Abstract
Greater parent–youth disagreement on youth symptomatology is associated with a host of factors (e.g., parental psychopathology, family functioning) that might impede treatment. Parent–youth disagreement may represent an indicator of treatment prognosis. Using data from the Child/ Adolescent Anxiety Multimodal Study, this study used polynomial regression and longitudinal growth modeling to examine whether parent–youth agreement prior to and throughout treatment predicted treatment outcomes (anxiety severity, youth functioning, responder status, and diagnostic remission, rated by an independent evaluator). When parents reported more symptoms than youth prior to treatment, youth were less likely to be diagnosis-free post-treatment; this was only true if the youth received cognitive-behavioral therapy (CBT) alone, not if youth received medication, combination, or placebo treatment. Increasing concordance between parents and youth over the course of treatment was associated with better treatment outcomes across all outcome measures (ps < .001). How parents and youth “co-report” appears to be an indicator of CBT outcome. Clinical implications and future directions are discussed.
Keywords: Informant discrepancies, youth anxiety, treatment, outcome monitoring
It is well established that parents and youth are often in low agreement over the presence and severity of youth psychopathology (Achenbach, McConaughy, & Howell, 1987; De Los Reyes, 2011). Although meaningful advances have been made in understanding why this disagreement occurs (see De Los Reyes et al. (2015) for a review), what can be made of these so-called informant discrepancies? Despite decades of work investigating causes and correlates of informant agreement, studies continue to simply conclude that multi-informant assessment is important (e.g. Lagattuta, Sayfan, & Bamford, 2012; Michels et al., 2013), with little guidance offered for interpreting discrepant reporting patterns, particularly within the context of treatment. With greater attention being paid to including ongoing evidence-based assessment practices in routine care (Jensen-Doss, 2011; Lambert & Shimokawa, 2011), understanding how to effectively use information gathered from multiple informants over the course of treatment may be useful for clinicians.
Prior cross-sectional work has linked higher disagreement on internalizing symptoms between parents and youth (i.e. higher discrepancies) with greater family dysfunction (Kolko & Kazdin, 1993) and higher parental psychopathology (Berg-Nielsen, Vika, & Dahl, 2003). Greater discrepancies on internalizing symptoms have also been predictive of greater future emotional and behavioral difficulties (Ferdinand, van der Ende, & Verhulst, 2004). Discrepancies between parents and youth may reflect poor communication between parents and children (Yeh & Weisz, 2001), greater parental stress (Kolko & Kazdin, 1993), and lack of child (or parent) insight into symptoms and impairment. Many of these identified correlates of discrepancies are also variables that negatively impact treatment outcomes for youth anxiety (e.g. family functioning, parental psychopathology; Peris et al., 2012; Southam-Gerow, Kendall, & Weersing, 2001). The extent to which parents and youth disagree on the need for and focus of treatment (i.e. the presence of youth psychopathology) may also negatively impact treatment adherence. High parent–youth discrepancy on youth symptoms may therefore serve as a proxy for a host of variables thought to impede treatment outcomes that are often not directly assessed in treatment.
Preliminary research suggests that pre-treatment disagreement and changes in disagreement over treatment may predict treatment outcomes for anxious youth. One study has linked greater pre-treatment discrepancies on a broad measure of youth psychopathology with lower parental involvement in therapy (Israel, Thomsen, Langeveld, & Stormark, 2007). A more recent study suggested that greater pre-treatment disagreement on anxiety treatment targets predicted poorer parental satisfaction with youth therapy (Hoffman & Chu, 2015). Additionally, in a trial of cognitive-behavioral therapy (CBT) for youth anxiety, youth who reported fewer anxiety symptoms than their parents during a pre-treatment diagnostic interview exhibited poorer treatment outcomes (Panichelli-Mindel, Flannery-Schroeder, Kendall, & Angelosante, 2005). The authors theorized that those youth were less willing to disclose negative symptoms and open up in therapy, which in turn may have prevented skill acquisition. Low youth insight or awareness into their own symptoms may also have impacted these findings. Recent work examining parent/youth disagreement on symptoms of post-traumatic stress disorder (PTSD) also suggested a similar pattern. Youth disagreeing more strongly with their parents on their PTSD symptoms at the start of treatment showed poorer treatment outcomes relative to youth who agreed with their parents (Humphreys, Weems, & Scheeringa, 2015).
Over treatment, increasing agreement on anxiety symptoms between parents and youth may indicate improvement in a number of important psychosocial domains (e.g. increased youth willingness to disclose negative feelings, improved parent–youth communication). Similarly, consistently greater disagreement could reflect higher family stresses and conflict within the dyad or family environment. Some data suggest that the magnitude of parent/youth agreement on anxiety over the course of CBT for anxiety is relatively stable (Safford, Kendall, Flannery-Schroeder, Webb, & Sommer, 2005), and that parents and youth may generally agree on improvement in youth anxiety symptoms post-treatment (Benjamin, Puleo, & Kendall, 2011). When consistency in parent/youth agreement on anxiety symptoms was examined in relation to treatment outcomes among youth with social phobia, levels of disagreement between parents and youth remained consistently high from pre- to post-treatment for those youth considered treatment non-responders (De Los Reyes, Alfano, & Beidel, 2010). In contrast, responders were more likely to demonstrate increasing agreement on their anxiety with their parents over treatment.
These initial findings indicate that parent/youth disagreement may serve as a prognostic indicator for treatment outcome, but conclusions are hampered by several limitations. In defining parent/ youth disagreement, prior work has dichotomized youth as either “disclosers” or “non-disclosers” based on whether or not they reported fewer symptoms than their parent (Panichelli-Mindel et al., 2005). This approach likely reduces the variability associated with discrepancies. Additionally, prior work using baseline parent/youth agreement to predict treatment factors (with the exception of Humphreys et al., 2015) has frequently relied on the use of a difference score between parent and youth report as the predictor variable. This approach has been recently criticized (for more details, see Laird & De Los Reyes, 2013; Laird & Weems, 2011) and limits interpretability of previous findings. Finally, work assessing discrepancies on anxiety symptoms before and after treatment provided initial evidence that changes in parent/youth agreement over treatment may be meaningful (De Los Reyes et al., 2010). However, little is known about how disagreement changes throughout treatment and how to interpret these changes.
