Abstract
Objective
To conduct a systematic review and meta-analyses to assess the effect of manual therapy interventions for healthy but unsettled, distressed and excessively crying infants and to provide information to help clinicians and parents inform decisions about care.
Methods
We reviewed published peer-reviewed primary research articles in the last 26 years from nine databases (Medline Ovid, Embase, Web of Science, Physiotherapy Evidence Database, Osteopathic Medicine Digital Repository, Cochrane (all databases), Index of Chiropractic Literature, Open Access Theses and Dissertations and Cumulative Index to Nursing and Allied Health Literature). Our inclusion criteria were: manual therapy (by regulated or registered professionals) of unsettled, distressed and excessively crying infants who were otherwise healthy and treated in a primary care setting. Outcomes of interest were: crying, feeding, sleep, parent–child relations, parent experience/satisfaction and parent-reported global change.
Results
Nineteen studies were selected for full review: seven randomised controlled trials, seven case series, three cohort studies, one service evaluation study and one qualitative study.
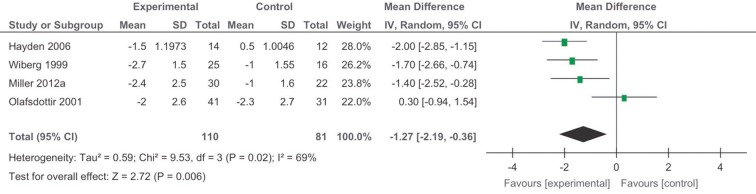
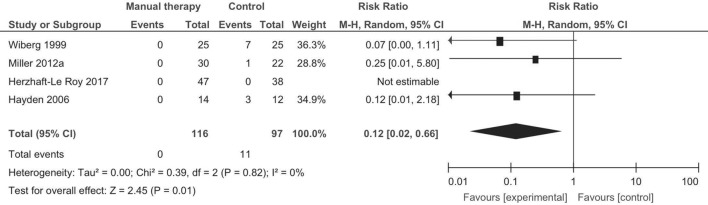
We found moderate strength evidence for the effectiveness of manual therapy on: reduction in crying time (favourable: −1.27 hours per day (95% CI −2.19 to –0.36)), sleep (inconclusive), parent–child relations (inconclusive) and global improvement (no effect). The risk of reported adverse events was low: seven non-serious events per 1000 infants exposed to manual therapy (n=1308) and 110 per 1000 in those not exposed.
Conclusions
Some small benefits were found, but whether these are meaningful to parents remains unclear as does the mechanisms of action. Manual therapy appears relatively safe.
PROSPERO registration number
CRD42016037353.
Keywords: Manual Therapy, Paediatrics, ’colic', Excessive Crying, Infants
Strengths and limitations of this study.
Meaningful outcomes for parents with distressed, unsettled and excessively crying infants were investigated to help inform their decisions about seeking manual therapy care for their infants.
Compiling evidence for distressed, unsettled and excessively crying infants based on multiple ‘clinical diagnoses’ using varied definitions is difficult.
The mechanism of action of complex interventions was not explained by the pragmatic research investigations used in this review.
Low to moderate quality studies limited the certainty of conclusions, suggesting they are liable to change with further research.
Introduction
Unsettled infant behaviour and colic are terms used to describe a range of behaviours in infants aged up to 12 months that include prolonged episodes of crying, difficulties with sleeping and/or feeding.1 Reports suggest a prevalence of approximately 20%,2 and the incidence is equal between sexes.3 The problems are found more commonly in first-borns and infants who have siblings who also had this condition.4–6 High levels of multiple health service use have been found in the postpartum period, including visits to emergency departments.1 4 A cost burden analysis found that the annual cost to the UK National Health Service of infant crying and sleeping problems in the first 12 weeks of life was £65 million.5 There are associations between unsettled infant behaviour and high maternal depression scores,6 and the natural crying peak at 6 weeks coincides with the peak age for severe infant injury or death as a result of child abuse.7
Many aetiological factors for unsettled infant behaviour have been explored including diet, feeding and digestive issues,8–11 musculoskeletal strains and disorders,12 13 developmental progress14–17 and parenting.18–22 Despite extensive research, causative factors and effective treatment remain elusive.
Medicalising these symptoms is controversial as they are seen as self-limiting with infants normally settling after 12 weeks. However, coping with these infants during this period can be very difficult.
Manual therapists offer a mix of health screening, education, advice, psychological support and touch therapy for these infants. Manual treatment is based on the premise that infants may have musculoskeletal strains or limitations affecting comfort, feeding and gut motility causing distress. A previous Cochrane review (2012) of manual therapy and colic meta-analysed data from six randomised controlled trials (RCTs) and found small positive (statistically significant) changes in crying time outcomes overall. However, a sensitivity analysis of data from only RCT studies where parents were blinded to treatment did not show beneficial effects.23 Other analyses showed a small beneficial effect for sleep but not for ‘recovery’. The studies included in this review were generally small and methodologically prone to bias, so definitive conclusions could not be drawn and effects were downgraded accordingly.23
There are some concerns around the safety of manual techniques in the treatment of infants, but published data of cases of serious adverse events are rare.24 No reviews to our knowledge have explored qualitative research and non-specific effects such as parental confidence and satisfaction. In this review, we aimed to update the Cochrane review23 of RCTs for crying time and investigate non-RCT studies and outcomes that are important to parents, rather than biomedical markers alone that might be of more interest to primary researchers exploring aetiology as our selected population was infants that were considered healthy.
Method
Types of studies
We included the following types of peer-reviewed studies in our search: RCTs, prospective cohort studies, observational studies, case–control studies, case series, questionnaire surveys and qualitative studies. We excluded single-case studies and non-peer reviewed literature (editorials, letters, master’s and undergraduate theses). Systematic reviews were identified to inform our research and for citation tracking. There were no language restrictions in our search criteria.
Types of participants
Participants were aged between 0 months and 12 months (infants) when they received manual therapy treatment. They were healthy, thriving and not receiving other medical interventions. Their presenting symptoms were excessive crying, distress and unsettledness; they might also be described as having colic, constipation, breastfeeding/feeding difficulties and/or gastro-oesophageal reflux/discomfort.
‘Colic’ was determined using the Wessel ‘rule of three’25 or Rome III26 criteria. The latter considers infants to have colic if they were thriving and healthy but had paroxysms of irritability, fussing or crying lasting for a total or more than 3 hours a day and occurring on more than 3 days a week for more than 1 week.26
We excluded studies that included infants requiring treatment for conditions that needed specialist or hospital-based clinical care for conditions such as: respiratory disorders, developmental disorders (learning and motor), cystic fibrosis, cerebral palsy, otitis media, neuralgia, congenital torticolis or musculoskeletal trauma. We also excluded studies about plagiocephaly or brachycephaly.
