Abstract
Objectives:
Traditionally, healing after surgical endodontic retreatment (SER); i.e. apicectomy with or without a retrograde filling, is assessed in periapical radiographs (PR). Recently, the use of cone beam CT (CBCT) has increased within endodontics. Generally, CBCT detects more periapical lesions than PR, but basic research on the true nature of these lesions is missing.
The objective was to assess the diagnostic validity of PR and CBCT for determining inflammation in SER cases that were re-operated (SER-R) due to unsuccessful healing, using histology of the periapical lesion as reference for inflammation.
Methods:
Records from 149 patients, receiving SER 2004-10, were screened. In total 108 patients (119 teeth) were recalled for clinical follow-up examination, PR and CBCT, of which 74 patients (83 teeth) participated. Three observers assessed PR and CBCT as “successful healing” or “unsuccessful healing” using Rud and Molven’s criteria. SER-R was offered to all non-healed teeth with expected favourable prognosis for subsequent functional retention. During SER-R, biopsy was performed and histopathology verified whether or not inflammation was present.
Results:
All re-operated cases were assessed non-healed in CBCT while 11 of these were assessed successfully healed in PR. Nineteen biopsies were examined. Histopathologic diagnosis revealed 42% (teeth = 8) without periapical inflammation, 16% (teeth = 3) with mild inflammation and 42% (teeth = 8) with moderate to intense inflammation. A correct diagnosis was obtained in 58% with CBCT (true positives) and 63% with PR (true positives+true negatives).
Conclusions:
Of the re-operated teeth, 42% had no periapical inflammatory lesion, and hence no benefit from SER-R. Not all lesions observed in CBCT represented periapical inflammatory lesions.
Keywords: surgical endodontic retreatment, apicectomy, CBCT, periapical lesion, histopatholology
Introduction
Root canal treatment is performed to prevent or treat apic al periodontitis.1 In case a periapical inflammatory lesion develops after, or does not respond to, root canal treatment, the primary treatment can be considered unsuccessful and a retreatment may be relevant. Retreatment can be performed using either an orthograde approach; non-surgical endodontic retreatment, or a surgical approach; surgical endodontic retreatment (SER), i.e. apicectomy with or without a retrograde filling.
Traditionally, healing after SER is assessed in periapical radiographic images (PR). Since Rud et al2 and Molven et al3 introduced criteria for evaluat on of treatment outcome after SER, these criteria have been widely accepted and used in several follow-up studies.4
During recent years, the use of cone beam CT (CBCT) has increased for endodontic diagnostic tasks, including follow-up of SER.5 In general, more periapical lesions are detected in CBCT,4 also after SER,6 but basic research on the true nature (inflammation/no inflammation) of these radiographic lesions is still scarce. A recent human ex-vivo study has used histopathology to assess periapical inflammation in lesions found by CBCT. The authors demonstrated an almost complete agreement between CBCT and histopathologic diagnosis. However, this study did not include root-canal treated teeth.7 Other studies have pertained to differentiate between apical periodontitis and radicular cysts using CBCT with histology as a reference standard, and found that it was not possible to discriminate between the two entities in CBCT.8,9
The aim of the present study was to assess the diagnostic validity of PR and CBCT in SER cases that were re-operated (SER-R) due to persistent periapical lesion, using histopathology as reference for presence and degree of inflammation.
Methods and Materials
Patients
The present study was a follow-up study of teeth previously treated by SER at Department of Dentistry, Aarhus University, Denmark. Treatments performed within the period from January 2004 to December 2010 were included in the study, and patients were invited to a follow-up examination during the period from March 2012 to September 2016. The average follow-up period was 7 years (range 5–11 years).
