Abstract
Background
Evidence-based interventions exist for prevention of chronic disease in older adults. Partnering with community organizations may provide a mechanism for disseminating these interventions.
Objective
To describe the partnership and program implementation by the Arthritis Foundation (AF) and the University of Pittsburgh.
Methods
The AF Exercise Program (AFEP; an existing evidence-based program) was enhanced with the “10 Keys”™ to Healthy Aging (a prevention-focused program bundling the most common risk factors for chronic disease and disability in older adults and applies behavior change strategies to enhance prevention). The program was delivered in 20 sessions over 10 weeks by community health workers in a cluster-randomized trial.
Lessons Learned
Partnering with an organization having an existing infrastructure supports program delivery at the community level. This partnership provided programming in 54 sites across Pittsburgh and surrounding communities.
Conclusions
This collaborative partnership created a productive synergy maximizing strengths in both research and program delivery.
Keywords: Community, partnership, exercise, preventive behavior, prevention, healthy aging
Chronic diseases are responsible for 7 out of 10 deaths in Americans each year and account for 75% of health care spending.1 Approximately 90% of older adults age 65 and older have at least one chronic health condition, many of which are preventable2,3 with cumulative effects impacting quality of life and health care costs.4 Prevention strategies for these chronic conditions have not been largely successful as less than half of adults age 65 years and older receive services critical for preventing disease and disability.5 The low rates of preventive service use may be owing to dependence on a health care system which is more focused on treatment of disease rather than prevention. In this context, a community-based program that addresses behavior change and self-management offers a potential solution for primary and secondary prevention of chronic disease. Such programs need to be strategically planned and implemented to effectively reduce risk.
A potential mechanism for disseminating and sustaining chronic disease prevention programs is to partner with organizations with parallel missions. These organizations can provide an ideal framework for implementation given their existing infrastructure and links to community partners. This paper describes a collaborative approach used to develop, implement, and evaluate a program designed to increase physical function, decrease pain and stiffness, and improve self-management behaviors and preventive service use in older adults.
THE PARTNERSHIP
In 2009, The Center for Aging and Population Health Prevention Research Center (CAPH-PRC) at the University of Pittsburgh partnered with the AF in western Pennsylvania to collaborate on programming efforts. The Community Coalition, an advisory board to the CAPH-PRC, recommended this partnership given that arthritis is the leading cause of disability in adults6 and is often accompanied by physical inactivity,7 thus increasing risk for chronic disease. The partnership was first developed through one of the CAPH-PRC investigators who worked with the AF.
The AF has existing national, regional, and local programs in which a large number of diverse populations are reached. One of their existing programs is the AFEP. The AFEP is an evidence-based program that was shown to improve arthritis symptoms, upper and lower extremity function, self-management behaviors, and self-efficacy without adverse events (Quitoni K. An evaluation of the People With Arthritis Can Exercise (PACE) program [unpublished report]. 2000).8–15
In 2001, the CAPH-PRC developed the “10 Keys”™ to Healthy Aging Program (“10 Keys”™), which bundles the most common risk factors chronic disease and applies evidence-based behavior change strategies to prevent disease and disability in older adults.16–18 The “10 Keys”™ include control of blood pressure, glucose, and low-density lipoprotein cholesterol, smoking cessation, cancer screenings, immunizations, physical activity, musculoskeletal health, social contact, and combating depression. Because both the AF and the CAPH-PRC had existing evidence-based programs, infrastructure, and resources, a collaborative partnership was formed to modify and enhance existing programming and to strategize for effective implementation. The motivation for enhancing the AFEP with the “10 Keys”™ was to promote awareness and behavior change strategies around the primary issues supporting healthy aging. The product of this collaboration was a 10-week, 20-session program called the AFEP + “10 Keys”™.
