A 49-year-old woman who had previously undergone Roux-en-Y gastric bypass (RYGB) presented to an outside hospital with cholangitis. Because her RYGB anatomy precluded conventional ERCP, the outside hospital team achieved biliary access by means of EUS-directed transgastric ERCP (EDGE). ERCP with plastic biliary stent placement was completed successfully. During the procedure, the lumen-apposing metal stent (LAMS) that was used to create the gastrogastric fistula (GGF) became dislodged. The GGF was salvaged by placement of a fully covered esophageal stent, which was anchored into place with a full-thickness clip and 4 double-pigtail stents. She presented to our institution 10 months later after gaining 20 pounds because of the reversal of her bypass. To restore her bypass, we planned to repeat the ERCP to remove all transluminal stents and finally to close the GGF with endoscopic suturing (Video 1, available online at www.VideoGIE.org). The transgastric stents were identified traversing the GGF (Figs. 1A and B). The double-pigtail stents were removed with grasping forceps. The dislodged LAMS was then identified in the duodenal bulb and similarly removed. A duodenoscope was advanced to the ampulla, where the previously placed biliary stent was removed with a snare. A cholangiogram showed small filling defects in the common bile duct (Fig. 1C). Multiple balloon sweeps cleared the bile duct of small stones and sludge; a repeated cholangiogram confirmed ductal clearance. The gastroscope was reinserted. The esophageal stent and attached full-thickness metal clip were noted to be dislodged; both were subsequently removed with forceps (Fig. 1D). Argon plasma coagulation was used to denude the mucosa of the GGF and prepare it for suturing. Using an endoscopic suturing device, we placed a running suture across the GGF. The tract was then oversewn with an interrupted stitch (Figs. 1E and F). A final injection of contrast medium showed no extravasation into the remnant stomach. The patient underwent an uncomplicated cholecystectomy 2 weeks later. This case demonstrates successful closure by endoscopic suturing of an iatrogenic GGF resulting from performance of an EDGE procedure.
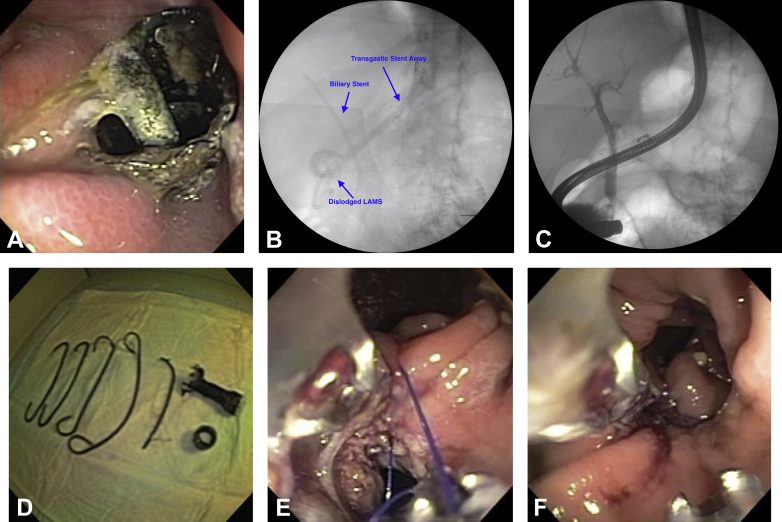
Figure 1.
A, Esophageal stent and double-pigtail stents traversing the gastrogastric fistula. B, Scout film showing stents in situ. C, Cholangiogram showing filling defects in common bile duct. D, Stents removed throughout procedure. E, Endoscopic suturing of gastrogastric fistula. F, Oversewn gastrogastric fistula adjacent to gastrojejunal anastomosis.
Disclosure
Dr DiMaio is a consultant for Boston Scientific. All other authors disclosed no financial relationships relevant to this publication.
Footnotes
Written transcript of the video audio is available online at www.VideoGIE.org.
Supplementary data
Use of endoscopic suturing to close an iatrogenic gastrogastric fistula, following trans-gastric ERCP.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Use of endoscopic suturing to close an iatrogenic gastrogastric fistula, following trans-gastric ERCP.