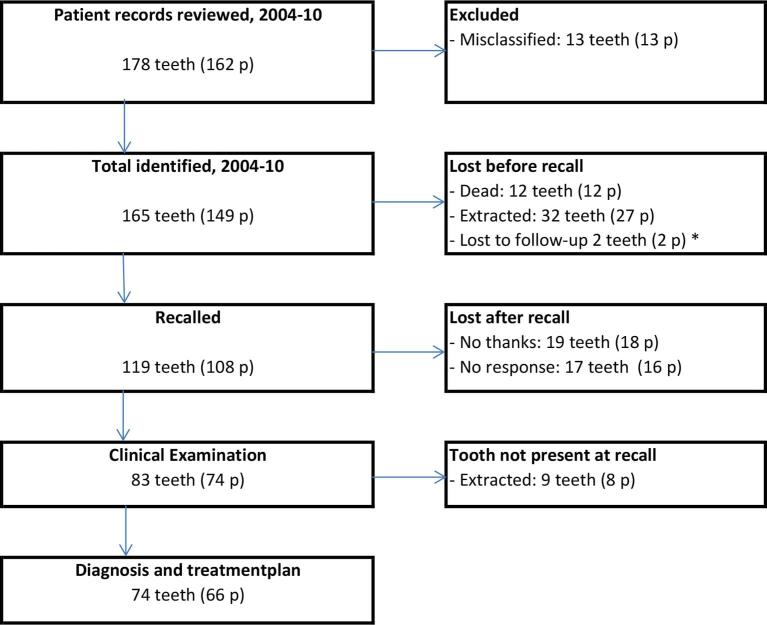
In the patient file archive, 162 patients (178 teeth) were identified, who initially met the inclusion criterion that a SER had been performed. After reading the complete patient files, one observer (CK) excluded 41 patients (46 teeth) for various reasons (treatment misclassification in the patient file system, death, extraction of the tooth of interest, or lost to follow-up). The remaining 108 patients (119 teeth) were invited to participate in a clinical and radiological follow-up examination including both a digital periapical image and a CBCT examination of the previously SER-treated area. In total, 74 patients (83 teeth) accepted the invitation and were clinically and radiographically examined. A flow-diagram of inclusion and exclusion of participants can be seen in Figure 1.
Figure 1.
Flow-diagram of teeth and participants. *One re-operation, one drop-out. p, number of persons; SER, surgical endodontic retreatment; PR, Periapical radiographic image; CBCT, cone beam CT.
The study protocol was approved by the regional Committee of Ethics (1-10-72-280-14) and the study conducted in accordance with the World Medical Association Declaration of Helsinki.
Clinical examination
The clinical examination was performed by one experienced examiner (CK). The clinical examination for the tooth in question included: soft tissue swelling, pain, tenderness on chewing or percussion, fistula, periodontal status, tooth mobility, and type and quality of coronal restoration.
Radiographic examination
Periapical radiographs were obtained using a “Gendex 1000 DC” X-ray unit (Gendex Corporation, Milwaukee, WI), paralleling technique, 65 kV, 10 mA, and a film-focus distance of 28 cm. The exposure time was adjusted to the individual patient and region. A photostimulable storage phosphor plate system was used with a spatial resolution of 755 × 1025 pixels (Dürr Dental VistaScan Plus, Dürr Dental AG, Bietigheim-Bissingen, Germany). CBCT examination was performed with Scanora® 3D (Soredex Oy, Tuusula, Finland) using a 6 × 6 cm field of view, resolution 0.133 mm, exposure parameters set at 90 kV, 10 mA and an exposure time of 23 s.
Observers and radiographic classification
All PR images and CBCT volumes were viewed in a quiet room with subdued lighting using two 24-inch flat screen monitors, Dell P2412H (Dell Inc., Round Rock, TX); one monitor to display the baseline PR (the immediate post-operative periapical image taken after the initial SER) and the other monitor for the 7-year follow-up PR or CBCT. Dedicated PACS software (DigiView, developed by programmer Erik Gotfredsen, Section of Oral Radiology, Aarhus University, Aarhus, Denmark) was used to display the periapical radiographs, and the observers were able to enhance viewing parameters (e.g., brightness and contrast). Software for viewing 3D image volumes (OnDemand, Cybermed Inc., Daejeon, South Korea) was used for a dynamic evaluation of the CBCT volumes, and the observers could freely change all visualization parameters and perform individual sectioning.
First the baseline PR and the 7-year follow-up PR were compared, and subsequently the baseline PR and the CBCT sections. The periapical area of the tooth in question was scored separately by each method using the criteria for healing proposed by Rud et al2 and Molven et al3 as(1) complete healing; (2) incomplete healing; (3) uncertain healing and (4) unsatisfactory healing. Written scoring criteria and “atlas drawings” by Molven et al3 were available. If the tooth of interest had been extracted, this was scored as a separate category “EX”. Three experienced observers (two endodontists (CK, LLK) and one oral radiologist (RSN)) evaluated all radiographic images and CBCT volumes.
