Abstract
Introduction
Concomitant with the growth of music intervention research, are concerns about inadequate intervention reporting and inconsistent terminology, which limits validity, replicability, and clinical application of findings.
Objective
Examine reporting quality of music intervention research, in chronic and acute medical settings, using the Checklist for Reporting Music-based Interventions. In addition, describe patient populations and primary outcomes, intervention content and corresponding interventionist qualifications, and terminology.
Methods
Searching MEDLINE, PubMed, CINAHL, HealthSTAR, and PsycINFO we identified articles meeting inclusion/exclusion criteria for a five-year period (2010-2015) and extracted relevant data. Coded material included reporting quality across seven areas (theory, content, delivery schedule, interventionist qualifications, treatment fidelity, setting, unit of delivery), author/journal information, patient population/outcomes, and terminology.
Results
Of 860 articles, 187 met review criteria (128 experimental; 59 quasi-experimental), with 121 publishing journals, and authors from 31 countries. Overall reporting quality was poor with < 50% providing information for four of the seven checklist components (theory, interventionist qualifications, treatment fidelity, setting). Intervention content reporting was also poor with < 50% providing information about the music used, decibel levels/volume controls, or materials. Credentialed music therapists and registered nurses delivered most interventions, with clear differences in content and delivery. Terminology was varied and inconsistent.
Conclusions
Problems with reporting quality impedes meaningful interpretation and cross-study comparisons. Inconsistent and misapplied terminology also create barriers to interprofessional communication and translation of findings to patient care. Improved reporting quality and creation of shared language will advance scientific rigor and clinical relevance of music intervention research.
Keywords: reporting quality, music, music therapy, intervention, systematic review
Both public interest in and publication of music intervention studies are increasing, with more than 1,300 articles indexed in PubMed over the last 20 years and 190 review articles examining the benefits of music interventions for a variety of health conditions and outcomes. The NIH-Kennedy Center Sound Health: Music and the Mind initiative is also working to accelerate our understanding about the use of music for health benefit through interdisciplinary scientific collaboration.[1] Concomitant with this growth are concerns about inadequate intervention descriptions and inconsistent terminology in published research, which limits validity, replicability, and clinical application of findings.[2–10] The growth of music therapy as standard care, along with increased use of music listening and music-facilitated movement interventions delivered by a variety of healthcare professionals, necessitates close examination of intervention reporting to improve specificity of meta-analyses, interprofessional communication, and integration of research findings into practice.
Reporting guidelines and music intervention research
The Consolidated Standards for Reporting Trials (CONSORT) and Transparent Reporting of Evaluations with Non-randomized Designs (TREND) guidelines were developed to improve the quality and transparency of published research, with one specific item on each checklist dedicated to intervention reporting.[11, 12] Subsequent publications explored the complexities of behavioral and non-pharmacological interventions, resulting in elaborated CONSORT guidelines for intervention reporting.[13–16] However, music interventions are especially difficult to fully describe due to the complexity of music stimuli (e.g., rhythm, pitch, tempo, harmonic structure, timbre), variety of music experiences (e.g., active music making vs. receptive music listening), and other factors unique to music interventions. To determine whether music intervention reporting guidelines were necessary, Robb and Carpenter (2009) examined how authors described music interventions and found significant gaps in reporting that hinder cross-study comparisons, generalization, and integration of findings into practice.[17] Subsequently, Robb, Burns, and Carpenter (2011) developed Reporting Guidelines for Music-based Interventions that specify seven components of music interventions that publishing authors are encouraged to report and discuss.[9]
The Reporting Guidelines for Music-based Interventions are available through the Equator Network and in the past six years referenced by authors in ninety-five publications, including nine review articles.[18, 19] Based on recent reviews, several areas of reporting continue to be problematic including the absence of intervention theory or scientific rationale for the specified use of music,[20–22] details about the music used, [21–26] and information about who selected the music (patient, investigator, or therapist based on assessment).[25–27]
An additional concern has been inconsistent and inaccurate use of terminology that is well defined and consistently applied across studies. [21, 25] For example, some authors have used the term “music therapy” interchangeably, and at time inaccurately, with other terms to describe their intervention. [21] This creates confusion and contributes to problems with interprofessional communication because “music therapy” refers to a profession (as does nursing, occupational therapy, or medicine) and indicates the education, training, and credentials of the professional delivering the intervention, rather than providing information about the specific intervention.
Early and recent Cochrane reviews examining the benefits of music interventions for a variety of client and patient populations have raised awareness about the need to differentiate between music interventions that are delivered by a credentialed music therapist and those delivered by other health professionals. [2, 5, 8, 10, 31] Based on the background and training of the person providing the intervention, these reviewers have noted marked differences in intervention content, mode of delivery, and the use of clinical assessment to tailor intervention content based on patient needs and responses – and these factors are important to consider when conducting cross-study comparisons and meta-analyses. Using a two-category classification system (i.e., interventions delivered by credentialed music therapists and interventions delivered by other healthcare providers), Cochrane Review authors have been able to glean important information about the differential benefits of these two “types” of interventions for several patient populations. [3, 8] More importantly, they have begun to isolate specific attributes of the music intervention that may be responsible for change and patient factors that will help predict who would benefit from what “type” of intervention.
This differentiation is important as we seek to identify the mechanisms of action responsible for changes observed in music intervention research, and patient factors that predict who will derive the most benefit from which intervention. However, as noted by Cochrane Review authors, [3, 8] improved and consistent intervention reporting across all professions investigating the use of music to improve health will allow for more meaningful and nuanced subgroup analyses that move beyond the broader two-category classification system focused on professional background and training.
The primary aim of this systematic review was to examine the reporting quality of music intervention research published from 2010 through 2015. Our secondary aim was to gain a more complete picture of where music intervention research is being conducted (patient populations and primary outcomes of interest), as well as content of music interventions and training of those delivering interventions. Unique to this analysis was an examination of terminology to improve interprofessional communication and collaboration through improved consistency of terms, and development of shared language. Because our primary aim was to examine reporting quality, we looked at studies across a wide range of clinical populations, music interventions, and outcomes. Given the heterogeneous nature of the resulting data set, an examination of intervention efficacy would not yield meaningful data and was considered beyond the scope of the current review. The following research questions guided our review:
What is the quality of music intervention reporting in published research?
What is the professional background of authors publishing music intervention research and where are they publishing their work?
What patient populations and outcomes are investigators studying?
What terms do authors use to describe music interventions and are those terms defined?
What is the education, professional background, and/or training of individual(s) who are delivering music interventions?
What is the content of music interventions and does it vary based on education, professional background, and/or training of the interventionist?
Methods
Identification of relevant studies
An interprofessional team comprised of undergraduate honors nursing students from Indiana University School of Nursing, undergraduate music therapy students from University of Kansas School of Music, and a graduate student and faculty member from each program conducted this review. As the first comprehensive review of music intervention reporting quality, our intent was to establish a baseline review that would capture reporting just prior to and after publication of the Music-based Intervention Reporting Guidelines. Establishing a baseline review for publications spanning 2010-2015 will help determine whether reporting quality improves over the next five to ten years. We operationally defined music interventions in healthcare as the use of music to manage symptoms, improve quality of life, promote physical and/or psychosocial function, and/or promote well-being (including spirituality) in patients with chronic or acute health conditions. We used this definition to inform article inclusion and exclusion criteria.
Inclusion criteria
Peer reviewed articles published January 1, 2010 through December 31, 2015.
Articles published in English.
Music or music experiences are the primary intervention modality.
Intervention addresses a specified clinical need.
Patients involved in the study have a chronic or acute medical condition.
Experimental and quasi-experimental studies using randomized and non-randomized controlled trial designs.
Exclusion Criteria
Not a clinical music intervention study (e.g. basic music perception or science studies that use music as a stimulus in a laboratory context).
Music was not a primary intervention modality (i.e. bundled interventions where music was not an essential component).
Non-experimental study designs.
Review articles or program descriptions.
Studies with individuals without a medical condition, well populations, dental patients, or interventions targeting at-risk populations (e.g. preventive).
Search strategies
We searched for articles using MEDLINE, PubMed, CINAHL, HealthSTAR, and PsycINFO databases. Our search terms were music and music therapy AND intervention or interventions. Limits added to the database search included: 2010-2015, English Only, Humans Only, Clinical Trials, All, Comparative Study, Controlled Clinical Trial, Evaluation Studies, Journal Articles, Observational Study, Randomized Controlled Trial (See Appendix A for Full Electronic Search Strategy). This review was designed to examine reporting quality of peer-reviewed publications; therefore, grey literature, hand searching, and expert sources were not included.
Data extraction
We used the Music-based Intervention Reporting Guidelines checklist to examine reporting quality,[9] and developed a tool (with corresponding definitions) to guide secondary data extraction for each reviewed article (See Appendix B). Using this tool, we recorded the seven reporting criteria specified in the guidelines, author and journal information, study design, terminology, patient population, interventionist education/professional background, and intervention content.
Five interprofessional student dyads (one music therapy and one nursing undergraduate student) worked together to screen articles and extract data, with faculty members (SR, DHA) providing a subsequent, independent review for each article. First, we identified relevant articles using two levels of screening, followed by data extraction. First level screening included a review of study titles and abstracts, followed by second level screening of full text articles. Following article identification, two independent reviewers (one student dyad and one faculty reviewer) extracted data. At each level of screening and data extraction, results were compared across reviewers and discrepancies resolved through discussion and group consensus. As a final step, the first author entered data for each article into a customized Access database, which is a Microsoft database management system.
We minimized data extraction bias with three strategies: 1) the use of interprofessional student dyads (music therapy; nursing); 2) independent review and data extraction by each member of the student dyad, followed by reconciliation of any discrepancies within that dyad; and 3) second independent review and data extraction by the faculty team members, followed by reconciliation of any discrepancies. In this study, we were interested in the quality and content of intervention reporting; therefore, we did not assess risk of bias for individual studies.
Results
Based on our search for relevant articles published between January 1, 2010 and December 31, 2015, we identified 860 articles. After removing duplicate articles (n=7), remaining titles and abstracts (n=853) were divided among team members and independently screened by two reviewers for inclusion or exclusion, with any discrepancies resolved through group consensus. After reviewing abstracts, we excluded an additional 618 articles, leaving 235 articles for full-text review. Based on full-text reviews, we excluded an additional 48 articles, resulting in our final data set of 187 articles (see Appendix C for references). The PRISMA Flow Diagram (Figure 1) illustrates the article identification process and reasons for article exclusion.
Figure 1.
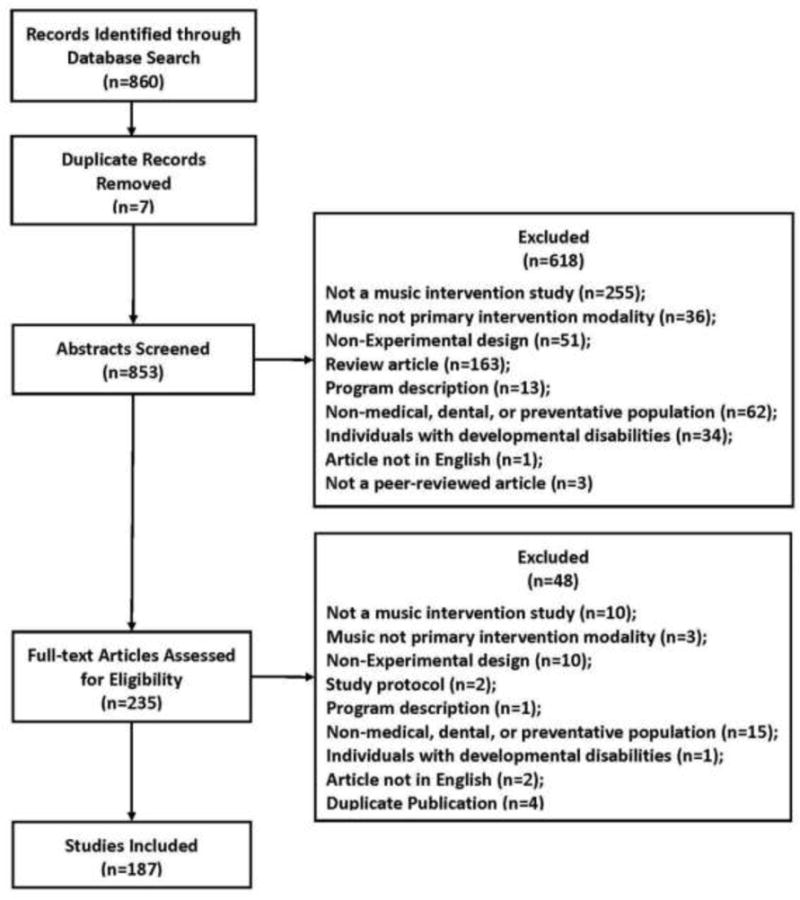
PRISMA flow diagram
Study characteristics
Of the 187 articles included in the analysis, 128 were experimental and 59 quasi-experimental studies. Authors were from 31 countries, with the majority from the United States (n=64), followed by Taiwan (n=18), Australia (n=14), Iran (n=11) and China (n=10). Four studies had authors from more than one country.
Music intervention reporting quality
In Table 1, we report the valid percent of studies that provided information for each of the seven reporting criteria. Here we identify each reporting area as strong (≥ 80%), moderate (60-79%), or poor (≤ 59%) based on Table 1 summative data.
Table 1.
Quality of intervention reporting based on the Checklist for Reporting Music-based Interventions
| Music-based Intervention Reporting Criteria | Reviewed Studies | |
|---|---|---|
| Yes (n) Valid % |
No (n) Valid % |
|
|
A: Intervention Theory/Rationale (n=187) Provide a rationale for the music selected; specify how qualities and delivery of the music are expected to impact targeted outcomes. |
(96) 51% | (91) 49% |
|
B: Intervention Content Provide precise details of the music intervention and, when applicable, descriptions of procedures for tailoring interventions to individual participants. | ||
| B.1: Person Selecting the Music (n=187) Specify who selected the music: pre-selected by investigator, participant from limited set, participant selected from own collection, tailored based on patient assessment. |
(166) 89% | (21) 11% |
| B.2: Music Specify the specific source of published/recorded music, or describe qualities of improvised/original music: | ||
| (1) When using published music, provide reference for sheet music or sound recording. (n=162)a, b | (25) 15% | (137) 85% |
| (2) When using improvised or original music, describe the music’s overall structure (e.g., form, elements, instruments). (n=64)b, c | (34) 53% | (30) 47% |
| B.3. Music Delivery Method (Live or Recorded) | ||
| When using live music, specify: (n=81)d, e (1) Who delivered the music, and |
(67) 83% | (14) 17% |
| (2) Size of the performance group (e.g., interventionist only, interventionist and participant). | (50) 62% | (31) 38% |
| When using recorded music, specify: (n=139)e, f (1) Placement of playback equipment and/or the use of headphones vs. speakers, |
(90) 65% | (49) 35% |
| (2) Decibel level of music delivered and/or use of volume controls to limit decibels. | (32) 23% | (107) 77% |
| B.4: Intervention Materials Specify music and/or non-music materials. | ||
| (1) Music materials (n=187) | (64) 34% | (123) 66% |
| (2) Non-music materials (n=76)g | (26) 34% | (50) 66% |
| B.5: Intervention Strategies (n=187) Describe music-based intervention strategies under investigation (e.g., music listening, songwriting, improvisation, rhythmic auditory stimulation). |
(187) 100% | (0) 0% |
|
C: Intervention Delivery Schedule (n=187) Report number of sessions, session duration, and session frequency. | ||
| (1) Number of Sessions | (160) 86% | (27) 14% |
| (2) Session Duration | (152) 81% | (35) 19% |
| (3) Session Frequency | (166) 89% | (21) 11% |
| D: Interventionist (n=187) | ||
| (1) Specify interventionist qualifications and/or credentials. | (78) 42% | (109) 58% |
| (2) Specify how many interventionists deliver study conditions. | (68) 32% | (119) 64% |
|
E: Treatment Fidelity (n=187) Describe strategies used to ensure that treatment and/or control conditions were delivered as intended (e.g., interventionist training, manualized protocols, and intervention monitoring). |
(38) 20% | (149) 80% |
|
F: Setting (n=187) Describe where the intervention was delivered (i.e., location, privacy level, ambient sound). | ||
| (1) Location | (90) 48% | (97) 52% |
| (2) Privacy level | (34) 18% | (153) 82% |
| (3) Ambient sound | (22) 12% | (165) 88% |
|
G: Unit of Delivery (n=187) Specify whether interventions were delivered to individuals or groups of individuals, including group size. |
(171) 91% | (16) 9% |
Note: Reporting table used with permission. Robb SL, Burns DS, & Carpenter JS. (2011). Reporting guidelines for music-based interventions. Journal of Health Psychology, 16(2), 342-352.
