The development of balloon enteroscopy–assisted endoscopic retrograde cholangiopancreatography (BE-ERCP) has allowed the endoscopic treatment of a biliary anastomotic stricture in patients with surgically altered anatomy. However, challenging cases have remained. In particular, when the stricture is severe, occasionally the anastomotic site cannot be detected making BE-ERC impossible and forcing the patient to undergo percutaneous transhepatic biliary drainage (PTBD) with a resulting poor quality of life. Recently, EUS-guided biliary drainage has been developed as an alternative to PTBD. The new digital per-oral cholangioscope (DPCS) SpyGlass DS System (Boston Scientific Japan, Tokyo, Japan) has also been developed, with marked improvements in terms of image quality and system setup. Video 1 (available online at www.VideoGIE.org) shows antegrade therapy by use of this new DPCS through the EUS-guided hepaticogastrostomy (EUS-HGS) route for a stricture of the biliojejunal anastomotic site.
The patient was a 77-year-old man who had undergone a Whipple surgical procedure for pancreatic cancer 7 months previously. He presented with jaundice and abdominal pain without fever. Laboratory tests revealed hyperbilirubinemia and elevated hepatobiliary enzymes. Abdominal CT showed dilatated bilateral intrahepatic bile ducts and a stricture of the biliojejunal anastomotic site (Fig. 1). First, double BE-ERCP was performed, but it failed because of a nonvisible anastomotic site (Fig. 2). EUS-HGS was performed with a 19G needle and attempts were made to pass a guidewire antegrade through the EUS-HGS route, but the attempt failed (Fig. 3). Thus, an 8F plastic stent (Through Pass Type IT, Gadelius Medical, Tokyo, Japan) was placed from the stomach into the intrahepatic bile duct for biliary decompression (Fig. 4). One month later, we again attempted to make an antegrade guidewire pass into the stricture of the anastomosis; however, this was still not possible. Therefore, because of this failure, we achieved detection using the new DPCS through the EUS-HGS route, and a 10F plastic stent (Through Pass, Gadelius Medical) was placed for dilation of the EUS-HGS route to allow smooth insertion of the DPCS (Fig. 5). Nevertheless, it is worth noting that the cost of SpyGlass does not justify its use except in the rare case in which a guidewire cannot be advanced through the anastomosis under fluoroscopic guidance. After 1 week, a catheter for cholangiography was inserted through the EUS-HGS route, and a cholangiogram revealed a severe stricture at the anastomotic site. The DPCS was then inserted over the guidewire through the EUS-HGS route into the distal end of the biliary duct. Eventually, the anastomotic site could be detected as a pinhole, and a 0.025-inch guidewire could pass through the stricture. Dilation was gradually achieved with a Soehendra stent retriever catheter (Cook Japan, Tokyo, Japan) and a 15-mm balloon dilation catheter (CRE Balloon Dilatation Catheters, Boston Scientific Japan). Finally, an 8F plastic stent (Through Pass Type IT, Gadelius Medical) could be placed from the stomach to the jejunum through the anastomotic site (Fig. 6 and Video 1). During these procedures, there were no adverse events. In conclusion, the new DPCS with good visualization through the EUS-HGS route detected a severe stricture of the biliojejunal anastomotic site, and antegrade dilation and stent placement were successful. A series of these therapies may be considered as an alternative therapy in selected patients with a severe stricture of the biliojejunal anastomotic site.
Figure 1.
Enhanced CT of the abdomen, showing dilatated bilateral intrahepatic bile ducts (A and B) and stricture of the biliojejunal anastomotic site (C).
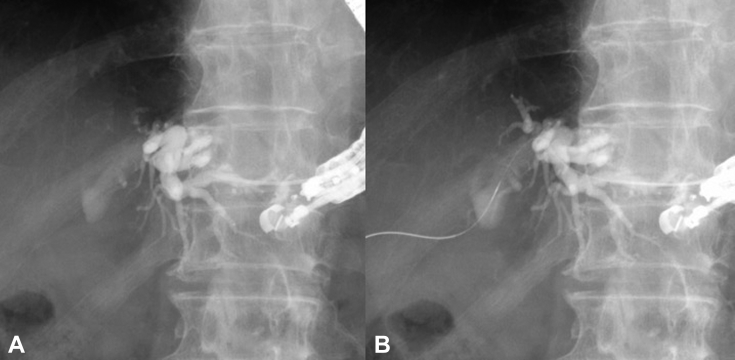
Figure 2.
Double-balloon enteroscopy–assisted ERCP was attempted but failed because of the nonvisible anastomotic site (A, fluoroscopic image, B, endoscopic image).
Figure 3.
A, EUS-guided hepaticogastrostomy (EUS-HGS) performed with use of a 19G needle. B, Attempt to pass an antegrade guidewire through the EUS-HGS route into the stricture of the biliojejunal anastomotic site was not possible.
Figure 4.
Stent placement in endoscopic ultrasound-guided hepaticogastrostomy. An 8F plastic stent (Through Pass Type IT, Gadelius Medical) was placed from the stomach into the intrahepatic bile duct for biliary decompression (A, fluoroscopic image, B, endoscopic image).
Figure 5.
A, Second attempt to pass an antegrade guidewire through the endoscopic ultrasound-guided hepaticogastrostomy (EUS-HGS) route into the stricture of the biliojejunal anastomotic site was not possible. B, A 10F plastic stent (Through Pass, Gadelius Medical) was placed for dilation of the EUS-HGS route to allow smooth insertion of a digital per-oral cholangioscope.
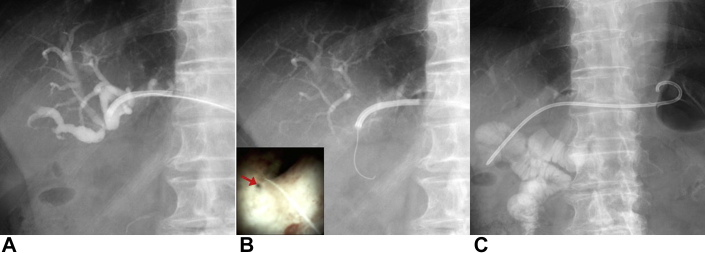
Figure 6.
Recanalization after biliojejunostomy by use of a new digital per-oral cholangioscope (DCPS) through the hepaticogastrostomy route. A, The DPCS was inserted though the endoscopic ultrasound-guided hepaticogastrostomy route. B, A 0.025-inch guidewire could pass through the stricture of the biliojejunal anastomotic site (red arrow) under DPCS guidance. C, An 8F plastic stent (Through Pass Type IT, Gadelius Medical) could be placed from the stomach to the jejunum through the anastomotic site.
Disclosure
All authors disclosed no financial relationships relevant to this publication.
Footnotes
Written transcript of the video audio is available online at www.VideoGIE.org.
Supplementary data
Recanalization after biliojejunostomy using a new digital per oral cholangioscope through the hepaticogastrostomy route.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Recanalization after biliojejunostomy using a new digital per oral cholangioscope through the hepaticogastrostomy route.