiing. Clin Orthop Relat Res. 1980;153:230-231. [PubMed] [Google Scholar]
- 13. Gervasio O, Zaccone C. Surgical approach to ulnar nerve compression at the elbow caused by the epitrochleoanconeus muscle and a prominent medial head of the triceps. Neurosurgery. 2008;62(3)(suppl 1):186-192; discussion 192-3. [DOI] [PubMed] [Google Scholar]
- 14. Goldfarb CA, Sutter MM, Martens EJ, et al. Incidence of re-operation and subjective outcome following in situ decompression of the ulnar nerve at the cubital tunnel. J Hand Surg Eur Vol. 2009;34(3):379-383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gonzalez MH, Lotfi P, Bendre A, et al. The ulnar nerve at the elbow and its local branching: an anatomic study. J Hand Surg Br. 2001;26(2):142-144. [DOI] [PubMed] [Google Scholar]
- 16. Henry M. Modified intramuscular transposition of the ulnar nerve. J Hand Surg Am. 2006;31(9):1535-1542. [DOI] [PubMed] [Google Scholar]
- 17. Hoffmann R, Siemionow M. The endoscopic management of cubital tunnel syndrome. J Hand Surg Br. 2006;31(1):23-29. [DOI] [PubMed] [Google Scholar]
- 18. Jana N, Barik S, Arora N. Current use of medical eponyms—a need for global uniformity in scientific publications. BMC Med Res Methodol. 2009;9:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Karatas A, Apaydin N, Uz A, et al. Regional anatomic structures of the elbow that may potentially compress the ulnar nerve. J Shoulder Elbow Surg. 2009;18(4):627-631. [DOI] [PubMed] [Google Scholar]
- 20. Kleinman WB. Cubital tunnel syndrome: anterior transposition as a logical approach to complete nerve decompression. J Hand Surg Am. 1999;24(5):886-897. [DOI] [PubMed] [Google Scholar]
- 21. Levy DM, Apfelberg DB. Results of anterior transposition for ulnar neuropathy at the elbow. Am J Surg. 1972;123(3):304-308. [DOI] [PubMed] [Google Scholar]
- 22. Macnicol MF. The results of operation for ulnar neuritis. J Bone Joint Surg Br. 1979;61-B(2):159-164. [DOI] [PubMed] [Google Scholar]
- 23. Mahan MA, Gasco J, Mokhtee DB, et al. Anatomical considerations of fascial release in ulnar nerve transposition: a concept revisited. J Neurosurg. 2015;123(5):1216-1222. [DOI] [PubMed] [Google Scholar]
- 24. Martinoli C, Bianchi S, Gandolfo N, et al. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics. 2000;20:Spec No:S199-213; discussion S-7. [DOI] [PubMed] [Google Scholar]
- 25. Mazurek MT, Shin AY. Upper extremity peripheral nerve anatomy: current concepts and applications. Clin Orthop Relat Res. 2001;383:7-20. [DOI] [PubMed] [Google Scholar]
- 26. O’Driscoll SW, Horii E, Carmichael SW, et al. The cubital tunnel and ulnar neuropathy. J Bone Joint Surg Br. 1991;73(4):613-617. [DOI] [PubMed] [Google Scholar]
- 27. O’Hara JJ, Stone JH. Ulnar nerve compression at the elbow caused by a prominent medial head of the triceps and an anconeus epitrochlearis muscle. J Hand Surg Br. 1996;21(1):133-135. [DOI] [PubMed] [Google Scholar]
- 28. Osborne GV. Compression neuritis of the ulnar nerve at the elbow. Hand. 1970;2(1):10-13. [DOI] [PubMed] [Google Scholar]
- 29. Osborne GV. The results of transposition of the ulnar nerve for traumatic ulnar neuritis. J Bone Joint Surg. 1957;39B(4):778-802. [DOI] [PubMed] [Google Scholar]
- 30. Osborne GV, Orith MCH. Ulnar neuritis. Postgrad Med J. 1959;35(405):392-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Osterman AL, Spiess AM. Medial epicondylectomy. Hand Clin. 2007;23(3):329-337, vi. [DOI] [PubMed] [Google Scholar]
- 32. Palmer BA, Hughes TB. Cubital tunnel syndrome. J Hand Surg Am. 2010;35(1):153-163. [DOI] [PubMed] [Google Scholar]
- 33. Polatsch DB, Melone CP, Jr, Beldner S, et al. Ulnar nerve anatomy. Hand Clin. 2007;23(3):283-289, v. [DOI] [PubMed] [Google Scholar]
- 34. Posner MA. Compressive neuropathies of the ulnar nerve at the elbow and wrist. Instr Course Lect. 2000;49:305-317. [PubMed] [Google Scholar]
- 35. Poujade T, Hanouz N, Lecoq B, et al. Ultrasound-guided surgical treatment for ulnar nerve entrapment: a cadaver study. Chir Main. 2014;33(4):256-262. [DOI] [PubMed] [Google Scholar]
- 36. Shahabpour M, Kichouh M, Laridon E, et al. The effectiveness of diagnostic imaging methods for the assessment of soft tissue and articular disorders of the shoulder and elbow. Eur J Radiol. 2008;65(2):194-200. [DOI] [PubMed] [Google Scholar]
- 37. Vanderpool DW, Chalmers J, Lamb DW, et al. Peripheral compression lesions of the ulnar nerve. J Bone Joint Surg Br. 1968;50(4):792-803. [PubMed] [Google Scholar]
- 38. Wilson TJ, Tubbs RS, Yang LJ. The anconeus epitrochlearis muscle may protect against the development of cubital tunnel syndrome: a preliminary study. J Neurosurg. 2016;125(6):1533-1538. [DOI] [PubMed] [Google Scholar]
- 39. Yamada K, Nagaoka M, Nagao S, et al. Anatomical study of Osborne’s ligament elongation in relation to elbow flexion. Nihon Univ J Med. 2013;72(3):154-158. [Google Scholar]


