Abstract
Objectives
Fines have been proposed as means for reducing non-attendance in healthcare. The empirical evidence of the effect of fines is however limited. The objective of this study is to investigate the effectiveness and cost-effectiveness of fining non-attendance at outpatient clinics.
Design, participants and setting
1:1 randomised controlled trial of appointments for an outpatient clinic, posted to Danish addresses, between 1 May 2015 and 30 November 2015. Only first appointment for users was included. Healthcare professionals and investigators were masked.
Intervention
A fine of DKK250 (€34) was issued for non-attendance. Users were informed about the fine in case of non-attendance by the appointment letter, and were able to reschedule or cancel until the appointment. A central administration office administered the fine system.
Main outcome measures
The main outcome measures were non-attendance of non-cancelled appointments, fine policy administration costs, net of productivity consequences and probability of fining non-attendance being cost-effective over no fining for a range of hypothetical values of reduced non-attendance.
Results
All of the 6746 appointments included were analysed. Of the 3333 appointments randomised to the fine policy, 130 (5%) of non-cancelled appointments were unattended, and of the 3413 appointments randomised to no-fine policy, 131 (5%) were unattended. The cost per appointment of non-attendance was estimated at DKK 56 (SE 5) in the fine group and DKK47 (SE 4) in the no-fine group, leading to a non-statistically significant difference of DKK10 (95% CI –9 to 22) per appointment attributable to the fine policy. The probability of cost-effectiveness remained around 50%, irrespective of increased values of reduced non-attendance or various alternative assumptions used for sensitivity analyses.
Conclusions
At a baseline level of around 5%, fining non-attendance does not seem to further reduce non-attendance. Future studies should focus on other means for reduction of non-attendance such as nudging or negative reinforcement.
Trial registration number
Keywords: non-attendance, randomized controlled trial, fines, fines for non-attendance
Strength and limitations of this study.
The strengths include a well-described context and nuanced effect measures.
Further, a main strength is the randomised allocation.
The main limitations include alternative fine amounts and generalisability to settings with lower patient volume or more specialised services where the flexibility of production could be more restricted.
Introduction
Non-attendance at scheduled appointments in outpatient clinics potentially affects society at all levels. Healthcare users may face longer waiting times, frustrated staff and poorer health outcomes.1–3 Healthcare staff may face difficulties planning their work efficiently and providing the service level that they judge to be appropriate. The healthcare system does not reach its potential in terms of productivity, efficiency and, ultimately, overall cost containment.4 At a societal level, and particularly when healthcare is tax financed, the sense of social justice may be affected if non-attendance is perceived as a matter of disrespect.
It is claimed that up to 25% of all planned appointments in outpatient service have been non-attended, but when accounting for cancellation on the part of the provider or the user, non-attendance accounts for only 5%–10% of appointments in somatic healthcare.5–9 In this work, non-attendance is defined as the phenomenon of users who have an appointment (not cancelled by the provider) but do not show up at the specified time and location without giving notice.
In a systematic literature review on the effect of various means for reducing non-attendance of somatic healthcare appointments, it was concluded that telephone, mail and text/short message service reminders reduced non-attendance by 9.4%, 8.6% and 7.6%, respectively.10 In another review, it was recommended that automated reminders should be routine practice, although it was noted that evidence of the cost-effectiveness of reminders was lacking.11 One of the most recent studies reports that flexible booking systems, where the patient is offered a choice between all available time slots in an online booking system, could further reduce non-attendance.12 While these areas of research are ongoing, both reminders and flexible bookings have been widely implemented, but non-attendance appears to remain an issue.
According to neoclassical economic theory, the threat of being fined for non-attendance could incentivise users to remember their appointments.4 More than 20 years ago, two independent observational studies suggested that fines could reduce non-attendance by between 14% and 54%.13 14 In the modern context, however, these estimates appear to have limited validity, and robust experimental evidence for the effect of fines in healthcare is lacking. Although the use of fines for the regulation of individual behaviour is widespread in relation to crime and traffic offences, in the case of public healthcare, there is limited experience, according to the scientific literature.
In Denmark, there are examples of privately practising specialists, dentists and physiotherapists who issue fines for non-attendance. There has been intense debate concerning the legitimacy of general practitioners using fines because it could have detrimental effects on equal access to healthcare. Nevertheless, there has been a political interest in this method aiming at reducing non-attendance, and nationally representative surveys have revealed that citizens have positive attitudes towards the use of such fine. Furthermore, qualitative research has shown that patients accept the use of fines and are positive towards this becoming a national policy.15 The objective of this study is to investigate the effectiveness and cost-effectiveness of a fine of DKK250 (€34) for non-attendance at outpatient appointments in comparison with the situation where there is no fine for non-attendance. The cost-effectiveness analysis is restricted to a healthcare perspective, essentially assessing the administration cost of a fine policy—net of any productivity consequences—versus the proportion of non-cancelled appointments that are non-attended. To the best of the authors’ knowledge, this study is the first experimental assessment of the effect of fines on non-attendance in public healthcare.