The intervention
We included studies where the manual therapy intervention was delivered in primary care by statutorily registered or regulated professional(s). This included osteopaths, chiropractors, physiotherapists and any other discipline using manual contact as the primary therapeutic component. The intervention or therapy had to involve physical and/or manual contact with the patient for therapeutic intent, administered without the use of mechanical, automated, electronic, computer or pharmacological aids/products/procedures. We excluded mixed or multidisciplinary interventions where the response to the manual therapy elements would have been unclear/undeterminable. Studies where the professional trained a non-professional to deliver the therapy or where parents delivered the therapy were excluded also.
Types of outcome measures
Outcomes of interest were unsettled behaviours, experience/satisfaction and global change scores. Unsettled behaviours included, for example, excessive crying, lack of sleep, displays of distress or discomfort (back arching and drawing up of legs) and difficulty feeding. Adverse events data were also collected.
Selection of articles
Nine electronic databases were searched from January 1990 to January 2017 in the last 26 years: Medline Ovid, Embase, Web of Science (WOS), Physiotherapy Evidence Database, Osteopathic Medicine Digital Repository, Cochrane (all databases), Index of Chiropractic Literature, Open Access Theses and Dissertations and Cumulative Index to Nursing and Allied Health Literature. We selected this timeframe because our scoping work revealed that most papers prior to January 1990 were theory-driven position papers on the manual therapy care of infants and for pragmatic reasons in terms of access to full-text original articles.
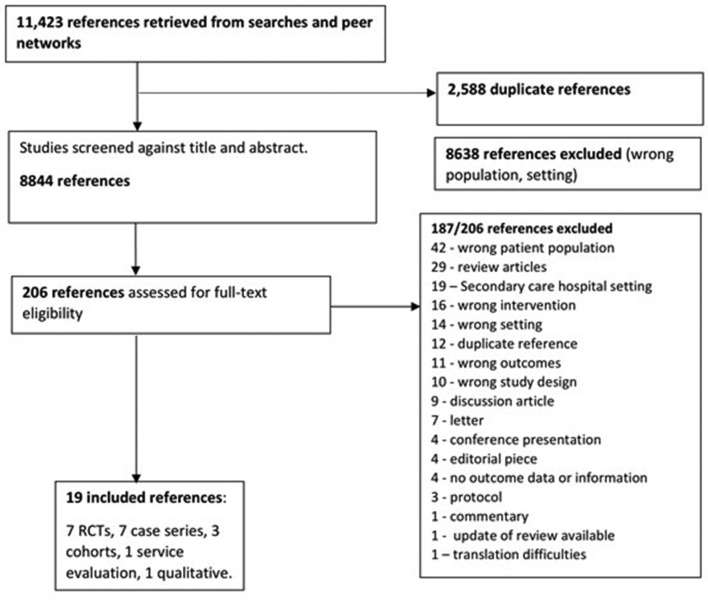
The main search string (modified for the different engines) is included in the electronic online supplementary appendices. It included the key terms: musculoskeletal, manipulation, manual and physical therapy, physiotherapy, osteopathy and chiropratic with infant baby and new borns. We updated the search to the end of January 2017 using Medline Ovid and search alerts from Embase, Cochrane and WOS. We also located articles through peer networks. Four reviewers (the authors in two teams of two) reviewed the titles and abstracts, then the full texts independently. Where there was disagreement between the reviewers, a third reviewer from the other team arbitrated the final decision to select reject. Review articles retrieved in the search were citation tracked to identify additional studies. Covidence software was used to organise and classify the articles.27 See figure 1 for a flow chart of the search process.
Figure 1.
Flow chart of search process for the review. RCTs, randomised controlled trials.
bmjopen-2017-019040supp001.pdf (271.1KB, pdf)
Quality appraisal of included studies
Two reviewers independently rated the quality of each included study (either CM/JE or DC/AP). We used the appropriate quality appraisal tools for each type of study design.28–30 An overall quality score for each study was assigned by summing the number of quality criteria that were present. For RCTs: six risk of bias criteria were assessed28 (5–6 quality criteria evaluated as present indicated low risk of bias=high quality, 3–4=moderate quality and 1–2=low quality). For cohorts: 11 quality criteria were assessed29 (8–11 quality criteria evaluated as present=high quality, 4–7=moderate quality, 0–3=low quality). For case series: nine quality criteria were assessed30 (if 7–9 quality criteria were present=high quality, if 3–6=moderate quality and if 0–3=low quality). For qualitative studies: 10 criteria were assessed29 (if 8–10 quality criteria were present=high quality, 4–7=moderate quality and 0–3=low quality). All low quality cohort and case series studies were regarded as severely methodologically flawed and were not included in the final analyses.
Data extraction and synthesis
One reviewer extracted the data and another checked the data extractions (all authors).
Analyses
We aimed to meta-analyse data for RCTs and matched or paired cohort studies. For RCTs, we planned to extract final value scores for each group and convert them to standardised mean differences and weighted mean differences for comparison using a random effects model due to the expected differences in treatment protocols and effects between studies. Where there was a majority of either change or final value scores, we planned sensitivity analysis to check ‘consistency’/meaning of the meta-analyses. We planned to extract risk ratios (RR) for comparison of adverse events between treatment and control groups. I2 was used to calculate heterogeneity. RevMan software (V.5.3) was used to conduct the meta-analyses.
For non-RCT studies, analyses proposed were descriptive and narrative, but change scores and RRs were extracted where possible. If there were a sufficient number of qualitative studies, we proposed to organise and synthesise findings from the qualitative data, by identifying emergent themes and subthemes.
Strength of evidence
We rated the strength of evidence across studies for each outcome, as either high, moderate or low, taking note of the quality and overall direction of results (inconclusive, favourable or unfavourable).31 Strength of evidence was considered as follows:
High
Consistent results from at least two high-quality RCTs, or other well-designed studies, conducted in representative populations where the conclusion is unlikely to be strongly affected by future studies.
Moderate
Available evidence from at least one higher quality RCT or two or more lower quality RCTs but constrained by: number, size, quality, inconsistency in findings and limited generalisability to clinical practice. The conclusions are likely to be affected by future studies.
Low
Evidence was insufficient with limitations in data provision, number, power, quality, inconsistency in results and findings not generalisable to clinical practice. All studies that were rated as low quality were treated as inconclusive regardless of author findings.
Two reviewers rated the quality and strength of evidence, and a consensus vote was used in cases of disagreement.
Results
Search results
A total of 11 423 studies were retrieved. After duplicate removal, 8844 studies remained. There were 8638 references excluded by title and abstract predominantly because the population was not appropriate; for example, the children were too old and/or treatment settings were not primary care. We acquired full text for 206 references and 19 of these fulfilled our inclusion criteria. Reasons for exclusion are listed in figure 1.