ORGANIZATION ROLES AND RESPONSIBILITIES AND COMMUNICATION
The local chapter of the AF and the CAPH-PRC shared responsibilities for the program (Table 1). Both the AF and CAPH-PRC recruited instructors, integrated the content of the programs, and shared training costs. The CAPH-PRC was responsible for new site and participant recruitment and research-related tasks including data collection, data entry, and analysis, and the AF was responsible for facilitating engagement of existing sites and training new instructors. A Research Advisory Board was formed consisting of two representatives from the AF and three representatives from CAPH-PRC. Bi-weekly meetings were held with additional contact made as needed in order to address any program challenges. Although the study design and selection of measures was driven by the researchers, the AF had considerable input into training and implementation. The CAPH-PRC provided all recruitment materials, instructor manuals, participant materials, training on human subject research, and a small stipend for instructors. A representative from the AF also sat on the Data Safety Monitoring Committee for the study.
Table 1.
Roles and Responsibilities of Partner Organizations for Implementation of the AFEP + “10 Keys”™
| Arthritis Foundation | Center for Aging and Population Health Prevention Research Center |
|---|---|
| AFEP training for instructors | “10 Keys”™ and human subjects training for instructors |
| Supplied AFEP exercise manuals | Supplied “10 Keys”™ manuals |
| Recruitment of instructors with AFEP certification | Recruitment of instructors |
| Recruitment of existing AFEP sites | Recruitment of community sites |
| Assessment of the appropriateness of new sites (flooring, access, size) | Participant recruitment in collaboration with sites and assessment of the appropriateness of new sites |
| Processing of AF required forms | Data collection, processing, and analyses |
| Instructor interviews post program |
Abbreviation: AFEP, Arthritis Foundation Exercise Program.
METHODS
Overall Approach
The enhanced program was implemented in two phases. Phase 1 was a pilot and feasibility study conducted in four community sites (reported separately). Results from this pilot informed Phase 2, which was a cluster randomized trial testing the effectiveness of the enhanced AFEP + “10 Keys”™ compared with the AFEP alone.
Study Design
This study was a cluster randomized trial with the community site as the unit of randomization. Fifty-four sites were randomized. Sites included 13 senior centers (24.1%), 15 residential facilities (27.8%), 9 churches (16.7%), 5 community centers (9.3%), 4 YMCAs (7.4%), 4 fitness centers/clubs (7.4%), and 4 libraries (7.4%).
Site Identification
Communities with high morbidity and mortality in Allegheny County, Pennsylvania, were targeted for recruitment. Morbidity and mortality rates were based on previous analyses that used data from the U.S. Bureau of the Census and the Department of Health Vital Statistics, Pennsylvania.19,20 Initially, program sites were identified through networking at community events and word of mouth. Research staff visited site administrators to describe the program and explain the research procedures, including randomization. Once sites agreed to participate, they signed the “AF Program Co-sponsorship Agreement,” which outlined commitment to training, adherence to minimum facility standards, program implementation, and program monitoring. They also signed a “Site Agreement Form” which provided permission for the research to take place at the site, and randomization. Sites were matched on key community demographic characteristics derived from the U.S. Census data,21 including the proportion of the population 65 years or older, the proportion of the population 65 years or older and below the federal poverty level, and race.
Instructor Recruitment and Training
The AF staff sent a description of the program to previously certified AFEP instructors. Additional instructors were identified by recruited sites or by word of mouth. Once instructors expressed interested in the AFEP + “10 Keys”™ they participated in a 1-day training session. They were also required to be certified in CPR. Instructors received training in the “10 Keys”™ by completing an online educational module (www.caph.pitt.edu). Over a 2-year period, 77 instructors were trained.
Human Subjects
The University of Pittsburgh Institutional Review Board approved the study. Because the intervention was a research study that took place in community sites and was delivered by a lay member of the community, instructors were required to complete training in ethical conduct of research which was provided by CAPH-PRC research staff. The training consisted of a one-hour session on ethics in human subject research. The content included materials available from the Institutional Review Board and those developed by CAPH-PRC specific to the research study. Subject matter included the Belmont Principles,22 informed consent, social and educational research concepts, confidentiality, and study design. Case studies reflecting anticipated challenges of the research study were presented and discussed.