Several studies (n=4) lacked enough information to determine if authors used published music; these were coded as ‘no’ not reported.
The number of studies across “published music” and “improvised or original music” exceeds total studies reviewed (n=187) because some studies (n=31) used both published music and improvised/original music, with additional studies (n=8) captured across both areas due to poor reporting.
Several studies (n=8) lacked enough information to determine if authors used improvised or original music; these were coded as ‘no’ not reported.
One study lacked enough information to determine if authors used published music and was coded as ‘no’ not reported.
The number of studies across “live” and “recorded” exceeds total studies reviewed (n=187) because some studies (n=25) used both live and recorded music, with additional studies (n=8) captured across both areas due to poor reporting.
Several studies (n=7) lacked enough information to determine if authors used improvised or original music; these were coded as ‘no’ not reported.
Applies only to studies using non-music materials.
Reporting for Intervention Theory/Rationale was poor, with about half providing a theoretical framework or rationale that guided the selection of music and/or music-based experiences, and informed the hypothesized relationship of the specified music intervention to the outcome of interest.
Intervention Content reporting, which is comprised of five sub-categories, was strong for two areas including person selecting the music (89%), and music intervention strategies under investigation (100%). Overall reporting quality for the music delivery method subcategory, which has four additional sub-components (two for live music and two for recorded music), was moderate. For live music, reporting was strong for reporting the person who delivered the music (83%) and moderate for size of the performance group (62%). For recorded music, reporting was moderate for placement of playback equipment and/or the use of headphone versus speakers (65%), but poor for specifying decibel level (i.e., volume) of music delivered or the use of volume controls (23%). Finally, reporting quality was poor for two subcategories, music and intervention materials. For music, very few studies provided a reference for sound recordings or sheet music (15%), and for those studies that used improvised or original music, only 53% described the music’s compositional features such as form, tempo, harmonic structure, or instrumentation. For intervention materials, only 34% of studies that used music materials as part of the intervention (e.g., playback equipment, musical instruments) provided specific information about those materials, such as manufacturer, model, or type. Similarly, only 34% of studies provided detailed information about non-music materials (e.g., scarves).
Intervention Delivery Schedule is comprised of three areas including number of sessions, session duration, and session frequency. Reporting was strong for number of sessions (86%), session duration (81%), and session frequency (89%).
Reporting for Interventionist is comprised of two areas and both were poor. Of the studies reviewed, only 42% specified the interventionists’ qualifications and/or credentials, and only 36% reported how many interventionists delivered study conditions.
Reporting for Treatment Fidelity was poor, with only 20% of studies describing strategies used to ensure that intervention conditions were delivered as intended across participants and interventionists.
Setting is comprised of three areas related to the treatment setting (i.e., location) and sound environment (i.e., privacy level, ambient sound) in the treatment location. Reporting was poor across all three areas, with few studies reporting the intervention location (48%), privacy level (18%), or ambient sound (12%).
Reporting for Unit of Delivery was strong, with 91% of studies indicating whether the intervention was delivered to individuals or groups of individuals.
Publishing authors and journal characteristics
To determine authors’ professional backgrounds, coders looked at credentials, author information, and biographical entries. Degree and affiliation alone were not considered adequate given increased interprofessional staffing in university and healthcare institutions. For half of the studies (n=96, 51%), we were unable to identify the professional background of at least one contributing author. For articles where at least one author’s professional background could be identified (total number of articles = 91; total number of authors = 181), the following professions were represented: music therapy (n=54), nursing (n=52), medicine (n=48), and other (n=27). Professional backgrounds captured as ‘other’ included twelve different professions such as statistics, psychology, and occupational therapy.
Studies were published across 121 different journals, with a majority of identified journals publishing only one experimental or quasi-experimental music intervention study over the 5-year review period (n=99, 82%). Journals with the highest number of publications during the review period included the Journal of Music Therapy (n=14, 12%), Journal of Clinical Nursing (n=11, 9%), Music and Medicine (n=8, 7%), The Arts in Psychotherapy (n=7, 6%), and Complementary Therapies in Medicine (n=6, 5%).
Patient populations studied and corresponding outcomes
Based on patient population descriptions provided by publishing authors, we grouped studies into fifteen categories, and listed the most frequently studied outcomes for each population (Table 2). The four most frequently studied populations included surgical (n=32; 17%), Alzheimer’s/dementia (n=26; 14%), acute mental health (n=21, 11%), and cancer (n=18, 10%). In Table 2, we also list the most frequently examined outcomes for each patient population (i.e., measured in ≥ three studies; exception emergency room and tinnitus where criteria is ≥ two studies). To capture variability, we also report the number of studies where investigators measured an outcome “other” than those most frequently reported.
Table 2.
Populations studied and corresponding outcomes
| Patient Population | (n) % | Corresponding Outcomes (most frequently cited)a |
(n) Valid % |
|---|---|---|---|
|
| |||
| Surgical | (32) 17% | Anxiety | (22) 69% |
| Pain | (14) 44% | ||
| Vitalsb | (9) 28% | ||
| Sedation | (6)19% | ||
| Depressive Symptoms | (4) 13% | ||
| Satisfaction | (4) 13% | ||
| Stress | (4) 13% | ||
| Relaxation | (3) 9% | ||
| Otherc | (11) 34% | ||
|
| |||
| Alzheimer’s/Dementia | (26) 14% | Agitation | (11) 42% |
| Emotional State/Mood | (6) 23% | ||
| Quality of Life/Well-being | (6) 23% | ||
| Depressive Symptoms | (5) 19% | ||
| Cognitive Function | (5) 19% | ||
| Behavior State | (5) 19% | ||
| Anxiety | (4) 15% | ||
| Participation | (3) 12% | ||
| Communication | (3) 12% | ||
| Otherc | (9) 35% | ||
|
| |||
| Acute Mental Health | (21) 11% | Depressive Symptoms | (7) 33% |
| Other Disorder-Specific Symptoms | (4) 19% | ||
| Mood | (3) 14% | ||
| Anxiety | (3) 14% | ||
| Otherc | (16) 76% | ||
|
| |||
| Cancer | (18) 10% | Pain | (10) 56% |
| Anxiety | (9) 50% | ||
| Quality of Life/Well-being | (5) 28% | ||
| Vitalsb | (4) 22% | ||
| Relaxation | (3) 17% | ||
| Otherc | (17) 89% | ||
|
| |||
| Disease/Symptom Managementd | (13) 7% | Pain | (6) 46% |
| Anxiety | (5) 38% | ||
| Quality of Life/Well-being | (4) 31% | ||
| Vitalsb | (4) 31% | ||
| Depressive Symptoms | (3) 23% | ||
| Otherc | (9) 69% | ||
|
| |||
| Infants/NICU/PICU | (11) 6% | Vitalsb | (5) 45% |
| Behavioral State/Distress | (5) 45% | ||
| Otherc | (6) 55% | ||
|
| |||
| Brain/Spinal Cord & Neurological Disorders | (11) 6% | Mobility | (4) 36% |
| Quality of Life/Well-being | (4) 36% | ||
| Voice Quality | (3) 27% | ||
| Cognitive Function | (3) 27% | ||
| Otherc | (8) 73% | ||
|
| |||
| Heart, Lung, & Kidney | (10) 5% | Pain | (4) 40% |
| Anxiety | (3) 30% | ||
| Dyspnea | (3) 30% | ||
| Otherc | (10) 100% | ||
|
| |||
| Intensive Care Unit | (10) 5% | Sedation | (5) 60% |
| Anxiety | (4) 60% | ||
| Vitalsb | (3) 40% | ||
| Otherc | (7) 70% | ||
|
| |||
| Pregnancy/Labor & Delivery | (10) 5% | Pain | (6) 60% |
| Anxiety | (5) 50% | ||
| Otherc | (5) 50% | ||
|
| |||
| Acute Care/Hospitalization | (7) 4% | Pain | (5) 71% |
| Vitalsb | (4) 57% | ||
| Anxiety | (4) 57% | ||
| Mood | (3) 43% | ||
| Otherc | (4) 57% | ||
|
| |||
| Older Adults/Long-Term Care | (7) 4% | Depressive Symptoms | (4) 57% |
| Otherc | (7) 100% | ||
|
| |||
| Diagnosticse | (6) 3% | Pain | (5) 83% |
| Anxiety | (4) 66% | ||
| Satisfaction | (3) 50% | ||
| Otherc | (2) 33% | ||
|
| |||
| Emergency Room | (3) 2% | Anxiety | (2) 67% |
| Pain | (2) 67% | ||
| Otherc | (2) 67% | ||
|
| |||
| Tinnitus | (2) 1% | Tinnitus Severity | (2) 100% |
| Otherc | (2) 100% | ||
Specific outcomes are listed when measured in ≥ 3 studies (exception is Emergency Room and Tinnitus where we list outcomes reported in ≥ 2 studies).
Vitals includes heart rate, blood pressure, respiration rate, oxygen saturation.
Other refers to the number of studies where investigators measured an outcome other than those listed in the table.
Patients’ care focused on disease/symptom management (e.g., fibromyalgia, diabetes, chronic pain).
Patients undergoing diagnostic procedures (e.g., colonoscopy, needle electromyography).
Music intervention terminology
Across the 187 reviewed articles, authors used 51 different music intervention terms in the introduction and review of literature (Table 3). Of the 51 terms, 38 appeared in only one article, eight terms across two articles, and one term across three articles. The most frequently used terms included music therapy (n=129), music intervention (n=50), music listening (n=19), and music medicine (n=9). A majority of the time, authors did not provide a definition for terms (n=152, 58%). In Table 3, we further categorized the 51 terms into three levels of specificity, including broad or general terms (n=19), terms with increased specificity (n=17), and terms referencing a specific technique, experience, or intervention (n=15). Publishing authors defined specific terms more frequently than general terms (82% vs. 39%).
Table 3.
Music intervention terminology specificity and definition frequency
| Terminology/Specificity (General to Specific) |
Frequency (n) |
Definition Provided (n) Valid % |
|
|---|---|---|---|
| Yes | No | ||
| GENERAL (n= 19 Terms) | |||
| Music Therapy | 129 | (54) 42% | (75) 58% |
| Music Intervention | 50 | (10) 20% | (40) 80% |
| Music Listening | 19 | (7) 37% | (12) 63% |
| Music Medicine | 9 | (6) 67% | (3) 33% |
| Music Activity | 2 | (2) 100% | – |
| Music Program | 2 | – | (2) 100% |
| Therapeutic Music | 2 | – | (2) 100% |
| Individualized Music | 1 | (1) 100% | – |
| Music as Therapy | 1 | – | (1) 100% |
| Music as a Nursing Intervention | 1 | – | (1) 100% |
| Music as a Therapeutic Modality | 1 | (1) 100% | – |
| Integrative Therapy | 1 | (1) 100% | – |
| Group Music Activities | 1 | (1) 100% | – |
| Auditory Intervention | 1 | (1) 100% | |
| Oriental Medicine Music Therapy | 1 | (1) 100% | – |
| Non-Pharmacological/Complementary | 1 | (1) 100% | – |
| Neuro-Music Therapy | 1 | – | (1) 100% |
| Music Supported Therapy | 1 | (1) 100% | – |
| Music Supported Music Therapy | 1 | (1) 100% | – |
| SUBTOTAL | 225 | (87) 39% | (138) 61% |
| INCREASED SPECIFICITY (n=17 Terms) | |||
| Music Relaxation | 2 | (1) 50% | (1) 50% |
| Relaxation and Music | 2 | – | (2) 100% |
| Sedative Music | 2 | (2) 100% | – |
| Cognitive Behavioral Music Therapy | 2 | (1) 50% | (1) 50% |
| Ambient Therapy | 2 | (1) 50% | (1) 50% |
| Music Analgesia | 1 | (1) 100% | – |
| Imagery with Music | 1 | (1) 100% | – |
| Contingent Music | 1 | – | (1) 100% |
| Audio-analgesia | 1 | – | (1) 100% |
| Passive Music Listening | 1 | – | (1) 100% |
| Slow Breathing | 1 | (1) 100% | – |
| Sleep Induced Music | 1 | (1) 100% | – |
| Singing Training | 1 | – | (1) 100% |
| Recreational Music Therapy | 1 | – | (1) 100% |
| Purpose-Designed Musical Compositions | 1 | – | (1) 100% |
| Neurologic Music Therapy | 1 | (1) 100% | – |
| Preferred Music Listening | 1 | (1) 100% | – |
| SUB-TOTAL | 22 | (11) 50% | (11) 50% |
| SPECIFIC TECHNIQUE or INTERVENTION (n=15 Terms) | |||
| Rhythmic Auditory Stimulation | 3 | (1) 33% | (2) 67% |
| Modified Melodic Intonation Therapy | 1 | (1) 100% | – |
| Melodic Intonation Therapy | 1 | (1) 100% | – |
| Heidelberg Model of Music Therapy for Tinnitus | 1 | (1) 100% | – |
| Guided Imagery with Theta Music | 1 | (1) 100% | – |
| Binaural Beat | 1 | (1) 100% | – |
| Jacquez-Dalcroze Eurhythmics | 1 | (1) 100% | – |
| Therapeutic Music Video Intervention | 1 | (1) 100% | – |
| Tailor-Made Notched Music Training | 1 | (1) 100% | – |
| Ronnie Gardiner Rhythm and Music Method | 1 | (1) 100% | – |
| Music Reminiscence Therapy | 1 | (1) 100% | – |
| Patterned Sensory Enhancement | 1 | (1) 100% | – |
| Neuromonics | 1 | (1) 100% | – |
| YUBA Method | 1 | – | (1) 100% |
| Music Therapeutic Caregiving | 1 | (1) 100% | – |
| SUB-TOTAL | 17 | (14) 82% | (3) 18% |
| TOTAL: TERMS (n=51) | 264 | (112) 42% | (152) 58% |
Interventionist education, professional background, and training
In Table 4, we summarize interventionist education, professional background, and training. A majority of authors (n=166, 89%) did not specify interventionist education level (i.e., bachelors, masters, doctorate), and 58% (n=108) provided no information on professional background. Of those providing information on professional background, a majority of interventionists were credentialed music therapists (n=61, 33%), followed by registered nurses (n=12, 6%). Five articles indicated the interventionist had specialized training, but only one offered information on degree level, and none provided information on professional background.
Table 4.
Interventionist education, professional background, and training
| Interventionist Education, Professional Background, Training (n=187 studies) |
(n)a Valid % | Degree Level (n) Valid % |
|||
|---|---|---|---|---|---|
| Bachelors | Masters | Doctorate | Not Specified | ||
|
Professional Background (Requires Degree & Credentialing) | |||||
| Credentialed Music Therapist (MT) | (61) 33% | (3) 5% | (7) 12% | (8)13% | (43) 70% |
| Registered Nurse (RN) | (12) 6% | – | (1) 8% | – | (11) 92% |
| Counselor | (1) < 1% | – | – | – | (1) 100% |
| Neuropsychologist | (1) < 1% | – | – | – | (1) 100% |
| Psychiatrist | (1) < 1% | – | – | – | (1) 100% |
| Psychotherapist | (1) < 1% | – | – | – | (1) 100% |
| Occupational Therapist | (1) < 1% | – | – | – | (1) 100% |
| Certificates | |||||
| NMT Certificateb | (2) 1% | – | – | – | (2) 100% |
| Certified Music Practitioner | (1) < 1% | (1) 100% | – | – | – |
| Certified RGRM Facilitator | (1) < 1% | – | – | – | (1) 100% |
| Other | |||||
| Music Therapeutic Caregiving Training | (1) < 1% | – | – | – | (1) 100% |
| Sonas Training | (1) < 1% | – | – | – | (1) 100% |
| Professional Musician | (1) < 1% | – | – | – | (1) 100% |
RGRM= Ronnie Gardiner Rhythm and Music; NMT= Neurologic Music Therapy
Three studies had interprofessional intervention delivery.