For both radiographic modalities, the periapical scores were registered by each observer, and a consensus was reached by selecting the most frequent score. In case of disagreement (three different scores), the three observers discussed the case until consensus was reached. The consensus Rud & Molven classification was dichotomized into “successful healing” (scores 1 and 2) and “unsuccessful healing” (scores 3 and 4).3
If the tooth was assessed as unsuccessfully healed in PR and/or CBCT, all the available information on the patient was evaluated, including data from the clinical examination, before it was decided if the patient should be offered a re-operation (SER-R) or not. Only teeth with a reasonable prognosis for functional retention, including sufficient periodontal support and tooth substance to allow favourable prosthetic restorability after the new surgical procedure, were offered SER-R.
SER-R procedure
All patients accepting SER-R were re-operated by one endodontist (CK). Under local anesthesia a mucoperiostal flap was raised. Bone removal over the lesion was performed with a round bur to expose the periapical lesion. The soft tissue of the periapical lesion was carefully removed in toto by surgical spoons and immediately fixed in neutral buffered 10% formalin (pH 7.2, 20°C) for histopathological examination. The resection surface was smoothened using a fissure bur and the retrograde preparation made with retro-tips in an ultrasonic hand piece (Satelec Newtron P5, Satelec Acteon, Merignac, France). After hemostasis was obtained, the retro-preparation was cleaned using 3% H2O2, dried by paper points, and filled with Mineral Trioxide Aggregate (ProRoot MTA White, Dentsply Tulsa Dental, Tulsa, OK). In one case, in which ultrasonic preparation was impossible due to a long cast metal post, the resection surface was shallowed lightly with a round diamond bur and Retroplast (Retroplast Trading, Rørvig, Denmark) used as retrograde filling material. The surgical area was thoroughly cleaned with sterile saline and the soft tissue closed using 5–0 sutures (Vicryl, Ethicon, Somerville, NJ). Sutures were removed after 7–10 days.
Histopathological examination of the removed soft tissue
The formalin-fixed tissues were dehydrated in graded alcohols and embedded in paraffin. Sections of 3–4 µm were cut using a microtome (Leica GmbH, Nussloch Eisfeld, Nussloch, Germany) and stained with haematoxylin and eosin for routine histopathological examination under light microscopy. One oral pathologist (JR) assessed all biopsies and made standard histopathological examinations and reports. At a separate setting, all biopsies were reviewed by the same oral pathologist in order to classify them as having either no inflammation (scar-like fibrous tissue and/or normal appearing bone fragments), mild inflammation (fibrous tissue with slight infiltration with lymphocytes), or moderate to intense inflammation (fibrous tissue with moderate to heavy infiltrate with lymphocytes/plasma cells and/or granulation tissue).
Data management and analyses
Data was presented as counts and percentages with the tooth as the unit of analysis.
Results
Nine teeth (in 8 patients) had been extracted at the follow-up examination and hence, 66 patients with 74 teeth were included in the study analysis (Figure 1). The mean age of the 74 patients was 66 years (range 39–90) for males and 61 years (range 31–82) for females. The mean follow-up period for these 74 patients was 7 years and 4 months (range 5 years and 3 months–11 years and 4 months).
In five cases (two PR, three CBCT) of disagreement (three different scores) the consensus score was sealed by discussion between the three observers.
Table 1 shows the dichotomized consensus Rud & Molven categories for scores in PR and CBCT. In 54 cases (73%) there was an agreement in the scores in PR and CBCT, whereas there was a disagreement in 20 cases (27%). In 19 out of these 20 cases, the healing was scored unsuccessful in CBCT and successful in PR. Only one case was assessed unsuccessful in PR, but successful in CBCT.
Table 1.
Dichotomized Rud & Molven categories (consensus observer) for scores in PR and CBCT
| CBCT assessment | |||
|---|---|---|---|
| PR assessment | Successful | Unsuccessful | Total |
| Successful | 41 | 19 | 60 |
| Unsuccessful | 1 | 13 | 14 |
| Total | 42 | 32 | 74 |
PR, periapical radiograph; CBCT, cone beam CT.
Successful = Rud & Molven score 1 + 2; Unsuccessful = Rud & Molven score 3 + 4.