Participant Recruitment
Recruitment began once research staff, program instructor, and site staff collaboratively agreed on a start date. Recruitment methods were also discussed and agreed upon. The CAPH-PRC provided materials for each site to distribute internally and/or in the surrounding community through mailings, postings, church bulletins, websites, or pre-program “promotions” that demonstrated the program and allowed potential participants to meet the instructor. Recruitment costs were shared by the CAPH-PRC and the sites.
Screening
Interested members of the community either contacted the CAPH-PRC staff directly or the site provided a list of interested participants who were subsequently called by the research staff. During this call, potential participants were given information about the program and were screened for eligibility for the research study. Eligibility criteria included age 50 years or older, no surgery or cardiac event in the past 6 months, and no use of oxygen therapy. Those not interested in the research study were still invited to participate in the program.
Program Content
Sessions for sites randomized to the AFEP group were 60 minutes long and consisted of exercise and 3 to 5 minutes of health education. The exercise included a joint check, warm-up, active range of motion, strengthening, joint check, cool down, and relaxation. Sessions for the AFEP + “10 Keys”™ group consisted of the same exercises and 10 to 20 minutes of health information and health behavior change strategies from the “10 Keys”™. The first session of the week was an introduction to a “Key,” and the second session of the week was reinforcement of the “Key.” The essential components of the “10 Keys”™ portion of the program included 1) the Personal Goals and Action Steps for each “Key” and 2) the Prevention in Practice Report (Figure 1). At the final session of the program, every participant received a certificate of completion and a manual from the AF with a detailed description and diagram of each exercise. The AFEP + “10 Keys”™ participants also received a “10 Keys”™ to Healthy Aging Resource Guide.
Figure 1.
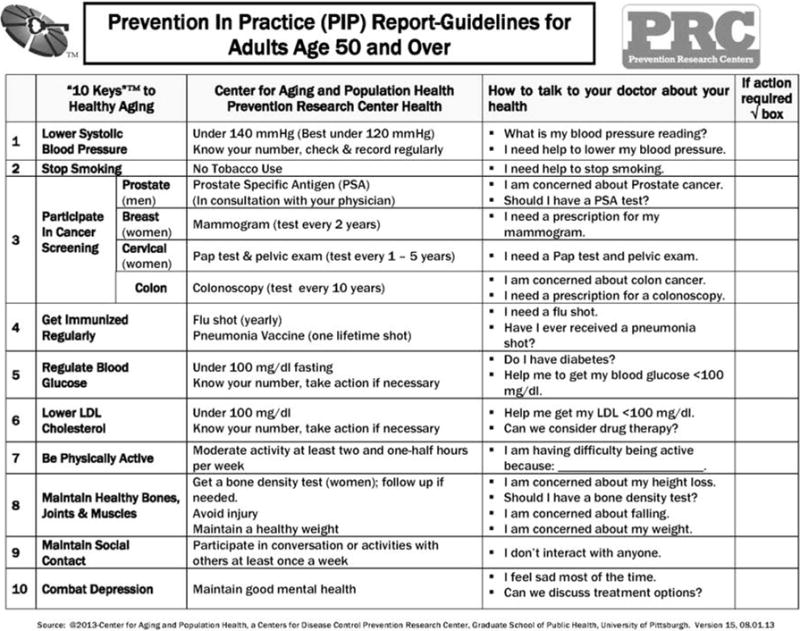
Prevention in Practice (PIP) Report
Maintenance
Sites randomized to the AFEP + “10 Keys”™ were offered four booster or maintenance sessions after the 10-week program was complete. These sessions were added after the initial 10 weeks to enhance awareness and reinforce behavior change strategies around healthy aging. Group meetings were facilitated by the class instructor or research staff. These non-exercise sessions focused on goal setting, action steps, and problem solving. The instructor assisted participants in defining realistic and measurable goals to maintain or make progress on their preventive health behaviors.