There were 19 primary studies included: seven RCTs,32–38 seven case series,39–45 three cohort studies,46–48 one service evaluation survey49 and one qualitative study.50 One other primary study was excluded due to translation difficulties of technical terms in Chinese medicine.51 All studies were published between January 1990 and January 2017. Countries represented across the studies were the UK,32–34 41–43 46 47 49 USA,35 40 48 Canada,38 Australia,39 44 50 Norway36 and Denmark.37 45 The following conditions were represented in the studies: colic (11 studies),32–34 36 37 39 40 43 45–47 gastro-oesophageal reflux (2 studies),35 40; breastfeeding difficulties (5 studies)38 42 44 48 49 and infant signs of distress (described as headache) (1 study).41 With the exception of four studies, all used chiropractic intervention. The other four studies used massage therapy35 and osteopathic intervention.33 38 49 Eight studies used control groups.32–36 38 46 47 The controls varied across studies, from no physical treatment33 34 36 46 47 to a sham treatment35 38 or drug.37 See table 1 for characteristics of included studies.
Table 1.
Characteristics, study design and quality rating of included studies
| Author, year | Country of study | Participants reported condition | Type of study design and follow-up period (FU) | Intervention | Outcomes reported | Quality appraisal |
| Browning and Miller,32 2008 | UK | Colic | Randomised controlled trial (RCT) (spinal manual therapy versus occipital decompression FU: 4 weeks post-treatment |
Chiropractic | Sleep Resolution of symptoms |
High |
| Hayden and Mullinger,33 2006 | UK | Colic | RCT Osteopathic treatment versus no treatment FU: 4 weeks |
Osteopathy | Parents involvement Sleep Crying |
Mod |
| Herzhaft-Le Roy et al, 38 2017 | Canada | Breastfeeding difficulties | RCT groups: osteopathic treatment versus sham FU: over 10 days |
Osteopathy+lactation consultant | Feeding Nipple pain Global improvement |
High |
| Miller et al,34 2012 | UK | Colic | RCT: treatment blinded versus treatment not blinded versus no treatment blinded FU: 10 days |
Chiropractic | Crying Improved Global change |
High |
| Neu et al,35 2014 | USA | Gastro-oesophageal reflux | Pilot RCT: massage versus no massage FU: 6 weeks |
Massage therapy | Parent–child relations | High |
| Olafsdottir et al,36 2001 | Norway | Colic | RCT: chiropractic versus no treatment FU: over 8–14 days |
Chiropractic | Crying hours Improvement of symptoms | Mod |
| Wiberg et al,37 1999 | Denmark | Colic | RCT: chiropractic versus dimethicone FU: between 8 and 11 days |
Chiropractic | Daily hours of infantile colic | Low |
| Miller and Phillips,47 2009a | UK | Colic | Controlled cohort study FU: behaviour at 2–3 years of age |
Chiropractic | Sleep Temper tantrums |
Low |
| Miller and Newell,46 2012b | UK | Colic | Prospective cohort study FU: end of treatment (duration, not reported) |
Chiropractic | Consolability, crying personal stress, sleep |
Low |
| Miller et al,49 2016 | UK | Breastfeeding difficulties | Service evaluation (survey) FU: 6–12 weeks after attending clinic |
Chiropractic and midwife | Breastfeeding | Mod |
| Vallone,48 2004 | USA | Breastfeeding difficulties | Cohort study: infants with breastfeeding difficulties versus infants without difficulties FU: over 6–8 weeks |
Chiropractic | Feeding | Low |
| Davies,39 2007 | Australia | Irritable bowel syndrome | Case series FU: over 30 days |
Chiropractic | Resolution of symptoms | Mod |
| Elster,40 2009 | USA | Acid reflux and/or colic | Retrospective case series FU: over 2 weeks–6 months |
Chiropractic | Resolution of symptoms | Low |
| Marchand et al,41 2009 | UK | ‘Headache’ behaviours | Retrospective case series FU: none |
Chiropractic | Improvement of symptoms | Low |
| Miller and Benfield,43 2008 | UK | Colic | Retrospective case review FU: over a 2-year period |
Chiropractic | Adverse events | Mod |
| Miller and Miller,42 2009 | UK | Breastfeeding difficulties | Prospective case series FU: within a 2-week period |
Chiropractic | Improvement in feeding Number of treatments |
Mod |
| Stewart,44 2012 | Australia | Breastfeeding difficulties | Case review/before and after study FU: at end of treatment (duration, not reported) |
Chiropractic | Improvement feeding behaviour | Low |
| Wiberg and Wiberg,45 2010 | Denmark | Colic | Retrospective review of clinical records FU: 11 years |
Chiropractic | Crying time | Mod |
| Cornall,50 2015 | Australia | Breastfeeding difficulties | Qualitative study FU: none |
Osteopathy | Observation regarding ‘the osteopathic therapeutic cycle’ | High |
In the few cases where there was uncertainty with selection choice, these were all resolved after discussion with a third reviewer.
Quality assessment
The methodological quality of the studies varied (table 2). Five studies were rated as high quality: four RCTs (low risk of bias)32 34 35 38 and a qualitative study.50 Seven were of moderate quality.33 36 39 42 43 45 49 The remaining seven were rated as low quality due to severe methodological flaws (eg, small samples, the treating clinician observed and reported outcomes)37 39 41 44 46–48 (table 2). The non-RCT studies rated as low quality were excluded from further analyses.
Table 2.
Quality appraisal of studies
| RCTs* | Neu et al,35 2014 | Wiberg and Wiberg,45 1999 | Hayden and Mullinger,33 2006 | Miller et al,34 2012 | Olafsdottir et al,36 2001 | Browning and Miller,32 2008 | Herzaft-Le Roy et al,38 2017 |
| 1. Sequence generation | L | L | L | L | U | L | L |
| 2. Allocation concealment | L | U | U | L | L | U | L |
| 3. Blinding of parents | L | H | H | L | L | L | L |
| 4. Blinding of outcome assessors | L | L | H | L | L | L | L |
| 5. Incomplete outcome data | L | H | L | H | U | L | L |
| 6. Selective outcome reporting | L | U | L | L | U | L | H |
| Quality assessment | High | Low | Mod | High | Mod | High | High |
| Cohort studies† | Vallone, 48 2004 | Miller and Phillips, 47 2009 | Miller et al, 34 2012 | Miller et al, 49 2016 | |||
| 1. Clear focused issue? | Yes | Yes | No | Yes | |||
| 2. Cohort recruitment acceptable? | CD | Yes | CD | No | |||
| 3. Exposure accurately measured? | No | CD | No | CD | |||
| 4. Outcome accurately measured? | No | No | No | No | |||
| 5a. Confounders identified? | No | No | CD | Yes | |||
| 5b. Confounders considered appropriately? | No | No | No | Yes | |||
| 6a. Follow-up complete enough? | CD | No | CD | CD | |||
| 6b. Follow-up long enough? | CD | Yes | Yes | CD | |||
| 9. Results believable? | No | No | CD | Yes | |||
| 10. Results applicable? | No | No | CD | No | |||
| 11. Results consistent with others? | CD | NA | CD | Yes | |||
| Quality assessment | Low | Low | Low | Mod |
| Case series‡ | Elster, 40 2009 | Miller and Miller 42 2009 | Stewart, 44 2012 | Miller and Benfield, 43 2008 | Wiberg and Wiberg, 45 2010 | Davies and Jamison, 39 2007 | Marchand and Miller, 41 2009 |
| 1. Question clearly stated? | Yes | Yes | No | Yes | Yes | Yes | Yes |
| 2. Population clearly described? | No | Yes | No | Yes | Yes | Yes | CD |
| 3. Were cases consecutive? | CD | Yes | CD | Yes | Yes | Yes | CD |
| 4. Were subjects comparable? | CD | Yes | CD | Yes | Yes | Yes | CD |
| 5. Intervention clearly described? | No | No | No | No | No | Yes | No |
| 6. Outcomes consistent and appropriate across all participants? | No | No | No | No | No | No | No |
| 7. Follow-up adequate? | CD | CD | No | CD | No | CD | CD |
| 8. Statistics described and appropriate? | No | NA | Yes | Yes | CD | NA | NA |
| 9. Results clear? | No | Yes | No | Yes | No | No | No |
| Quality assessment | Low | Mod | Low | Mod | Mod | Mod | Low |
| Qualitative studies† | Cornall, 50 2015 | ||||||
| 1. Clear research question? | Yes | ||||||
| 2. Qual. method appropriate? | Yes | ||||||
| 3. Research design appropriate | Yes | ||||||
| 4. Recruitment strategy appropriate? | Yes | ||||||
| 5. Data collection appropriate? | Yes | ||||||
| 6. Relationship between researchers and participants considered? | Yes | ||||||
| 7. Ethics considered? | Yes | ||||||
| 8. Data analysis rigorous? | Yes | ||||||
| 9. Findings clear? | Yes | ||||||
| 10. Research valuable? | Yes | ||||||
| Quality assessment | High |
Green indicates a positive quality attribute; Amber indicates unclear quality; Red indicates low or negative quality.