In total 33 teeth (in 33 patients) displayed a periapical lesion at the 7-year follow-up after SER, interpreted as pathology with at least one of the radiographic modalities. Of these, 23 teeth (in 23 patients) were assessed to fulfil the clinical inclusion criteria for SER-R. Ten patients were not offered SER-R despite a radiographic diagnosis of unsuccessful healing. The reasons for excluding these cases from SER-R are listed in Table 2.
Table 2.
Cases with a radiographic diagnosis of unsuccessful periapical healing
| SER-R offered | |
| Patient accepted | 20a |
| Patient refused | 3 |
| Total | 23 |
| SER-R not offered due to unfavourable prognosis | |
| Advanced marginal periodontitis | 5 |
| Short root | 1 |
| Vertical root fracture | 1 |
| Tooth not prosthetically restorable | 3 |
| Total | 33 |
One specimen lost during processing to the oral pathologist.
SER-R, surgical endodontic retreatment Re-operation.
Twenty patients accepted the offer of SER-R (three refused re-operation), and the full volume of periapical soft tissue was removed and saved in all 20 teeth. During processing, one specimen was lost, leaving 19 patients (6 males, 13 females) with 19 teeth (15 maxillary, 4 mandibular) to be included in the histological analysis.
The mean age of the 19 patients was 62 years (range 39–72) for males and 56 years (range 31–75) for females. The mean follow-up period for these 19 patients was 7 years and 10 months (range 5 years and 3 months–10 years and 9 months). The mean time span from follow-up CBCT to SER-R was 35 days (range 0–83).
Table 3 shows the relation between the radiographic and histopathological classifications. The histopathological examination resulted in 42% (8 teeth) with no inflammation, 16% (3 teeth) with mild inflammation, and 42% (8 teeth) with intense inflammation. Figures 2–4shows examples of PR, CBCT and histology of SER-R cases.
Table 3.
Dichotomized Rud & Molven categories (consensus observer) for scores in periapical images and CBCT vs histopathological diagnosis of SER-R teeth
| Radiographic diagnosis | |||
|---|---|---|---|
| Histopathologic diagnosis | PR successful or CBCT unsuccessful |
PR unsuccessful or CBCT unsuccessful |
Total |
| No signs of inflammation | 6 | 2 | 8 |
| Mild inflammation | 2 | 1 | 3 |
| Intense inflammation | 3 | 5 | 8 |
| Total | 11 | 8 | 19 |
PR, periapical radiograph; CBCT, cone beam CT.
Successful = Rud & Molven score 1 + 2; Unsuccessful = Rud & Molven score 3 + 4.
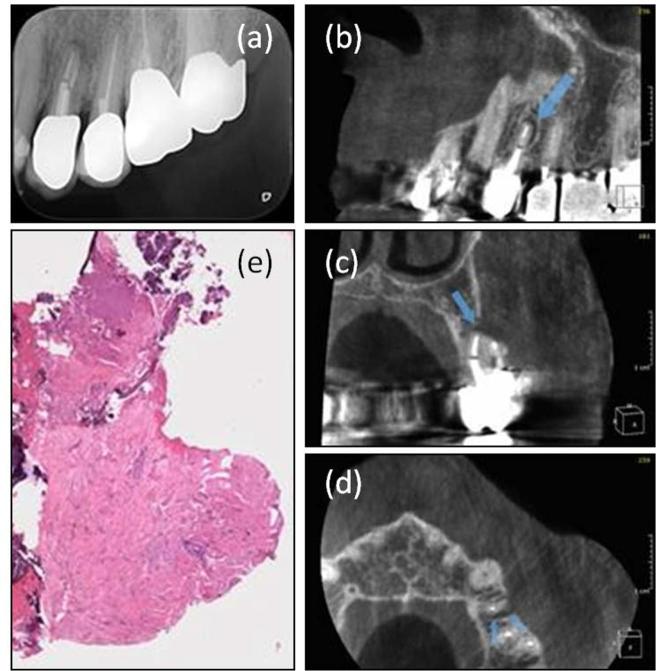
Figure 2.
Examples of included cases with periapical radiographic image, CBCT sections and histopathology. Case 1 Tooth 24, 10-year follow-up, no inflammation. (a) PR showing unsuccessful healing. (b) CBCT, sagittal section showing unsuccessful healing, blue arrow points at periapical radiolucency. (c) CBCT, coronal section showing unsuccessful healing, blue arrow points at periapical radiolucency. (d) CBCT, horizontal section showing unsuccessful healing, blue arrows point at periapical radiolucency. (e) Biopsy of periapical lesion (H&E), fibrous/scar tissue with no inflammation.