Program Measures
All participants signed the AF release form and completed a survey of demographic information, arthritis diagnosis, and pre-program exercise patterns. Within the first week of the program, research staff obtained informed consent from the subset of participants expressing interest in the research study. The research study included a detailed assessment of health and function at baseline, after the program, 6 months, and 1 year to evaluate the effectiveness of the enhanced program (AFEP + “10 Keys”™) compared with the AFEP alone. Assessments included height, weight and blood pressure, the Short Physical Performance Battery,23,24 and questionnaires (pre ventive behaviors; Western Ontario and McMaster Universities Osteoarthritis Index scales: pain, stiffness, and function25,26; Stanford Patient Education Research Center Self-efficacy scale27; and the modified Self-efficacy Scale [PRESS]). During the last session of the program, participants completed an anonymous survey to evaluate the instructor, exercises, health messages, and overall satisfaction with the program.
Analysis
Quantitative data were first analyzed to examine the distribution, frequencies, and normality of the data. To examine the difference between groups, the chi-square test was used for dichotomous outcomes and the Student t test for continuous variables. Mixed models were used to adjust for the correlation among participants within site. The p-values presented are from adjusted mixed models. All data were analyzed using SAS version 9.3 (Cary, NC).
Qualitative Methods
Participants provided testimonials about the program and were invited to suggest program improvements (Table 2). Testimonials were categorized into themes. Semi-structured interviews were conducted with instructors and analyzed for relevant process improvement information. Responses to the following three questions were examined: “Were there any barriers to leading your program?”, “What was the most challenging aspect of leading the program?”, and “If you could repeat the experience, would you make any changes?” Two staff members (L.V., S.K.) independently analyzed participant responses using ATLAS.ti,28 a software program for qualitative data analysis. Discrepancies were adjudicated by the research coordinator (J.V.B.). An inter-rater reliability of 94% was achieved using a calculated kappa statistic.29
Table 2.
Themes Emerging from Participant Testimonials and Feedback in the AFEP + “10 Keys”™ Program
| Theme | Illustrative Quotes |
|---|---|
| All AFEP participants | |
| Improved function | “I was suffering from severe arthritis in my shoulders and upper muscle in my arms. In the morning my pain was so great I could not remove my quilt to get out of bed. Since I have been taking this arthritis class I have improved immensely with little or no pain.” “I feel 100% better since starting the program. Much more range of motion, easier to climb stairs, much easier to pick up dropped objects. Sense of balance is better although I need much more work on this! Overall, excellent program!” “Since joining our class I am so much more flexible. I can move more easily & the pain has diminished.” |
| I could do it | “Was very helpful for me. I could do most of the exercises even though I’m 90 years old.” “Exercise are low impact and manageable.” “It got me back to basic every day. Doable exercises.” |
| Socialization | “This program motivated me to get out and move during the winter months… [The] best part was meeting some wonderful people and making new friends.” “The social aspect was wonderful. We laughed and interacted so much, the exercise time just zipped by.” “This program gets me out of my apartment and I meet very nice people.” “It was great exercising with a group and I looked forward to exercising every week.” |
| AFEP + “10 Keys”™ participants | |
| Disease prevention knowledge | “It made me realize how important it is to keep check on health, like doing exercises, checking with doctor on blood work, and immunization tests. Knowing the effects of my medications, how important diet is, and monitoring my blood pressure.” “I learned a lot about high blood pressure, sodium, how many products have sodium, osteoporosis – painful, no warning. Keep active and walk as far as you can and do little more each day. Exercise even in the winter.” “Made me aware of [the] importance of drinking more water, the importance of social contact, and the importance of watching [my] blood pressure.” |
| Preventive action | “Decided to add more time to my exercise program. Cut down on salt. Got tetanus shot from GP.” “Since I have been taking the class I have been paying more attention to my diet consuming less sugar. When I go shopping I do pay attention [to] what I am buying and take time to see what is in the product. I never paid too much attention before.” “Made the decision to get a bone density test.” “It is beginning to make me take charge of my diet decisions. Being diabetic I already know what to do but I don’t do everything I need to do.” |
Abbreviation: AFEP, Arthritis Foundation Exercise Program.