No studies have examined whether these relationships between parent–youth discrepancies on anxiety symptoms and treatment outcomes differ between psychotherapy and pharmacological interventions. As pharmacological interventions require less active participation between youth, parents, and therapists than psychotherapy, the association between discrepancies and outcomes may be less strong for youth treated with medication versus psychotherapy. Similarly, aspects of CBT, such as emotion identification and exposure exercises, may reduce discrepancies by improving youth symptom recognition and establishing a shared vocabulary in ways that medication does not. Thus, changes over the course of treatment may be more likely to occur within psychological therapy, rather than medication. Alternatively, accurate titration of medication for anxiety may be dependent on the extent to which parents and youth agree on symptom changes; high disagreement may make accurate medication prescription difficult for physicians. Additionally, youth or parent willingness to adhere to a medication regimen may be influenced by informant perception of a need for treatment.
This study examined (1) whether pre-treatment parent–youth disagreement on youth anxiety symptoms predicted treatment outcomes across CBT and pharmacotherapy, (2) how discrepancies changed over treatment and whether this differed for medication versus CBT, and (3) whether increasing concordance between youth and parents over the course of treatment was associated with better outcomes in both treatments for pediatric anxiety. Limitations of previous studies were addressed by applying the latest recommendations for the study of informant agreement (i.e. polynomial regression coefficients; Laird & De Los Reyes, 2013) to address the first aim of this article; growth modeling was used to understand how agreement changes over treatment to address the second and third aims. It was expected that greater disagreement at pretreatment and continued discordance between parents and youth will predict poorest youth outcomes, and that these relationships would be pronounced when youth received psychological therapy compared to medication.
Method
This study analyzed data gathered at four time points over the active treatment phase in Child/ Adolescent Anxiety Multimodal Study (CAMS) (Walkup et al., 2008; pre-treatment through 12 weeks). Detailed information on study design and outcomes can be found elsewhere (Compton et al., 2010; Ginsburg et al., 2011). Briefly, youth met diagnostic criteria for generalized, social, or separation anxiety disorder and were randomized to one of four treatment conditions: CBT (n = 139), sertraline (n = 133), their combination (n = 140), and pill placebo (n = 76). Youth and parents participated in full assessment batteries with Independent Evaluators (IEs) at pre-treatment (T1) and post-treatment (12 weeks, T4), and completed briefer assessment batteries at Week 4 (T2) and Week 8 (T3). All procedures were approved by the Institutional Review Boards at each treatment site and all participants provided informed consent prior to participation.
Participants
Youth and parent participants (N = 488 dyads) were those who participated in CAMS. Youth were between the ages of 7 and 17 (M = 10.7 years, standard deviation (SD) = 2.8 years), were 49.6% female, and were largely Caucasian (n = 385, 78.9%). Parent participants were largely mothers (n = 428, 88.1%).
Measures
Parent and youth report of anxiety symptoms
Discrepancies were examined at T1–T4 using the youth and parent forms of the Screen for Child Anxiety Related Disorders (SCARED), which assesses youth anxiety over the previous 2 weeks (Birmaher et al., 1999; Birmaher et al., 1997). Psychometric properties of the SCARED are well documented (Birmaher et al., 1999; Hale, Raaijmakers, Muris, & Meeus, 2005).The Total Anxiety score was used and showed excellent internal consistencies in this sample (Cronbach’s αs range: .93–.94 and .90–.93 across T1–T4 for youth and parents, respectively). The SCARED’s parallel forms for parents and youth—its ordinal, graduated scale items, and demonstration of measurement equivalence between parents and youth (Dirks et al., 2014)—makes it an optimal discrepancy measure (Achenbach, 2011).
Treatment outcomes
The Clinical Global Impressions Scale–Improvement (CGI-I; Guy, 1976), Clinical Global Impressions Scale–Severity (CGI-S; Guy, 1976), Children’s Global Assessment Scale (CGAS; Shaffer et al., 1983), and diagnostic remission indexed outcomes for the current study. IE-rated measures were chosen as the primary outcome variables to avoid confounding outcome ratings with individual parent and youth reports. CAMS IEs were master’s level clinicians or higher who were blind to youth treatment condition and were not the youths’ treating clinician. IEs completed all four outcome measures at the conclusion of acute treatment (T4). The CGI-I measures improvement over the course of treatment, with lower scores indicating better response; for purposes of analyses, participants were dichotomized into treatment responders (CGI-I of 1 = Very Much Improved or 2 = Much Improved) and non-responders (CGI-I > 2). The CGI-S assesses anxiety severity, with higher scores indicating greater severity. The CGAS, rated on a scale of 0–100, provides a global rating of youth functional impairment; lower scores indicate higher impairment. Diagnostic remission was defined as the absence of all three study entry diagnoses at post-treatment on the Anxiety Disorders Interview Schedule for Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; DSM-IV-TR), Child Version (ADIS-IV C/P; Silverman & Albano, 1996).
Additional variables of interest
Parent/youth agreement was hypothesized to capture a host of factors that might impede treatment progress. To test whether disagreement was capturing this type of information, hypothesized correlates of disagreement were included in analyses. Prior work with this sample demonstrated that higher parental psychopathology was associated with greater disagreement between parents and youth, with parents reporting higher symptoms than their children (Becker et al., 2016). Youth age, youth gender, youth functioning, and family functioning (assessed at baseline) were also correlated with individual informants’ report. These previously established cross-sectional correlates of agreement were included as potential explanatory variables in analyses and were assessed as follows:
Parental psychopathology. The Global Severity Index (GSI) and the anxiety score from the Brief Symptom Inventory (BSI; Derogatis & Melisaratos, 1983) assessed parental psychopathology (Cronbach’s α = .95 and .81 for the GSI and anxiety scores, respectively).