Both professionals were also Credentialed Music Therapists.
Music intervention content and interventionist professional background
In Table 5, we summarize the number (single component vs. multiple components) and type of music experiences that comprised the music interventions in this review. We defined single component interventions as interventions comprised of one music experience, and multiple component interventions as those comprised of two or more music experiences. Because some studies had multiple music intervention arms, the total number of interventions (n=201) exceed the number of articles (n=187).
Table 5.
Music intervention content and interventionist professional background
| Music Experience Intervention Components (Definition) (Total Interventions n=201)a |
(n) Valid % | Interventionist Professional Background | |||
|---|---|---|---|---|---|
| Not Specified | Credentialed Music Therapist | Registered Nurse | Otherb | ||
|
| |||||
| Single Component Interventions (n=136) | |||||
|
| |||||
|
Listening Participants listen to live or recorded music. |
(104) 76%b | (75) 72% | (14)13% | (12) 12% | (4) 4% |
| Live Music | (13) 12% | (5) 38% | (6) 46% | – | (2) 15% |
| Recorded Music | (91) 88%b | (70) 77% | (8) 9% | (12) 13% | (2) 2% |
|
| |||||
|
Music-Assisted Relaxation Music used to structure relaxation exercises (e.g., progressive muscle relaxation, autogenic). |
(7) 5% | (5) 71% | (2) 29% | – | – |
|
| |||||
|
Re-Creating Music by Singing/Playing Instruments Participants sing and/or play pre-composed songs/music. |
(3) 2% | (1) 33% | (1) 33% | (1) 33% | |
|
| |||||
|
Improvisation Participants or interventionist creates music in the moment. |
(3) 2% | – | (3) 100% | – | – |
|
| |||||
|
Lyric Analysis Participants discuss meaning of song lyrics. |
(4) 3% | – | (3)75% | – | (1) 25% |
|
| |||||
|
Songwriting Participants engage in lyric writing and/or musical composition. |
(3) 2% | (1) 33% | (2) 67% | – | – |
|
| |||||
|
Imagery Music used to support or facilitate visual imagery. |
(1) <1% | (1) 100% | |||
|
| |||||
|
Movement Music used to structure, facilitate, or encourage movement. |
(2) 1% | (1) 50% | (1) 50% | – | – |
|
| |||||
|
Breathing Entrainment Rhythmic/temporal qualities of music structure rate of breathing; synchronization between breathing/rate of music. |
(1) <1% | (1) 100% | – | – | – |
|
| |||||
|
Instrument/Vocal Play Play that combines non-music play materials with singing and/or playing instruments (e.g., children’s finger puppet action songs) |
(1) <1% | – | (1) 100% | – | – |
|
| |||||
| Other | |||||
|
| |||||
| Music Recreation | (3) 2% | – | (3) 100% | – | – |
|
| |||||
| Pacifier Activated Lullaby/Music | (2) 1% | (1) 50% | (1) 50% | – | – |
|
| |||||
| Therapeutic Singing | (1) <1% | (1) 100% | – | – | – |
|
| |||||
| Modified Melodic Intonation Therapy | (1) <1% | – | (1) 100% | – | – |
|
| |||||
| Multiple Component Interventions (n=65) | |||||
|
| |||||
|
Re-Creating Music by Singing/Playing Instruments Participants sing and/or play pre-composed songs/music. |
(38) 58%b | (11) 29% | (24) 63% | (1) 3% | (4) 11% |
|
| |||||
|
Listening Participants listen to live or recorded music. |
(35) 54%b | (12) 34% | (21) 60% | (2) 6% | (2) 6% |
|
| |||||
|
Improvisation Participants or interventionist creates music in the moment. |
(23) 35% | (5) 22% | (18) 78% | – | – |
|
| |||||
|
Movement Music used to structure, facilitate, or encourage movement. |
(21) 32%b | (7) 33% | (12) 57% | (1) 5% | (3) 14% |
|
| |||||
|
Music-Assisted Relaxation Music used to structure relaxation exercises (e.g., progressive muscle relaxation, autogenic). |
(16) 25%b | (2)13% | (12) 75% | – | (3) 19% |
|
| |||||
|
Imagery Music used to support or facilitate visual imagery. |
(13) 20% | (3) 23% | (8) 61% | (1) 8% | (1) 8% |
|
| |||||
|
Instrument/Vocal Play Play that combines non-music play materials with singing and/or playing instruments (e.g., children’s finger puppet action songs) |
(12) 18% | (6) 50% | (6) 50% | – | – |
|
| |||||
|
Songwriting Participants engage in lyric writing and/or musical composition. |
(12) 18% | (1) 8% | (11) 92% | – | – |
|
| |||||
|
Lyric Analysis Participants discuss meaning of song lyrics. |
(8) 12% | (1) 12% | (6) 76% | – | (1) 12% |
|
| |||||
|
Breathing Entrainment Rhythmic/temporal qualities of music structure rate of breathing; synchronization between breathing/rate of music. |
(7) 11% | (1) 14% | (6) 86% | – | – |
|
| |||||
| Other | |||||
|
| |||||
| Music Reminiscence or Life Review | (7) 11% | (3) 43% | (4) 57% | ||
|
| |||||
| Vocal Breathing Exercises, Therapeutic Singing, or Singing Instruction | (5) 8% | (2) 40% | (2) 40% | (1) 20% | |
|
| |||||
| Song Recording or Music Video Creation | (3) 5% | (3) 100% | |||
|
| |||||
| Music Attention Control Training | (2) 3%b | (2) 100% | (1) 50% | ||
|
| |||||
| Music Assisted Counseling | (1) 2% | (1) 100% | |||
|
| |||||
| Vibroacoustic Stimulation | (1) 2% | (1) 100% | |||
|
| |||||
| Music Recreation | (1) 2% | (1) 100% | |||
Several studies had more than one music intervention arm, resulting in 201 interventions.
This intervention component was delivered by more than one interventionist from different professional backgrounds.
About two-thirds of the interventions had a single music experience component (n=136, 68%), and of those the majority (n=104, 76%) were music listening interventions that used either live (12%) or recorded music (88%). The remaining interventions (n=65, 32%) had multiple music experience components with the majority having two (n=22, 34%) or three (n=28, 43%) components, followed by four (n=6, 9%), five (n=5, 7%), six (n=2, 3%), eight (n=1, 2%) and ten (n=1, 2%) music experience components. Table 5 provides a detailed list of music experiences used in single and multiple component interventions.
Table 5 also provides information about the professional background of interventionists delivering each type of music intervention experience. For those studies reporting interventionist qualifications for single component interventions, registered nurses delivered only recorded music listening interventions and credentialed music therapists delivered a majority of live music listening interventions, as well as interventions that used other music experiences such as improvisation, lyric analysis, songwriting, or movement (see Table 5). Credentialed music therapists also delivered most multiple component interventions. Three studies used interprofessional teams to deliver interventions, one was a single component intervention and two were multicomponent.
Discussion
Overall, reporting quality for music intervention studies was poor. Less than half of the reviewed studies provided information for four of the seven reporting checklist components including intervention theory, interventionist background/qualifications, treatment fidelity, and setting. In addition, we found mixed levels of reporting for intervention content, with less than half of reviewed studies providing information about the music, decibel level/use of volume controls, or materials. The absence of information across these areas is concerning because it lessens the scientific rigor, impact, and clinical relevance of the resulting work. We focus our discussion on findings related to intervention reporting in the areas of theory, interventionist qualifications, intervention content and fidelity, followed by identified problems with terminology that inhibit clear reporting.
Theory may be considered the most important reporting variable because it drives intentional use of music that is informed by research about social, psychological, perceptual, and/or neurobiological responses to music. There needs to be a clear scientific premise for why an investigator expects the specified use of music to influence the outcome of interest. Yet, less than half of the reviewed studies included a theoretical framework or offered a scientific rationale. Identifying and measuring not only outcomes, but also the proposed mechanisms of action allow investigators to move beyond basic questions about efficacy, and begin answering questions about how, why, and for whom an intervention works.[9, 20, 28–30]
Recent Cochrane reviews examining music interventions for a variety of client and patient populations have raised awareness about important differences in intervention content, complexity, and delivery that are directly related to the education, training, and professional background of the interventionist.[2, 3, 5, 8, 10, 31] Less than half of reviewed articles provided information about interventionist qualifications, but of those that did provide this information, credentialed music therapists and registered nurses delivered a majority of interventions. Consistent with each professions’ training and scope of practice, music therapists used a wide range of music experiences that included both single and multiple-component interventions, while a majority of nurse delivered interventions used recorded music listening as a single-component intervention.
The professional background and training of music therapists and other healthcare professionals (e.g., nursing, medicine, physical therapy) are different, and will influence their understanding about the nuances of music that influence clinical outcomes and their skill in using music as a therapeutic modality. As such, it is understandable and appropriate that intervention content would vary based on professional background. Equally important is the knowledge that nurses and other healthcare providers contribute through identification and understanding of health problems that may be amenable to music interventions. An important aspect of research translation and the development of targeted interventions is determining the type of intervention (content and complexity) that provides the greatest benefit, based on patient-specific factors, and the level of skill (interventionist qualifications) required to deliver that intervention. Investigators have begun to examine differential benefits of music interventions based on professional background and content,[3, 8, 21] but improved and consistent reporting are needed to conduct more meaningful and nuanced subgroup analyses to better inform selection and delivery of music interventions.
Despite music being the primary intervention modality, few authors provided detailed information about the music. This finding is consistent with prior reviews, and severely limits investigators ability to identify characteristics of music responsible for change and conduct quality cross-study comparisons.[2, 3, 8, 17] We know that compositional features of the music itself are often responsible for outcomes. For example, the use of rhythm, tempo, melodic contour, and/or harmonic structure to improve gait parameters[8, 32, 33] regulate breathing[34–36] regulate emotion, [37] elicit imagery[38–40] or influence other physiological or psychosocial responses.[33] We also know that relational aspects of interventions, such as group music making or the use of improvisation, are important features that also contribute to positive health outcomes. [41–43] Providing detailed descriptions of the music and music experiences used is essential if we are to examine and understand potential mechanisms of action. This is particularly relevant for the large number of single component intervention studies we identified where recorded music listening was the primary intervention component in managing acute pain and anxiety. Despite the large number of studies published, evidence to support its integration into healthcare remains equivocal, and is likely due to the absence of theory and detailed reporting that would enable more meaningful cross-study comparisons.
Treatment fidelity includes methodological strategies that help to ensure consistent intervention delivery over the course of a clinical trial, strengthening investigators’ ability to attribute any observed benefits to the intervention under examination [44–46]. Given the complexity of music interventions, especially multiple component interventions, it is essential that investigators specify essential elements of the intervention and implement strategies to monitor consistent delivery. Unfortunately, few of the reviewed studies included information about treatment fidelity. Improvements in fidelity will reduce random and unintended intervention variability within studies and in turn may help address inconsistent findings observed across studies [44–46].
Finally, investigators need to provide a full description of the setting where music interventions are delivered, including privacy levels (e.g., open area vs. private room) and the amount of ambient sound in the environment. Understanding the sound environment influences our ability to interpret and translate findings to the clinical practice setting. For example, the introduction of music into an already stimulating environment, as opposed to a quiet environment, may be an important factor that contributes to patient outcomes. For some vulnerable populations, such as those with dementia or premature infants, this also becomes a safety issue due to changes or developmental readiness to integrate sensory information [47–50].
Unique to this review was an examination of terminology used to describe music interventions. We found that publishing authors used a wide variety of terms that were frequently undefined. Although not part of our data collection, our team also noticed that at times terms were misapplied and we recommend subsequent reviews examine this variable. This is concerning because inconsistent, undefined, and misapplied terms impede accurate and consistent reporting, as well as meaningful interpretation of study findings. Professional background and training likely influence publishing authors’ use, understanding, and interpretation of music terminology, and their assumptions about whether selected terms will be understood by an interdisciplinary readership. We also found that a large number of journals are publishing music intervention research, but on an infrequent basis. Journals that publish one article a year may be unfamiliar with music reporting guidelines and have diminished access to qualified reviewers, representing additional factors that likely contribute to inconsistencies in terminology.
Consistent with previous reviews, we found that the term “music therapy” or “music therapy intervention” was often misapplied and used as a global reference for all music interventions.[3, 21] However, the term only communicates information about the professional background and training of the individual who delivered the intervention, in this case a credentialed music therapist. Because “music therapy” is a profession-specific term, as is nursing, physical therapy, or speech therapy, it should not be used to describe interventions delivered by healthcare professionals who do not hold music therapy degree training and/or credentialing. This does not mean that music interventions delivered by other healthcare professionals do not have therapeutic benefit or value; rather the term is specific to one profession and only communicates a level of training and defined scope of practice. Even when used accurately, the term “music therapy” can be problematic because it is a global term that provides limited information about the actual intervention. Establishing standard terms and definitions will improve interprofessional communication, but will require a collaborative effort.
Discussions among our interprofessional team members revealed how our own professional background (nursing or music therapy) influenced our understanding and interpretation of study content as we scrutinized and discussed article content throughout the review process. Our interprofessional team represents a microcosm of the primary professions who are conducting music intervention research, and our experiences suggest that clarity of terminology will lessen confusion and improve interprofessional communication.
As such, we recommend that in addition to using a global term, such as music intervention, that publishing authors also use and define terms that are more descriptive of intervention content such as “recorded music listening program” or “group singing intervention” followed by details about the professional background and training of the person delivering the intervention. Authors will also want to define music terms that may be unfamiliar to those with limited musical training. Establishing standard terms and definitions will improve interprofessional communication, delineation of music intervention content and delivery across professions, and translation of findings to practice.
Strengths of our study included use of an interprofessional team, an established checklist to assess reporting quality, and multiple, independent reviewers to increase validity and diminish risk of bias. Limitations included exclusion of non-English studies and strategies to identify articles published in non-indexed journals, which increased our risk for bias.
Conclusions
Findings from this systematic review reveal significant problems with reporting quality for music intervention research in healthcare that directly impedes meaningful cross-study comparisons, interpretation, replication, and generalization of findings. In addition, inconsistent and misapplied terminology represent a barrier to interprofessional communication and meaningful translation of findings to direct patient care. Problems with reporting quality and terminology may be due in part to several systemic challenges including differences in the professional background of investigators engaged in music intervention research, the large number and variety of publishing journals, and limited awareness and uptake of music intervention reporting guidelines. To improve reporting quality, we recommend that authors, journal editors, and reviewers use the Reporting Guidelines for Music-based Interventions to inform study design, dissemination, and peer review. We also recommend an interprofessional consensus meeting to develop and adopt shared language that accurately reflects the emerging continuum of music interventions, which will ultimately improve communication, collaboration, and meaningful uptake of findings to improve patient care.
Highlights.
Publication of music intervention studies are increasing, as are concerns about inadequate intervention reporting and inconsistent terminology.
Less than 50% of published music intervention studies provide enough detail about the music intervention, inhibiting meaningful interpretation and cross-study comparisons.
Credentialed music therapists and registered nurses deliver most music interventions, with clear differences in both content and delivery.
Terminology used to label and describe music interventions are varied, inconsistent, and at times misapplied creating barriers to interprofessional communication.
Increased awareness and use of the Checklist for Reporting Music-Based Interventions are recommended to improve reporting quality, scientific rigor, and clinical relevance of music intervention research.
Acknowledgments
This study was funded in part by the first author’s grant funding from the NIH, National Institute of Nursing Research (R01 NR015789).
Appendix A. Full Electronic Search Strategy
-
#1
music/all subheadings
-
#2
music therapy/all subheadings
-
#3
#1 AND #2
-
#4
intervention/all subheadings
-
#5
interventions/all subheadings
-
#6
#4 OR #5
-
#7
#3 AND #6
-
#8
#7 with following limits applied: English Only; Humans Only; Clinical Trials, All; Comparative Study; Controlled Clinical Trial; Evaluation Studies; Journal Articles; Observational Study; Randomized Controlled Trial.