RESULTS
Baseline characteristics of the 462 research participants showed no significant differences in demographic characteristics (Table 3), physical function, or proportion with chronic diseases or chronic disease risk factors at baseline between the AFEP + “10 Keys”™ and AFEP group. Program participants were on average 73 years old, female (88%), and White (80%), with two-thirds having an education beyond high school. A diagnosis of arthritis was self-reported by 81% of participants. The final results of the trial will be available in a separate publication.
Table 3.
Baseline Characteristics of 462 Participants in 54 Sites of the AFEP + “10 Keys”™ Cluster Randomized Trial
| Sociodemographic Characteristics | Total Participants (N = 462) | AFEP + “10 Keys”™ (n = 229) | AFEP Alone(n = 233) | p Value |
|---|---|---|---|---|
| Ages, mean ± SD (range) | 72.7 ± 7.83 (51–91) | 72.4 ± 7.63 (53–90) | 73.1 ± 8.02 (51–91) | 0.9534 |
| Female, n (%) | 406 (87.9) | 203 (88.7) | 203 (88.7) | 0.9459 |
| Race, n (%) | 0.9611 | |||
| White | 366 (80.3) | 173 (77.2) | 193 (83.2) | |
| Black | 81 (17.8) | 47 (21.0) | 34 (14.7) | |
| Other | 9 (1.9) | 4 (1.8) | 5 (2.1) | |
| Education, n (%) | 0.9862 | |||
| High school or less | 168 (37.0) | 76 (34.2) | 92 (39.7) | |
| Some college or higher | 286 (63.0) | 146 (65.8) | 140 (60.3) | |
| Income, n (%) | 0.6241 | |||
| <$25,000 | 203 (49.9) | 92 (45.8) | 111 (53.9) | |
| ≥$25,000 | 204 (50.1) | 109 (54.2) | 95 (46.1) |
Abbreviations: AFEP, Arthritis Foundation Exercise Program; SD, standard deviation.
Satisfaction Survey
Data from the first 331 participants completing the satisfaction survey were analyzed. Eighty-nine percent rated the class as “good” or above for all questions. Additionally, 132 (40%) offered comments on program improvement. Forty-eight of these comments (36%) suggested increased duration or frequency of the program. Among all participants, three primary themes were identified. They included improved function, self-efficacy, and socialization (Table 2). Among those who participated in the enhanced program themes included disease prevention knowledge and preventive action.
Results from the semi-structured interviews from the first 28 instructors and participant feedback regarding programmatic issues were divided among three themes: organization, site, or individual (Table 4).
Table 4.
Themes Emerging from the AFEP + “10 Keys”™ Program Phase 2 Participant Feedback and Semi-Structured Instructor Interviews
| Level | Theme | Illustrative Quotes |
|---|---|---|
| Organizational (CAPH-PRC) | Educational delivery | “Give the exercise manual earlier and incorporate its use throughout the program to increase the likelihood of continued use.” “A few visuals or charts would be helpful to absorb different aspects of the program.” “Give us copies of exercises that we could do on the days that we don’t have your program.” |
| Community outreach | “Promote to persons who do not exercise, or those who exercise very little.” “The program should come to the Swissvale area and make it convenient to get to by bus.” “… everyone I told about the program wants to find one too—where is the information about what is available?” |
|
| Community (sites) | Site and equipment | “The elevator was broken the first 2 weeks.” “Have water in the room. It took me 7 weeks before I realized there was water in the other room…” “Other people were in the room, [there was] no door between the program and other space.” |
| Class environment | “Room temp varied—too much—either too hot or too cold on some days.” “Quieter music so we can hear the instructor. The choice of music was delightful—the kind we are familiar with but it is more important to hear the instructor….” “The gym was always too cold and there is an echo, it was difficult to hear sometimes.” |
|
| Individual | Instructor traits | “The instructor would be better if she slowed down. It’s hard to keep up with her.” “Instructions [should] be more direct; sometimes [they are] hard to follow.” “More emphasis on how/why movement helps.” “With two different instructors (Monday and Wednesday) maybe more communication between the two to know what they each covered.” |
| Participant traits | “Loss of hearing. Pain and health issues prevented many from coming regularly.” “Felt the participants were not regimented to attend class on time. They came in as they may.” “Some participants need a little one on one.” |
Abbreviation: AFEP, Arthritis Foundation Exercise Program.