Youth functioning. The CGAS assessed youth functioning at T1.
Family functioning. The Brief Family Assessment Measure (BFAM; Skinner, Steinhauer, & Santa-Barbara, 1995) assessed overall family functioning; higher scores indicate more family dysfunction. Internal consistencies were adequate for parent (α = .84) and youth (α = .76) reports.
Additional variables of potential interest included socioeconomic status, racial minority status, and presence of diagnostic comorbidity; these were not related to informant reporting in this sample and were therefore not examined further.
Analysis plan
Consistent with recent recommendations for the study of informant agreement (Laird & De Los Reyes, 2013; Laird & Weems, 2011), a polynomial regression coefficients approach (Edwards, 2002) examined the relationship between pre-treatment discrepancies and treatment outcome, which uses an interaction term calculated between parent and youth symptom reports. A significant interaction term indicates that a high (or low) score from one informant is more or less strongly associated with the dependent variable when the other informant is also reporting a high (or low) score. Unlike the more commonly used difference score approach, this approach controls for the main effects of parent and youth scores on outcomes and isolates the effect of the discrepancy from the individual informant effects on examined variables (cf. Laird & De Los Reyes, 2013). To examine whether treatment modality moderated the relationship between baseline discrepancies and outcomes, three-way interaction terms were calculated between discrepancies (i.e. the interaction between parent and youth report) and treatment condition, dummy coded to contrast the placebo, medication, and combination groups with the CBT group.
Multiple group latent growth modeling analysis (LGM) in MPlus (Muthén & Muthén, 1998–2011) was used to model trajectories of discrepancies over the course of treatment. Rates of change were estimated using absolute values of the raw difference scores. To account for the magnitude and direction of discrepancies in analyses, trajectories were modeled separately for dyads in which (1) parents initially reported the same or more symptoms than youth at T1 (the Parent Reported High group, n = 357), and (2) those in which youth reported more symptoms than their parents at T1 (the Youth Reported High group, n = 128). Comparison of a series of nested models determined whether initial discrepancies (i.e. model intercepts) and changes in discrepancies over time (i.e. trajectory slopes) differed between these two groups. To examine whether changes in discrepancies differed across treatments, treatment condition was dummy coded with placebo as the referent and regressed on trajectory slopes; follow-up contrasts also compared changes in discrepancies across the active treatment conditions. To examine whether decreasing discrepancies between parents and youth over treatment predicted better outcomes, slope estimates from the final multiple group model were regressed on treatment outcome variables using structural regression analyses for outcome variables.
Control/explanatory variables
Consistent with prior CAMS analyses, all outcome analyses controlled for baseline anxiety severity (CGI-S) and treatment site. When significant effects were found, youth age, youth gender, youth functioning, parental psychopathology, and family functioning were added to models individually as control variables in each model to determine whether discrepancies continued to be significant after accounting for these variables. Should discrepancies no longer be significant, this would suggest the control variable may partially explain the relationship between discrepancies and treatment outcome.
Missing data
Consistent with prior CAMS analyses, multiple imputation (MI) with 20 imputations handled missing data. However, trajectory modeling analyses relied on comparing nested models within the context of multiple group analysis. As comparing nested models in MPlus is not possible with multiply imputed datasets, full information maximum likelihood addressed missing data for these analyses.
Results
Preliminary analyses examined correlations between parent and youth SCARED scores over treatment. Correlations between parents and youth were moderate at T1–T4 (T1 = .41, T2 = .47, T3 = .47, and T4 = .52), and increased across time points, suggesting examining change over time was appropriate. At T1, parents reported more symptoms than did youth on average (Parent M = 32.1, SD = 12.9; Youth M = 23.4, SD = 15.1; t(487) = 12.57, p < .001). Raw difference scores ranged from −35 to 60 (M = 8.6, SD = 15.3); 128 (26.2%) youth reported more symptoms than their parents.
Does pre-treatment parent/youth disagreement predict treatment outcome?
Using the polynomial regression approach, pre-treatment disagreement did not predict anxiety severity (β = .03, p = .53), youth functioning (β = −.04, p = .46), treatment responder status (odds ratio (OR) = 1.00, 95% confidence interval (CI): [1.00, 1.01], p = .67), or treatment remission (OR = 1.00, 95% CI: [1.00, 1.01], p = .94) at the end of treatment across the full sample, which was contrary to hypothesis. However, a significant treatment by reporting pattern interaction emerged for treatment remission (p < .05). Follow-up analyses indicated that within the CBT condition only, lower likelihood of remission occurred when parents reported more symptoms than youth at pretreatment (high discrepancy). Specifically, when youth reported low levels of symptoms (1 SD below the mean), higher parent report (i.e. increasing disagreement) predicted increased likelihood youth would not remit (OR = 1.07, 95% CI: [1.01, 1.14], p = .04). When youth reported high levels of their own symptoms (1 SD above the mean), parent report did not predict remission (OR = .98, 95% CI: [.92, 1.05], p = .55). This effect was not present in the other active treatment conditions. This held after controlling for baseline youth functioning, family functioning, and youth age. Controlling for parental psychopathology reduced the significance of the discrepancy (p = .10), suggesting higher parental psychopathology may partially account for this effect. Parental psychopathology itself did not predict remission (OR = 2.61, 95% CI: [.87, 7.83], p = .09). Treatment condition did not moderate the relationship between T1 discrepancies and other outcome measures.
How does parent/youth disagreement change over treatment?
