Abstract
Purpose:
To review the nature of firecracker-related ocular injuries at a tertiary eye hospital in northern India following the firecracker ban and also to review the level of awareness among the victims.
Methods:
A cross-sectional observational study involving the patients presenting with firecracker-related ocular injuries from October 18 to 27, 2017 were assessed for demographic distribution, detailed ocular evaluation, and a questionnaire related to the awareness about the injuries.
Results:
A total of 68 patients were observed. Fifty patients (74.5%) were males. This year, a majority of patients were from outside Delhi. Uttar Pradesh constituted the most 38.23% of the patients followed by Haryana 30.88%, Delhi 23.5%, and Bihar 7.35%. Visual acuity varied from 6/6 to no perception of light. Open globe injury was observed in 56 patients (82.35%) who commonly had zone I injury. A significant number of patients (88.23%) were aware of firecracker-related injuries, and a large number of such injuries (58.8%) occurred in those who were not actively involved in the ignition of firecrackers but were in the vicinity.
Conclusion:
This year, following a ban, the number of firecracker-related ocular injuries reported from areas outside Delhi outnumbered as compared to within Delhi. However, firecracker-related ocular injuries are still a major cause of significant visual loss, especially involving the bystanders. Thus, firecracker-related celebrations should be monitored with a stringent protocol.
Keywords: Awareness, firecracker ban, ocular injuries
Ocular firecracker injuries are observed in large numbers during festival seasons in India. The nature of injuries varies from mild to grievous injury leading to profound visual loss (PL negative). A significant proportion of these injuries are seen in the pediatric age group. Loss of vision in children is of great concern as apart from the visual disability which will last throughout their life, it also affects their learning capability and lifestyle and causes psychological trauma to the children and their caretakers. The aim of this study is to evaluate the pattern of ocular injuries and geographic differences in injuries following the ban on firecrackers sale in Delhi this year and to assess the basic level of awareness related to firecracker injuries.
Methods
Patients following firecracker injury presenting to ocular emergency services at Dr. Rajendra Prasad Centre for Ophthalmic Sciences, AIIMS, New Delhi, from October 18 to 27, 2017 were included in the study. All patients underwent initial assessment for the nature of injuries by a single observer, and the following parameters were noted: age, sex, laterality, duration of injury, address of patient, visual acuity (VA) at presentation, zone of injury, slit lamp examination to note the details of cornea, anterior chamber, iris, and the lens. A dilated fundus examination was performed whenever feasible.
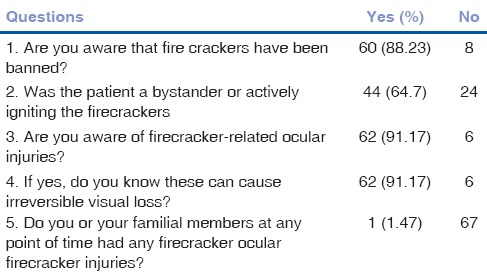
Patients in whom a detailed fundus evaluation was not possible due to media opacity, a gentle B scan ultrasound was performed over the closed eyelids by the same observer. After a complete ocular evaluation, every patient/caretaker were asked the following questions related to the awareness about firecracker-related ocular injuries: (1) Are you aware of firecrackers ban in the national capital? (2) Was the patient a bystander or actively igniting the firecracker. (3) Are you aware of firecracker-related ocular injuries? (4) If yes, do you know these can cause irreversible visual loss? (5) Do you or your family members at any point in time have had any firecracker ocular firecracker injuries? All patients received appropriate surgical or medical therapy at our ocular emergency.
Results
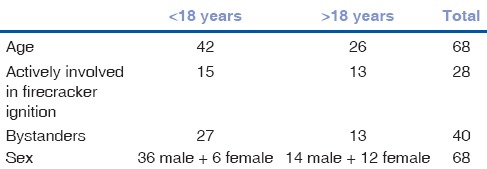
During a 10-day observation period, a total of 68 patients presented with firecracker-related ocular injuries, varying from simple conjunctival hemorrhage to partial autoevisceration [Fig. 1]. Fifty patients were males. The age varied from 6 years to 60 years with a mean age of 16 years. Forty-two (61.76%) patients were < 18 years old [Table 1]. The duration of the injury and the first medical attention varied from 30 min to 24 h with the median being 4 h. Patients within the national capital presented early (30 min to 2 h), whereas patients from rural areas of neighboring states sought medical attention at a variable time from few hours to 1 day at the nearby hospital, but the referred cases spent more time in seeking medical attention. The right eye was involved in 41 cases (60.29%), left eye in 25 cases (36.76%), and the injuries were bilateral in 2 cases (2.9%). Geographically, 26 patients (38.23%) belonged to Uttar Pradesh, 21 patients (30.88%) belonged to Haryana, 16 patients (23.5%) belonged to Delhi, and 5 patients (7.35%) belonged to Bihar [Graph 1].