Organizational level
Educational Delivery
In general, participants recommended that more resources for the “10 Keys”™ materials (e.g., handouts, visual guides) would enhance the experience. Others suggested earlier delivery of the AFEP manual to facilitate learning at home. Another common theme suggested that the content focus more on arthritis (e.g., including nutritional information about arthritis prevention and treatment).
Community Outreach
Both participants and instructors expressed a desire to extend the reach of the program. Participants also requested more accessible information about future classes (to inform family and friends) and broader recruitment strategies to increase community participation in the program.
Community level
Site and Equipment
Instructors conveyed dissatisfaction with certain site characteristics, such as classroom size, lack of on-site parking, elevator accessibility, and room acoustics. Participants tended to request improvements to equipment, for example, weights and exercise bands.
Class Environment
Participants and instructors alike made suggestions to improve the overall classroom atmosphere. Proposed modifications included using lower volume music and addressing poor air quality and uncomfortable room temperature.
Individual Level
Instructor Traits
In general, participants requested that instructors teach a wider range of exercise rigor and speak more loudly in class. Both participants and instructors felt that improved inter-instructor communication would enhance classes taught by multiple instructors. In addition, instructors noted personal traits that hindered their delivery of the program, for example, language barriers (for international instructors), and difficulty adjusting to differing fitness or functional capabilities of participants.
Participant Traits
In general, instructors mentioned health of participants as a challenge to effective class execution (e.g., absences owing to hospitalizations). Frequently noted health issues included seasonal illnesses, falls, hearing loss, allergies, and functional impairments. Instructors also mentioned concerns regarding participant focus and punctuality.
DISCUSSION
In this paper, formation of a partnership between the CAPH-PRC and the AF was described. The partnership was established successfully based on mutual agreement for program development, use of resources, and roles in program implementation. The enhanced exercise program, with behavioral strategies for healthy aging, supported the goals of both organizations to increase physical activity and physical function while improving awareness of and participation in the use of recommended preventive services. Through this partnership, 77 community health workers were trained to deliver the program in 54 sites.
Recently, the Centers for Disease Control and Prevention (CDC) published “Enhancing Use of Clinical Preventive Services Among Older Adults – Closing the Gap.”30 The CDC report prioritized recommendations by organizing them into two categories: “featured preventive services” for which they had state and national data about use of services and “additional preventive services,” which were given less emphasis. “Featured” services included influenza and pneumococcal vaccinations; breast and colorectal cancer screening; diabetes, lipid disorders, and osteoporosis screenings; and smoking cessation counseling. “Additional” services included zoster vaccination; cervical cancer screening; alcohol use, depression and obesity screening and counseling; aspirin use; and blood pressure screening. On average, one-fourth to one-third of the population in our study area did not receive these services representing a large gap in primary and secondary prevention. The CDC report also advocates for an “expanded chronic care model” for delivering preventive services, which would link health system and community efforts. The U.S. Preventive Service Task Force guidelines for older adults will assist in clinical provision of appropriate preventive services, however, completely relying on the health care system structured around a ‘treatment of illness’ model to provide these services is problematic.
There are existing community-based programs for older adults such as Silver Sneakers,31 Enhance Fitness,32 and the Chronic Disease Self-Management Program.33 Our model for partnering with a national organization like the AF provides a unique venue for dissemination of community-based programming on a large scale given their broad reach to heterogeneous older adult populations.