Appendix B. Data extraction tool and definitions
DATA EXTRACTION TOOL: Music Intervention Research in Healthcare (See Corresponding Definitions Page)
TEAM NUMBER/MEMBERS: __________________________________
ARTICLE: __________________________________________________
| Author/Journal Information | CIRCLE | Page #: | ||
|---|---|---|---|---|
| Country of Origin | Circle all that apply: 1) United States; 2) Canada 3) Europe 4) Australia 5) South Korea 6) Japan 7) Indonesia 8) Other Specify: |
|||
| Authors’ Profession: | Circle all that apply: 1) music therapy 2) nursing 3) psychology/psychiatry 4) medicine 5) other |
|||
| Study Design | CIRCLE ONE | |||
| Study Design |
Experimental Designs (more than one group; randomization) 1) 2 groups, randomized trial (randomization; control group; pre/post-test) 2) 2 groups, post-test only (randomization; control group; posttest only) 3) Randomized, Wait-list control Group 4) Factorial design 5) Cross over design 6) Other Quasi-Experimental Designs Designs without Control Groups: 1) One-group, posttest only 2) One-group pretest/posttest Designs that Use a Control Group, but no Pretest 1) Post-test only, non-equivalent groups 2) Case Control Design Designs that use control groups & pretests 1) Untreated control group design w/dependent pre/posttest samples 2) Matching through cohort controls Interrupted time-series designs 1) Single group time series design 2) Nonequivalent control group time series design |
|||
|
Outcome of Interest/Corresponding Measure Example: Outcome of Interest: Anxiety Corresponding Measure: STAI |
Outcomes (list) | Measures (list) | ||
| Terminology (Terms/Definitions) | CIRCLE/LIST | Page #: | ||
| Did the authors use any of the following terms? | Circle all that apply: 1) Music Therapy 2) Music Medicine 3) Music Intervention 4) Other (please specify) |
|||
| Did the authors define these terms? Indicate page number where term is defined | Yes | No | ||
| Patient Population/Clinical Situation | LIST | Page #: | ||
| List all terms used to describe the patient population & clinical situation being studied. Examples: Cancer Patients Undergoing Surgery Cancer Patients/Chemotherapy Surgical Patients/Pre/Post-Op Alzheimer/Dementia Patients/Gait training |
||||
| Music-based Intervention Reporting Criteria | CIRCLE/LIST | Page #: | ||
|
A: Rationale for Music Selection/Intervention Theory Provided a rationale for the music selected; specified how qualities and delivery of the music are expected to impact targeted outcomes. |
Yes | No | ||
|
B: Intervention Content Provided precise details of the music intervention and, when applicable, descriptions of procedures for tailoring interventions to individual participants. Please code the following 5 areas: | ||||
|
B.1: Person Selecting the Music Specified who selected the music. |
Yes |
No |
||
| If yes, circle one: (1) pre-selected by investigator, (2) participant selected from limited set, (3) participant selected from own collection, (4) tailored based on patient assessment. (5) other | ||||
| B.2: Music | ||||
| When using published music, provided reference for sheet music or sound recording. | Yes | No | ||
| When using improvised or original music, described the music’s overall structure (i.e., form, elements, instruments, etc). | Yes | No | ||
|
B.3. Music Delivery Method (Live or Recorded) | ||||
| When using live music: | ||||
| (1) specified who delivered the music | Yes | No | ||
| (2) specified the size of the performance group (e.g., interventionist only, interventionist and participant) | Yes | No | ||
| When using recorded music: | ||||
| (1) specified placement of playback equipment and/or the use of headphones vs. speakers, | Yes | No | ||
| (2) Specified decibel level of music delivered and/or use of volume controls to limit decibels. | Yes | No | ||
| B.4: Intervention Materials | ||||
| Specified music material | Yes | No | ||
| Specified non-music materials | Yes | No | ||
|
B.5: Intervention Strategies Described music-based intervention strategies under investigation. |
Yes If yes, circle all that apply: 1) Breathing Entrainment 2) Imagery 3) Music-assisted relaxation 4) Songwriting 5) Lyric Analysis 6) Movement 7) Re-creating music by singing/playing instrument 8) Improvisation 9) Instrument/vocal play 10) Listening 11) Other (please specify) |
No | ||
| C: Intervention Delivery Schedule | ||||
| Reported number of sessions, | Yes | No | ||
| Reported session duration, | Yes | No | ||
| Reported session frequency | Yes | No | ||
| D: Interventionist | ||||
| Specified qualifications (i.e., degree) | Yes Please list: |
No | ||
| Specified credentials (i.e., certifications) | Yes Please list: |
No | ||
| Specified how many interventionists delivered study conditions | Yes Specify #: |
No | ||
|
E: Treatment Fidelity Described any strategies used to ensure that treatment and/or control conditions were delivered as intended (e.g., interventionist training, manualized protocols, and intervention monitoring) |
Yes | No | ||
| F: Setting | ||||
| Specified where intervention was delivered (i.e., location) | Yes List location: |
No | ||
| Privacy level (e.g., private room, open treatment area) | Yes | No | ||
| Ambient Sound (e.g., noise level in the environment) | Yes | No | ||
| G: Unit of Delivery | ||||
| Specified whether interventions were delivered to individuals or groups of individuals. | Yes If yes, circle one: Individual Group |
Yes | ||
DEFINITIONS: Data Extraction Tool
Author/Journal Information
Country of Origin: Where did the study take place? The setting (or location) of the study should be described in the article. You can also look at the affiliation(s) of the contributing authors to determine where the study was conducted.
Authors’ Profession: On the title page, each author will have his/her credentials listed. Their credentials will be a better indicator of their professional background than their university or hospital affiliation. Some articles will provide author biographies.
Study Design
Study Design: See hand-out for overview of experimental/quasi experimental study designs.
-
Outcome(s) of Interest: What were the primary clinical outcomes of interest? There will often be more than one outcome. Other variables that might be measured (but you do not need to list) are baseline characteristics, mediators, or moderators.
A mediator is a variable that accounts for how effects will occur by accounting for the relationship between the independent (e.g., intervention) and dependent (i.e., outcome) variables.
A moderator is a variable that that accounts for the strength of the relationship between the independent (e.g., intervention) and dependent (i.e., outcome) variables.
Corresponding Measure: Provide the name of the instrument used to measure each outcome of interest.
Terminology
Look for the use of terms like “music therapy”, “music medicine”, or “music intervention” that may be used to globally describe the intervention. Circle or list terms, indicate if authors defined terms, and log the page number where you found this information. Record other terms that authors use to describe the intervention, indicate if a definition was provided and log the page number where you found this information.
Patient Population/Clinical Situation
List terms used to describe the patient population and clinical situation being studied. For example, a study that is using music to reduce anxiety in cancer patients pre-operatively – you would list CANCER PATIENTS; SURGICAL; PRE-OP
Music-Based Intervention Reporting
Rationale for Music Selection/Intervention Theory: Do the authors explain how/why they would expect music to address the clinical problem of interest? Do the authors specify an underlying theory for the intervention? This could be an explicit statement of a theory (e.g., Social Learning Theory) or it could be a summary of research findings supporting the relationship of the music to the outcomes of interest.
- Person Selecting the Music
- Pre-selected by Investigator: Selected by investigator and standardized across patients.
- Participant-Selected from Limited Set: Participants chose from standard set of music selected by investigator.
- Participant Selected from Own Collection: Participants use music from their own collection.
- Tailored based on Patient Assessment: Music selected by interventionist based on participant-specific needs.
- Music (published; original; improvised):
- Published: When using pre-recorded or playing live music that has been written by someone other than the interventionist, did the author provide a list of song titles/publisher information?
- Original/Improvised: When using music composed specifically for the study, or when music was improvised as a part of the intervention, did the author describe the structure/style of the music (e.g., form, elements, tempo, harmonic structure, etc)?
- Music Delivery Method (live or recorded):
- Live music: This is music that was played/sung for the participant. Did the authors specify who performed the music (i.e., was it the interventionist or someone else)? Did the author indicate the size of the performing group (i.e., was it the interventionist alone or was it a group of instrumentalists/singers)?
- Recorded Music: This is music that was played from a recording. Did the author(s) describe the playback equipment and/or use of headphone vs. speakers? Did the authors specify the db level of the music (i.e., loudness of the sound) and/or the use of volume controls to limit db level?
- Intervention Materials:
- Specific list of musical materials: List specific music-materials used (e.g., six nylon string acoustic guitar) vs. general list (e.g., guitar).
- Specific list of non-musical materials: List specific non-music materials used (e.g., five plastic frogs) vs. a general list (e.g., toys).
- Intervention Strategies (or methods):
- Breathing Entrainment: Rhythmic/temporal qualities of music to structure rate of breathing; synchronization between breathing/rate of music
- Imagery: Music used to support visual imagery (specify if Bonny Method of Guided Imagery/Music used)
- Music-Assisted Relaxation: Music used to structure relaxation exercises (e.g., progressive muscle relaxation, autogenics)
- Songwriting: participants engage in lyric writing and/or musical composition
- Lyric Analysis: participants discuss meaning of song lyrics
- Movement: music is used to structure, facilitate, and/or encourage movement
- Re-Creating Music by Singing/Playing Instruments: participants sing and/or play pre-composed songs/music
- Improvisation: participant or interventionist creates music in the moment
- Instrument/Vocal Play: play that combines non-music play materials with singing and/or instrument play
- Listening: participants listen to music
- Intervention Delivery Schedule:
- Number of Sessions: Total number of sessions participants received
- Session Duration: How long session(s) last (e.g., 30 minutes)
- Frequency of Sessions: Frequency and timing of sessions (e.g., 2 sessions per week)
- Interventionist:
- Qualifications: Degree of individuals delivering the intervention (e.g., Bachelor’s Nursing; Bachelor’s Music Therapy, Masters Nursing, etc)
- Credentials: Credentials or certifications of individuals delivering intervention (e.g., MT-BC, CNA)
- Number of Interventionists: How many interventionists delivered study conditions?
Treatment Fidelity: Did the authors describe any strategies used to ensure that treatment and/or control conditions were delivered as intended (e.g., interventionist training, manualized protocols, intervention monitoring)?
- Setting:
- Location: Where the intervention was delivered (e.g., home, examination room, patients private room, recovery room, etc).
- Privacy Level: Privacy level of space where the intervention was delivered (e.g., open treatment area with six patient beds divided by curtains).
- Ambient Sound: Sound level of treatment environment reported as db level or in descriptive terms (e.g., quiet area, high level of ambient noise).
Unit of Delivery: Specify whether intervention was delivered to individuals or groups of individuals.
Appendix C. Reference list for reviewed studies
- 1.Abd-Elshafy SK, Khalaf GS, Abo-Kerisha MZ, Ahmed NT, Abd El-Aziz MA, Mohamed MA. Not All Sounds Have Negative Effects on Children Undergoing Cardiac Surgery. Journal of cardiothoracic and vascular anesthesia. 2015;29(5):1277–84. doi: 10.1053/j.jvca.2015.01.005. [DOI] [PubMed] [Google Scholar]
- 2.Abraham A, Drory VE. Listening to music during electromyography does not influence the examinee’s anxiety and pain levels. Muscle & Nerve. 2014;50(3):445–7. doi: 10.1002/mus.24291. [DOI] [PubMed] [Google Scholar]
- 3.Alipour Z, Eskandari N, Ahmari Tehran H, Eshagh Hossaini SK, Sangi S. Effects of music on physiological and behavioral responses of premature infants: a randomized controlled trial. Complementary Therapies In Clinical Practice. 2013;19(3):128–32. doi: 10.1016/j.ctcp.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Allred KD, Byers JF, Sole ML. The effect of music on postoperative pain and anxiety. Pain Management Nursing: Official Journal Of The American Society Of Pain Management Nurses. 2010;11(1):15–25. doi: 10.1016/j.pmn.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Amengual JL, Rojo N, Veciana de Las Heras M, Marco-Pallarés J, Grau-Sánchez J, Schneider S, et al. Sensorimotor plasticity after music-supported therapy in chronic stroke patients revealed by transcranial magnetic stimulation. Plos One. 2013;8(4):e61883. doi: 10.1371/journal.pone.0061883. -e. doi: 10.1371/journal.pone.0061883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amini E, Rafiei P, Zarei K, Gohari M, Hamidi M. Effect of lullaby and classical music on physiologic stability of hospitalized preterm infants: a randomized trial. Journal Of Neonatal-Perinatal Medicine. 2013;6(4):295–301. doi: 10.3233/NPM-1371313. [DOI] [PubMed] [Google Scholar]
- 7.Argstatter H, Grapp M, Hutter E, Plinkert PK, Bolay H-V. The effectiveness of neuro-music therapy according to the Heidelberg model compared to a single session of educational counseling as treatment for tinnitus: A controlled trial. Journal of Psychosomatic Research. 2015;78(3):285–92. doi: 10.1016/j.jpsychores.2014.08.012. [DOI] [PubMed] [Google Scholar]
- 8.Arroyo-Anlló EM, Díaz JP, Gil R. Familiar music as an enhancer of self-consciousness in patients with Alzheimer’s disease. Biomed Research International. 2013;2013:752965. doi: 10.1155/2013/752965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barry P, O’Callaghan C, Wheeler G, Grocke D. Music therapy CD creation for initial pediatric radiation therapy: a mixed methods analysis. Journal of music therapy. 2010;47(3):233–63. doi: 10.1093/jmt/47.3.233. [DOI] [PubMed] [Google Scholar]
- 10.Bauer BA, Cutshall SA, Anderson PG, Prinsen SK, Wentworth LJ, Olney TJ, et al. Effect of the combination of music and nature sounds on pain and anxiety in cardiac surgical patients: a randomized study. Alternative Therapies In Health And Medicine. 2011;17(4):16–23. [PubMed] [Google Scholar]
- 11.Bauer CL, Victorson D, Rosenbloom S, Barocas J, Silver RK. Alleviating distress during antepartum hospitalization: a randomized controlled trial of music and recreation therapy. Journal Of Women’s Health (2002) 2010;19(3):523–31. doi: 10.1089/jwh.2008.1344. [DOI] [PubMed] [Google Scholar]
- 12.Beaulieu-Boire G, Bourque S, Chagnon F, Chouinard L, Gallo-Payet N, Lesur O. Music and biological stress dampening in mechanically-ventilated patients at the intensive care unit ward-a prospective interventional randomized crossover trial. Journal Of Critical Care. 2013;28(4):442–50. doi: 10.1016/j.jcrc.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 13.Bibb J, Castle D, Newton R. The role of music therapy in reducing post meal related anxiety for patients with anorexia nervosa. Journal of Eating Disorders. 2015;3:1–6. doi: 10.1186/s40337-015-0088-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Binns-Turner PG, Wilson LL, Pryor ER, Boyd GL, Prickett CA. Perioperative music and its effects on anxiety, hemodynamics, and pain in women undergoing mastectomy. AANA Journal. 2011;79(4 Suppl):S21–S7. [PubMed] [Google Scholar]
- 15.Binson B, Lertmaharit S, Satayaprakop P, Chongthanakorn K, Boonyakrai C, Klinphaetkit S, et al. Effects of music intervention on patients undergoing hemodialysis in the Bangkok Metropolitan Administration Hospitals. Music and medicine: An interdisciplinary journal. 2013;5(3):188–93. Record Type: Main Record Document Type: Article in a periodical. Physical Medium: print. [Google Scholar]