As noted, trajectories of the raw difference score were examined separately and simultaneously for the Youth Reported High group and Parent Reported High groups at each time point using multiple group longitudinal growth modeling. Specified factor loadings corresponded directly to the treatment time interval (0, 4, 8, and 12). Linear change represented good fit for the Youth Reported High group (χ2(5) = 3.49, p = .62; comparative fit index (CFI) = 1.00; root mean square error of approximation (RMSEA) < .001; standardized root mean square residual (SRMR) = .05). Inspection of the data for the Parent Reported High group indicated more change occurred between T1 and T2 in this group. Freely estimating T2 with linear change estimates resulted in a well-fitting model (χ2(5) = 11.97, p = .04; CFI = .96; RMSEA = .06; SRMR = .05), with T2 estimated at 6.46 weeks. Models including quadratic change components were tested to avoid over-simplification; this resulted in poor convergence across discrepancy groups. Thus, the multiple group models used linear change estimates.
To determine whether intercept and slope estimates differed between the two discrepancy groups, a model was first tested constraining both intercept and slope estimates equal between groups (χ2(12) = 52.64, p < .001). Next, a model was specified allowing intercepts to vary, which resulted in a better fitting model (χ2(1) = 13.93, p < .001). Next, slopes were allowed to vary between groups. This again resulted in a better fitting model (χ2(1) = 23.25, p < .001), indicating that initial levels and rates of changes in discrepancies differed depending on who initially reported more symptoms (see Figure 1). The final multiple group model fit well (χ2(10) = 15.46, p = .12; CFI = .97; RMSEA = .05; SRMR = .05). Within the Youth Reported High group, there was significant model-predicted discrepancy at T1 (intercept = 10.13, standard error (SE) = .63, p < .001); however, no significant change in agreement occurred over treatment (slope = −.11, SE = .08, p = .16). Within the Parent Reported High group, there was also significant disagreement at the start of treatment (intercept = 15.39, SE = .57, p < .001). However, in contrast to the Youth Reported High group, significant change occurred in discrepancies over treatment (slope = −.59, SE = .06; p < .001). Thus, on average, disagreement decreased by .59 points for each week of treatment in this group. Significant variability was observed around the intercepts and slopes for both discrepancy groups (ps < .05), suggesting variance to be explained by predictors.
Figure 1.
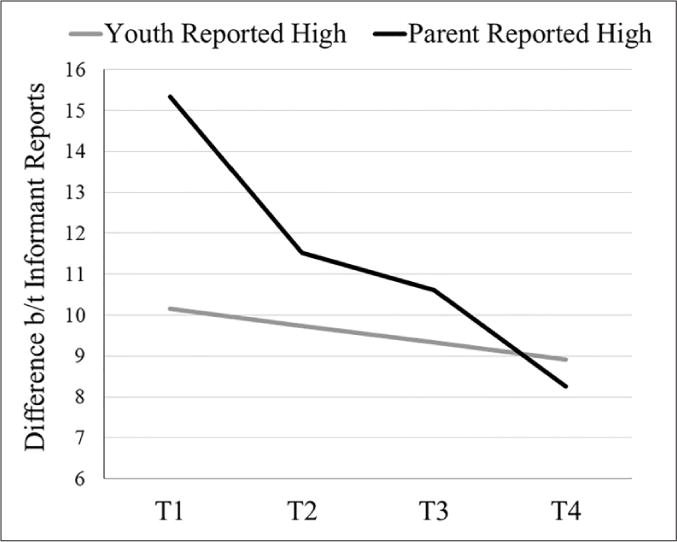
Model estimated mean differences between parent and youth report on the discrepancies across treatment. Separate trajectories are shown for when youth reported higher symptoms than parents (Youth Reported High, n = 128), and when parents reported higher symptoms than did youth (Parent Reported High, n = 357). Intercept and slope estimates significantly differed between the two groups.
Does change in agreement differ by treatment condition?
Within the Youth Reported High group, none of the three active treatment conditions showed differences in change in agreement relative to placebo (combination b = −.02, SE = .17, p = .93; sertraline b = −.05, SE = .21, p = .81; CBT b = −.02, SE = .20, p = .94). Follow-up contrasts indicated no significant differences between the medication conditions and CBT (combination b = .01, SE = .16, p = .93; sertraline b = −.03, SE = .18, p = .87) or between the two medication conditions (b = −.02, SE = .07, p = .82). In contrast, within the Parent Reported High group, youth in the two medication conditions showed significantly greater decreases in discrepancies (i.e. showed increased concordance) compared to youth placebo (combination b = −.42, SE = .11, p < .001; sertraline b = −.40, SE = .11, p < .001); the CBT and placebo groups did not differ (b = −.17, SE = .11, p = .13). Follow-up contrasts indicated both medication conditions showed greater decreases in discrepancies than did CBT (combination b = −.26, SE = .09, p = .006; sertraline b = −.24, SE = .09, p = .009). There were no differences between the two medication groups (b = −.02, SE = .09, p = .82). Thus, contrary to hypotheses, greater decrease in discrepancies was seen among youth receiving medication (combination and sertraline) versus youth receiving CBT alone. While the rate with which agreement increased over treatment varied across treatment conditions, there were significant increases in concordance within each of the four treatment arms. This increasing agreement and difference across treatment arms only held for the Parent Reported High group.
Does increasing concordance between parents and youth predict better treatment outcome?
Within the Youth Reported High group, changes in disagreement did not predict outcomes on any measure. In contrast, within the Parent Reported High group, slope estimates significantly predicted all four outcome variables. Specifically, greater increases in concordance between parents and youth over the course of treatment predicted lower youth anxiety severity (b = 1.54), better youth functioning (b = −10.53), and increased likelihood of youth being rated a treatment responder (OR = 3.27) and achieving diagnostic remission (OR = 2.89; all ps < .001, see Table 1). Relationships held after controlling for treatment condition, parental psychopathology, family functioning, youth age and gender, and baseline functioning (CGAS).
Table 1.