Our data support the feasibility, acceptability and community benefit of the program. Participants noted improvements in their physical function, felt the program was manageable for their level of fitness, and enjoyed the social aspect of classes. Participants also noted increased disease prevention knowledge, and many took action to improve their health.
LIMITATIONS
Although our program was well-received throughout the community, program implementation did present several challenges. First, complying with human subject regulations at the community level was complex. We were able to address this complexity by working closely with the institutional review board to develop and implement training for instructors. Second, every site had a unique organizational structure that had to be considered before program implementation. This variability enhanced external validity but challenged internal validity. The commitment of the CAPH-PRC to community engagement meant that all sites provided input on program implementation. This participatory model addressed the context in which the program was delivered and was critical for successful implementation. Another limitation of our work is the population reached by the program which was largely female, Caucasian, and more educated. This limits the generalizability of our results to more underserved populations. However, our partnership with the AF positions the CAPH-PRC to expand outreach.
In conclusion, our collaborative approach created a productive synergy at the organizational level, thereby maximizing the strengths in both research and program delivery at the community level and outcomes at the individual level. Future initiatives will include the addition of systematic criteria for instructor selection, training, consultation and coaching, staff and program evaluation, fidelity of program delivery, facilitative and administrative supports, and systems intervention.34 This process will examine both process and implementation outcomes. Community based programs such as the one described, may offer a solution for enhancing health and wellness in older adults.
Acknowledgments
This study was funded by the Centers for Disease Control and Prevention, Health Promotion and Disease Prevention Research Center, U48DP001918.
References
- 1.National Center for Chronic Disease Prevention and Health Promotion, editor. Centers for Disease Control and Prevention. The Power of Prevention: Chronic Disease…the public health challenge of the 21st century. Atlanta, GA: 2009. [Google Scholar]
- 2.Anderson G. Chronic Care: Making the Case for Ongoing Care. Robert Wood Johnson Foundation; 2010. [Google Scholar]
- 3.Centers for Disease Control and Prevention. Healthy Aging. Atlanta, GA: National Center for Chronic Disease Prevention and Health Promotion; 2011. [Google Scholar]
- 4.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA-J Am Med Assoc. 2002;288:2469. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 5.US Department of Health & Human Services. Healthy People 2020. Washington, DC: US Department of Health & Human Services; [Google Scholar]
- 6.National Center for Chronic Disease Prevention and Health Promotion Division of Population Health Centers for Disease Control and Prevention, editor. Centers for Disease Control and Prevention. Addressing the nation’s most common cause of disability. At a glance 2015. Atlanta: Centers for Disease Control and Prevention; 2015. [Google Scholar]
- 7.Shih M, Hootman JM, Kruger J, Helmick CG. Physical activity in men and women with arthritis, National Health Interview Survey. Am J Prev Med. 2006;30:386. doi: 10.1016/j.amepre.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Anderson JM. Evaluation of the PACE exercise program and its effect on self-eficacy, pain, depression, and functional ability. Atlanta: Emory University; 1991. [Google Scholar]
- 9.Arthritis Foundation. Arthritis Foundation PACE exercise program evaluation. 1987 [Google Scholar]
- 10.Boutaugh ML. Arthritis Foundation community-based physical activity programs: effectiveness and implementation issues. Arthritis Rheum. 2003;49:463. doi: 10.1002/art.11050. [DOI] [PubMed] [Google Scholar]