*Cochrane Risk of Bias Tool.28
†Critical Appraisal Skills Programme checklist for cohort studies and qualitative studies.29
‡National Institutes of Health quality assessment tool for case series.30
CD, cannot determine; H, high risk of bias; L, low; NA, not applicable; RCTs, randomised controlled trials; U, Unclear.
Review findings
Table 3 shows the results from studies reporting similar outcomes. Six studies reported outcomes related to improvement in feeding,38 42 44 48–50 seven reported a reduction in crying time,32–34 36 37 45 46 five reported global improvement in symptoms,32 34 36 39 40 four reported sleep outcomes32 33 38 46 and three reported outcomes about parent–child relations.33 35 46 The remaining outcomes were from one study only.
Table 3.
Findings from included studies by similar outcomes
| Author, year (quality rating) | Participants, n and age | Outcomes and findings/results (parent-reported outcomes unless otherwise stated) | Magnitude or direction of effect: moderate to high-quality studies only |
| Reduction in crying: overall strength of evidence: moderate | |||
| Miller et al,34 2012* (high) |
n=104 Age: <8 weeks |
Mean crying times of all groups decreased by day 10, mean decrease was: treatment blinded (TB): 44.4% (P<0.001), treatment not blinded (TNB): 51.2% (P<0.001) and no treatment blinded (NTB): 18.6% (P<0.05). (1) TB versus NTB: using cut-off of 2 or less hours of crying per day and more than 30% change, respectively. Day 10: 12.0 (95% CI 2.1 to 68) and 3 (95% CI 0.8 to 9). (2) TB versus NTB: reduction −1.4 hours of mean crying time (95% CI −2.5 to −0.3) at day 10. (3) TB versus TNB: no significant difference between blinded treatment groups. Adjusted ORs: 0.7 (95% CI 0.2 to 2.0) and 0.5 (95% CI 0.1 to 1.6) at days 8 and 10, respectively. |
Significant favourable effect in the treatment group of 1.4 hours less crying |
| Browning and Miller,32 2008* (high) |
n=43 Age: <8 weeks |
At 4-week post-trial, there was complete resolution of colic symptoms (includes crying) in 18/22 infants in the spinal manual therapy (SMT) group and in 14/21 in the occipital decompression group (OSD) as perceived by the parent (rate ratio of 1.23 (95% CI 0.86 to 1.76)). Infants treated with SMT were 20% more likely to resolve compared with infants treated with OSD. Not statistically significant. | No difference between groups; both treatment groups improved. Head-to-head trial. |
| Hayden and Mullinger33 2006* (moderate) | n=28 Age: 10–83 days |
There was a statistically significant difference between the two groups in the mean reduction in crying time of 1.0 (95% CI 0.14 to 2.19) hours/24 hours. Overall reduction in crying time from weeks 1 to 4 was 63% in the treatment compared with 23% in the control group. |
Significant favourable effect in treatment group of 1 less hour of crying. |
| Olafsdottir et al,36 2001* (moderate) | n=100 Age: 3–9 weeks |
There was no difference between those treated and not treated (Student’s t-test, P=0.982). A reduction in crying hours per day in both groups was seen during the study, from a mean of 5.1 to 3.1 hours per day in the treatment group and from 5.4 to 3.1 hours in the control group. | No difference between groups; both treatment groups improved. |
| Wiberg and Wiberg,45 2010 (moderate) | n=276 Age: 0–3 months |
No apparent link between the clinical effect of chiropractic treatment and a natural decline in crying was found. | No clinical difference between treatment and natural decline. |
| Wiberg et al,37 1999* (low) | n=45 Age: mean 5.4 weeks |
There was a significantly larger reduction in colic symptoms from pretreatment to days 8–11 in the manipulation group (−1.0 hour/day, ±0.4 SE) compared with the dimethicone group (−2.7 hour/day, ±0.3 SE). | Inconclusive (low quality). |
| Sleeping time: overall strength of evidence: moderate | |||
| Herzhaft-Le Roy et al,38 2017* (high) | n=97 Age: mean 15 days |
16.5% of mothers in the osteopathic treatment group reported that their infants slept better, appeared soothed or better enjoyed lying on their back in the days that followed treatment. | Inconclusive: favourable outcome but only reported in the treatment group. |
| Browning and Miller,32 2008* (high) |
n=43 Age: <8 weeks |
At day 14, the mean hours of sleep per day were significantly increased in both groups (SMT, by 1.66 hours/day, P<0.01; OSD, by 1.03 hours day, P<0.01). | No difference between groups; both treatment groups improved. |
| Hayden and Mullinger,33 2006* (moderate) | n=28 Age: 10–83 days |
There was a significant difference between treated and control groups: mean increase in sleeping time of 1.17 hours/24 hours more (95% CI 0.29 to 2.27) (P<0.05). Overall improvement in sleeping time by week 4 was 11% for the treated group and less than 2% in the control group (mean % change). |
Significant favourable effect in treatment group of 1.17 hours of more sleeping. |
| Parent–child relations: overall strength of evidence: moderate | |||
| Neu et al,35 2014*(high) | n=43 Age: 4–12 weeks |
Effect size (ES) massage group relative to the non-massage group for sensitivity to cues, social-emotional growth fostering, cognitive growth and fostering (0.24 to 0.56: small to moderate. Not significant). Response to distress (ES −0.18) in unintended direction (not significant). |
Inconclusive: non-significant favourable effects in the treatment group. |
| Hayden and Mullinger,33 2006* (moderate) | n=28 Age: 10–83 days |
The mean difference in contact time between weeks 1 and 4 for the treated group was 1.3 hours (P<0.015) and 2 hours for the control group. | Significant favourable effects with less contact time required for the treated group compared with control. |
| Global improvement/resolution of symptoms: overall strength of evidence: moderate | |||
| Miller et al,34 2012*(high) | n=104 Age: <8 weeks |
Treatment group blinded versus non-blinded treatment group (adjusted OR (95% CI), 44.3 (7.7 to 253)). | Significant favourable effect in change with treatment. |
| Browning and Miller,32 2008* (high) | n=43 Age: <8 weeks |
At 4-week post-trial, there was complete resolution of colic symptoms in 18/22 infants in the SMT group and in 14/21 in the OSD group as perceived by the parent (rate ratio of 1.23 (95% CI 0.86 to 1.76). Infants treated with SMT were 20% more likely to resolve compared with infants treated with OSD. Not statistically significant. | No difference between groups; both treatment groups improved. |
