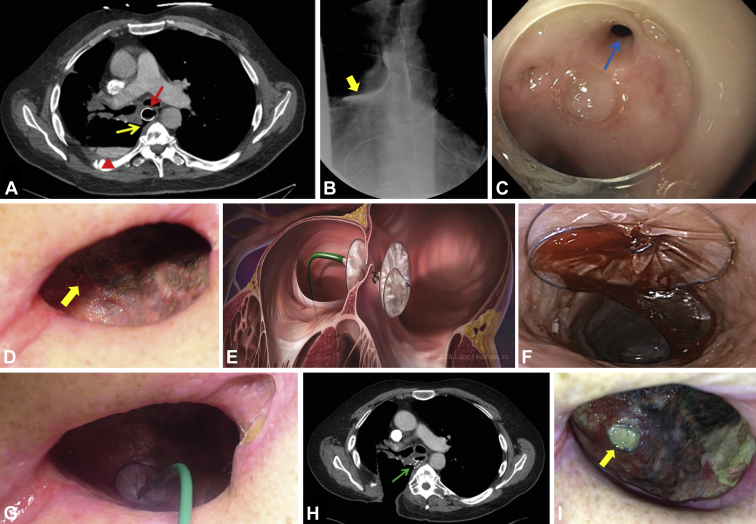
A 55-year-old man with a radiation-induced esophageal stricture experienced an esophagopleural fistula (EPF) as an adverse event of endoscopic balloon dilation therapy. Despite 9 months of covered esophageal stent treatment, the fistula persisted (Figs. 1A and B). Owing to its recessed position and fibrotic nature, endoclip closure was unlikely to be beneficial (Fig. 1C). The patient underwent an Eloesser flap thoracostomy, and 2 months later, an atrial septal occluder was deployed (Fig. 1D; Video 1, available online at www.VideoGIE.org). The cavernostomy wound was unpacked. Under endoscopic guidance, an atrial septal occluder device was passed through the fistula and into the esophagus (Fig. 1E). The proximal end of the occluder was deployed and pulled against the esophageal wall. The distal end was then deployed in a standard fashion (Fig. 1F). Once the occluder was deployed, the distal end was sutured to the chest wall in 2 locations with 4-0 Polysorb suture (Polysor, Covidien, Medtronic, Minneapolis, Minn), to ensure anchoring and prevent disruption with dressing changes (Fig. 1G). An initial esophagogram performed 1 week after deployment showed a persistent leak, but time was allowed to achieve tissue ingrowth of the device, and at 4 weeks, closure of the fistula was confirmed (Figs. 1H and I). An atrial septal occluder device should be considered for persistent EPFs that fail conventional therapy.
Figure 1.
A, Abdominal CT scan confirming the persistent esophagopleural fistula (yellow arrow), an adequately placed stent (red arrow), and a right pleural effusion (arrowhead).B, Esophagram showing contrast medium leaking into the right pleural space (yellow arrow).C, Upper endoscopy revealing a 5-mm fistulous opening in the proximal esophagus (blue arrow).D, Side view of the chest wall demonstrating the thoracostomy window, and the subtle fistulous opening (yellow arrow).E, Scheme of the atrial septal occluder device that was deployed under endoscopic guidance. Copyright 2012 by W.L. Gore & Associates, Inc. Reprinted by permission of W.L. Gore & Associates, Inc. F, Endoscopic view of the esophagus, showing the proximal end of the deployed atrial occluder device covering the fistulous opening. G, Side view of the chest wall showing the deployed atrial septal occluder covering the fistulous defect. H, 4-week follow-up CT scan of the abdomen, showing device and closed defect (green arrow).I, Side view of the chest wall demonstrating the septal occluder covered by fibrous connective tissue (yellow arrow).
Disclosure
All authors disclosed no financial relationships relevant to this publication.
Footnotes
Written transcript of the video audio is available online at www.VideoGIE.org.
Supplementary data
Closure of a persistent esophagopleural fistula with use of an atrial septal occluder device.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Closure of a persistent esophagopleural fistula with use of an atrial septal occluder device.