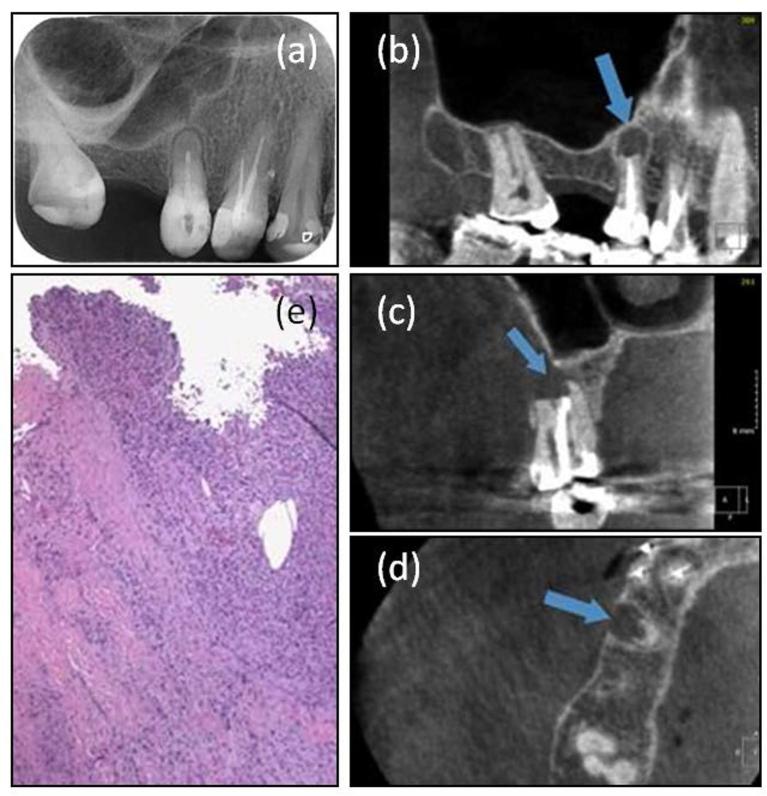
Figure 4.
Examples of included cases with periapical radiographic image, CBCT sections and histopathology. Case 3 Tooth 15, 7-year follow-up, granulation tissue, intense inflammation. (a) PR showing unsuccessful healing. (b) CBCT, sagittal section showing unsuccessful healing, blue arrow points at periapical radiolucency. (c) CBCT, coronal section showing unsuccessful healing, blue arrow points at periapical radiolucency. (d) CBCT, horizontal section showing unsuccessful healing, blue arrow points at periapical radiolucency. (e) Biopsy of periapical lesion (H&E), granulation tissue/fibrous tissue with intense inflammation.
Figure 3.
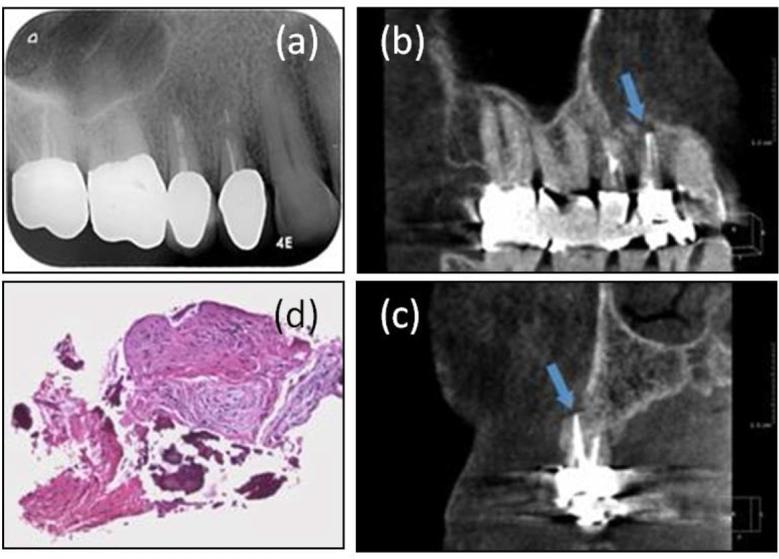
Examples of included cases with periapical radiographic image, CBCT sections and histopathology. Case 2 Tooth 14, 7-year follow -up, mild inflammation. (a) PR showing successful healing. (b) CBCT, sagittal section showing unsuccessful healing, blue arrow points at periapical radiolucency. (c) CBCT, coronal section showing unsuccessful healing, blue arrow points at periapical radiolucency. (d) Biopsy of periapical lesion (H&E), fibrous tissue with mild inflammation.