Figure 1.

Ocular injuries varied from simple conjunctival hemorrhage (a), clear corneal perforation (b), closed globe injury with hyphema (c), corneal edema (d), eyelid abrasion (e), full-thickness eyelid laceration (f), diffuse facial burns with bilateral cornea involvement (g), to partial autoevisceration (h and i)
Table 1.
Demographic profile
Graph 1.

Geographical distribution
VA varied from no perception of light to 6/6 on Snellen's VA charting. Nine patients (13.23%) had a VA between 6/12 and 6/6, ten patients (14.70%) had a VA between 6/36 and 6/18, twenty-six patients (38.23%) had VA between hand movement close to face to 6/60, twenty patients (29.41%) had VA of perception of light positive to hand movement close to face, and three patients (4.41%) denied perception of light [Graph 2].
Graph 2.
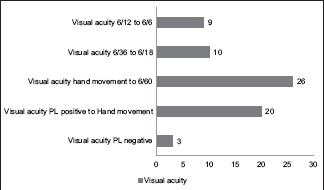
Visual acuity at presentation
Slit lamp biomicroscopic anterior segment findings according to Birmingham Eye Trauma Terminology System included open globe injury in 56 patients (82.35%) and closed globe injury in 12 patients (17.65%). Within the category of open globe injuries, forty-six patients had globe rupture due to high velocity injuries, ten patients had full-thickness laceration due to foreign bodies, and among them, the foreign bodies were superficial in two patients and intraocular in eight patients. In cases of closed globe injuries, eight patients had contusion injuries such as hyphema of varying grades with glaucoma and lamellar laceration in the form of conjunctival laceration in four patients [Graph 3]. Similarly, in term of zones, thirty-six patients (64%) had zone I injury, fourteen patients had (25%) zone II, and six patients (11%) had zone III injuries [Graph 4]. Adnexal injuries included simple skin abrasion in 6 patients, full-thickness eyelid laceration not involving the canalicular system in 3 patients, and involvement of the canaliculus in 1 patient. Periorbital bony injuries were not noted in any of the patients.
Graph 3.
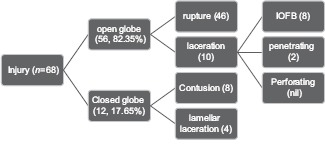
Pattern of ocular injuries according to Birmingham Eye Trauma Terminology System classification
Graph 4.
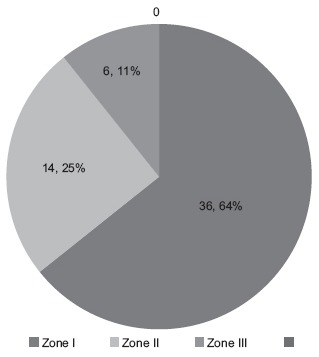
Zone-wise ocular injury categorization
Posterior segment was not visible on indirect ophthalmoscopy in 62 patients, whereas in remaining six patients, a satisfactory retinal examination was possible. The cause of media opacity included corneal edema, hyphema, cataract, and vitreous hemorrhage; all these patients underwent B scan ultrasound by a single observer. However, ultrasound was anechoic in 38 patients (out of 62), vitreous hemorrhage in 16 patients, retinal detachment in five patients and retained intraocular foreign body in eight patients, and choroidal detachment in two patients (some patients had multiple findings).
Based on the questionnaire about the awareness related to firecracker-related ocular injuries, sixty (88.23%) patients/caretakers were aware that selling firecrackers has been banned in the national capital. Forty-four patients (64.7%) were bystanders or who were not actively involved in igniting the firecrackers. Sixty-two patients (91.17%) were aware of firecracker-related ocular injuries which can cause irreversible visual loss. Only one patient (1.47%) had the history of firecracker injury in the family [Table 2].
Table 2.
Questionnaire related responses
In this same period of 10 days around Deepawali last year, our center treated 168 cases of firecracker-related ocular injuries. We do not have a detailed data analysis of previous year's cases. However, if we compare the number of cases alone, there seems to be a nearly 60% reduction in the number of cases.