Changes in agreement as a predictor of treatment outcome.
| CGI-S | Model fit
|
Predicting from slope
|
Predicting from intercept
|
||||
|---|---|---|---|---|---|---|---|
| χ2 (df) | b (SE) | β (SE) | b (SE) | β (SE) | CGI-S R2 | ||
| 104.2 (71)*** | |||||||
| Parent Reported High | 1.54 (.07)*** | .70 (.05)*** | .07 (.02)*** | .39 (.11)*** | .37*** | ||
| Youth Reported High | .74 (.55) | .28 (.15) | <.01 (.05) | <.01 (.15) | .22* | ||
|
| |||||||
| CGAS | Model fit
|
Predicting from slope
|
Predicting from intercept
|
||||
| χ2 (df) | b (SE) | β (SE) | b (SE) | β (SE) | CGAS R2 | ||
|
| |||||||
| 106.9 (71)** | |||||||
|
| |||||||
| Parent Reported High | −10.53 (2.56)*** | −.59 (.10)*** | −.43 (.15)** | −.29 (.11)** | .29*** | ||
| Youth Reported High | −1.98 (3.19) | −.09 (.15) | .09 (.35) | .04 (.14) | .16* | ||
|
| |||||||
| Responder statusa | Model fit
|
Predicting from slope
|
Predicting from intercept
|
||||
| χ2 (df) | OR | b (SE) | p | OR | b (SE) | p | |
|
| |||||||
| 81.98 (70) | |||||||
| Parent Reported High | 3.27 | 1.19 (.21) | <.001 | 1.07 | .07 (.01) | <.001 | |
| Youth Reported High | 1.31 | .27 (.30) | .36 | 1.01 | .01 (.04) | .83 | |
|
| |||||||
| Diagnostic remissionb | Model fit
|
Predicting from slope
|
Predicting from intercept
|
||||
| χ2 (df) | OR | b (SE) | p | OR | b (SE) | p | |
|
| |||||||
| 82.98 (70) | |||||||
| Parent Reported High | 2.89 | 1.06 (.22) | <.001 | 1.07 | .07 (.01) | <.001 | |
| Youth Reported High | 1.60 | .47 (.31) | .14 | 1.01 | .01 (.03) | .72 | |
CGI-S: Clinical Global Impressions Scale–Severity; df degrees of freedom; SE: standard error; CGAS: Children’s Global Assessment Scale; OR: odds ratio.
Intercepts and slopes were freely estimated across groups for all models. Relationships between slope and intercepts to outcome variables were allowed to vary between groups. Presented models controlled for the relationship of baseline anxiety severity and treatment site on outcome measures.
Responders were coded as 0; non-responders were coded as 1.
Remission was coded as 0; non-remission was coded as 1.
p < .05;
p < .01;
p < .001.
Post hoc analyses
As change trajectories differed based on which informant initially reported higher symptoms, t-tests examined differences between these two discrepancy groups on T1 variables. Relative to the Youth Reported High group, youth in the Parent Reported High group were younger (t(486) = 2.11, p = .04, Cohen’s d = .22) and lower functioning on the CGAS at pre-treatment (t(486) = 2.75, p = .006, Cohen’s d = .28). Both parents and youth in the Parent Reported High group also reported better family functioning (Parent BFAM t(486) = 2.06, p = .04, Cohen’s d = .21; Youth BFAM t(486) = 3.90, p < .001, Cohen’s d = .40). Parental anxiety and global psychopathology did not differ between groups (all ps > .05).
Discussion
Results provide some support for the idea that initial levels of disagreement can serve as a prognostic indicator for youth treatment outcomes. Consistent with hypotheses, youth were less likely to be in diagnostic remission at post-treatment when parents reported more symptoms than youth; however, this was only true when youth were assigned to the CBT condition. Follow-up analyses suggest that higher parental psychopathology associated with this reporting pattern may underlie this finding. In contrast, pre-treatment discrepancies did not predict outcomes in the medication or the combination conditions.
Results of growth modeling analyses indicated that, on average, informant discrepancies decreased over treatment, but only when parents reported more symptoms than youth at T1. Although it was hypothesized that CBT would have a greater impact on agreement by increasing youth insight into their own symptoms and addressing parenting issues, results did not support this: greater increases in concordance were observed in both medication conditions relative to CBT alone. Perhaps most interestingly, consistent with hypotheses, when parents reported more symptoms than youth at the start of treatment, increasing concordance between parents and youth over the course of treatment predicted better acute outcomes across all measurement indices.
Several clinical implications can be drawn. In instances where a “parent high/youth low” reporting is observed when youth present for services, clarification of disagreements may be a helpful first step in cognitive-behavioral treatment. If there is a failure to improve concordance, more intensive and/or communication-focused therapy, the use of medication as a monotherapy, or combination treatment approaches may be indicated. In addition, results demonstrating that increasing agreement between parents and youth over the course of treatment was associated with better outcomes suggest that discrepancies may be able to be used to monitor treatment progress within treatments. While the exact ways in which these co-reporting patterns should be interpreted will require additional replication and further study, results of this study suggest that attention to whether symptom reports remain discrepant or come to concordance (i.e. “co-reporting”) for parents and youth who present in disagreement at the start of treatment may be a way for clinicians to monitor treatment progress.
Results were generally in line with hypotheses but several questions remain. First, why did concordance improve more in the medication conditions than in CBT alone? Timing of expected symptom change between the treatment conditions may be an explanation. For youth who received medication, symptom change may be noticeable earlier in treatment. While it may take multiple weeks for some youth to see benefit from medication, it is possible these early medication responders may have driven this increased concordance in the medication conditions. In contrast, symptom change for youth receiving CBT may be variable (Chu, Skriner, & Zandberg, 2013) and less observable until the exposure sessions are initiated (typically considered the most potent CBT ingredient for anxiety; Kendall et al., 1997), which was typically around Week 7 of CAMS (Compton et al., 2010). Thus, for the CBT-only condition, only the last one to two time points may have captured changes in agreement in this study. Measuring agreement over a longer period of time or more frequently may capture changes occurring within CBT. Alternatively, while the CBT manual used in CAMS (Coping Cat; Kendall & Hedtke, 2006) includes several parent sessions, it is primarily youth-oriented. More improvements in concordance might have been observed in a more parent-oriented or family-based CBT (e.g. Peris & Piacentini, 2013; Wood, Piacentini, Southam-Gerow, Chu, & Sigman, 2006).