Methods
Design
The study was designed as a parallel, randomised controlled trial of 6746 appointments allocated to fine policy (n=3333) or to usual practice of no-fine policy (n=3413). Appointment status was followed from the time when an appointment was made until the date when the appointment had passed, and eventually when a fine had been settled or handed over to the tax authorities because of non-payment. Appointments made during the period from 1 May 2015 to 30 November 2015 were included.
This article follows the recommendations of the Consolidated Standards of Reporting Trials statement and the Consolidated Health Economic Evaluation Reporting Standards statement.16 17 The trial has been registered in current controlled trials by ISRCTN61925912, and a trial protocol has been previously published.18
Randomisation, masking and concealing
The randomisation was conducted when the appointment letter was issued; appointments allocated to the group that would involve fine for non-attendance without giving notice included an attachment describing the fine policy, whereas appointments allocated to the group following the usual practice of no fine did not include this attachment. Healthcare professionals, administrative staff and investigators were masked until the main results had been announced at a research meeting.
The randomisation procedure was based on a computerised and fully automatic random number draw from a binomial distribution. The letters E and K, for which only an external data manager knew the code, were assigned. The randomisation was concealed by the computerised technique, with the result of randomisation revealed to the appointment holder immediately in the majority of cases (via electronic appointment letters, which were general policy) or after processing time by the postal service (hard copy appointment letters sent to citizens without access to electronic mail).
Participants
Consecutive first-time appointments during the inclusion window and scheduled by an appointment letter were included in the trial. Appointment letters addressed to non-Danish addresses (Greenland and Faroe Islands) were excluded, as were appointments concerning physiotherapy and occupational therapy.18
Setting
The setting was an orthopaedic outpatient clinic of a regional hospital in Denmark. The Danish system is characterised by general practitioners acting as gatekeepers to the hospital sector and a national policy for a maximum waiting time to diagnosis of 30 days. The orthopaedic clinic’s activities have been detailed in a previous report focusing on the extent and possible explanations of non-attendance in the year before this trial was initiated.5 Of an annual volume of around 18 500 appointments, it was shown that 19% were cancelled and 5% were non-attended.18
Intervention
An attachment was enclosed to the appointment letter. This attachment informed the individual that in the case of non-attendance without giving notice, a fine of DKK250 (€34) would be issued. The size of the fine was determined by the Danish Ministry of Health and corresponds to the existing fine for specialised care. The individual was further informed that a secretary could be contacted for cancellation or rebooking during normal office hours, and that a central regional administrative office (Corporate Finance, Central Denmark Region) would handle any questions concerning the fine policy (preappointment requests, complaints, payment issues and so on). No deadline was set for giving notice; cancellation on the part of the user was accepted right up until the time of appointment. Apart from this attachment, the intervention did not alter the usual circumstances for the appointment.
A secretary at the orthopaedic department collected and registered non-attendance on a daily basis and sent a list to the central regional administrative office once a week. Fines were then issued and sent to the individuals by the same form of mail as used for the appointment letter. Fine recipients were given 4 weeks until the due date for payment. In the case of non-payment, users received up to two reminder letters, after which the settlement was handed over to the tax authorities.
Sample size
The study was powered to detect a reduction in non-attendance of at least 1.58 percentage points (from 4.8% to 3.22%), based on a χ2 test and 90% power. This would be obtainable at a sample size of 6500 appointments, randomised 1:1 to intervention and control.
Effectiveness
The primary effectiveness measure was non-attendance of a non-cancelled appointment without notice. The secondary effectiveness measures included cancellation on the part of the hospital, cancellation on the part of the user (giving notice about non-attendance) and, for users fined, the extent of payments and complaints. A data manager who was external to the research team extracted these data from the electronic patient file system and handed them over to the research team.
Costs
The costs of running a fine policy from a healthcare perspective were estimated by activity-based costing of the administration and register-based costing of the potential productivity loss when an appointment was unattended. All estimates are reported in their original currency (DKK) for the price year 2017 (DKK745=€100).