| Davies and Jamison,39 2007 (moderate) | n=52 Age: median 7 weeks |
45 of 52 improved. One in four infants required only one adjustment (treating chiropractor reported data). |
Inconclusive: favourable descriptive statistics only. No control group. |
| Olafsdottir et al,36 2001*(moderate) | n=100 Age: 3–9 weeks |
69.9% of treatment groups versus 60% control showed some degree of improvement (Fisher’s exact test, P=0.374). | No difference between groups; both treatment groups improved. |
| Improvement in feeding: overall strength of evidence: low | |||
| Herzhaft-Le Roy et al,38 2017* (high) | n=97 Age: mean 15 days |
Ability to latch improved more in the treatment group (time 3, mean score=9.22, SD=0.92) than in the control group (time 3, mean score=8.18, SD=1.60); P=0.001. | Significant favourable effect in those having osteopathic treatment. |
| Miller et al,49 2016 (moderate) |
n=85. Age: <4 weeks |
7% (n=5) reported no difference in feeding after attending the clinic. 86% reported exclusive breastfeeding at follow-up (compared with the 26% at start of the study). Relative RR of exclusive breastfeeding after attending the clinic was 3.6 (95% CI 2.4 to 5.4). |
Significant favourable effect in those attending the clinic. |
| Miller et al,42 2009 (moderate) | n=114 Age: 2 days–12 weeks |
All showed improvement. 78% (n=89) were able to be exclusively breastfed after 2–5 treatments, within a 2-week time period. 20% (n=23) required at least some bottle-feeding. | Inconclusive descriptive statistics only. No control group. Favourable findings. |
| Cornall,50 2015 (high) | n=13 Mothers/osteopath dyads Age: mothers: median=32 years and newborns |
Findings support optimal breastfeeding through a progressive, transitional cycle process, which is supported by four interrelated categories: (1) connecting; (2) assimilating; (3) rebalancing; and (4) empowering. The findings outline contextual determinants that shaped women’s views and experiences, osteopaths’ professional identity and healthcare as a commodity. | Qualitative data affirming the need for a structured yet creative and individualised approach to infant manual therapy, with the goal of helping the mother to achieve optimal breastfeeding. |
| Maternal satisfaction: overall strength of evidence: low | |||
| Miller et al,49 2016 (moderate) | n=85. Age: <4 weeks. |
98% (n=83) planned to continue breastfeeding their baby and would recommend the clinic to friends. | Inconclusive: favourable descriptive statistics only. No control group. |
| Nipple pain: overall strength of evidence: low | |||
| Herzhaft-Le Roy et al,38 2017* (high) | n=97 Age: mean 15 days |
VAS mean scores over time (P=0.713). No statistical difference between groups. | No difference between groups. |
| Adverse events | |||
| Miller and Benfield,43 2008 (moderate) | n=697 Age: 75% <12 weeks |
7/697 of those attending treatment at clinic reported adverse reactions to treatment, 5 of these were treated for colic. Reactions reported were mild, transient and no medical care required. | Adverse events are minimal and transient. |
*Randomised controlled trials.
VAS, visual analogue scale.
Meta-analyses
A meta-analysis was only possible for the RCTs with outcomes measuring reduction in crying time and for adverse events.
Meta-analyses for global improvement in symptoms, parent–child relations, sleeping time and feeding were not possible because: several studies did not have a ‘no-treatment’ control group,32 39 40 42 44 48–50 did not present data at their primary endpoints,34 36 did not collect enough data or the data and outcomes were too heterogeneous.
Reduction in crying time
Seven studies reported data on crying time.32–34 36 37 45 46 There were sufficient data from four studies in the form of final value scores for the outcome of reduced crying time that could be meta-analysed for comparison of treatment effects. This replicated a previous meta-analysis.23 Our replicated meta-analysis (figure 2) gave a slightly different but still significant outcome for reduced crying time of −1.27 (95% CI −2.19 to −0.36) hours per day (figure 2). The difference is due to apportioned weighting given by the different versions of RevMan. One study37 used dimethicone as a comparison; the other studies’ controls were no treatment or placebo. We classified dimethicone as a placebo control (see figure 2). Parents were blinded to their child’s treatment in only two of the studies included in the meta-analysis.34 36
Figure 2.
Reduction in crying: RCTs mean difference. *Like Dobson et al,23 we were unable to determine the SD for the Olafsdottir et al 36 data. The Dobson review assigned the SD of change scores based on the correlation coefficient of other, similar studies, because personal correspondence was not successful with the author. We used the data from the Dobson et al review. **Miller34 is the same study labelled Miller46 in the Dobson review, which was a conference report in advance of the 2012 publication.
Adverse events
We were able to extract dichotomous data for adverse events and calculate RRs for meta-analysis (figure 3). Of the eight studies that reported presence or absence of adverse events,33 34 37–39 42 43 45 three studies reported there were no adverse events,38 42 45 two reported adverse events after manual therapy39 43 and three reported adverse events (worsening symptoms) in the control group.33 34 37
Figure 3.
Adverse events meta-analysis: RCTs relative risk. RCTs, randomised conrolled trials.
Using data from all the studies reporting adverse events, there were 1308 infants exposed to manual therapy and nine non-serious adverse events recorded, giving an incidence rate of seven non-serious events per 1000 infants. Conversely, there were 11 non-serious adverse events in the infants not exposed to manual therapy (n=97), giving an incidence rate of around 110 per 1000 infants.
Figure 3 shows the meta-analysis for the RCTs, which was possible for four studies.33 34 37 38 There was an overall RR of 0.12 (95% CI 0.12 to 0.66); that is, those who had manual therapy had an 88% reduced risk of having an adverse event compared with those who did not have manual therapy.
Discussion
In this systematic review, we searched for both RCT and non-RCT evidence. We found seven RCTs and 12 non-RCTs investigating the effects of manual therapy on healthy but unsettled, distressed and excessively crying infants treated in primary care.