Second, why did changes in informant agreement predict outcomes? It was hypothesized that discrepancies may capture a range of information that plays a role in treatment outcomes. However, controlling for variables associated with discrepancies in the models, as well as for the effect of treatment condition, did not account for all of the variability explained by changes in discrepancies. One explanation may be that changes in discrepancies reflect changes in the constructs measured at baseline. For example, it may be improvements in family functioning co-occur with changes in discrepancies which lead to improved outcomes. Previous work demonstrated that improvements in family functioning and parental mental health occurred concomitantly with youth treatment improvement (Keeton et al., 2013); changes in discrepancies may therefore be occurring as a function of changes in these constructs. Future research looking at changes in these variables as discrepancies change may be a useful next step.
Alternatively, constructs not measured in this study might explain these findings. For example, parent–youth communication is one factor theorized to contribute to relationships between discrepancies and outcomes. CAMS did not include a measure of communication, so this theory could not be tested. Future work should examine how parent–youth communication or other unmeasured variables of theoretical interest (e.g. youth social desirability) may explain relationships between discrepancies and treatment outcomes.
Third, why did discrepancies relate to outcome only when parents reported more symptoms than youth at the start of treatment? This “parent high/youth low” reporting pattern, the most common in this sample, is one most clearly associated with treatment risk factors in this sample (i.e. higher parental psychopathology, poorer treatment outcome in CBT), and may be also associated with poor youth self-awareness of symptoms, although it was not possible to directly assess this in this sample. It is possible that informant agreement may predict outcomes only in the context of this reporting pattern. An alternative explanation may be reduced statistical power associated with the Youth Reported High group. This group was much smaller than the Parent Reported High group, and exhibited discrepancies of smaller magnitude and variability.
Finally, are changes in discrepancies capturing unique information or reflecting effects of treatment? An alternative notion is that observed concordance occurs as a byproduct of improvement as anxiety severity decreases. To some extent, changes in discrepancies are likely driven by parent and youth perception of treatment benefit. However, group differences in changes in discrepancies (combination = sertraline > CBT = placebo) did not mirror the primary acute anxiety treatment outcomes of the CAMS trial (combination > sertraline = CBT > placebo), lending support for the idea that discrepancies are at least in part capturing treatment information (e.g. improvement in family functioning) beyond treatment outcome main effects. This was further supported by the fact that discrepancies predicted treatment outcome even after accounting for treatment condition.
Results should be interpreted along with study limitations. Change in disagreement over time was indexed via raw difference scores, which have noted limitations (Laird & De Los Reyes, 2013). While the multiple group analytic approach in this study accounted for different agreement patterns (i.e. when parent reported higher symptoms than youth at the start of treatment or vice versa), the use of raw difference scores makes it difficult to parse out effects related to disagreement from main effects of each informant. Also, while a study strength was the use of blind IE-rated outcomes, there are associated limitations. Currently, there is no fully “objective” method to assess youth anxiety treatment outcomes. IEs rely on parent and youth symptom report along with clinical judgment to assign ratings, and studies suggest that IEs may align more with parent report of symptoms than youth report (Grills & Ollendick, 2003). Whether this reflects IE perceptions of parents as more accurate reporters or a potential bias is unknown. Caution may be indicated in interpreting IE ratings as fully objective.
This study had several other strengths. It is one of only a handful of studies to examine temporal changes in discrepancies, and one of the first to examine how they relate to treatment outcomes using the polynomial regression approach. This study advances prior work examining changes in discrepancies over treatment by including multiple time points. Use of CAMS data allowed for adequately powered, complex analyses to address research questions. Incorporating identified correlates of discrepancies into analyses allowed for identifying why discrepancies might relate to treatment outcomes. This study also led to preliminary clinical recommendations for how informant agreement can be used to predict and monitor treatment outcomes by identifying co-reporting patterns (i.e. parent high/youth low symptom report) that may be prognostic of poorer outcomes in CBT. Additionally, results demonstrated that chronic disagreement between parents and youth over the course of treatment may serve as a warning sign for poorer youth outcomes across treatment modalities.
Findings present several future directions. Future studies with more frequent assessment could determine at what point in treatment continued parent/youth disagreement first emerges as a warning sign for poor treatment outcome. Such information could enhance the development of monitoring and feedback systems (Kelley & Bickman, 2009). As including both parents and youth in outcome monitoring efforts may increase sensitivity for identifying cases at risk of treatment failure than parent report alone (Cannon, Warren, Nelson, & Burlingame, 2010), examining whether co-reporting could enhance progress monitoring is an exciting next step.
Acknowledgments
ClinicalTrials.gov Number NCT00052078.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported the National Institute of Mental Health grants U01MH64089, U01MH64107, U01MH64003, U01MH63747, U01MH064092, and U01MH64088 awarded to the PIs of the Child/Adolescent Anxiety Multimodal Study, and NIMH grant F31 MH102852-01A1 awarded to the first author.
Biographies
Emily M Becker-Haimes is a post-doctoral fellow at the Center for Mental Health Policy and Services Research at the University of Pennsylvania. Her work focuses on understanding how to increase the use of evidence-based practices for youth mental health in routine clinical care settings, with a particular focus on intervention for pediatric anxiety disorders.
Amanda Jensen-Doss is an associate professor in the Child Division of the Department of Psychology at the University of Miami. Her research focuses on three themes: 1) to identify the strengths and limitations of current youth mental health care in clinical care settings, 2) to identify experimentally supported assessment tools and treatments that are most ready for dissemination to these settings, and 3) to bridge the gap between clinical services and evidence-based practices (EBPs) by testing the benefits of employing evidence-based assessment tools and treatments in clinical care settings.
Boris Birmaher is a child and adolescent psychiatrist and holds the Endowed Chair in Early Onset Bipolar Disease and is Professor of Psychiatry, University of Pittsburgh School of Medicine. Dr. Birmaher is a widely recognized expert in pharmacological and biological studies of children and adolescents with mood and anxiety disorders.