The activity-based costing was conducted for the entire period of intervention at the relevant office under the regional healthcare administration. The persons handling all activities relating to the fine system (receiving the lists of non-attenders, issuing the fines, taking phone calls from citizens and so on) registered their time use. Valuation of time was on established internal rates from the regional health administration. These include load factors of 1.71 for non-productive time and 1.09 for vacation time. A further load factor was included for tasks related to management, secretarial work and so on, such that the total cost per hour amounted to DKK801. The costs of the postal service, including printing letters, and the costs of electronic letters were based on market prices of DKK6.66 and DKK0.54, respectively, per letter. Finally, an overhead rate of 21% was used to account for rent, office supplies, information technology, telephone and other such expenses.
Appointment characteristics were informed from the hospital’s electronic system, and productivity loss was counted in case of non-attendance, based on the usual definition of production value according to the diagnosis-related grouping casemix system (see online supplementary appendix 1).
bmjopen-2017-019969supp001.pdf (136.3KB, pdf)
Cost-effectiveness
The main analysis contrasts two different assumptions about the productivity loss when an appointment is non-attended: the case when the staff cannot substitute the time freed with other relevant activity when an appointment is non-attended (100% productivity loss), and the case when, for example, another individual is available and willing to step in from the waiting room (0% productivity loss). The use of the extreme scenarios of 0% vs 100% productivity loss was made in retrospect of a qualitative organisational survey, demonstrating that the production in most cases is fully flexible such that the productivity loss approaches 0%, and to balance that with the most conservative assumption of 100% productivity loss. The net benefit framework19 20 is used to convert the overall cost and effect differences into a net monetary benefit for a range of hypothetical values of willingness-to-pay per 1% reduction in non-attendance. Cost-effectiveness acceptability curves are used to illustrate the results.21
Sensitivity analysis of the cost-effectiveness results
The administration cost of a fine system is potentially affected by economies of scale, such that, if it were rolled out in an entire healthcare system, it might be less costly than is estimated here. Therefore, a first sensitivity analysis is conducted under the assumption of a halved administration cost. When a user informs the provider that he/she does not plan to attend an appointment, some time lag occurs before the health professionals receive the message and reschedule their plans. Nevertheless, this protocol specified no deadline for cancellations. As a secondary sensitivity analysis, non-attendance was ignored to mimic that it made no difference. Finally, fines could have an effect not only on non-attendance but also on cancellation, which was, therefore, considered together with non-attendance in a third sensitivity analysis.
Statistical analysis
Conventional summary statistics were used for reporting the baseline characteristics. All of the analyses of outcomes adhere to the intention-to-treat principle, and all analyses are unadjusted. Effectiveness was analysed as frequencies, and the χ2 test was used to assess differences in counts between randomisation groups. Costs were analysed as arithmetic means, with bootstrapped SEs based on 10 000 replications, and differences between randomisation groups were reported along with 95% CI. A general significance level of 5% was used, and all analyses were undertaken in Stata V.14 for Mac.
User consent was not obtained in accordance with the Danish law given that the trial is considered to be a quality-improvement project and because the intervention does not affect the service provision once a person shows up to receive care.
Results
Participant flow
Of the 13 203 appointments scheduled at the clinic during the inclusion period, 6746 were eligible for inclusion and were randomised, resulting in 3333 in the fine group and 3413 in the no-fine group (see figure 1). There were no missing data on outcomes, and all randomised appointments were evaluated.
Figure 1.
Flow chart of the trial.
Included appointments
Both genders and all ages were represented in the appointments included in the trial (see table 1). The average distance from the user’s home to the hospital was 27 km, and the average wait from referral to appointment was around 30 days. Summer and autumn seasons were over-represented because the inclusion period ran from May to November. Wednesday and Thursday were under-represented when appointments were scheduled as a result of production planning. The majority of the included appointments concerned treatments exclusive of surgery (between 52% and 54%) or follow-ups (between 40% and 42%), whereas diagnostics and surgery each covered around 3%. None of the baseline characteristics were statistically significantly different between the randomisation groups.
Table 1.