- 16.Björkman I, Karlsson F, Lundberg A, Frisman GH. Gender differences when using sedative music during colonoscopy. Gastroenterology Nursing: The Official Journal Of The Society Of Gastroenterology Nurses And Associates. 2013;36(1):14–20. doi: 10.1097/SGA.0b013e31827c4c80. [DOI] [PubMed] [Google Scholar]
- 17.Bradt J, Potvin N, Kesslick A, Shim M, Radl D, Schriver E, et al. The impact of music therapy versus music medicine on psychological outcomes and pain in cancer patients: a mixed methods study. Supportive Care in Cancer. 2015;23(5):1261–71. doi: 10.1007/s00520-014-2478-7. [DOI] [PubMed] [Google Scholar]
- 18.Canga B, Azoulay R, Raskin J, Loewy J. AIR: Advances in Respiration - Music therapy in the treatment of chronic pulmonary disease. Respiratory medicine. 2015;109(12):1532–9. doi: 10.1016/j.rmed.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Carr C, d’Ardenne P, Sloboda A, Scott C, Wang D, Priebe S. Group music therapy for patients with persistent post-traumatic stress disorder–an exploratory randomized controlled trial with mixed methods evaluation. Psychology And Psychotherapy. 2012;85(2):179–202. doi: 10.1111/j.2044-8341.2011.02026.x. [DOI] [PubMed] [Google Scholar]
- 20.Chang F-Y, Huang H-C, Lin K-C, Lin L-C. The effect of a music programme during lunchtime on the problem behaviour of the older residents with dementia at an institution in Taiwan. Journal Of Clinical Nursing. 2010;19(7-8):939–48. doi: 10.1111/j.1365-2702.2009.02801.x. [DOI] [PubMed] [Google Scholar]
- 21.Chang H-K, Peng T-C, Wang J-H, Lai H-L. Psychophysiological responses to sedative music in patients awaiting cardiac catheterization examination: a randomized controlled trial. The Journal Of Cardiovascular Nursing. 2011;26(5):E11–E8. doi: 10.1097/JCN.0b013e3181fb711b. [DOI] [PubMed] [Google Scholar]
- 22.Chaput-McGovern J, Silverman MJ. Effects of music therapy with patients on a post-surgical oncology unit: A pilot study determining maintenance of immediate gains. The Arts in Psychotherapy. 2012;39(5):417–22. doi: 10.1016/j.aip.2012.06.008. [DOI] [Google Scholar]
- 23.Chen L-C, Wang T-F, Shih Y-N, Wu L-J. Fifteen-minute music intervention reduces pre-radiotherapy anxiety in oncology patients. European Journal Of Oncology Nursing: The Official Journal Of European Oncology Nursing Society. 2013;17(4):436–41. doi: 10.1016/j.ejon.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 24.Chen X, Seth RK, Rao VS, Huang JJ, Adelman RA. Effects of music therapy on intravitreal injections: a randomized clinical trial. Journal Of Ocular Pharmacology And Therapeutics: The Official Journal Of The Association For Ocular Pharmacology And Therapeutics. 2012;28(4):414–9. doi: 10.1089/jop.2011.0257. [DOI] [PubMed] [Google Scholar]
- 25.Chlan LL, Engeland WC, Savik K. Does music influence stress in mechanically ventilated patients? Intensive & Critical Care Nursing. 2013;29(3):121–7. doi: 10.1016/j.iccn.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chlan LL, Weinert CR, Heiderscheit A, Tracy MF, Skaar DJ, Guttormson JL, et al. Effects of patient-directed music intervention on anxiety and sedative exposure in critically ill patients receiving mechanical ventilatory support: a randomized clinical trial. JAMA. 2013;309(22):2335–44. doi: 10.1001/jama.2013.5670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chorna OD, Slaughter JC, Wang L, Stark AR, Maitre NL. A pacifier-activated music player with mother’s voice improves oral feeding in preterm infants. Pediatrics. 2014;133(3):462–8. doi: 10.1542/peds.2013-2547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chu H, Yang C-Y, Lin Y, Ou K-L, Lee T-Y, O’Brien AP, et al. The impact of group music therapy on depression and cognition in elderly persons with dementia: a randomized controlled study. Biological Research For Nursing. 2014;16(2):209–17. doi: 10.1177/1099800413485410. [DOI] [PubMed] [Google Scholar]
- 29.Chuang C-Y, Han W-R, Li P-C, Song M-Y, Young S-T. Effect of long-term music therapy intervention on autonomic function in anthracycline-treated breast cancer patients. Integrative Cancer Therapies. 2011;10(4):312–6. doi: 10.1177/1534735411400311. [DOI] [PubMed] [Google Scholar]
- 30.Chu-Hui-Lin Chi G, Young A, McFarlane J, Watson M, Coleman RL, Eifel PJ, et al. Effects of music relaxation video on pain and anxiety for women with gynaecological cancer receiving intracavitary brachytherapy: a randomised controlled trial. Journal of Research in Nursing. 2015;20(2):129–44. doi: 10.1177/1744987114529298. [DOI] [Google Scholar]
- 31.Colwell CM, Edwards R, Hernandez E, Brees K. Impact of music therapy interventions (listening, composition, Orff-based) on the physiological and psychosocial behaviors of hospitalized children: a feasibility study. Journal Of Pediatric Nursing. 2013;28(3):249–57. doi: 10.1016/j.pedn.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 32.Comeaux T, Steele-Moses S. The Effect of Complementary Music Therapy on the Patient’s Postoperative State Anxiety, Pain Control, and Environmental Noise Satisfaction. MEDSURG Nursing. 2013;22(5):313–8. [PubMed] [Google Scholar]
- 33.Conklyn D, Novak E, Boissy A, Bethoux F, Chemali K. The effects of modified melodic intonation therapy on nonfluent aphasia: a pilot study. Journal Of Speech, Language, And Hearing Research: JSLHR. 2012;55(5):1463–71. doi: 10.1044/1092-4388(2012/11-0105). [DOI] [PubMed] [Google Scholar]
- 34.Conklyn D, Stough D, Novak E, Paczak S, Chemali K, Bethoux F. A home-based walking program using rhythmic auditory stimulation improves gait performance in patients with multiple sclerosis: a pilot study. Neurorehabilitation And Neural Repair. 2010;24(9):835–42. doi: 10.1177/1545968310372139. [DOI] [PubMed] [Google Scholar]
- 35.Cooke ML, Moyle W, Shum DHK, Harrison SD, Murfield JE. A randomized controlled trial exploring the effect of music on agitated behaviours and anxiety in older people with dementia. Aging & Mental Health. 2010;14(8):905–16. doi: 10.1080/13607861003713190. [DOI] [PubMed] [Google Scholar]
- 36.Cox E, Nowak M, Buettner P. Managing agitated behaviour in people with Alzheimer’s disease: the role of live music. British Journal of Occupational Therapy. 2011;74(11):517–24. doi: 10.4276/030802211X13204135680866. [DOI] [Google Scholar]
- 37.Cox E, Nowak M, Buettner P. Live music promotes positive behaviours in people with Alzheimer’s disease. The British Journal of Occupational Therapy. 2014;77(11):556–64. doi: 10.4276/030802214X14151078348477. [DOI] [Google Scholar]
- 38.Crawford I, Hogan T, Silverman MJsue. Effects of music therapy on perception of stress, relaxation, mood, and side effects in patients on a solid organ transplant unit: A randomized effectiveness study. Arts in Psychotherapy. 2013;40(2):224–9. doi: 10.1016/j.aip.2013.02.005. [DOI] [Google Scholar]
- 39.Cross K, Flores R, Butterfield J, Blackman M, Lee S. The effect of passive listening versus active observation of music and dance performances on memory recognition and mild to moderate depression in cognitively impaired older adults. Psychological Reports. 2012;111(2):413–23. doi: 10.2466/10.02.13.PR0.111.5.413-423. [DOI] [PubMed] [Google Scholar]
- 40.de Niet G, Tiemens B, Hutschemaekers G. Can mental healthcare nurses improve sleep quality for inpatients? British Journal Of Nursing (Mark Allen Publishing) 2010;19(17):1100–5. doi: 10.12968/bjon.2010.19.17.78558. [DOI] [PubMed] [Google Scholar]
- 41.Dehcheshmeh FS, Rafiei H. Complementary and alternative therapies to relieve labor pain: A comparative study between music therapy and Hoku point ice massage. Complementary Therapies in Clinical Practice. 2015;21(4):229–32. doi: 10.1016/j.ctcp.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 42.del Olmo MJ, Rodríguez Garrido C, Ruza Tarrío F. Music therapy in the PICU: 0- to 6-month-old babies. Music and Medicine. 2010;2(3):158–66. doi: 10.1177/1943862110370462. [DOI] [Google Scholar]
- 43.del Olmo MJ, Ruza Tarrío F, Rodríguez Garrido C, Carrasco Marina P. The Effects of a Music Therapy Intervention in PICU as Measured by the Comfort Behavior Scale. Music & Medicine. 2015;7(2):20–4. [Google Scholar]
- 44.Devare Phadke SS, Parkar H, Yardi S. Effect of Music Intervention on Immediate Post Operative Coronary Artery Bypass Graft Surgery (CABG) Patients. Indian Journal of Physiotherapy & Occupational Therapy. 2014;8(4):106–11. doi: 10.5958/0973-5674.2014.00021.5. [DOI] [Google Scholar]
- 45.Dijkstra BM, Gamel C, van der Bijl JJ, Bots ML, Kesecioglu J. The effects of music on physiological responses and sedation scores in sedated, mechanically ventilated patients. Journal Of Clinical Nursing. 2010;19(7-8):1030–9. doi: 10.1111/j.1365-2702.2009.02968.x. [DOI] [PubMed] [Google Scholar]
- 46.Dunn KS, Riley-Doucet CK. Comparative analysis of two musical genres within a multisensory environmental intervention. Journal Of Holistic Nursing: Official Journal Of The American Holistic Nurses’ Association. 2013;31(1):62–70. doi: 10.1177/0898010112461977. [DOI] [PubMed] [Google Scholar]
- 47.Dvorak AL. Music Therapy Support Groups for Cancer Patients and Caregivers: A Mixed-Methods Approach. Canadian Journal of Music Therapy. 2015;21(1):69–105. [Google Scholar]
- 48.Easter B, DeBoer L, Settlemyre G, Starnes C, Marlowe V, Tart RC. The impact of music on the PACU patient’s perception of discomfort. Journal Of Perianesthesia Nursing: Official Journal Of The American Society Of Perianesthesia Nurses. 2010;25(2):79–87. doi: 10.1016/j.jopan.2010.01.017. [DOI] [PubMed] [Google Scholar]
- 49.Eckhouse DR, Hurd M, Cotter-Schaufele S, Sulo S, Sokolowski M, Barbour L. A Randomized Controlled Trial to Determine the Effects of Music and Relaxation Interventions on Perceived Anxiety in Hospitalized Patients Receiving Orthopaedic or Cancer Treatment. Orthopaedic Nursing. 2014;33(6):342–51. doi: 10.1097/NOR.0000000000000098. [DOI] [PubMed] [Google Scholar]
- 50.Elefant C, Baker FA, Lotan M, Lagesen SK, Skeie GO. The effect of group music therapy on mood, speech, and singing in individuals with Parkinson’s disease–a feasibility study. Journal Of Music Therapy. 2012;49(3):278–302. doi: 10.1093/jmt/49.3.278. [DOI] [PubMed] [Google Scholar]
- 51.Eley R, Gorman D. Didgeridoo playing and singing to support asthma management in Aboriginal Australians. The Journal Of Rural Health: Official Journal Of The American Rural Health Association And The National Rural Health Care Association. 2010;26(1):100–4. doi: 10.1111/j.1748-0361.2009.00256.x. [DOI] [PubMed] [Google Scholar]
- 52.Erkkilä J, Punkanen M, Fachner J, Ala-Ruona E, Pöntiö I, Tervaniemi M, et al. Individual music therapy for depression: randomised controlled trial. The British Journal Of Psychiatry: The Journal Of Mental Science. 2011;199(2):132–9. doi: 10.1192/bjp.bp.110.085431. [DOI] [PubMed] [Google Scholar]
- 53.Forooghy M, Mottahedian Tabrizi E, Hajizadeh E, Pishgoo B. Effect of Music Therapy on Patients’ Anxiety and Hemodynamic Parameters During Coronary Angioplasty: A Randomized Controlled Trial. Nursing And Midwifery Studies. 2015;4(2):e25800–e. doi: 10.17795/nmsjournal25800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fredenburg HA, Silverman MJsue. Effects of cognitive-behavioral music therapy on fatigue in patients in a blood and marrow transplantation unit: A mixed-method pilot study. Arts in Psychotherapy. 2014;41(5):433–44. doi: 10.1016/j.aip.2014.09.002. [DOI] [Google Scholar]
- 55.Fredenburg HA, Silverman MJ. Effects of music therapy on positive and negative affect and pain with hospitalized patients recovering from a blood and marrow transplant: A randomized effectiveness study. Arts in Psychotherapy. 2014;41(2):174–80. doi: 10.1016/j.aip.2014.01.007. [DOI] [Google Scholar]
- 56.Fritz TH, Vogt M, Lederer A, Schneider L, Fomicheva E, Schneider M, et al. Benefits of listening to a recording of euphoric joint music making in polydrug abusers. Frontiers in Human Neuroscience. 2015;9 doi: 10.3389/fnhum.2015.00300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Galan L, Bringas ML, Valdes-Sosa PA, Zaldivar M, Martinez-Montes K, Chongo DM, et al. Effectiveness of music therapy as an aid to neurorestoration of children with severe neurological disorders. Frontiers in Neuroscience. 2015;9:1–15. doi: 10.3389/fnins.2015.00427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Garunkstiene R, Buinauskiene J, Uloziene I, Markuniene E. Controlled trial of live versus recorded lullabies in preterm infants. Nordic Journal of Music Therapy. 2014;23(1):71–88. doi: 10.1080/08098131.2013.809783. [DOI] [Google Scholar]
- 59.Good M, Albert JM, Anderson GC, Wotman S, Cong X, Lane D, et al. Supplementing relaxation and music for pain after surgery. Nursing Research. 2010;59(4):259–69. doi: 10.1097/NNR.0b013e3181dbb2b3. [DOI] [PubMed] [Google Scholar]
- 60.Good M, Albert JM, Arafah B, Anderson GC, Wotman S, Cong X, et al. Effects on postoperative salivary cortisol of relaxation/music and patient teaching about pain management. Biological Research For Nursing. 2013;15(3):318–29. doi: 10.1177/1099800411431301. [DOI] [PubMed] [Google Scholar]
- 61.Grocke D, Bloch S, Castle D, Thompson G, Newton R, Stewart S, et al. Group music therapy for severe mental illness: a randomized embedded-experimental mixed methods study. Acta Psychiatrica Scandinavica. 2014;130(2):144–53. doi: 10.1111/acps.12224. [DOI] [PubMed] [Google Scholar]
- 62.Gruhlke LC, Patrício MC, Moreira DM. Mozart, but not the Beatles, reduces systolic blood pressure in patients with myocardial infarction. Acta cardiologica. 2015;70(6):703–6. doi: 10.2143/AC.70.6.3120183. [DOI] [PubMed] [Google Scholar]
- 63.Guerrero JM, Castaño PM, Schmidt EO, Rosario L, Westhoff CL. Music as an auxiliary analgesic during first trimester surgical abortion: a randomized controlled trial. Contraception. 2012;86(2):157–62. doi: 10.1016/j.contraception.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 64.Guétin S, Giniès P, Siou DKA, Picot M-C, Pommié C, Guldner E, et al. The effects of music intervention in the management of chronic pain: a single-blind, randomized, controlled trial. The Clinical Journal Of Pain. 2012;28(4):329–37. doi: 10.1097/AJP.0b013e31822be973. [DOI] [PubMed] [Google Scholar]
- 65.Gutgsell KJ, Schluchter M, Margevicius S, DeGolia PA, McLaughlin B, Harris M, et al. Music Therapy Reduces Pain in Palliative Care Patients: A Randomized Controlled Trial. Journal of Pain & Symptom Management. 2013;45(5):822–31. doi: 10.1016/j.jpainsymman.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 66.Gutiérrez EOF, Camarena VAT. Music therapy in generalized anxiety disorder. The Arts in Psychotherapy. 2015;44:19–24. doi: 10.1016/j.aip.2015.02.003. [DOI] [Google Scholar]
- 67.Hammar LM, Emami A, Götell E, Engström G. The impact of caregivers’ singing on expressions of emotion and resistance during morning care situations in persons with dementia: an intervention in dementia care. Journal Of Clinical Nursing. 2011;20(7-8):969–78. doi: 10.1111/j.1365-2702.2010.03386.x. [DOI] [PubMed] [Google Scholar]
- 68.Han L, Li JP, Sit JWH, Chung L, Jiao ZY, Ma WG. Effects of music intervention on physiological stress response and anxiety level of mechanically ventilated patients in China: a randomised controlled trial. Journal Of Clinical Nursing. 2010;19(7-8):978–87. doi: 10.1111/j.1365-2702.2009.02845.x. [DOI] [PubMed] [Google Scholar]
- 69.Hanser SB, Butterfield-Whitcomb J, Kawata M, Collins BE. Home-based music strategies with individuals who have dementia and their family caregivers. Journal Of Music Therapy. 2011;48(1):2–27. doi: 10.1093/jmt/48.1.2. [DOI] [PubMed] [Google Scholar]
- 70.Hartling L, Newton AS, Liang Y, Jou H, Hewson K, Klassen TP, et al. Music to reduce pain and distress in the pediatric emergency department: a randomized clinical trial. JAMA Pediatrics. 2013;167(9):826–35. doi: 10.1001/jamapediatrics.2013.200. [DOI] [PubMed] [Google Scholar]
- 71.Heidari S, Babaii A, Abbasinia M, Shamali M, Abbasi M, Rezaei M. The Effect of Music on Anxiety and Cardiovascular Indices in Patients Undergoing Coronary Artery Bypass Graft: A Randomized Controlled Trial. Nursing & Midwifery Studies. 2015;4(4):1–7. doi: 10.17795/nmsjournal31157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hogan TJ, Silverman MJ. Coping-Infused Dialogue through Patient-Preferred Live Music: A Medical Music Therapy Protocol and Randomized Pilot Study for Hospitalized Organ Transplant Patients. Journal of Music Therapy. 2015;52(3):420–36. doi: 10.1093/jmt/thv008. [DOI] [PubMed] [Google Scholar]