Philip C Kendall is distinguished university professor and Laura H. Carnell Professor of Psychology at Temple University where he is also the director of the Child and Adolescent Anxiety Disorders Clinic. An active researcher and scholar his CV lists over 650 publications, including his treatment program (e.g., Coping cat) for anxiety in youth.
Golda S Ginsburg is professor of Psychiatry and director of the Child Anxiety and Mood Program at University of Connecticut Health, has been involved in the assessment, prevention, and treatment of pediatric anxiety disorders for over 20 years.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Achenbach TM. Commentary: Definitely more than measurement error: But how should we understand and deal with informant discrepancies? Journal of Clinical Child & Adolescent Psychology. 2011;40:80–86. doi: 10.1080/15374416.2011.533416. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin. 1987;101:213–232. doi: 10.1037/0033-2909.101.2.213. [DOI] [PubMed] [Google Scholar]
- Becker EM, Jensen-Doss A, Kendall PC, Birmaher B, Ginsburg GS. All anxiety is not created equal: Correlates of parent/youth agreement vary across subtypes of anxiety. Journal of Psychopathology and Behavioral Assessment. 2016:1–10. doi: 10.1007/s10862-016-9544-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamin CL, Puleo CM, Kendall PC. Informant agreement in treatment gains for child anxiety. Child & Family Behavior Therapy. 2011;33:199–216. doi: 10.1080/07317107.2011.595987. [DOI] [Google Scholar]
- Berg-Nielsen TS, Vika A, Dahl AA. When adolescents disagree with their mothers: CBCL-YSR discrepancies related to maternal depression and adolescent self-esteem. Child: Care, Health and Development. 2003;29:207–213. doi: 10.1046/j.1365-2214.2003.00332.x. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, Neer SM. The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Cannon JA, Warren JS, Nelson PL, Burlingame GM. Change trajectories for the Youth Outcome Questionnaire self-report: Identifying youth at risk for treatment failure. Journal of Clinical Child & Adolescent Psychology. 2010;39:289–301. doi: 10.1080/15374411003691727. [DOI] [PubMed] [Google Scholar]
- Chu BC, Skriner LC, Zandberg LJ. Shape of change in cognitive behavioral therapy for youth anxiety: Symptom trajectory and predictors of change. Journal of Consulting and Clinical Psychology. 2013;81:573–587. doi: 10.1037/a0033390. [DOI] [PubMed] [Google Scholar]
- Compton SN, Walkup JT, Albano AM, Piacentini JC, Birmaher B, Sherrill JT, Waslick BD. Child/Adolescent Anxiety Multimodal Study (CAMS): Rationale, design, and methods. Child and Adolescent Psychiatry and Mental Health. 2010;4 doi: 10.1186/1753-2000-4-1. Article 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A. Introduction to the special section: More than measurement error: Discovering meaning behind informant discrepancies in clinical assessments of children and adolescents. Journal of Clinical Child & Adolescent Psychology. 2011;40:1–9. doi: 10.1080/15374416.2011.533405. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Alfano CA, Beidel DC. The relations among measurements of informant discrepancies within a multisite trial of treatments for childhood social phobia. Journal of Abnormal Child Psychology. 2010;38:395–404. doi: 10.1007/s10802-009-9373-6. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Augenstein TM, Wang M, Thomas SA, Drabick DA, Burgers DE, Rabinowitz J. The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin. 2015;141:858–900. doi: 10.1037/a0038498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: An introductory report. Psychological Medicine. 1983;13:595–605. doi: 10.1017/S0033291700048017. [DOI] [PubMed] [Google Scholar]
- Dirks MA, Weersing VR, Warnick E, Gonzalez A, Alton M, Dauser C, Woolston J. Parent and youth report of youth anxiety: Evidence for measurement invariance. The Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2014;55:284–291. doi: 10.1111/jcpp.12159. [DOI] [PubMed] [Google Scholar]
- Edwards JR. Alternatives to difference scores: Polynomial regression and response surface methodology. In: Drasgow F, Schmitt N, editors. The Jossey-Bass business & management series. San Francisco, CA: Jossey-Bass; 2002. pp. 350–400. [Google Scholar]
- Ferdinand RF, van der Ende J, Verhulst FC. Parent-adolescent disagreement regarding psychopathology in adolescents from the general population as a risk factor for adverse outcome. Journal of Abnormal Psychology. 2004;113:198–206. doi: 10.1037/0021-843X.113.2.198. [DOI] [PubMed] [Google Scholar]
- Ginsburg GS, Kendall PC, Sakolsky D, Compton SN, Piacentini J, Albano A, March J. Remission after acute treatment in children and adolescents with anxiety disorders: Findings from the CAMS. Journal of Consulting and Clinical Psychology. 2011;79(6):806–813. doi: 10.1037/a0025933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grills AE, Ollendick TH. Multiple informant agreement and the anxiety disorders interview schedule for parents and children. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42:30–40. doi: 10.1097/00004583-200301000-00008. [DOI] [PubMed] [Google Scholar]
- Guy W. ECDEU assessment manual for psychopharmacology, revised (US Department of Health, Education, and Welfare publication [ADM]) Rockville, MD: National Institute of Mental Health; 1976. [Google Scholar]
- Hale WW, Raaijmakers Q, Muris P, Meeus W. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED) in the general adolescent population. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44:283–290. doi: 10.1097/00004583-200503000-00013. [DOI] [PubMed] [Google Scholar]
- Hoffman LJ, Chu BC. Target problem (mis) matching: Predictors and consequences of parent–youth agreement in a sample of anxious youth. Journal of Anxiety Disorders. 2015;31:11–19. doi: 10.1016/j.janxdis.2014.12.015. [DOI] [PubMed] [Google Scholar]