Characteristics of included appointments (n=6746)
| No fine (n=3413) |
Fine (n=3333) |
|
| Gender of user | ||
| Female | 1761 (51.60) | 1718 (51.55) |
| Male | 1652 (48.40) | 1615 (48.45) |
| Age of user in years, mean (SD) | 48 (0.36) | 48 (0.37) |
| Kilometres between home and hospital, mean (SD) | 27 (0.41) | 27 (0.45) |
| Day of the week | ||
| Monday | 740 (21.68) | 772 (23.16) |
| Tuesday | 764 (22.38) | 751 (22.53) |
| Wednesday | 493 (14.44) | 458 (13.74) |
| Thursday | 619 (18.14) | 648 (19.44) |
| Friday | 797 (23.35) | 704 (21.12) |
| Days from referral to appointment, mean (SD) | 29 (0.55) | 30 (0.56) |
| Season | ||
| Spring | 130 (3.81) | 113 (3.39) |
| Summer | 1345 (39.41) | 1383 (41.49) |
| Autumn | 1723 (50.48) | 1597 (47.91) |
| Winter | 215 (6.30) | 240 (7.20) |
| Subspecialty | ||
| Hip | 239 (7.00) | 221 (6.63) |
| Hand | 321 (9.41) | 339 (10.17) |
| Knee | 656 (19.22) | 663 (19.89) |
| Back | 291 (8.53) | 286 (8.58) |
| Shoulder/elbow | 744 (21.80) | 762 (22.86) |
| Foot | 428 (12.54) | 389 (11.67) |
| Scapula alata | 16 (0.47) | 12 (0.36) |
| Arm | 6 (0.18) | 6 (0.18) |
| Leg | 11 (0.32) | 7 (0.21) |
| Unspecified | 701 (20.54) | 648 (19.44) |
| Appointment type | ||
| Follow-up | 1428 (41.84) | 1326 (39.78) |
| Treatment | 1768 (51.80) | 1804 (54.13) |
| Diagnostics | 107 (3.14) | 112 (3.36) |
| Surgery | 110 (3.22) | 91 (2.73) |
Values are n (%) unless otherwise stated.
None of the characteristics are significantly different between the groups (p<0.05).
Effectiveness and acceptance of the fine policy
There were no statistically significant differences between the randomisation groups in terms of cancellation or non-attendance (see table 2). Of the 3413 appointments in the no-fine group, 716 (21%) were cancelled, and of the 3333 in the fine group, 707 (21%) were cancelled. Of the 2697 appointments not cancelled in the no-fine group, 131 (5%) were non-attended, and of the 2626 appointments in the fine group, 130 (5%) were non-attended.
Table 2.
The effect of fine on cancellation and non-attendance (n=6746)
| No fine (n=3413) | Fine (n=3333) | P values | |
| n (%) | n (%) | ||
| Cancellation | |||
| By hospital | 533 (15.62) | 513 (15.39) | 0.798 |
| By user | 183 (5.36) | 194 (5.82) | 0.412 |
| Total cancellation | 716 (20.98) | 707 (21.21) | 0.814 |
| Non-attendance | |||
| Of non-cancelled appointments | 131 (4.86 | 130 (4.95) | 0.875 |
| Of all appointments | 131 (3.84) | 130 (3.90) | 0.895 |
Complaints and payment status were monitored in the fine group as a reflection of the acceptance of the fine policy (see table 3). Of the 130 valid fines issued, only 27 (21%) were paid (three after complaints). Of the 103 unpaid fines, a complaint was made in 22 cases (21%), whereas the remaining 81 (79%) were unpaid even after two reminder letters.
Table 3.
Complaint and payment status for the fines issued (n=130)
| n | % of paid/unpaid | % of all | |
| Paid | |||
| Without complaint | 24 | 88.89 | 18.46 |
| With complaint | 3 | 11.11 | 2.31 |
| Total paid | 27 | 100.00 | 20.77 |
| Unpaid | |||
| Without complaint | 81 | 78.64 | 62.31 |
| With complaint | 22 | 21.36 | 16.92 |
| Total unpaid | 103 | 100.00 | 79.23 |
Costs and cost-effectiveness
An administration cost of DKK7.72 per appointment was estimated for the fine policy, based on the micro costing (see table 4). This cost was based on: 727 staff min used on answering phone calls, or mail from users, with questions or complaints; 650 min used to issue the fines and generate credit notes, in the cases where the fine was annulled after complaint; and 155 min used on other fine-related administration tasks.
Table 4.
Administrative costs of fine, based on microcosting of activity in the intervention component of the trial (n=3333) (2017 DKK)
| Units | Unit cost | Total | Total per appointment | |
| Office clerk | ||||
| Telephone/mail (min) | 727 | 13 | 9451 | 2.84 |
| Invoices and credit notes (min) | 650 | 13 | 8450 | 2.54 |
| Other fine-related administration (min) | 155 | 13 | 2015 | 0.60 |
| Subtotal office clerk | NA | NA | 19 916 | 5.98 |
| Materials | ||||
| Fine letter (electronic) | 129 | 0.54 | 70 | 0.02 |
| Fine letter (postal mail) | 14 | 6.66 | 93 | 0.03 |
| Reminder letter | 178 | 6.66 | 1185 | 0.36 |
| Subtotal materials | NA | NA | 1348 | 0.40 |
| Total exclusive overhead | 21 264 | 6.38 | ||
| Overhead | 4466 | 1.34 | ||
| Total inclusive overhead | 25 730 | 7.72 | ||
NA, not applicable.