Using Brontfort et al’s approach to overall evidence rating we found: moderate strength evidence for a small positive effective of manual therapy on reduction in crying time, inconclusive evidence for sleep and parent–child relations and no effects for global improvement (table 3).
Previous systematic reviews from 2012 and 201423 52 concluded there was favourable but inconclusive and weak evidence for manual therapy for infantile colic. Since 2014, two new RCTs have been published: one pilot study RCT (n=18)35 and one high-quality RCT (n=97)38 but neither presented new data on crying time for the meta-analysis. These two new RCTs blinded the parents to treatment, but they reported outcomes on feeding and global improvement and parent–child relations, respectively. This meant we were unable to update the meta-analyses conducted by Dobson et al.23
We considered all methodological study types narratively and looked at: direction of effect, quality of the study and results presented (table 3). However, because the low quality studies were so methodologically flawed, we did not include their results in the final analyses (this indicates a need for more scientific rigour in this field of research). We were still able to review the effects of manual therapy on multiple outcomes in 12 of our 19 selected studies. With the exception of reduced crying time, the findings were inconclusive, and the absence of effect shown for global improvements might suggest that the reduction in crying time of just over 1 hour was not sufficient enough to be meaningful for parents.
We anticipated that there would be more measurement of outcomes related to parent satisfaction and confidence or parent–child relations, but only five studies reported these outcomes.33 35 46 49 50 This paucity of information about the reciprocity of parent–infant psychosocial development indicates a gap in the literature considering the importance of the parent–infant dyad in positive bonding53 and the relationship between parent mood and psychosocial development of infants.54–57
Results in context with other research
The Cochrane review by Dobson et al 23 included two studies that we excluded because they were not peer reviewed: one a master’s thesis58 and one from conference proceedings.59 We repeated the Dobson et al sensitivity meta-analysis for peer-reviewed studies only, using their imputed SD for one study.36 The data extracted were the same, but the meta-analysis results were slightly different due the different versions of RevMan assigning different weights (we used RevMan V.5.3, while Dobson et al used RevMaN V.5.1). Both showed a significant reduction in the weighted mean difference of just over 1 hour in daily crying time (−1.01 hours (95% CI −1.78 to –0.24)23 vs −1.27 hours (95% CI −2.19 to –0.36)). As mentioned above, whether this reduction of around 1 hour of daily crying is meaningful to parents remains to be answered.
The I2 statistic in our meta-analysis and Dobson et al’s23 were 69% and 55%, respectively, indicating heterogeneity between the studies analysed. This was not unexpected due to the potential variation in treatments (and hence effects), loose diagnostic criteria and the power of the samples for the RCTs. Therefore, the results have to be considered with caution and are likely to change with further research. The meta-analysis helps illustrate and indicate that future research in this field requires well-powered studies, flexible but protocolised treatment and parental blinding.
Dobson et al 23 conducted a sensitivity meta-analysis to explore parent blinding to their infant’s treatment (Miller et al 34 and Olafsdottir et al 36), and interestingly, their results showed that there was no difference in crying time between groups with blinding.
Our searches also revealed 19 references to other systematic reviews of manual therapy paediatric care for conditions that were not the focus of our review, for example, otitis media, asthma, cerebral palsy and motor development. Our review draws similar conclusions to these other reviews; that is, more high-quality RCTs are needed, but methodological problems with research in this field might preclude researchers taking on this challenge. The gold standard to test effectiveness is the RCT, but double-blinding is not possible (one cannot blind the treating therapist) and some parents are reluctant to blinding and being separated from their child. Other issues particular to allied, complementary and alternative therapies include: loose definitions and diagnostic criteria, describing and/or protocolising interventions that are bespoke and determining the active elements of these multicomponent interventions. These problems are further compounded by the self-limiting nature of many childhood conditions.
These methodological issues may help explain the equivocal findings, small numbers recruited and low-quality assessments presented in systematic reviews.
Data about non-specific effects of treatment, such as the impact of care on parental confidence, and clinician reassurance were not found, possibly because these are difficult to assess as direct, indirect or independent of the study intervention. In one study we reviewed,36 all infants and parents received the same support, advice and non-manual therapy care. They found no difference in outcomes between the group who had manual therapy in addition, and both groups improved over time. The authors of this study suggested that the counselling, support and natural progression of the condition played a more powerful role than the manual therapy.
It remains unclear what the active components of a manual therapy consultation are, but we suggest that it would be valuable to understand why parents seek manual therapy care, despite the presence of other healthcare providers.
Safety
The safety data we extracted regarding adverse events indicated that manual therapy is a relatively low risk intervention, reflecting similar findings in other studies.24 The definitions of adverse events recorded in the studies reviewed ranged from ‘worsening symptoms’ to seeking other forms of care: a comprehensive prospective cohort study specifically focused on adverse events in children is necessary to draw better conclusions.
Strengths and limitations
This was a comprehensive and rigorously conducted review that included studies in all languages, including a growing number of articles published from China (titles and abstracts were in English for indexing). There was one Chinese paper that was selected for full paper review. We translated this article, but we were unable to fully interpret and understand the treatment given and the outcomes that related to Chinese Traditional Medicine energy points.51 In other words, the therapeutic paradigm presented was beyond our knowledge from a Western medicine perspective.
Inclusion criteria were specific to our population of interest, that is, thriving infants who were inexplicably unsettled, distressed and excessively crying who were treated in primary care. This symptom-based approach to selection permitted the inclusion of studies relating to various diagnoses, for example, breastfeeding, gastric and behavioural problems. However, this latitude could also be interpreted as a weakness, since definitions of unsettledness, distress and excessive crying and otherwise healthy were not always clear. Perhaps a more stringent, universally accepted definition of ‘colic’ is required. We may have failed to include some studies due to the authors’ descriptions of their populations.
Future research
Outcomes for parental satisfaction and confidence were under-researched, and we did not find much data about these. Collecting parent outcomes may provide more informative data about the active components of care.
A well-powered RCT with parental blinding, blinded assessment of reported outcomes, testing both non-specific and manual therapy effects of manual therapist care is needed to supplement research in this area.
Conclusions
We found moderate favourable evidence for the reduction in crying time in infants receiving manual therapy care (around 1 hour per day), but this may change with further research evidence. We still do not know if this result is meaningful to parents or if the reduction is due to the manual therapy component of care or other aspects of care. For other outcomes, the strength of evidence was low and inconclusive.
Supplementary Material
Footnotes
Contributors: DC conceptualised and designed the study, contributed to the data selection, extraction and analysis, drafted the initial manuscript, reviewed and revised the manuscript and approved the final manuscript submitted. CM managed the data, contributed to the data selection and extraction and did the meta-analyses, reviewed and revised drafts of the manuscript and approved the final manuscript submitted. AP and JE contributed to the data selection and extraction, reviewed and revised drafts of the manuscript and approved the final manuscript submitted. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: CM had financial support from the National Council for Osteopathic Research from crowd-funded donations.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Full datasets, analyses and all full searches are available on request from the corresponding author at d.carnes@qmul.ac.uk. No individual patient level data was used in this study.