- Humphreys KL, Weems CF, Scheeringa MS. The role of anxiety control and treatment implications of informant agreement on child PTSD symptoms. Journal of Clinical Child & Adolescent Psychology. 2015 doi: 10.1080/15374416.2015.1094739. Advance online publication, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel P, Thomsen PH, Langeveld JH, Stormark KM. Parent–youth discrepancy in the assessment and treatment of youth in usual clinical care setting: Consequences to parent involvement. European Child & Adolescent Psychiatry. 2007;16:138–148. doi: 10.1007/s00787-006-0583-y. [DOI] [PubMed] [Google Scholar]
- Jensen-Doss A. Practice involves more than treatment: How can evidence-based assessment catch up to evidence-based treatment? Clinical Psychology: Science and Practice. 2011;18:173–177. doi: 10.1111/j.1468-2850.2011.01248.x. [DOI] [Google Scholar]
- Keeton CP, Ginsburg GS, Drake KL, Sakolsky D, Kendall PC, Birmaher B, Walkup JT. Benefits of child-focused anxiety treatments for parents and family functioning. Depression and Anxiety. 2013;30:865–872. doi: 10.1002/da.22055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley SD, Bickman L. Beyond outcomes monitoring: Measurement feedback systems (MFS) in child and adolescent clinical practice. Current Opinion in Psychiatry. 2009;22:363–368. doi: 10.1097/YCO.0b013e32832c9162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall PC, Flannery-Schroeder E, Panichelli-Mindel SM, Southam-Gerow M, Henin A, Warman M. Therapy for youths with anxiety disorders: A second randomized clinical trial. Journal of Consulting and Clinical Psychology. 1997;65:366–380. doi: 10.1037/0022-006X.65.3.366. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Hedtke KA. Cognitive-behavioral therapy for anxious children: Therapist manual. Ardmore, PA: Workbook Publishing; 2006. [Google Scholar]
- Kolko DJ, Kazdin AE. Emotional/behavioral problems in clinic and nonclinic children: Correspondence among child, parent and teacher reports. The Journal of Child Psychology and Psychiatry, and Allied Disciplines. 1993;34:991–1006. doi: 10.1111/j.1469-7610.1993.tb01103.x. [DOI] [PubMed] [Google Scholar]
- Lagattuta KH, Sayfan L, Bamford C. Do you know how I feel? Parents underestimate worry and overestimate optimism compared to child self-report. Journal of Experimental Child Psychology. 2012;113:211–232. doi: 10.1016/j.jecp.2012.04.001. [DOI] [PubMed] [Google Scholar]
- Laird RD, De Los Reyes A. Testing informant discrepancies as predictors of early adolescent psychopathology: Why difference scores cannot tell you what you want to know and how polynomial regression may. Journal of Abnormal Child Psychology. 2013;41:1–14. doi: 10.1007/s10802-012-9659-y. [DOI] [PubMed] [Google Scholar]
- Laird RD, Weems CF. The equivalence of regression models using difference scores and models using separate scores for each informant: Implications for the study of informant discrepancies. Psychological Assessment. 2011;23(2):388–397. doi: 10.1037/a0021926. [DOI] [PubMed] [Google Scholar]
- Lambert MJ, Shimokawa K. Collecting client feedback. Psychotherapy. 2011;48:72–79. doi: 10.1037/a0022238. [DOI] [PubMed] [Google Scholar]
- Michels N, Vanaelst B, Stoppie E, Huybrechts I, Bammann K, Henauw S, Sioen I. Parental and children’s report of emotional problems: Agreement, explanatory factors and event-emotion correlation. Child and Adolescent Mental Health. 2013;18:180–186. doi: 10.1111/j.1475-3588.2012.00672.x. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6th. Los Angeles, CA: Author; 1998–2011. [Google Scholar]
- Panichelli-Mindel SM, Flannery-Schroeder E, Kendall PC, Angelosante AG. Disclosure of distress among anxiety-disordered youth: Differences in treatment outcome. Journal of Anxiety Disorders. 2005;19:403–422. doi: 10.1016/j.janxdis.2004.04.003. [DOI] [PubMed] [Google Scholar]
- Peris TS, Piacentini J. Optimizing treatment for complex cases of childhood obsessive compulsive disorder: A preliminary trial. Journal of Clinical Child & Adolescent Psychology. 2013;42:1–8. doi: 10.1080/15374416.2012.673162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peris TS, Sugar CA, Bergman RL, Chang S, Langley A, Piacentini J. Family factors predict treatment outcome for pediatric obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology. 2012;80:255–263. doi: 10.1037/a0027084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safford SM, Kendall PC, Flannery-Schroeder E, Webb A, Sommer H. A longitudinal look at parent–child diagnostic agreement in youth treated for anxiety disorders. Journal of Clinical Child & Adolescent Psychology. 2005;34:747–757. doi: 10.1207/s15374424jccp3404_16. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S. A Children’s Global Assessment Scale (CGAS) Archives of General Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. Anxiety disorders interview schedule for children for DSM–IV: (Child and Parent Versions) San Antonio, TX: Psychological Corporation/Graywind; 1996. [Google Scholar]
- Skinner H, Steinhauer P, Santa-Barbara J. FAM-III manual. Toronto, Ontario, Canada: Multi-Health Systems; 1995. [Google Scholar]
- Southam-Gerow MA, Kendall PC, Weersing VR. Examining outcome variability: Correlates of treatment response in a child and adolescent anxiety clinic. Journal of Clinical Child Psychology. 2001;30:422–436. doi: 10.1207/S15374424JCCP3003_13. [DOI] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, Kendall PC. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JJ, Piacentini JC, Southam-Gerow M, Chu BC, Sigman M. Family cognitive behavioral therapy for child anxiety disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45:314–321. doi: 10.1097/01.chi.0000196425.88341.b0. [DOI] [PubMed] [Google Scholar]
- Yeh M, Weisz JR. Why are we here at the clinic? Parent-child (dis)agreement on referral problems at outpatient treatment entry. Journal of Consulting and Clinical Psychology. 2001;69:1018–1025. doi: 10.1037/0022-006X.69.6.1018. [DOI] [PubMed] [Google Scholar]