The productivity loss resulting from non-attendance was observed to be similar in the randomisation groups, with an average value of around DKK50 per appointment, and with a difference between randomisation groups of DKK2 (CI –11 to 15) per appointment. This generated a total cost of non-attendance of DKK47 (SE 4) per appointment in the no-fine group and DKK56 (SE 5) per appointment in the fine group, leading to a non-statistically significant difference of DKK10 (CI –9 to 22) per appointment (see table 5).
Table 5.
The effect of a fine on the costs of non-attendance per appointment (2017 DKK)
| No fine (n=3413) |
Fine (n=3333) |
Difference (95% CI) |
|
| Administrative cost of fine policy | NA | 7.72 (NA) | 7.72 (NA) |
| Production value of non-attended appointments | |||
| Consultation | 8.66 (1.30) | 8.26 (1.27) | –0.39 (–3.98 to 3.19) |
| Consultation with X-ray | 6.86 (1.52) | 8.08 (1.71) | 1.22 (–2.93 to 6.08) |
| Extended consultation | 15.55 (2.48) | 17.55 (2.64) | 2.00 (–5.16 to 9.17) |
| Extended consultation with X-ray | 14.18 (2.75) | 12.28 (2.61) | –1.89 (–9.29 to 5.50) |
| Decompression of carpal tunnel | 0.00 (0.00) | 2.48 (1.99) | 2.48 (–1.43 to 6.40) |
| Minor excision | 1.62 (1.03) | 0.00 (0.00) | –1.62 (–3.64 to 0.40) |
| Total production value | 46.88 (4.34) | 48.68 (4.90) | 1.80 (–10.99 to 14.58) |
| Grand total | 46.88 (4.33) | 56.40 (4.96) | 9.52 (–3.41 to 22.44) |
Values are means (bootstrapped SE).
NA, not applicable.
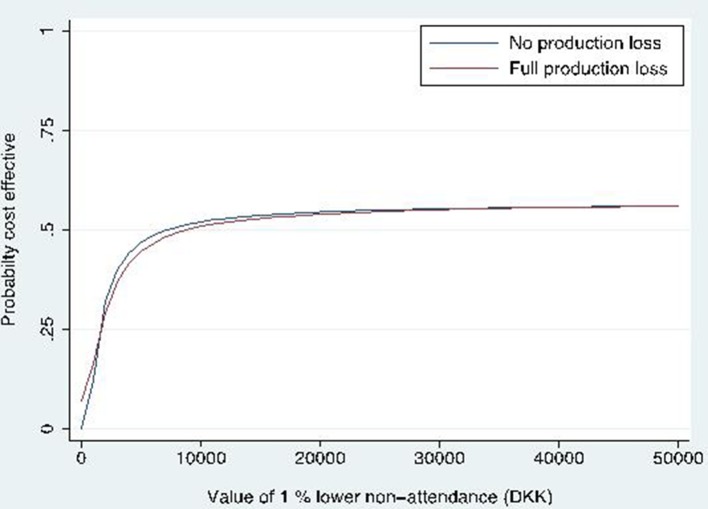
The probability of a fine policy being cost-effective over no-fine policy was found to converge to just above 50% for values of reducing non-attendance above DKK10 000 (see figure 2). The extent to which productivity was affected in the case of non-attendance had little effect on cost-effectiveness because of the lack of statistically significant cost and effect differences between fine and no-fine policies. This also applied to the results of the sensitivity analyses which did not substantially affect the main result (see figure 3).
Figure 2.
Probability of the fine being cost-effective compared with no fine for hypothetical values of willingness-to-pay for reducing non-attendance. DKK, DKK.
Figure 3.

Assessment of the influence of alternative scenarios on the main result. DKK, DKK; non-att., non-attendance.
Discussion
Despite a power to detect a reduction in non-attendance of 1.5% from the expected baseline level of around 4%, no effect was observed, and the degree of non-attendance was equivalent with and without a fine policy of DKK250 (€34) in case of non-attendance. Thus, we can also state that we did not observe any consequences for departmental productivity and that the probability of a fine policy being cost-effective did not substantially exceed 50%, given the lack of clear directions observed in cost and effect differences between the randomisation groups. However, a number of complexities apply to this seemingly straightforward interpretation.