- 11.Callahan LF, Mielenz T, Freburger J, et al. A randomized controlled trial of the People with Arthritis Can Exercise Program: symptoms, function, physical activity, and psychosocial outcomes. Arthritis Care Res. 2008;59:92. doi: 10.1002/art.23239. [DOI] [PubMed] [Google Scholar]
- 12.Doyle MA, Farrar V, Ryan S, Sisola S. An evaluation of PACE [abstract] Arthritis Care and Research. 1990;3:S7. [Google Scholar]
- 13.Kennedy C, Walker K, Linnel S, Johnson R, Sockler J. Effect of exercise on social activity and health status in women with RA [abstract] Research Quarterly for Exercise and Sport. 1992;63:A. [Google Scholar]
- 14.Schoster Britta, Callahan Leigh F, Meier Andrea, Mielenz Thelma, DiMartino Lisa. The People with Arthritis Can Exercise (PACE) Program: A Qualitative Evaluation of Participant Satisfaction. Preventing Chronic Disease. 2005 [PMC free article] [PubMed] [Google Scholar]
- 15.Suomi R, Collier D. Effects of arthritis exercise programs on functional fitness and perceived activities of daily living measures in older adults with arthritis. Arch Phys Med Rehabil. 2003;84:1589. doi: 10.1053/s0003-9993(03)00278-8. [DOI] [PubMed] [Google Scholar]
- 16.Newman AB, Bayles CM, Milas CN, McTigue K, Williams K, Robare JF, Taylor CA, Albert SM, Kuller LH. The ‘10 Keys’™ to Healthy Aging: Findings From an Innovative Prevention Program in the Community. Journal of Aging and Health. 2010;22:547. doi: 10.1177/0898264310363772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robare JF, Bayles CM, Newman AB, Williams K, Milas C, Boudreau R, McTigue K, Albert SM, Taylor C, Kuller LH. The ‘10 Keys’ to Healthy Aging: 24-Month Follow-Up Results From an Innovative Community-Based Prevention Program. Health Education & Behavior. 2011;38:379. doi: 10.1177/1090198110379575. [DOI] [PubMed] [Google Scholar]
- 18.Center for Aging and Population Health Prevention Research Center. The “10 Keys”™ to Healthy Aging. Center for Aging and Population Health Prevention Research Center; 2012. [Google Scholar]
- 19.“Allegheny County Death records 2005–2008.”
- 20.U.S. Census Bureau. 2005–2009 American Community Survey Allegheny County. 2011 [Google Scholar]
- 21.U.S. Census Bureau. “2010 Census Summary File 1,” in using American FactFinder. 2010 [Google Scholar]
- 22.The National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. The Belmont Report. Ethical Principles and Guidelines for the Protection of Human Subjects of Research. Washington, DC: 1979. [PubMed] [Google Scholar]
- 23.Guralnik JM, Ferrucci L, Simonsick EM, et al. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995:556. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol Med Sci. 1994;49:M85. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 25.Bellamy N. In: WOMAC Osteoarthritis Index: User guide IX. Centre of National Research on Disability and Rehabilitation Medicine, editor. Herston, Queensland: 2009. [Google Scholar]
- 26.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumotol. 1988;15:1833. [PubMed] [Google Scholar]
- 27.Lorig K, Stuart A, Ritter P, Gonzalez V, Laurent D, Lynch J. Outcome measures for health and education and other health care interventions. Thousand Oaks, CA: 1996. [Google Scholar]
- 28.ATLAS.ti 7.
- 29.Sim J, Wright CC. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Physical Therapy. 2005;85:257. [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Enhancing Use of Clinical Preventive Services Among Older Adults. In: Centers for Medicare and Medicaid Services Agency for Healthcare Research and Quality, editor. AARP. Washington, DC: Administration on Aging; 2011. [Google Scholar]
- 31.Healthways. Silver Sneakers Fitness. 2014 [Google Scholar]
- 32.Belza B, Snyder S, Thompson M, LoGerfo J. Enhance Fitness, an innovative community-based senior exercise program. Topics in Geriatric Rehabilitation. 2010;26:299. [Google Scholar]
- 33.Lorig K, Sobel DS, Stewart AL, Brown WB, Bandura A, Ritter P, Gonzaez VM, Laurent DD, Holman HR. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalizations: A randomized trial. Med Care. 1999;37:5. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 34.Fixsen DL, Naoom SF, Blase KA, Friedman RM, Wallace F. Implementation Research: A synthesis of the Literature. Tampa, FL: University of South Florida, Louis de la Parte Florida Mental Health Institute; 2005. [Google Scholar]