- 73.Horne-Thompson A, Bolger K. An investigation comparing the effectiveness of a live music therapy session and recorded music in reducing anxiety for patients with amyotrophic lateral sclerosis/motor neurone disease. Australian Journal of Music Therapy. 2010;21:23–38. [Google Scholar]
- 74.Hosseini SE, Bagheri M, Honarparvaran N. Investigating the effect of music on labor pain and progress in the active stage of first labor. European Review For Medical And Pharmacological Sciences. 2013;17(11):1479–87. [PubMed] [Google Scholar]
- 75.Huang S-T, Good M, Zauszniewski JA. The effectiveness of music in relieving pain in cancer patients: a randomized controlled trial. International Journal Of Nursing Studies. 2010;47(11):1354–62. doi: 10.1016/j.ijnurstu.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 76.Hunter BC, Oliva R, Sahler OJZ, Gaisser DA, Salipante DM, Arezina CH. Music therapy as an adjunctive treatment in the management of stress for patients being weaned from mechanical ventilation. Journal Of Music Therapy. 2010;47(3):198–219. doi: 10.1093/jmt/47.3.198. [DOI] [PubMed] [Google Scholar]
- 77.Hutson C, Orrell M, Dugmore O, Spector A. Sonas: a pilot study investigating the effectiveness of an intervention for people with moderate to severe dementia. American journal of Alzheimer’s disease and other dementias. 2014;29(8):696–703. doi: 10.1177/1533317514534756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hwang E-y, Oh S-h. A comparison of the effects of music therapy interventions on depression, anxiety, anger, and stress on alcohol-dependent clients: A pilot study. Music and medicine: An interdisciplinary journal. 2013;5(3):136–44. [Google Scholar]
- 79.Janata P. Effects of Widespread and Frequent Personalized Music Programming on Agitation and Depression in Assisted Living Facility Residents With Alzheimer-Type Dementia. Music & Medicine. 2012;4(1):8–15. doi: 10.1177/1943862111430509. [DOI] [Google Scholar]
- 80.Jiemin Z, Hong-Gu H, Xiuzhu Z, Haixia W, Yaru G, Benlan Y, et al. Pain relief effect of breast feeding and music therapy during heel lance for healthy-term neonates in China: A randomized controlled trial. Midwifery. 2015;31(3):365–72. doi: 10.1016/j.midw.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 81.Jiménez-Jiménez M, García-Escalona A, Martín-López A, De Vera-Vera R, De Haro J. Intraoperative stress and anxiety reduction with music therapy: a controlled randomized clinical trial of efficacy and safety. Journal Of Vascular Nursing: Official Publication Of The Society For Peripheral Vascular Nursing. 2013;31(3):101–6. doi: 10.1016/j.jvn.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 82.Johnson B, Raymond S, Goss J. Perioperative music or headsets to decrease anxiety. Journal Of Perianesthesia Nursing: Official Journal Of The American Society Of Perianesthesia Nurses. 2012;27(3):146–54. doi: 10.1016/j.jopan.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 83.Johnson L, Deatrick EJ, Oriel K. The Use of Music to Improve Exercise Participation in People with Dementia: A Pilot Study. Physical & Occupational Therapy in Geriatrics. 2012;30(1):102–8. [Google Scholar]
- 84.Keith DR, Weaver BS, Vogel RL. The effect of music-based listening interventions on the volume, fat content, and caloric content of breast milk-produced by mothers of premature and critically ill infants. Advances In Neonatal Care: Official Journal Of The National Association Of Neonatal Nurses. 2012;12(2):112–9. doi: 10.1097/ANC.0b013e31824d9842. [DOI] [PubMed] [Google Scholar]
- 85.Kim J. Music therapy with children who have been exposed to ongoing child abuse and poverty: A pilot study. Nordic Journal of Music Therapy. 2015;24(1):27–43. doi: 10.1080/08098131.2013.872696. [DOI] [Google Scholar]
- 86.Koca Kutlu A, Eren AG. Effects of music on complications during hemodialysis for chronic renal failure patients. Hemodialysis international International Symposium on Home Hemodialysis. 2014;18(4):777–84. doi: 10.1111/hdi.12161. [DOI] [PubMed] [Google Scholar]
- 87.Koenig J, Oelkers-Ax R, Kaess M, Parzer P, Lenzen C, Hillecke TK, et al. Specific music therapy techniques in the treatment of primary headache disorders in adolescents: a randomized attention-placebo-controlled trial. The Journal Of Pain: Official Journal Of The American Pain Society. 2013;14(10):1196–207. doi: 10.1016/j.jpain.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 88.Korhan EA, Khorshid L, Uyar M. The effect of music therapy on physiological signs of anxiety in patients receiving mechanical ventilatory support. Journal Of Clinical Nursing. 2011;20(7-8):1026–34. doi: 10.1111/j.1365-2702.2010.03434.x. [DOI] [PubMed] [Google Scholar]
- 89.Korhan EA, Uyar M, Eyigör C, Hakverdioğlu Yönt G, Çelik S, Khorshıd L. The effects of music therapy on pain in patients with neuropathic pain. Pain Management Nursing: Official Journal Of The American Society Of Pain Management Nurses. 2014;15(1):306–14. doi: 10.1016/j.pmn.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 90.Krick CM, Grapp M, Daneshvar-Talebi J, Reith W, Plinkert PK, Bolay HV. Cortical reorganization in recent-onset tinnitus patients by the Heidelberg Model of Music Therapy. Frontiers in Neuroscience. 2015;9:1–9. doi: 10.3389/fnins.2015.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kulkarni S, Johnson PCD, Kettles S, Kasthuri RS. Music during interventional radiological procedures, effect on sedation, pain and anxiety: a randomised controlled trial. The British Journal Of Radiology. 2012;85(1016):1059–63. doi: 10.1259/bjr/71897605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kunikullaya KU, Goturu J, Muradi V, Hukkeri PA, Kunnavil R, Doreswamy V, et al. Music versus lifestyle on the autonomic nervous system of prehypertensives and hypertensives–a randomized control trial. Complementary Therapies in Medicine. 2015;23(5):733–40. doi: 10.1016/j.ctim.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 93.Lai W-S, Chao C-SC, Yang W-P, Chen C-H. Efficacy of guided imagery with theta music for advanced cancer patients with dyspnea: a pilot study. Biological Research For Nursing. 2010;12(2):188–97. doi: 10.1177/1099800409347556. [DOI] [PubMed] [Google Scholar]
- 94.Lee J-H, Kim S-K, Ko S-J, Lee S-H, Lee J-H, Kim M-J, et al. The Effect of Oriental Medicine Music Therapy on Idiopathic Chronic Fatigue. Journal of Alternative & Complementary Medicine. 2015;21(7):422–9. doi: 10.1089/acm.2014.0271. [DOI] [PubMed] [Google Scholar]
- 95.Lee K-C, Chao Y-H, Yiin J-J, Hsieh H-Y, Dai W-J, Chao Y-F. Evidence that music listening reduces preoperative patients’ anxiety. Biological Research For Nursing. 2012;14(1):78–84. doi: 10.1177/1099800410396704. [DOI] [PubMed] [Google Scholar]
- 96.Li C-H, Liu C-K, Yang Y-H, Chou M-C, Chen C-H, Lai C-L. Adjunct effect of music therapy on cognition in Alzheimer’s disease in Taiwan: A pilot study. Neuropsychiatric Disease and Treatment. 2015;11 doi: 10.2147/NDT.S73928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Li X-M, Yan H, Zhou K-N, Dang S-N, Wang D-L, Zhang Y-P. Effects of music therapy on pain among female breast cancer patients after radical mastectomy: results from a randomized controlled trial. Breast Cancer Research And Treatment. 2011;128(2):411–9. doi: 10.1007/s10549-011-1533-z. [DOI] [PubMed] [Google Scholar]
- 98.Li Y, Dong Y. Preoperative music intervention for patients undergoing cesarean delivery. International Journal Of Gynaecology And Obstetrics: The Official Organ Of The International Federation Of Gynaecology And Obstetrics. 2012;119(1):81–3. doi: 10.1016/j.ijgo.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 99.Lin M-F, Hsieh Y-J, Hsu Y-Y, Fetzer S, Hsu M-C. A randomised controlled trial of the effect of music therapy and verbal relaxation on chemotherapy-induced anxiety. Journal Of Clinical Nursing. 2011;20(7-8):988–99. doi: 10.1111/j.1365-2702.2010.03525.x. [DOI] [PubMed] [Google Scholar]
- 100.Lin Y, Chu H, Yang C-Y, Chen C-H, Chen S-G, Chang H-J, et al. Effectiveness of group music intervention against agitated behavior in elderly persons with dementia. International Journal Of Geriatric Psychiatry. 2011;26(7):670–8. doi: 10.1002/gps.2580. [DOI] [PubMed] [Google Scholar]
- 101.Liu Y, Petrini MA. Effects of music therapy on pain, anxiety, and vital signs in patients after thoracic surgery. Complementary Therapies in Medicine. 2015;23(5):714–8. doi: 10.1016/j.ctim.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 102.Liu Y-H, Chang M-Y, Chen C-H. Effects of music therapy on labour pain and anxiety in Taiwanese first-time mothers. Journal Of Clinical Nursing. 2010;19(7-8):1065–72. doi: 10.1111/j.1365-2702.2009.03028.x. [DOI] [PubMed] [Google Scholar]
- 103.Loewy JKA-MAP. The Effects of Music Therapy on Vital Signs, Feeding, and Sleep in Premature Infants. Pediatrics. 2013;131(5):902–18. doi: 10.1542/peds.2012-1367. [DOI] [PubMed] [Google Scholar]
- 104.Lu S-F, Lo C-HK, Sung H-C, Hsieh T-C, Yu S-C, Chang S-C. Effects of group music intervention on psychiatric symptoms and depression in patient with schizophrenia. Complementary Therapies In Medicine. 2013;21(6):682–8. doi: 10.1016/j.ctim.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 105.Madson AT, Silverman MJ. The effect of music therapy on relaxation, anxiety, pain perception, and nausea in adult solid organ transplant patients. Journal Of Music Therapy. 2010;47(3):220–32. doi: 10.1093/jmt/47.3.220. [DOI] [PubMed] [Google Scholar]
- 106.Mandel SE, Davis BA, Secic M. Effects of music therapy and music-assisted relaxation and imagery on health-related outcomes in diabetes education: a feasibility study. The Diabetes Educator. 2013;39(4):568–81. doi: 10.1177/0145721713492216. [DOI] [PubMed] [Google Scholar]
- 107.Markovich R, Kazunori T. The Effects of Single-Session Music Therapy Interventions in Comparison with a Cognitive Behavioral Intervention on Mood with Adult Psychiatric Inpatients in an Acute-Care Setting: A Quasi-Experimental Trial. Music Therapy Perspectives. 2015;33(2):118–27. doi: 10.1093/mtp/miv030. [DOI] [Google Scholar]
- 108.Martindale F, Mikocka-Walus AA, Walus BP, Keage H, Andrews JM. The effects of a designer music intervention on patients’ anxiety, pain, and experience of colonoscopy: a short report on a pilot study. Gastroenterology nursing: the official journal of the Society of Gastroenterology Nurses and Associates. 2014;37(5):338–42. doi: 10.1097/SGA.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 109.Matto HC, Tompkins CJ, Ihara ES, Inoue M, Byrd A. Results from a music, imagery, and movement treatment intervention in a long-term care facility. Families in Society. 2015;96(4):277–83. doi: 10.1606/1044-3894.2015.96.32. [DOI] [Google Scholar]
- 110.McLeod R. Evaluating the effect of music on patient anxiety during minor plastic surgery. Journal Of Perioperative Practice. 2012;22(1):14–8. doi: 10.1177/175045891202200102. [DOI] [PubMed] [Google Scholar]
- 111.Meeuse JJ, Koornstra JJ, Reyners AKL. Listening to music does not reduce pain during sigmoidoscopy. European Journal Of Gastroenterology & Hepatology. 2010;22(8):942–5. doi: 10.1097/MEG.0b013e328336ec6e. [DOI] [PubMed] [Google Scholar]
- 112.Merakou K, Varouxi G, Barbouni A, Antoniadou E, Karageorgos G, Theodoridis D, et al. Blood Pressure and Heart Rate Alterations through Music in Patients Undergoing Cataract Surgery in Greece. Ophthalmology & Eye Diseases. 2015;(7):7–12. doi: 10.4137/OED.S20960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ming Hung H, Flowerdew R, Parker M, Fachner J, Odell-Miller H. Individual music therapy for managing neuropsychiatric symptoms for people with dementia and their carers: a cluster randomised controlled feasibility study. BMC Geriatrics. 2015;15(1):1–19. doi: 10.1186/s12877-015-0082-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Mohammadi AZ, Shahabi T, Panah FM. An evaluation of the effect of group music therapy on stress, anxiety and depression levels in nursing home residents. 2011;17(1):55–68. [Google Scholar]
- 115.Nagata K, Iida N, Kanazawa H, Fujiwara M, Mogi T, Mitsushima T, et al. Effect of listening to music and essential oil inhalation on patients undergoing screening CT colonography: a randomized controlled trial. European Journal of Radiology. 2014;83(12):2172–6. doi: 10.1016/j.ejrad.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 116.Narme P, Clément S, Ehrlé N, Schiaratura L, Vachez S, Courtaigne B, et al. Efficacy of musical interventions in dementia: evidence from a randomized controlled trial. Journal Of Alzheimer’s Disease: JAD. 2014;38(2):359–69. doi: 10.3233/JAD-130893. [DOI] [PubMed] [Google Scholar]
- 117.Ni C-H, Tsai W-H, Lee L-M, Kao C-C, Chen Y-C. Minimising preoperative anxiety with music for day surgery patients - a randomised clinical trial. Journal Of Clinical Nursing. 2012;21(5-6):620–5. doi: 10.1111/j.1365-2702.2010.03466.x. [DOI] [PubMed] [Google Scholar]
- 118.Nilsson U. Effectiveness of music interventions for women with high anxiety during coronary angiographic procedures: a randomized controlled. European Journal Of Cardiovascular Nursing: Journal Of The Working Group On Cardiovascular Nursing Of The European Society Of Cardiology. 2012;11(2):150–3. doi: 10.1016/j.ejcnurse.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 119.Norouzi F, Keshavarz M, SeyedFatemi N, Montazeri A. The impact of kangaroo care and music on maternal state anxiety. Complementary Therapies In Medicine. 2013;21(5):468–72. doi: 10.1016/j.ctim.2013.07.006. [DOI] [PubMed] [Google Scholar]
- 120.O’Konski M, Bane C, Hettinga J, Krull K. Comparative effectiveness of exercise with patterned sensory enhanced music and background music for long-term care residents. Journal Of Music Therapy. 2010;47(2):120–36. doi: 10.1093/jmt/47.2.120. [DOI] [PubMed] [Google Scholar]
- 121.Olischar M, Shoemark H, Holton T, Weninger M, Hunt RW. The influence of music on aEEG activity in neurologically healthy newborns ≥32 weeks’ gestational age. Acta Paediatrica (Oslo, Norway: 1992) 2011;100(5):670–5. doi: 10.1111/j.1651-2227.2011.02171.x. [DOI] [PubMed] [Google Scholar]
- 122.Oneda B, Ortega KC, Gusmão JL, Araújo TG, Mion D., Jr Sympathetic nerve activity is decreased during device-guided slow breathing. Hypertension Research: Official Journal Of The Japanese Society Of Hypertension. 2010;33(7):708–12. doi: 10.1038/hr.2010.74. [DOI] [PubMed] [Google Scholar]
- 123.Onieva-Zafra MD, Castro-Sánchez AM, Matarán-Peñarrocha GA, Moreno-Lorenzo C. Effect of music as nursing intervention for people diagnosed with fibromyalgia. Pain Management Nursing: Official Journal Of The American Society Of Pain Management Nurses. 2013;14(2):e39–e46. doi: 10.1016/j.pmn.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 124.Onieva-Zafra MD, Castro-Sánchez AM, Matarán-Peñarrocha GA, Moreno-Lorenzo C. Effect of music as nursing intervention for people diagnosed with fibromyalgia. Pain Management Nursing: Official Journal Of The American Society Of Pain Management Nurses. 2013;14(2):e39–e46. doi: 10.1016/j.pmn.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 125.Park H. Effect of music on pain for home-dwelling persons with dementia. Pain Management Nursing: Official Journal Of The American Society Of Pain Management Nurses. 2010;11(3):141–7. doi: 10.1016/j.pmn.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 126.Parlar Kilic S, Karadag G, Oyucu S, Kale O, Zengin S, Ozdemir E, et al. Effect of music on pain, anxiety, and patient satisfaction in patients who present to the emergency department in Turkey. Japan Journal Of Nursing Science: JJNS. 2015;12(1):44–53. doi: 10.1111/jjns.12047. [DOI] [PubMed] [Google Scholar]
- 127.Phipps MA, Carroll DL, Tsiantoulas A. Music as a therapeutic intervention on an inpatient neuroscience unit. Complementary Therapies In Clinical Practice. 2010;16(3):138–42. doi: 10.1016/j.ctcp.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 128.Picard LM, Bartel LR, Gordon AS, Cepo D, Wu Q, Pink LR. Music as a sleep aid in fibromyalgia. Pain Research & Management. 2014;19(2):97–101. doi: 10.1155/2014/272108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Planas-Domingo J, Escudé Matamoros N, Farriols Danés C, Villar Abelló H, Mercadé Carranza J, Ruiz Ripoll AI, et al. Effectiveness of Music Therapy in Advanced Cancer Patients Admitted to a Palliative Care Unit: A Non-Randomized Controlled, Clinical Trial. Music & Medicine. 2015;7(1):23–31. [Google Scholar]
- 130.Pohl P, Dizdar N, Hallert E. The Ronnie Gardiner Rhythm and Music Method - a feasibility study in Parkinson’s disease. Disability And Rehabilitation. 2013;35(26):2197–204. doi: 10.3109/09638288.2013.774060. [DOI] [PubMed] [Google Scholar]