The randomised real world nature of the study design is a major strength in relation to assessing impacts on individual behaviour, and it is supported by the immediate concealment and strict masking of health professionals and investigators. Furthermore, the context is well described, and the effect measure is nuanced in terms of disentangling cancellation and non-attendance. However, experimental research on system-level policies is quite complex, in that effects could flow at several levels. A key dilemma, therefore, is whether to prioritise individual-level effects or organisational-level effects when defining the unit for randomisation. We judged that randomisation at the individual level would lead to the most important and first-line effect of attendance. It is also a prerequisite for broader consequences because if individuals do not react to a fine policy, the scope for organisational consequences of non-attendance quickly diminishes. If we on the other hand had observed an effect, we would have potentially overlooked derived effects at the organisational or societal level, such as the job satisfaction of staff and the preservation of the citizens’ sense of social justice.
The same argument applies to the cost side of the equation, where we adopted a relatively simple perspective on the administration costs of the fine policy and the potential consequences of non-attendance to productivity. That perspective omits more complex costs that, from the user perspective, might be significant if, for instance, the appointment is part of a series of appointments, or if the user lives far from the provider and/or is planning assistance to enable him/her to attend. Nevertheless, the well-defined but relatively narrow perspective of this trial does not represent a weakness because individuals simply did not react to the fine policy. Instead, we consider that the most important weaknesses of the trial relate to the implementation of the fine policy; that is, whether the amount of the fine was sufficient to generate a reaction and whether the way that it was presented to users (via the attachment to appointment letter) meant that they recognised the policy in time to react.
We are not aware of any studies that have assessed the dose–response relationship for fining non-attendance, and it should be noted that this relationship will be highly context specific and closely related not only to the income of users but also to, for example, their culture and experience with fines in other areas, infrastructure and likelihood of force majeure. The amount of DKK250 (€34) used in this trial was chosen because it was determined that it would not affect equity negatively and that all users would be able to pay. Furthermore, it was noted that similar (or indeed higher) fines have been imposed for years by privately practising practitioners. The lack of an effect could have arisen because the incentive to attend was too weak and/or because the user had no choice regarding non-attendance because he/she was unaware of the appointment or was restricted by ill health or other circumstances. We note, however, that the characteristics of non-attenders have previously been reported, and they do not indicate ill health.5 We are currently investigating whether certain patient groups were disproportionately affected by the fine policy such that it could have had consequences for access and equity. However, given the lack of an effect of the fine policy, there is little room for any detrimental effects on these aspects.
Unfortunately, although the reasons for non-attendance could have been formally investigated in the implementation research alongside the trial, this was not undertaken. However, 44 of the users in the fine group were interviewed as part of a qualitative focus group study which found that they were indeed aware of the fine policy.15 This suggests that the reason for non-attendance may not be restricted to carelessness or forgetfulness but that it could be a particular obstacle such as, for example, acute illness for which a fine policy has no effect. In an observational study on reasons for non-attendance in a neurological clinic, 28% were explained by forgetfulness, 16% by acute illness, 15% by administrative errors on the part of the clinic and 13% by the fact that the patient no longer felt the need, among others.8 When the reasons for non-attendance include illness or inability to cancel an appointment for which one does no longer feel the need, it raises the question whether non-attendance can be reduced much further down than the current 5%. Flexible booking and reminder systems seem to be able to reduce non-attendance down to 5%–10%, and once that has been achieved, remedies that target reasons beyond convenience and forgetfulness are required.
Research is ongoing in terms of the future direction for non-attendance and, in a number of recent studies, the role of the general practitioner, as well as the collaboration between general practice and specialised care, appears to be important. It is suggested that general practitioners should follow-up on their patients’ attendance at hospital appointments22 and that focusing on ‘banalities’, such as sharing updates and contact information, is important.23 24 Another stream of research focuses on the development of systems for identifying users at greatest risk of not attending who can then be supported in order to prevent non-attendance.25 Support could be in the form of service management tailored to specific groups26 or patient education and differentiated communication strategies; for example, for low-literacy groups.27 Finally, it has been suggested simply that more decentralised care should be considered, after years of centralisation and specialisation, where the distance between the users’ homes and the providers in many settings has increased.28
The main limitation of this study is its specific context of an orthopaedic clinic of the Danish national health service. Generalisability to other clinical specialties should be made with caution and considering the characteristics of the appointments and users including age, gender and functional ability.5 The generalisability of first-time appointments during the summer and autumn seasons should also be considered. While we believe that a patient’s reaction to the first threat of a fine is a good predictor for later reactions, we cannot rule out that repetitive threats and/or general experience with a fine system changes the behavioural response. On the one hand, experience could increase awareness and thereby the impact of fines and, on the other hand, experience could also generate knowledge on how to get a fine cancelled such that it is less of a threat. In this particular context of orthopaedics, one appointment letter is often used to cover more than one appointments. Had we chosen to include all as opposed to first-time appointments we could not have controlled the dose of fine attachments whereas in this case every person has had exactly one attachment to react to. As concerns seasonal variation, we have previously examined the characteristics of non-attended appointments (season, day of week and time of day) and found no evidence of seasonality.5
In conclusion, this study has contributed to the literature with the somewhat cheerless results that fining non-attendance might not reduce non-attendance levels much further if they have already been lowered to around 5%, based on optimisation of bookings and use of reminders. Future studies of other contexts, particularly those where non-attendance is a greater problem, might arrive at different conclusions. However, for contexts similar to the one examined in this study, further means of reducing non-attendance appears to relate to communication and collaboration between general practices and hospitals, and perhaps it needs to be accepted that non-attendance is a phenomenon that has a lower limit, below which it cannot be further reduced.