References
- 1. Don N, McMahon C, Rossiter C. Effectiveness of an individualized multidisciplinary programme for managing unsettled infants. J Paediatr Child Health 2002;38:563–7. 10.1046/j.1440-1754.2002.00042.x [DOI] [PubMed] [Google Scholar]
- 2. Hiscock H, Jordan B. 1. Problem crying in infancy. Med J Aust 2004;181:507–12. [DOI] [PubMed] [Google Scholar]
- 3. Johnson JD, Cocker K, Chang E. Infantile Colic: Recognition and Treatment. Am Fam Physician 2015;92:577–82. [PubMed] [Google Scholar]
- 4. McCallum SM, Rowe HJ, Gurrin L, et al. Unsettled infant behaviour and health service use: a cross-sectional community survey in Melbourne, Australia. J Paediatr Child Health 2011;47:818–23. 10.1111/j.1440-1754.2011.02032.x [DOI] [PubMed] [Google Scholar]
- 5. Morris S, James-Roberts IS, Sleep J, et al. Economic evaluation of strategies for managing crying and sleeping problems. Arch Dis Child 2001;84:15–19. 10.1136/adc.84.1.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vik T, Grote V, Escribano J, et al. Infantile colic, prolonged crying and maternal postnatal depression. Acta Paediatr 2009;98:1344–8. 10.1111/j.1651-2227.2009.01317.x [DOI] [PubMed] [Google Scholar]
- 7. Overpeck MD, Brenner RA, Trumble AC, et al. Risk factors for infant homicide in the United States. N Engl J Med 1998;339:1211–6. 10.1056/NEJM199810223391706 [DOI] [PubMed] [Google Scholar]
- 8. Hall B, Chesters J, Robinson A. Infantile colic: a systematic review of medical and conventional therapies. J Paediatr Child Health 2012;48:128–37. 10.1111/j.1440-1754.2011.02061.x [DOI] [PubMed] [Google Scholar]
- 9. Miller J, Weber S. Is infant colic an allergic reaction to cow’s milk: What is the evidence? J. Clin Chiro.Pediatr 2013;14:1097–102. [Google Scholar]
- 10. Sung V, CollettS deGT, et al. Probiotics to prevent or treat excessive infant crying: systematic review and meta-analysis. JAMA 2013;167:1150–7. [DOI] [PubMed] [Google Scholar]
- 11. Sung V, Hiscock H, Tang ML, et al. Treating infant colic with the probiotic Lactobacillus reuteri: double blind, placebo controlled randomised trial. BMJ 2014;348:g2107 10.1136/bmj.g2107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ernst E. Chiropractic spinal manipulation for infant colic: a systematic review of randomised clinical trials. Int J Clin Pract 2009;63:1351–3. 10.1111/j.1742-1241.2009.02133.x [DOI] [PubMed] [Google Scholar]
- 13. Langkau J, Miller J. An investigation of musculoskeletal dysfunction in infants includes a case series of KISS diagnosed children. J. Clin Chiro.Pediatr 2012;13:958–67. [Google Scholar]
- 14. Rao MR, Brenner RA, Schisterman EF, et al. Long term cognitive development in children with prolonged crying. Arch Dis Child 2004;89:989–92. 10.1136/adc.2003.039198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. St James-Roberts I, Peachey E. Distinguishing infant prolonged crying from sleep-waking problems. Arch Dis Child 2011;96:340–4. 10.1136/adc.2010.200204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wolke D, Bilgin A, Samara M. Systematic review and meta-analyses: fussing and crying durations and prevalence of colic in infants. J Pediatr 2017;185:55–61. 10.1016/j.jpeds.2017.02.020 [DOI] [PubMed] [Google Scholar]
- 17. Barr RG. Changing our understanding of infat Colic. Arch Pediatr Adolesc Med 2002;156:1172–4. 10.1001/archpedi.156.12.1172 [DOI] [PubMed] [Google Scholar]
- 18. Douglas PS, Hiscock H. The unsettled baby: crying out for an integrated multidisciplinary primary care approach. [DOI] [PubMed] [Google Scholar]
- 19. Talachian E, Bidari A, Rezaie MH. Incidence and risk factors for infantile colic in Iranian infants. World J Gastroenterol 2008;14:4662–6. 10.3748/wjg.14.4662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kurth E, Spichiger E, Cignacco E, et al. Predictors of crying problems in the early postpartum period. J Obstet Gynecol Neonatal Nurs 2010;39:250–62. 10.1111/j.1552-6909.2010.01141.x [DOI] [PubMed] [Google Scholar]
- 21. Dihigo SK. New strategies for the treatment of colic: modifying the parent/infant interaction. J Pediatr Health Care 1998;12:256–62. 10.1016/S0891-5245(98)90206-1 [DOI] [PubMed] [Google Scholar]
- 22. Wolke D, Gray P, Meyer R. Excessive infant crying: a controlled study of mothers helping mothers. Pediatrics 1994;94:322–32. [PubMed] [Google Scholar]
- 23. Dobson D, Lucassen PL, Miller JJ, et al. Manipulative therapies for infantile colic. Cochrane Database Syst Rev 2012;12:CD004796 10.1002/14651858.CD004796.pub2 [DOI] [PubMed] [Google Scholar]
- 24. Todd AJ, Carroll MT, Robinson A, et al. Adverse Events Due to Chiropractic and Other Manual Therapies for Infants and Children: A Review of the Literature. J Manipulative Physiol Ther 2015;38:699–712. 10.1016/j.jmpt.2014.09.008 [DOI] [PubMed] [Google Scholar]
- 25. Wessel MA, Cobb JC, Jackson EB, et al. Paroxysmal fussing in infancy, sometimes called colic. Pediatrics 1954;14:421–35. [PubMed] [Google Scholar]
- 26. Hyman PE, Milla PJ, Benninga MA, et al. Childhood functional gastrointestinal disorders: neonate/toddler. Gastroenterology 2006;130:1519–26. 10.1053/j.gastro.2005.11.065 [DOI] [PubMed] [Google Scholar]
- 27. Software. Melbourne, Australia: Csr: Veritas Health Innovation; http://www.covidence.org [Google Scholar]
- 28. Higgins J, Green S, Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]: The Cochrane Collaboration, 2011. http://www.handbook.cochrane.org [Google Scholar]
- 29. CASP: Critical Appraisal Skills Programme (CASP) 2014. CASP Checklists (URL used). Oxford: CASP, 2014. [Google Scholar]
- 30. National Institutes of Health (NIH). Quality Assessment Tool for Case Series Studies. 2014. https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/case_series
- 31. Bronfort G, Haas M, Evans R, et al. Effectiveness of manual therapies: the UK evidence report. Chiropr Osteopat 2010;18:3 10.1186/1746-1340-18-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Browning M, Miller J. Comparison of the short-term effects of chiropractic spinal manipulation and occipito-sacral decompression in the treatment of infant colic: a single-blinded, randomised, comparison trial. Clinical Chiropractic 2008;11:122–9. 10.1016/j.clch.2008.10.003 [DOI] [Google Scholar]