Discussion
Firecracker-related ocular injuries are of great concern globally. There are few reported case series in literature analyzing the nature of firecracker-related injuries in India[1,2,3] as well as globally.[4,5,6,7,8,9,10,11] This study mainly focuses on the nature of ocular injuries, geographical location of the patient following firecracker ban in the national capital, and few questions related to awareness/precautions one should take while igniting the firecrackers. This year in October, the honorable Supreme Court of India prohibited the sale of firecrackers in the national capital (Delhi-NCR region) due to severe air pollution. In 2016 at our center, we encountered a total of 168 cases of ocular injuries due to firecrackers. Usually, this is the number of patients with firecracker injuries handled every year at our center. This year, the number of cases with ocular injuries has come down to a total of 68 patients. This is nearly a 59.52% reduction in firecracker-related ocular injuries. Furthermore, the majority of cases presenting this year were from outside the national capital (76.5%). In our observation, 40 patients (58.8%) were bystanders whereas 28 patients (41.17%) were actively involved in igniting the firecrackers. Out of these 40 bystanders, 27 patients were <18 years of age. Among the 28 patients who were actively involved in the ignition of firecrackers, 15 were <18 years old. Most common firecracker types were bombs, where following a sudden explosion, multiple tiny particles inflicted the patient's eyes, face, and other body parts. The second most common type was failed/leftover cracker manipulation by the children to reignite the same leading to an unpredictable explosion and ocular injury. Surprisingly, a higher number of the patients with eye injuries were bystanders. This is probably as the person igniting the firecracker usually turns his/her back toward the explosion while the surrounding people are caught unaware. Similarly, a significant number of children got injured while manipulating with the residual/homemade/leftover firecracker.
None of the patients were wearing any protective measures while igniting the firecrackers. However, based on the response to the questions, a significant number of patients/caretakers were aware of firecracker-related ocular injuries. Despite this, none was using any protective measures. To conclude, this study highlights the decrease in a number of firecrackers-related ocular injuries at our center following a ban on firecracker sale in the national capital, but at the same time, a significant number of cases were encountered from outside the national capital. These ocular injuries lead to a significant visual loss in many patients which may not be fully recoverable in their lifetime. Patients/caretakers were aware of firecrackers-related ocular injuries, but unfortunately, the injuries were seen significantly in bystanders and unmonitored children which is of great concern. These can be reduced by proper education and creating greater awareness in society through every possible medium regarding the potential vision-threatening complications of firecrackers.
Conclusion
A ban on individuals igniting firecrackers in a nonprofessional, unsupervised environment does seem to help reduce the number of accidents caused by firecrackers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kumar R, Puttanna M, Sriprakash KS, Sujatha Rathod BL, Prabhakaran VC. Firecracker eye injuries during deepavali festival: A case series. Indian J Ophthalmol. 2010;58:157–9. doi: 10.4103/0301-4738.60095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arya SK, Malhotra S, Dhir SP, Sood S. Ocular fireworks injuries. Clinical features and visual outcome. Indian J Ophthalmol. 2001;49:189–90. [PubMed] [Google Scholar]
- 3.Puri V, Mahendru S, Rana R, Deshpande M. Firework injuries: A ten-year study. J Plast Reconstr Aesthet Surg. 2009;62:1103–11. doi: 10.1016/j.bjps.2007.12.080. [DOI] [PubMed] [Google Scholar]
- 4.Chang IT, Prendes MA, Tarbet KJ, Amadi AJ, Chang SH, Shaftel SS, et al. Ocular injuries from fireworks: The 11-year experience of a US level I trauma center. Eye (Lond) 2016;30:1324–30. doi: 10.1038/eye.2016.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jing Y, Yi-Qiao X, Yan-Ning Y, Ming A, An-Huaai Y, Lian-Hong Z, et al. Clinical analysis of firework-related ocular injuries during spring festival 2009. Graefes Arch Clin Exp Ophthalmol. 2010;248:333–8. doi: 10.1007/s00417-009-1292-2. [DOI] [PubMed] [Google Scholar]
- 6.Kuhn FC, Morris RC, Witherspoon DC, Mann L, Mester V, Módis L, et al. Serious fireworks-related eye injuries. Ophthalmic Epidemiol. 2000;7:139–48. [PubMed] [Google Scholar]
- 7.Lee RT. Fire-cracker injury to the eyes in Hong Kong. Br J Ophthalmol. 1966;50:666–9. doi: 10.1136/bjo.50.11.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sacu S, Ségur-Eltz N, Stenng K, Zehetmayer M. Ocular firework injuries at new year's eve. Ophthalmologica. 2002;216:55–9. doi: 10.1159/000048298. [DOI] [PubMed] [Google Scholar]
- 9.Witsaman RJ, Comstock RD, Smith GA. Pediatric fireworks-related injuries in the United States: 1990-2003. Pediatrics. 2006;118:296–303. doi: 10.1542/peds.2006-0790. [DOI] [PubMed] [Google Scholar]
- 10.Smith GA, Knapp JF, Barnett TM, Shields BJ. The rockets’ red glare, the bombs bursting in air: Fireworks-related injuries to children. Pediatrics. 1996;98:1–9. [PubMed] [Google Scholar]
- 11.Vassilia K, Eleni P, Dimitrios T. Firework-related childhood injuries in Greece: A national problem. Burns. 2004;30:151–3. doi: 10.1016/j.burns.2003.09.019. [DOI] [PubMed] [Google Scholar]