Supplementary Material
Acknowledgments
The authors wish to thank the recruitment site, the Orthopaedic Surgery Department at Viborg Regional Hospital, for their support, especially the medical secretaries for management of the data. The authors would also like to thank both Per Jensby and Mette Jensen from Corporate Finance, Central Denmark Region, for their administrative work related to the fine and the handling of patient complaints and requests. Finally, the authors are grateful for support from Chief Strategist Mogens Engsig-Karup from the IT Department, Central Denmark Region, for the implementation of the automatic randomisation system and from BI-designer Tommy Kieffer Sørensen from the Business Intelligence Unit, Central Denmark Region, for providing data.
Footnotes
Contributors: All authors conceived and designed the study. EEB and UV managed the conduction of the trial and collected the data. RS supervised the analytical design and analysis which was conducted by EEB. The manuscript was drafted by EEB, and all authors contributed to critical revision and approved the final manuscript.
Funding: This work was funded by Danish Regions, Ministry of Health and Prevention and Central Denmark Region.
Disclaimer: The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript.
Competing interests: None declared.
Ethics approval: The local ethics committee reviewed the project and considered it to be a quality-improvement project outside of their responsibility (see the Committee Law, Section 2, No. 1). The Ministry of Health and Prevention approved the trial protocol (see the Health Legislation, Section 233, Subsections 1 and 3).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data are owned by a third party and not available for public sharing.
Author note: EEB (Msc) is Research Assistant at the Department of Health Economics at DEFACTUM, Central Denmark Region. UV (PhD) is Senior Researcher at the Department of Health Services Research at DEFACTUM, Central Denmark Region. RS (PhD) is Professor of Health Economics at the Department of Public Health and the Department of Clinical Medicine at Aarhus University.
References
- 1. Kempny A, Diller GP, Dimopoulos K, et al. Determinants of outpatient clinic attendance amongst adults with congenital heart disease and outcome. Int J Cardiol 2016;203:245–50. 10.1016/j.ijcard.2015.10.081 [DOI] [PubMed] [Google Scholar]
- 2. Killaspy H, Banerjee S, King M, et al. Prospective controlled study of psychiatric out-patient non-attendance. Characteristics and outcome. Br J Psychiatry 2000;176:160–5. [DOI] [PubMed] [Google Scholar]
- 3. Stav K, Dwyer PL, Rosamilia A, et al. Long-term outcomes of patients who failed to attend following midurethral sling surgery--a comparative study and analysis of risk factors for non-attendance. Aust N Z J Obstet Gynaecol 2010;50:173–8. 10.1111/j.1479-828X.2010.01138.x [DOI] [PubMed] [Google Scholar]
- 4. Bech M. The economics of non-attendance and the expected effect of charging a fine on non-attendees. Health Policy 2005;74:181–91. 10.1016/j.healthpol.2005.01.001 [DOI] [PubMed] [Google Scholar]
- 5. Blæhr EE, Søgaard R, Kristensen T, et al. Observational study identifies non-attendance characteristics in two hospital outpatient clinics. Dan Med J 2016;63:A5283. [PubMed] [Google Scholar]
- 6. Menendez ME, Ring D. Factors associated with non-attendance at a hand surgery appointment. Hand 2015;10:221–6. 10.1007/s11552-014-9685-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Health and Social Care Information Centre. Hospital outpatient activity 2012–13. 2013. http://www.hscic.gov.uk/catalogue/PUB13005/hosp-outp-acti-2012-13-summrepo-rep.pdf
- 8. Roberts K, Callanan I, Tubridy N. Failure to attend out-patient clinics: is it in our DNA? Int J Health Care Qual Assur 2011;24:406–12. 10.1108/09526861111139214 [DOI] [PubMed] [Google Scholar]
- 9. Corfield L, Schizas A, Noorani A, et al. Non-attendance at the colorectal clinic: a prospective audit. Ann R Coll Surg Engl 2008;90:377–80. 10.1308/003588408X301172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Stubbs ND, Geraci SA, Stephenson PL, et al. Methods to reduce outpatient non-attendance. Am J Med Sci 2012;344:211–9. 10.1097/MAJ.0b013e31824997c6 [DOI] [PubMed] [Google Scholar]