- 33. Hayden C, Mullinger B. A preliminary assessment of the impact of cranial osteopathy for the relief of infantile colic. Complement Ther Clin Pract 2006;12:83–90. 10.1016/j.ctcp.2005.12.005 [DOI] [PubMed] [Google Scholar]
- 34. Miller JE, Newell D, Bolton JE. Efficacy of chiropractic manual therapy on infant colic: a pragmatic single-blind, randomized controlled trial. J Manipulative Physiol Ther 2012;35:600–7. 10.1016/j.jmpt.2012.09.010 [DOI] [PubMed] [Google Scholar]
- 35. Neu M, Schmiege SJ, Pan Z, et al. Interactions during feeding with mothers and their infants with symptoms of gastroesophageal reflux. J Altern Complement Med 2014;20:493–9. 10.1089/acm.2013.0223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Olafsdottir E, Forshei S, Fluge G, et al. Randomised controlled trial of infantile colic treated with chiropractic spinal manipulation. Arch Dis Child 2001;84:138–41. 10.1136/adc.84.2.138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wiberg JM, Nordsteen J, Nilsson N. The short-term effect of spinal manipulation in the treatment of infantile colic: a randomized controlled clinical trial with a blinded observer. J Manipulative Physiol Ther 1999;22:517–22. 10.1016/S0161-4754(99)70003-5 [DOI] [PubMed] [Google Scholar]
- 38. Herzhaft-Le Roy J, Xhignesse M, Gaboury I. Efficacy of an Osteopathic Treatment Coupled With Lactation Consultations for Infants' Biomechanical Sucking Difficulties. J Hum Lact 2017;33:165–72. 10.1177/0890334416679620 [DOI] [PubMed] [Google Scholar]
- 39. Davies NJ, Jamison JR. Chiropractic management of irritable baby syndrome. Chiropr J Aust 2007;37:25–9. [Google Scholar]
- 40. Elster E. Sixteen infants with acid reflux and colic undergoing upper cervical chiropractic care to correct vertebral subluxation: A retrospective analysis of outcome. J Pediatr Matern & Fam Health - Chiropr 2009. [Google Scholar]
- 41. Marchand AM, Miller JE, Mitchell C. Diagnosis and chiropractic treatment of infant headache based on behavioral presentation and physical findings: a retrospective series of 13 cases. J Manipulative Physiol Ther 2009;32:682–6. 10.1016/j.jmpt.2009.08.026 [DOI] [PubMed] [Google Scholar]
- 42. Miller JE, Miller L, Sulesund AK, et al. Contribution of chiropractic therapy to resolving suboptimal breastfeeding: a case series of 114 infants. J Manipulative Physiol Ther 2009;32:670–4. 10.1016/j.jmpt.2009.08.023 [DOI] [PubMed] [Google Scholar]
- 43. Miller JE, Benfield K. Adverse effects of spinal manipulative therapy in children younger than 3 years: a retrospective study in a chiropractic teaching clinic. J Manipulative Physiol Ther 2008;31:419–23. 10.1016/j.jmpt.2008.06.002 [DOI] [PubMed] [Google Scholar]
- 44. Stewart A. Paediatric chiropractic and infant breastfeeding difficulties: A pilot case series study involving 19 cases. Chiropr J Aust 2012;42:98–107. [Google Scholar]
- 45. Wiberg KR, Wiberg JM. A retrospective study of chiropractic treatment of 276 danish infants with infantile colic. J Manipulative Physiol Ther 2010;33:536–41. 10.1016/j.jmpt.2010.08.004 [DOI] [PubMed] [Google Scholar]
- 46. Miller J, Newell D. Prognostic significance of subgroup classification for infant patients with crying disorders: A prospective cohort study. J Can Chiropr Assoc 2012;56:40-8. [PMC free article] [PubMed] [Google Scholar]
- 47. Miller JE, Phillips HL. Long-term effects of infant colic: a survey comparison of chiropractic treatment and nontreatment groups. J Manipulative Physiol Ther 2009;32:635–8. 10.1016/j.jmpt.2009.08.017 [DOI] [PubMed] [Google Scholar]
- 48. Vallone S. Chiropractic Evaluation and Treatment of Muskuloskeletal Dysfunction in Infants Demonstrating. J Clin Chiro Pediatrics 2004;6:349–68. [Google Scholar]
- 49. Miller J, Beharie MC, Taylor AM, et al. Parent Reports of Exclusive Breastfeeding After Attending a Combined Midwifery and Chiropractic Feeding Clinic in the United Kingdom: A Cross-Sectional Service Evaluation. J Evid Based Complementary Altern Med 2016;21:85–91. 10.1177/2156587215625399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Cornall D. Promoting optimal breastfeeding through the osteopathic therapeutic cycle. Australia: Victoria University, 2015. [Google Scholar]
- 51. Wq H. Clinical observation on manipulation without syndrome differentiation in treating infantile diarrhea]. Zhong Xi Yi Jie He Xue Bao/Chin J Integr Med 2004;2:220–1. [DOI] [PubMed] [Google Scholar]
- 52. Clar C, Tsertsvadze A, Court R, et al. Clinical effectiveness of manual therapy for the management of musculoskeletal and non-musculoskeletal conditions: systematic review and update of UK evidence report. Chiropr Man Therap 2014;22:12 10.1186/2045-709X-22-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Costa R, Figueiredo B. Infant’s psychophysiological profile and temperament at 3 and 12 months. Infant Behav Dev 2011;34:270–9. 10.1016/j.infbeh.2011.01.002 [DOI] [PubMed] [Google Scholar]
- 54. Barr RG. Colic and crying syndromes in infants. Pediatrics 1998;102:1282–6. [PubMed] [Google Scholar]
- 55. Canivet CA, Ostergren PO, Rosén AS, et al. Infantile colic and the role of trait anxiety during pregnancy in relation to psychosocial and socioeconomic factors. Scand J Public Health 2005;33:26–34. 10.1080/14034940410028316 [DOI] [PubMed] [Google Scholar]
- 56. Rautava P, Helenius H, Lehtonen L. Psychosocial predisposing factors for infantile colic. BMJ 1993;307:600–4. 10.1136/bmj.307.6904.600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Reijneveld SA, Brugman E, Hirasing RA. Excessive infant crying: the impact of varying definitions. Pediatrics 2001;108:893–7. 10.1542/peds.108.4.893 [DOI] [PubMed] [Google Scholar]
- 58. Heber A, Senger U, [DIE OSTEOPATHISCHE BEHANDLUNGBEI3– MONATSKOLIK IM VERGLEICHZURKONVENTIONELLENTHERAPIE]. Osteopathic Treatment Of Infantile Colic Masters thesis. Germany: Akademie für Osteopathie (AFO), 2003. [Google Scholar]
- 59. Mercer C. A study to determine the efficacy of chiropractic spinal adjustments as a treatment protocol in the management of infantile colic. Durban, SA: Technikon Natal, Durban University, 1999. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-019040supp001.pdf (271.1KB, pdf)