With CBCT, a correct diagnosis (true positives) was obtained in 58% of all cases while with PR a correct diagnosis (true positives + true negatives) was obtained in 63%. As none of the SER-R cases were assessed successful in CBCT, no true or false negative findings could be calculated for this method. With PR, 26% (5 teeth) of all cases were false negatives. With CBCT 42% (8 teeth) of the scorings were false positives with no inflammation in the area according to the histopathological examination, whereas in PR fewer of the scorings were false positives (11%, 2 teeth).
Table 4 shows the relation between CBCT Rud & Molven score and histopathologic diagnosis of the SER-R teeth. When assessed as score 3 (uncertain healing) in CBCT, 6 out of 8 cases (75%) did not show any signs of inflammation, and when assessed as score 4 (unsatisfactory healing) in CBCT, 9 out of 11 (82%) cases showed signs of mild or intense inflammation at histopathological examination.
Table 4.
Rud & Molven score in CBCT vs histopathological diagnosis of SER-R teeth
| CBCT diagnosis | |||
|---|---|---|---|
| Histopathological diagnosis | Rud & Molven 3 | Rud & Molven 4 | Total |
| No signs of inflammation | 6 | 2 | 8 |
| Mild inflammation | 1 | 2 | 3 |
| Intense inflammation | 1 | 7 | 8 |
| Total | 8 | 11 | 19 |
CBCT, cone beam CT.
All SER-R patients with self-reported pain and sensitivity to percussion (n = 4) had a Rud & Molven score 4 in the CBCT, and all were classified as having intense inflammation in the biopsied periapical lesion.
Discussion
The present study is, to the knowledge of the authors, the first study to identify the true nature of the periapical tissue in SER cases assessed as unsuccessful based on clinical examination, PR and CBCT.
In classical studies of diagnostic accuracy, both successful and unsuccessful cases have to be compared to a reference standard. In the present study, for obvious ethical reasons, only cases diagnosed with apical periodontitis by radiography were offered SER-R. This allowed assessment of sensitivity (proportion of true positives out of all histopathologically positives). Possible periapical areas that appeared as successfully healed in PR and CBCT, but which were actually inflamed, were not included in this study and therefore it was not possible to assess specificity (proportion of true negatives out of all histopathologically negatives). Hence, the present study has to be classified as a study of clinical diagnostic validity. The present study is at Fryback and Thornbury10 level 4, describing the “therapeutic efficacy”. All cases assessed as unsuccessfully healed in either PR or CBCT were evaluated for SER-R.
The time period from CBCT acquisition to the surgical procedure (SER-R) was on average 35 days. This is a relatively short period of time compared to the follow-up period from 5 to 11 years, and it was regarded acceptable. All the cases had a diagnosis of chronic periapical periodontitis, and few, if any, changes in the inflammatory process were expected in the time span between CBCT and SER-R.
Literature agrees that overall, more periapical lesions are detected by CBCT compared to periapical images, however, most of the studies are in vitro or animal studies.4 Few studies have pertained to identify the true nature of these lesions. In an animal study investigating induced periapical lesions in dogs, a high agreement between CBCT and histology was reported.11 Previous studies in humans, using histology as the reference standard, have demonstrated that CBCT could not be used to discriminate between soft tissue structures like apical periodontitis and cysts.8,9 In a recent human ex vivo study, jaws with teeth were CBCT scanned and the periapical diagnosis verified by histopathology.7 An almost complete agreement between CBCT and histologic diagnosis was reported, however, the sample did not include any root-filled teeth, and more than 85% of the included teeth had apical periodontitis.