- 11. Hasvold PE, Wootton R. Use of telephone and SMS reminders to improve attendance at hospital appointments: a systematic review. J Telemed Telecare 2011;17:358–64. 10.1258/jtt.2011.110707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dusheiko M, Gravelle H. Choosing and booking-and attending? Impact of an electronic booking system on outpatient referrals and non-attendances. Health Econ 2017. 10.1002/hec.3552 [DOI] [PubMed] [Google Scholar]
- 13. Mäntyjärvi M. No-show patients in an ophthalmological out-patient department. Acta Ophthalmol 1994;72:284–9. 10.1111/j.1755-3768.1994.tb02760.x [DOI] [PubMed] [Google Scholar]
- 14. Lesaca T. Assessing the influence of a no-show fee on patient compliance at a CMHC. Adm Policy Ment Health 1995;22:629–31. 10.1007/BF02254826 [DOI] [Google Scholar]
- 15. Lou S, Frumer M, Olesen S, et al. Danish patients are positive towards fees for non-attendance in public hospitals. A qualitative study. Dan Med J 2016;63:A5252. [PubMed] [Google Scholar]
- 16. Husereau D, Drummond M, Petrou S, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMJ 2013;346:f1049 10.1136/bmj.f1049 [DOI] [PubMed] [Google Scholar]
- 17. Schulz KF, Altman DG, Moher D, et al. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Trials 2010;11:32 10.1186/1745-6215-11-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Blæhr EE, Kristensen T, Væggemose U, et al. The effect of fines on nonattendance in public hospital outpatient clinics: study protocol for a randomized controlled trial. Trials 2016;17:288 10.1186/s13063-016-1420-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Stinnett AA, Mullahy J. Net health benefits: a new framework for the analysis of uncertainty in cost-effectiveness analysis. Med Decis Making 1998;18(2 Suppl):S68–80. 10.1177/0272989X98018002S09 [DOI] [PubMed] [Google Scholar]
- 20. Hoch JS, Briggs AH, Willan AR, old S. Something old, something new, something borrowed, something blue: a framework for the marriage of health econometrics and cost-effectiveness analysis. Health Econ 2002;11:415–30. 10.1002/hec.678 [DOI] [PubMed] [Google Scholar]
- 21. Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ 2001;10:779–87. 10.1002/hec.635 [DOI] [PubMed] [Google Scholar]
- 22. Cameron E, Heath G, Redwood S, et al. Health care professionals' views of paediatric outpatient non-attendance: implications for general practice. Fam Pract 2014;31:111–7. 10.1093/fampra/cmt063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hirani N, Karafillakis EN, Majeed A. Why children do not attend their appointments: is there a need for an interface between general practitioners and hospitals allowing for the exchange of patients’ contact details? JRSM Open 2016;7:20 10.1177/2054270416648046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. French LR, Turner KM, Morley H, et al. Characteristics of children who do not attend their hospital appointments, and GPs' response: a mixed methods study in primary and secondary care. Br J Gen Pract 2017;67:e483–9. 10.3399/bjgp17X691373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Guedes R, Leite I, Baptista A. Dermatology missed appointments: an analysis of outpatient non-attendance in a general hospital’s population. Int J Dermatol 2014;53:39–42. 10.1111/j.1365-4632.2012.05710.x [DOI] [PubMed] [Google Scholar]
- 26. Hynes L, Byrne M, Dinneen SF, et al. Barriers and facilitators associated with attendance at hospital diabetes clinics among young adults (15-30 years) with type 1 diabetes mellitus: a systematic review. Pediatr Diabetes 2016;17:509–18. 10.1111/pedi.12198 [DOI] [PubMed] [Google Scholar]
- 27. Hung SL, Fu SN, Lau PS, et al. A qualitative study on why did the poorly-educated Chinese elderly fail to attend nurse-led case manager clinic and how to facilitate their attendance. Int J Equity Health 2015;14:10 10.1186/s12939-015-0137-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McLeod H, Heath G, Cameron E, et al. Introducing consultant outpatient clinics to community settings to improve access to paediatrics: an observational impact study. BMJ Qual Saf 2015;24:377–84. 10.1136/bmjqs-2014-003687 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-019969supp001.pdf (136.3KB, pdf)