- 131.Rafer L, Austin F, Frey J, Mulvey C, Vaida S, Prozesky J. Effects of jazz on postoperative pain and stress in patients undergoing elective hysterectomy. Advances in mind-body medicine. 2015;29(1):6–11. [PubMed] [Google Scholar]
- 132.Raglio A, Bellandi D, Baiardi P, Gianotti M, Ubezio MC, Zanacchi E, et al. Effect of Active Music Therapy and Individualized Listening to Music on Dementia: A Multicenter Randomized Controlled Trial. Journal of the American Geriatrics Society. 2015;63(8):1534–9. doi: 10.1111/jgs.13558. [DOI] [PubMed] [Google Scholar]
- 133.Rawtaer I, Mahendran R, Yu J, Fam J, Feng L, Kua EH. Psychosocial interventions with art, music, Tai Chi and mindfulness for subsyndromal depression and anxiety in older adults: A naturalistic study in Singapore. Asia-Pacific Psychiatry: Official Journal Of The Pacific Rim College Of Psychiatrists. 2015;7(3):240–50. doi: 10.1111/appy.12201. [DOI] [PubMed] [Google Scholar]
- 134.Ray KD, Mittelman MS. Music therapy: A nonpharmacological approach to the care of agitation and depressive symptoms for nursing home residents with dementia. Dementia (London, England) 2015 doi: 10.1177/1471301215613779. [DOI] [PubMed] [Google Scholar]
- 135.Ripollés P, Rojo N, Grau-Sánchez J, Amengual J, Càmara E, Marco-Pallarés J, et al. Music supported therapy promotes motor plasticity in individuals with chronic stroke. Brain Imaging & Behavior. 2016;10(4):1289–307. doi: 10.1007/s11682-015-9498-x. [DOI] [PubMed] [Google Scholar]
- 136.Robb SL, Burns DS, Stegenga KA, Haut PR, Monahan PO, Meza J, et al. Randomized clinical trial of therapeutic music video intervention for resilience outcomes in adolescents/young adults undergoing hematopoietic stem cell transplant: a report from the Children’s Oncology Group. Cancer. 2014;120(6):909–17. doi: 10.1002/cncr.28355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Ryu M-J, Park JS, Park H. Effect of sleep-inducing music on sleep in persons with percutaneous transluminal coronary angiography in the cardiac care unit. Journal Of Clinical Nursing. 2012;21(5-6):728–35. doi: 10.1111/j.1365-2702.2011.03876.x. [DOI] [PubMed] [Google Scholar]
- 138.Sakamoto M, Ando H, Tsutou A. Comparing the effects of different individualized music interventions for elderly individuals with severe dementia. International Psychogeriatrics. 2013;25(5):775–84. doi: 10.1017/S1041610212002256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Sand-Jecklin K, Emerson H. The impact of a live therapeutic music intervention on patients’ experience of pain, anxiety, and muscle tension. Holistic Nursing Practice. 2010;24(1):7–15. doi: 10.1097/HNP.0b013e3181c8e435. [DOI] [PubMed] [Google Scholar]
- 140.Satoh M, Yuba T, Tabei K-I, Okubo Y, Kida H, Sakuma H, et al. Music Therapy Using Singing Training Improves Psychomotor Speed in Patients with Alzheimer’s Disease: A Neuropsychological and fMRI Study. Dementia And Geriatric Cognitive Disorders Extra. 2015;5(3):296–308. doi: 10.1159/000436960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Schall A, Haberstroh J, Pantel J. Time series analysis of individual music therapy in dementia: Effects on communication behavior and emotional well-being. GeroPsych: The Journal of Gerontopsychology and Geriatric Psychiatry. 2015;28(3):113–22. doi: 10.1024/1662-9647/a000123. [DOI] [Google Scholar]
- 142.Shabanloei R, Golchin M, Esfahani A, Dolatkhah R, Rasoulian M. Effects of music therapy on pain and anxiety in patients undergoing bone marrow biopsy and aspiration. AORN journal. 2010;91(6):746–51. doi: 10.1016/j.aorn.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 143.Shirani Bidabadi S, Mehryar A. Music therapy as an adjunct to standard treatment for obsessive compulsive disorder and co-morbid anxiety and depression: A randomized clinical trial. Journal of Affective Disorders. 2015;184:13–7. doi: 10.1016/j.jad.2015.04.011. [DOI] [PubMed] [Google Scholar]
- 144.Shum A, Taylor BJ, Thayala J, Chan MF. The effects of sedative music on sleep quality of older community-dwelling adults in Singapore. Complementary Therapies In Medicine. 2014;22(1):49–56. doi: 10.1016/j.ctim.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 145.Silverman MJ. Effects of music therapy on change readiness and craving in patients on a detoxification unit. Journal of music therapy. 2011;48(4):509–31. doi: 10.1093/jmt/48.4.509. [DOI] [PubMed] [Google Scholar]
- 146.Silverman MJ. The effect of songwriting on knowledge of coping skills and working alliance in psychiatric patients: a randomized clinical effectiveness study. Journal Of Music Therapy. 2011;48(1):103–22. doi: 10.1093/jmt/48.1.103. [DOI] [PubMed] [Google Scholar]
- 147.Silverman MJ. Effects of group songwriting on motivation and readiness for treatment on patients in detoxification: a randomized wait-list effectiveness study. Journal Of Music Therapy. 2012;49(4):414–29. doi: 10.1093/jmt/49.4.414. [DOI] [PubMed] [Google Scholar]
- 148.Silverman MJ. Effects of music therapy on self- and experienced stigma in patients on an acute care psychiatric unit: a randomized three group effectiveness study. Archives Of Psychiatric Nursing. 2013;27(5):223–30. doi: 10.1016/j.apnu.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 149.Silverman MJ. Effects of music therapy on drug avoidance self-efficacy in patients on a detoxification unit: a three-group randomized effectiveness study. J Addict Nurs. 2014;25(4):172–81. doi: 10.1097/JAN.0000000000000047. [DOI] [PubMed] [Google Scholar]
- 150.Silverman MJ. Effects of a live educational music therapy intervention on acute psychiatric inpatients’ perceived social support and trust in the therapist: a four-group randomized effectiveness study. Journal of Music Therapy. 2014;51(3):228–49. doi: 10.1093/jmt/thu011. doi:jmt/thu011. [DOI] [PubMed] [Google Scholar]
- 151.Silverman MJ. Effects of family-based educational music therapy on acute care psychiatric patients and their family members: An exploratory mixed-methods study. Nordic Journal of Music Therapy. 2014;23(2):99–122. doi: 10.1080/08098131.2013.783097. [DOI] [Google Scholar]
- 152.Silverman MJ. Effects of lyric analysis interventions on treatment motivation in patients on a detoxification unit: a randomized effectiveness study. Journal of music therapy. 2015;52(1):117–34. doi: 10.1093/jmt/thu057. [DOI] [PubMed] [Google Scholar]
- 153.Silverman MJsue, Rosenow S. Immediate quantitative effects of recreational music therapy on mood and perceived helpfulness in acute psychiatric inpatients: An exploratory investigation. Arts in Psychotherapy. 2013;40(3):269–74. doi: 10.1016/j.aip.2013.04.001. [DOI] [Google Scholar]
- 154.Sliwka A, Nowobilski R, Polczyk R, Nizankowska-Mogilnicka E, Szczeklik A. Mild asthmatics benefit from music therapy. The Journal Of Asthma: Official Journal Of The Association For The Care Of Asthma. 2012;49(4):401–8. doi: 10.3109/02770903.2012.663031. [DOI] [PubMed] [Google Scholar]
- 155.Solé C, Mercadal-Brotons M, Galati A, De Castro M. Effects of group music therapy on quality of life, affect, and participation in people with varying levels of dementia. Journal Of Music Therapy. 2014;51(1):103–25. doi: 10.1093/jmt/thu003. [DOI] [PubMed] [Google Scholar]
- 156.Standley JM, Cassidy J, Grant R, Cevasco A, Szuch C, Nguyen J, et al. The Effect of Music Reinforcement for Non-Nutritive Sucking on Nipple Feeding Of Premature Infants. Pediatric Nursing. 2010;36(3):138–45. [PubMed] [Google Scholar]
- 157.Stein TR, Olivo EL, Grand SH, Namerow PB, Costa J, Oz MC. A pilot study to assess the effects of a guided imagery audiotape intervention on psychological outcomes in patients undergoing coronary artery bypass graft surgery. Holistic Nursing Practice. 2010;24(4):213–22. doi: 10.1097/HNP.0b013e3181e90303. [DOI] [PubMed] [Google Scholar]
- 158.Su C-P, Lai H-L, Chang E-T, Yiin L-M, Perng S-J, Chen P-W. A randomized controlled trial of the effects of listening to non-commercial music on quality of nocturnal sleep and relaxation indices in patients in medical intensive care unit. Journal Of Advanced Nursing. 2013;69(6):1377–89. doi: 10.1111/j.1365-2648.2012.06130.x. [DOI] [PubMed] [Google Scholar]
- 159.Sundar S, Ramesh B, Dixit PB, Venkatesh S, Das P, Gunasekaran D. Live Music Therapy as an Active Focus of Attention for Pain and Behavioral Symptoms of Distress During Pediatric Immunization. Clinical Pediatrics. 2016;55(8):745–8. doi: 10.1177/0009922815610613. [DOI] [PubMed] [Google Scholar]
- 160.Sung H-C, Chang AM, Lee W-L. A preferred music listening intervention to reduce anxiety in older adults with dementia in nursing homes. Journal Of Clinical Nursing. 2010;19(7-8):1056–64. doi: 10.1111/j.1365-2702.2009.03016.x. [DOI] [PubMed] [Google Scholar]
- 161.Sung H-c, Lee W-l, Li T-l, Watson R. A group music intervention using percussion instruments with familiar music to reduce anxiety and agitation of institutionalized older adults with dementia. International Journal Of Geriatric Psychiatry. 2012;27(6):621–7. doi: 10.1002/gps.2761. [DOI] [PubMed] [Google Scholar]
- 162.Sven-Olof Trängeberg Ö, Stomberg MW. Listening to music during regional anesthesia: patients’ experiences and the effect on mood. Journal Of Perianesthesia Nursing: Official Journal Of The American Society Of Perianesthesia Nurses. 2013;28(5):291–7. doi: 10.1016/j.jopan.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 163.Taghinejad H, Delpisheh A, Suhrabi Z. Comparison between massage and music therapies to relieve the severity of labor pain. Women’s Health (London, England) 2010;6(3):377–81. doi: 10.2217/whe.10.15. [DOI] [PubMed] [Google Scholar]
- 164.Tamplin J, Baker FA, Buttifant M, Berlowitz DJ. The effect of singing training on voice quality for people with quadriplegia. Journal Of Voice: Official Journal Of The Voice Foundation. 2014;28(1):128.e19–e26. doi: 10.1016/j.jvoice.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 165.Tamplin J, Baker FA, Grocke D, Brazzale DJ, Pretto JJ, Ruehland WR, et al. Effect of Singing on Respiratory Function, Voice, and Mood After Quadriplegia: A Randomized Controlled Trial. Archives of Physical Medicine & Rehabilitation. 2013;94(3):426–34. doi: 10.1016/j.apmr.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 166.William TH, Bertolo T, Dinh V, Jichici D, Hamielec Cindy M. Mozart piano sonatas as a nonpharmacological adjunct to facilitate sedation vacation in critically ill patients. Music Med. 2013;5(2):119–27. [Google Scholar]
- 167.Trombetti A, Hars M, Herrmann FR, Kressig RW, Ferrari S, Rizzoli R. Effect of music-based multitask training on gait, balance, and fall risk in elderly people: a randomized controlled trial. Archives Of Internal Medicine. 2011;171(6):525–33. doi: 10.1001/archinternmed.2010.446. [DOI] [PubMed] [Google Scholar]
- 168.Tsai P-L, Chen M-C, Huang Y-T, Lin K-C, Chen K-L, Hsu Y-W. Listening to classical music ameliorates unilateral neglect after stroke. The American Journal Of Occupational Therapy: Official Publication Of The American Occupational Therapy Association. 2013;67(3):328–35. doi: 10.5014/ajot.2013.006312. [DOI] [PubMed] [Google Scholar]
- 169.Vaajoki A, Kankkunen P, Pietilä A-M, Vehviläinen-Julkunen K. Music as a nursing intervention: effects of music listening on blood pressure, heart rate, and respiratory rate in abdominal surgery patients. Nursing & Health Sciences. 2011;13(4):412–8. doi: 10.1111/j.1442-2018.2011.00633.x. [DOI] [PubMed] [Google Scholar]
- 170.Vaajoki A, Pietilä A-M, Kankkunen P, Vehviläinen-Julkunen K. Effects of listening to music on pain intensity and pain distress after surgery: an intervention. Journal Of Clinical Nursing. 2012;21(5-6):708–17. doi: 10.1111/j.1365-2702.2011.03829.x. [DOI] [PubMed] [Google Scholar]
- 171.Vanderboom TL, Arcari PM, Duffy ME, Somarouthu B, Rabinov JD, Yoo AJ, et al. Effects of a music intervention on patients undergoing cerebral angiography: a pilot study. Journal Of Neurointerventional Surgery. 2012;4(3):229–33. doi: 10.1136/neurintsurg-2011-010052. [DOI] [PubMed] [Google Scholar]
- 172.Ventura T, Gomes MC, Carreira T. Cortisol and anxiety response to a relaxing intervention on pregnant women awaiting amniocentesis. Psychoneuroendocrinology. 2012;37(1):148–56. doi: 10.1016/j.psyneuen.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 173.Vink AC, Zuidersma M, Boersma F, de Jonge P, Zuidema SU, Slaets JPJ. The effect of music therapy compared with general recreational activities in reducing agitation in people with dementia: a randomised controlled trial. International Journal Of Geriatric Psychiatry. 2013;28(10):1031–8. doi: 10.1002/gps.3924. [DOI] [PubMed] [Google Scholar]
- 174.Walworth DD. Effect of live music therapy for patients undergoing magnetic resonance imaging. Journal of music therapy. 2010;47(4):335–50. doi: 10.1093/jmt/47.4.335. [DOI] [PubMed] [Google Scholar]
- 175.Wang Y, Tang H, Guo Q, Liu J, Liu X, Luo J, et al. Effects of Intravenous Patient-Controlled Sufentanil Analgesia and Music Therapy on Pain and Hemodynamics After Surgery for Lung Cancer: A Randomized Parallel Study. Journal of Alternative & Complementary Medicine. 2015;21(11):667–72. doi: 10.1089/acm.2014.0310. [DOI] [PubMed] [Google Scholar]
- 176.Warth M, Kessler J, Kotz S, Hillecke TK, Bardenheuer HJ. Effects of vibroacoustic stimulation in music therapy for palliative care patients: a feasibility study. BMC Complementary & Alternative Medicine. 2015;15:1–8. doi: 10.1186/s12906-015-0933-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Warth M, Keβler J, Hillecke TK, Bardenheuer HJ. Music Therapy in Palliative Care. Deutsches Aerzteblatt International. 2015;112(46):788–94. doi: 10.3238/arztebl.2015.0788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Weeks BP, Nilsson U. Music interventions in patients during coronary angiographic procedures: A randomized controlled study of the effect on patients’ anxiety and well-being. European Journal of Cardiovascular Nursing. 2011;10(2):88–93. doi: 10.1016/j.ejcnurse.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 179.Weiland TJ, Jelinek GA, Macarow KE, Samartzis P, Brown DM, Grierson EM, et al. Original sound compositions reduce anxiety in emergency department patients: a randomised controlled trial. The Medical Journal Of Australia. 2011;195(11-12):694–8. doi: 10.5694/mja10.10662. [DOI] [PubMed] [Google Scholar]
- 180.Wormit AF, Warth M, Koenig J, Hillecke TK, Bardenheuer HJ. Evaluating a treatment manual for music therapy in adult outpatient oncology care. Music and medicine: An interdisciplinary journal. 2012;4(2):65–73. [Google Scholar]
- 181.Yates GJ, Silverman MJ. Immediate effects of single-session music therapy on affective state in patients on a post-surgical oncology unit: A randomized effectiveness study. The Arts in Psychotherapy. 2015;44:57–61. doi: 10.1016/j.aip.2014.11.002. [DOI] [Google Scholar]
- 182.Yun SH, Gallant W. Evidence-based clinical practice: the effectiveness of music-based intervention for women experiencing forgiveness/grief issues. Journal Of Evidence-Based Social Work. 2010;7(5):361–76. doi: 10.1080/15433710903323870. [DOI] [PubMed] [Google Scholar]
- 183.Zavotsky KE, Banavage A, James P, Easter K, Pontieri-Lewis V, Lutwin L. The Effects of Music on Pain and Anxiety During Screening Mammography. Clinical Journal of Oncology Nursing. 2014;18(3):E45–E9. doi: 10.1188/14.CJON.E45-E49. [DOI] [PubMed] [Google Scholar]
- 184.Zengin S, Kabul S, Al B, Sarcan E, Dogan M, Yildirim C. Effects of music therapy on pain and anxiety in patients undergoing port catheter placement procedure. Complementary therapies in medicine. 2013;21(6):689–96. doi: 10.1016/j.ctim.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 185.Zhang CC, Mou L, Wang X, Guo D. Does live music benefits patients with brain and spinal injury? European Review For Medical And Pharmacological Sciences. 2015;19(17):3246–50. [PubMed] [Google Scholar]
- 186.Zhou K, Li X, Li J, Liu M, Dang S, Wang D, et al. A clinical randomized controlled trial of music therapy and progressive muscle relaxation training in female breast cancer patients after radical mastectomy: Results on depression, anxiety and length of hospital stay. European Journal of Oncology Nursing. 2015;19(1):54–9. doi: 10.1016/j.ejon.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 187.Zhou KN, Li XM, Yan H, Dang SN, Wang DL. Effects of music therapy on depression and duration of hospital stay of breast cancer patients after radical mastectomy. Chinese medical journal. 2011;124(15):2321–7. [PubMed] [Google Scholar]
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest
The authors declare that they have no conflicts of interest.