Periapical disease is often underestimated in PR when compared to a histopathological reference standard.12 It has been demonstrated that if a periapical lesion does not involve the cortical bone, it is most difficult to detect in a PR.13 In a study comparing the radiographic diagnosis based on PR of root canal-treated teeth ex-vivo with histology, all radiographically detectable periapical lesions were confirmed to be inflamed; furthermore 26% of the root canal-treated teeth without any radiographically detectable periapical lesion also showed signs of inflammation.14 The present study supports these findings since five of the included cases were assessed as successfully healed in periapical images, but had mild to moderate inflammation when examined histopathologically (Table 3).
Histopathological examination as a reference standard to assess treatment outcome is often difficult to obtain as this includes a surgical intervention. In 1972, Andreasen & Rud15 demonstrated a correlation between findings in periapical radiographs and inflammatory status in teeth having undergone SER. No studies have been performed to examine whether this correlation also exists between findings in CBCT and histopathology. When performing a biopsy from the periapical area during SER, different techniques can be used. Andreasen & Rud16 used a thin surgical bur to remove a block including the tooth apex and the surrounding structures. This method, although optimal for histopathological verification of the full periapical lesion, is problematic from an ethical point of view since it removes more bone and root dentine than may be necessary. In the present study, we carefully removed the periapical soft tissue in toto using surgical spoons. This approach is a standard part of SER and does not require unnecessary removal of bone or dentine.
In our sample, we found that 75% of teeth with a Rud & Molven score 3 (uncertain healing) in CBCT were without any inflammation. These lesions had healed by fibrous tissue. In the original definition by Rud & Molven, score 2 (incomplete healing) defined cases healed by fibrous tissue, also known as “scar tissue healing”.2,3 This may indicate that it is not always possible to differentiate between score 2 and 3 when the Rud & Molven scoring system is used for CBCT assessment. On the other hand, if a lesion was assessed as Rud & Molven score 4 (unsatisfactory healing) in a CBCT, 82% of the cases displayed inflammation upon histopathological examination. The Rud & Molven scoring system was developed for use in periapical imaging. This may, in part, explain the discrepancies in diagnostic assessment when transferred directly to use in CBCT assessment of periapical healing after SER. Hence, the development of a new healing assessment system based on CBCT seems feasible. This has recently been proposed by von Arx et al.,5 who investigated if the visualization of the periapical area in different planes allowed the observer to evaluate different healing parameters such as the presence and quality the cortical bone, the cancellous bone characteristics, and the ingrowth of bone on the resection surface. The authors evaluated these different parameters in a system for assessment of healing following SER using CBCT. However, histopathological examination of neither the successful nor unsuccessful cases was presented.
When it comes to false positive diagnoses the clinician has to compare the risk of under-diagnosis, and hence under-treatment, to the resources and patient risks and discomfort spent on over-treatment with no patient benefit. The clinician, together with the patient, has to decide if the price of over-treatment is worth paying and outweighs the consequences of other patients possibly being under-treated, if another diagnostic threshold is used. In the present study patient symptoms were a reliable indicator of a periapical inflammatory lesion. This parameter should be taken into account when dealing with the decision of performing SER-R or observe the case further.
Conclusions
In the present study, the correct radiographic diagnosis was obtained for 63 and 58% of cases respectively using PR and CBCT. More than 40% of the SER cases diagnosed as unsuccessfully healed at a 7-year follow-up after SER-R, showed no signs of periapical inflammation after histopathological examination of the periapical soft tissues, and these patients did not benefit from the SER-R procedure.
Most cases assessed as Rud & Molven score 3 in CBCT did not display any histopathological signs of inflammation, whereas in the vast majority of cases assessed as Rud & Molven score 4, inflammation could be verified by histopathology. Patient symptoms were a reliable indicator of an inflammatory periapical lesion.
Within the limitations of the present study, it could be concluded that caution should be exercised when using CBCT for assessment of periapical healing after SER. Further investigations are needed to explore non-invasive methods to discriminate between diseased and non-inflamed periapical soft tissues.
Contributor Information
Casper Kruse, Email: casper.kruse@dent.au.dk.
Rubens Spin-Neto, Email: rsn@dent.au.dk.
Jesper Reibel, Email: jrei@sund.ku.dk.
Ann Wenzel, Email: aw@dent.au.dk.
Lise-Lotte Kirkevang, Email: llki@dent.au.dk.
References
- 1.Ørstavik D, Pitt Ford TR. Essential endodontology: prevention and treatment of apical periodontitis. 2. ed Oxford, UK: Blackwell Munksgaard Ltd; 2008. 478 p. [Google Scholar]
- 2.Rud J, Andreasen JO, Jensen JE. Radiographic criteria for the assessment of healing after endodontic surgery. Int J Oral Surg 1972; 1: 195–214.10.1016/S0300-9785(72)80013-9 [DOI] [PubMed] [Google Scholar]
- 3.Molven O, Halse A, Grung B. Observer strategy and the radiographic classification of healing after endodontic surgery. Int J Oral Maxillofac Surg 1987; 16: 432–9.10.1016/S0901-5027(87)80080-2 [DOI] [PubMed] [Google Scholar]
- 4.Kruse C, Spin-Neto R, Wenzel A, Kirkevang LL. Cone beam computed tomography and periapical lesions: a systematic review analysing studies on diagnostic efficacy by a hierarchical model. Int Endod J 2015; 48: 815–28.10.1111/iej.12388 [DOI] [PubMed] [Google Scholar]
- 5.von Arx T, Janner SF, Hänni S, Bornstein MM. Evaluation of New Cone-beam computed Tomographic criteria for Radiographic healing evaluation after Apical surgery: assessment of repeatability and reproducibility. J Endod 2016; 42: 236–42.10.1016/j.joen.2015.11.018 [DOI] [PubMed] [Google Scholar]
- 6.von Arx T, Janner SF, Hänni S, Bornstein MM. Agreement between 2D and 3D radiographic outcome assessment one year after periapical surgery. Int Endod J 2016; 49: 915–25.10.1111/iej.12548 [DOI] [PubMed] [Google Scholar]
- 7.Kanagasingam S, Lim CX, Yong CP, Mannocci F, Patel S. Diagnostic accuracy of periapical radiography and cone beam computed tomography in detecting apical periodontitis using histopathological findings as a reference standard. Int Endod J 2017; 50: 417–26.10.1111/iej.12650 [DOI] [PubMed] [Google Scholar]
- 8.Simon JH, Enciso R, Malfaz JM, Roges R, Bailey-Perry M, Patel A. Differential diagnosis of large periapical lesions using cone-beam computed tomography measurements and biopsy. J Endod 2006; 32: 833–7.10.1016/j.joen.2006.03.008 [DOI] [PubMed] [Google Scholar]
- 9.Rosenberg PA, Frisbie J, Lee J, Lee K, Frommer H, Kottal S, et al. Evaluation of pathologists (histopathology) and radiologists (cone beam computed tomography) differentiating radicular cysts from granulomas. J Endod 2010; 36: 423–8.10.1016/j.joen.2009.11.005 [DOI] [PubMed] [Google Scholar]
- 10.Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Making 1991; 11: 88–94.10.1177/0272989X9101100203 [DOI] [PubMed] [Google Scholar]
- 11.de Paula-Silva FW, Wu MK, Leonardo MR, da Silva LA, Wesselink PR. Accuracy of periapical radiography and cone-beam computed tomography scans in diagnosing apical periodontitis using histopathological findings as a gold standard. J Endod 2009; 35: 1009–12.10.1016/j.joen.2009.04.006 [DOI] [PubMed] [Google Scholar]
- 12.Brynolf I. A histological and roentgenographic study of the periapical region of human upper incisors (Thesis. Odontologisk Revy 1967; 18: 1–176.5227225 [Google Scholar]
- 13.Bender IB, Seltzer S. Roentgenographic and direct observation of experimental lesions in bone: ii. 1961. J Endod 2003; 29: 707–12.10.1097/00004770-200311000-00006 [DOI] [PubMed] [Google Scholar]
- 14.Green TL, Walton RE, Taylor JK, Merrell P. Radiographic and histologic periapical findings of root canal treated teeth in cadaver. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997; 83: 707–11.10.1016/S1079-2104(97)90324-3 [DOI] [PubMed] [Google Scholar]
- 15.Andreasen JO, Rud J. Correlation between histology and radiography in the assessment of healing after endodontic surgery. Int J Oral Surg 1972; 1: 161–73.10.1016/S0300-9785(72)80006-1 [DOI] [PubMed] [Google Scholar]
- 16.Andreasen JO, Rud J. Modes of healing histologically after endodontic surgery in 70 cases. Int J Oral Surg 1972; 1: 148–60.10.1016/S0300-9785(72)80005-X [DOI] [PubMed] [Google Scholar]