References
- 1.Collins FS, Fleming R. Sound Health: An NIH-Kennedy Center Initiative to Explore Music and the Mind. Jama. 2017;317(24):2470–1. doi: 10.1001/jama.2017.7423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bradt J, Dileo C. Music interventions for mechanically ventilated patients. The Cochrane database of systematic reviews. 2014;(12):CD006902. doi: 10.1002/14651858.CD006902.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bradt J, Dileo C, Magill L, Teague A. Music interventions for improving psychological and physical outcomes in cancer patients. The Cochrane database of systematic reviews. 2016;(8):CD006911. doi: 10.1002/14651858.CD006911.pub3. [DOI] [PubMed] [Google Scholar]
- 4.Fuller T, Peters J, Pearson M, Anderson R. Impact of the transparent reporting of evaluations with nonrandomized designs reporting guideline: ten years on. Am J Public Health. 2014;104(11):e110–7. doi: 10.2105/AJPH.2014.302195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Geretsegger M, Mossler KA, Bieleninik L, Chen XJ, Heldal TO, Gold C. Music therapy for people with schizophrenia and schizophrenia-like disorders. The Cochrane database of systematic reviews. 2017;5:CD004025. doi: 10.1002/14651858.CD004025.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
- 7.Kamioka H, Tsutani K, Yamada M, Park H, Okuizumi H, Tsuruoka K, et al. Effectiveness of music therapy: a summary of systematic reviews based on randomized controlled trials of music interventions. Patient Prefer Adherence. 2014;8:727–54. doi: 10.2147/PPA.S61340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Magee WL, Clark I, Tamplin J, Bradt J. Music interventions for acquired brain injury. The Cochrane database of systematic reviews. 2017;1:CD006787. doi: 10.1002/14651858.CD006787.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robb SL, Burns DS, Carpenter JS. Reporting guidelines for music-based interventions. J Health Psychol. 2011;16(2):342–52. doi: 10.1177/1359105310374781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van der Steen JT, van Soest-Poortvliet MC, van der Wouden JC, Bruinsma MS, Scholten RJ, Vink AC. Music-based therapeutic interventions for people with dementia. The Cochrane database of systematic reviews. 2017;5:CD003477. doi: 10.1002/14651858.CD003477.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche PC, Devereaux PJ, et al. CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. 2010;63(8):e1–37. doi: 10.1016/j.jclinepi.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Des Jarlais DC, Lyles C, Crepaz N. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health. 2004;94(3):361–6. doi: 10.2105/ajph.94.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P, Group C Methods and processes of the CONSORT Group: example of an extension for trials assessing nonpharmacologic treatments. Annals of Internal Medicine. 2008;148(4):W60–6. doi: 10.7326/0003-4819-148-4-200802190-00008-w1. [DOI] [PubMed] [Google Scholar]
- 14.Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P, Group C Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Annals of Internal Medicine. 2008;148(4):295–309. doi: 10.7326/0003-4819-148-4-200802190-00008. [DOI] [PubMed] [Google Scholar]
- 15.Davidson KW, Goldstein M, Kaplan RM, Kaufmann PG, Knatterud GL, Orleans CT, et al. Evidence-based behavioral medicine: what is it and how do we achieve it?[see comment] Annals of Behavioral Medicine. 2003;26(3):161–71. doi: 10.1207/S15324796ABM2603_01. [DOI] [PubMed] [Google Scholar]
- 16.Gagnier JJ, Boon H, Rochon P, Moher D, Barnes J, Bombardier C. Reporting randomized, controlled trials of herbal interventions: an elaborated CONSORT statement. Annals of Internal Medicine. 2006;144(5):364–7. doi: 10.7326/0003-4819-144-5-200603070-00013. [DOI] [PubMed] [Google Scholar]
- 17.Robb SL, Carpenter JS. A review of music-based intervention reporting in pediatrics. J Health Psychol. 2009;14(4):490–501. doi: 10.1177/1359105309103568. Epub 2009/04/23. doi: 14/4/490 [pii] 10.1177/1359105309103568. [DOI] [PubMed] [Google Scholar]
- 18.Equator Network: Enhancing the QUAlity and Transparency Of health Research. Available from: www.equator-network.org.
- 19.Google Scholar Citation Report [Internet] [cited November 7, 2017] [Google Scholar]
- 20.Burns DS. Theoretical rationale for music selection in oncology intervention research: an integrative review. J Music Ther. 2012;49(1):7–22. doi: 10.1093/jmt/49.1.7. [DOI] [PubMed] [Google Scholar]
- 21.Lee JH. The Effects of Music on Pain: A Meta-Analysis. J Music Ther. 2016;53(4):430–77. doi: 10.1093/jmt/thw012. [DOI] [PubMed] [Google Scholar]
- 22.Reschke-Hernandez AE. Music-Based intervention reporting for children with autism: Implications for music therapy publication guidelines. Music Therapy Perspectives. 2012;30(2):167–75. [Google Scholar]
- 23.Ard J, W BL. Music therapy and stroke: An integrative review. Music and Medicine. 2016;8(4) [Google Scholar]
- 24.Sena Moore K. A systematic review on the neural effects of music on emotion regulation: implications for music therapy practice. J Music Ther. 2013;50(3):198–242. doi: 10.1093/jmt/50.3.198. [DOI] [PubMed] [Google Scholar]
- 25.Silverman JM, Letwin L, Nuehring L. Patient preferred live music with adult medical patients: A systematic review to determine implications for clinical practice and future research. The Arts in Psychotherapy. 2016;49:1–7. [Google Scholar]
- 26.Yinger OS, Gooding LF. A systematic review of music-based interventions for procedural support. J Music Ther. 2015;52(1):1–77. doi: 10.1093/jmt/thv004. [DOI] [PubMed] [Google Scholar]
- 27.Kim J, Stegemann T. Music listening for children and adolesents in health care contexts: A systematic review. The Arts in Psychotherapy. 2016;51:72–85. [Google Scholar]
- 28.Hanson-Abromeit D. A conceptual methodology to define the therapeutic function of music. Music Therapy Perspectives. 2015;33(1):25–38. [Google Scholar]
- 29.Corry M, Clarke M, While AE, Lalor J. Developing complex interventions for nursing: a critical review of key guidelines. Journal of clinical nursing. 2013;22(17-18):2366–86. doi: 10.1111/jocn.12173. [DOI] [PubMed] [Google Scholar]
- 30.Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. Int J Nurs Stud. 2013;50(5):587–92. doi: 10.1016/j.ijnurstu.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 31.Geretsegger M, Elefant C, Mossler KA, Gold C. Music therapy for people with autism spectrum disorder. The Cochrane database of systematic reviews. 2014;(6):CD004381. doi: 10.1002/14651858.CD004381.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stegemoller EL. Exploring a neuroplasticity model of music therapy. J Music Ther. 2014;51(3):211–27. doi: 10.1093/jmt/thu023. [DOI] [PubMed] [Google Scholar]
- 33.Hallam S, Cross I, Thaut M, editors. The Oxford Handbook of Music Psychology. 2nd. Oxford, UK: Oxford University Press; 2016. [Google Scholar]
- 34.Ang K, Maddocks M, Xu H, Higginson IJ. The Effectiveness of Singing or Playing a Wind Instrument in Improving Respiratory Function in Patients with Long-Term Neurological Conditions: A Systematic Review. J Music Ther. 2017;54(1):108–31. doi: 10.1093/jmt/thx001. [DOI] [PubMed] [Google Scholar]
- 35.Bardy BG, Hoffmann CP, Moens B, Leman M, Dalla Bella S. Sound-induced stabilization of breathing and moving. Ann N Y Acad Sci. 2015;1337:94–100. doi: 10.1111/nyas.12650. [DOI] [PubMed] [Google Scholar]
- 36.Tracy MF, Chlan L. Nonpharmacological interventions to manage common symptoms in patients receiving mechanical ventilation. Crit Care Nurse. 2011;31(3):19–28. doi: 10.4037/ccn2011653. [DOI] [PubMed] [Google Scholar]
- 37.Moore KS. A systematic review on the neural effects of music on emotion regulation: implications for music therapy practice. J Music Ther. 2013;50(3):198–242. doi: 10.1093/jmt/50.3.198. [DOI] [PubMed] [Google Scholar]
- 38.McKinney CH, Honig TJ. Health Outcomes of a Series of Bonny Method of Guided Imagery and Music Sessions: A Systematic Review. J Music Ther. 2017;54(1):1–34. doi: 10.1093/jmt/thw016. [DOI] [PubMed] [Google Scholar]
- 39.Kwekkeboom K, Huseby-Moore K, Ward S. Imaging ability and effective use of guided imagery. Res Nurs Health. 1998;21(3):189–98. doi: 10.1002/(sici)1098-240x(199806)21:3<189::aid-nur2>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 40.Lee SE, Han Y, Park H. Neural Activations of Guided Imagery and Music in Negative Emotional Processing: A Functional MRI Study. J Music Ther. 2016;53(3):257–78. doi: 10.1093/jmt/thw007. [DOI] [PubMed] [Google Scholar]
- 41.Aucouturier JJ, Canonne C. Musical friends and foes: The social cognition of affiliation and control in improvised interactions. Cognition. 2017;161:94–108. doi: 10.1016/j.cognition.2017.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Maratos A, Crawford MJ, Procter S. Music therapy for depression: it seems to work, but how? Br J Psychiatry. 2011;199(2):92–3. doi: 10.1192/bjp.bp.110.087494. [DOI] [PubMed] [Google Scholar]
- 43.Erkkila J, Punkanen M, Fachner J, Ala-Ruona E, Pontio I, Tervaniemi M, et al. Individual music therapy for depression: randomised controlled trial. Br J Psychiatry. 2011;199(2):132–9. doi: 10.1192/bjp.bp.110.085431. [DOI] [PubMed] [Google Scholar]
- 44.Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol. 2004;23(5):443–451. doi: 10.1037/0278-6133.23.5.433. [DOI] [PubMed] [Google Scholar]
- 45.Resnick B, et al. Treatment fidelity in behavior change research: a case example. Nurs Res. 2005;54(2):139–143. doi: 10.1097/00006199-200503000-00010. pii: 00006199-200503000-00010. [DOI] [PubMed] [Google Scholar]
- 46.Robb SL, Burns DS, Docherty SL, Haase JE. Ensuring treatment fidelity in a multi-site behavioral intervention study: implementing NIH behavior change recommendations in the SMART trial. Psychooncology. 2011;20:1193–1201. doi: 10.1002/pon.1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Johnson JK, Chow ML. Hearing and music in dementia. Handb Clin Neurol. 2015;129:667–687. doi: 10.1016/B978-0-444-62630-1.00037-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Joossee LL. Do sound levels and space contribute to agitation in nursing home residents with dementia? Research in Gerontological Nursing. 2012;5(3):174–84. doi: 10.3928/19404921-20120605-02. [DOI] [PubMed] [Google Scholar]
- 49.Hanson-Abromeit D. The newborn individualized developmental care and assessment program (NIDCAP) as a model for clinical music therapy interventions with premature infants. Music Ther Perspect. 2003;21:60–68. doi: 10.1093/mtp/21.2.60. [DOI] [Google Scholar]
- 50.Shoemark H, Hanson-Abromeit D, Stewart L. Constructing optimal experience for the hospitalized newborn through neuro-based music therapy. Front Hum Neurosci. 2015;9:487. doi: 10.3389/fnhum.2015.00487. [DOI] [PMC free article] [PubMed] [Google Scholar]


