Abstract
Background:
Transthoracic Doppler echocardiographic examination is commonly performed to define the diastolic ventricular function since it is widely available, noninvasive, and inexpensive with respect to other diagnostic imaging modalities. However, data regarding age- and gender-matched reference values are scanty and sometimes conflicting. This study aims to explore the physiologic variations of left ventricular (LV) E/e' ratio as assessed in a large cohort of healthy adults and to investigate clinical and echocardiographic correlates.
Methods:
From June 2007 to February 2014, 1168 healthy Caucasian adults (mean age 45.1 ± 15.6 years) performed standard echocardiographic examination (transthoracic echocardiogram).
Results:
E/e' constantly increases across all the age classes (P < 0.0001, analyses of variance both for males and females) with a strong statistically significant linear positive correlation with age. Stepwise multiple linear regression analysis identified age (P < 0.0001), LV mass (P < 0.001), LV end-diastolic volume (P < 0.01), and left atrial volume (P < 0.001) as the only independent determinants of E/e' ratio (model R2 = 0.54, P < 0.0001).
Conclusions:
In healthy subjects, transmitral E velocity to e' ratio changes in relation to the age: it increased with a statistically significant correlation in individuals older than 60 years. Hence, differences related to demographic and anthropometric measurements may potentially develop a misclassification of otherwise normal individuals when established on dichotomically suggested normal reference values. Our study can demonstrate that it is indispensable to apply specific cutoff related to the age and gender to properly assess LV diastolic function.
Keywords: Diastole, E/e', echocardiography, healthy adults, pulsed Doppler, reference ranges, tissue Doppler
INTRODUCTION
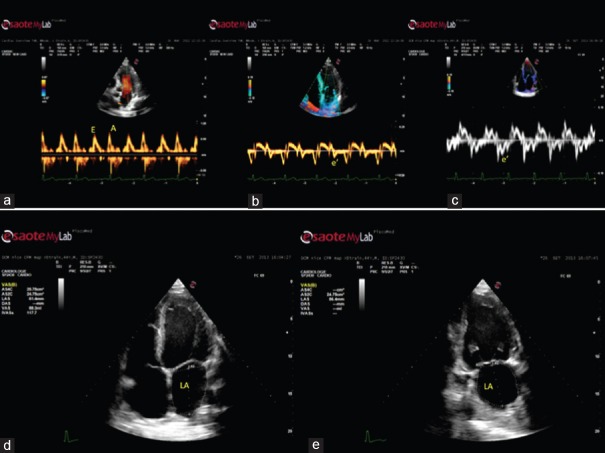
The evaluation of left ventricular (LV) diastolic function is considered an essential part of a complete echocardiographic examination.[1] Abnormalities of LV diastolic function have been described as part of the normal aging process, resulting from intrinsic myocardial changes due to an increased LV stiffness and impaired relaxation capacity of the LV.[2] Increased filling pressures should be considered as the principal feature related to continuous and dynamic age-related diastolic variation[3] that even in a preclinical phase is related to the development of heart failure and is predictive of all-cause mortality.[4,5] On the other hand, in patients presenting with dyspnea, the finding of increased LV diastolic pressures associated with a normal ejection fraction allows to identify a heart failure with preserved LV systolic function.[6] Early diastolic mitral annulus velocity (e') estimated by tissue Doppler (TD) and the ratio of the transmitral early peak velocity (E) by pulsed wave Doppler over e' (E/e') are the two key parameters for grading a diastolic dysfunction as they represent a reliable noninvasive surrogate for LV diastolic pressures.[7] In particular, the recent 2016 European Association of Cardiovascular Imaging/American Society of Echocardiography (EACVI/ASE) recommendations advise four variables for diagnosing diastolic dysfunction: annular e' velocity (septal e' <7 cm/s, lateral e' <10 cm/s), average E/e' ratio >14, left atrial (LA) maximum volume index >34 mL/m2, and peak tricuspid regurgitation velocity (TRV) >2.8 m/s[8] [Figure 1].
Figure 1.
Echocardiographic diastolic measurements in healthy subjects. The recent 2016 European Association of Cardiovascular Imaging/American Society of Echocardiography recommendations advise four variables for diagnosing diastolic dysfunction: annular e' velocity (septal e' <7 cm/s, lateral e' <10 cm/s), average E/e' ratio >14 (a-c panels), left atrial maximum volume index >34 mL/m2, (d-e panels), and peak tricuspid regurgitation velocity >2.8 m/s
As a result, age- and gender-matched reference values may be of paramount utility in a complete diastolic function assessment to identify and evaluate echocardiographic Doppler parameters in normal versus abnormal setting.
Therefore, this study aims to delineate the physiologic modifications related to age of LV E/e' ratio as assessed by standard Doppler echocardiography in healthy adults and to define the correlation between clinical and echocardiographic data.
METHODS
Study population
From June 2007 to February 2014, 1270 adults without cardiovascular risk factors and/or known cardiac pathologies performed an echocardiographic examination to echo-laboratories of the Division of Cardiology, “Cava de' Tirreni-Amalfi Coast,” University Hospital of Salerno, Luigi Vanvitelli University of Naples, and of the Department of Cardiology and Emergency Medicine of San Antonio Hospital, San Daniele del Friuli, Udine, Italy. Deliberately or for workability assessment, the individuals were evaluated about own risk of cardiovascular pathologies through a form to investigate history, cardiovascular risk conditions, and lifestyle.[9] In agreement with exclusion criteria, 79 individuals were not included: two coronary artery disease, 11 systemic arterial hypertension, four diabetes mellitus, nine body mass index >30 kg/m2, seven mild valvular insufficiency (three mitral, two aortic, and two tricuspid), two aortic stenosis, four bicuspid aortic valves, one hypertrophic cardiomyopathy, one aortic root dilation, one dilated cardiomyopathy, eight use of pharmacological therapy (hyperlipidemia, breast cancer, thyroid, gotta, and prostate disease), 20 elite athletes, and nine poor-quality echocardiographic examination. Moreover, 23 of the initially checked patients denied the enrollment in the echocardiographic protocol. Hence, the final study group was represented by 1168 healthy adults (mean age 45.1 ± 15.6 years, range 16–92; 555 [47.5%] men).[9]
Imaging protocol
Standardized transthoracic echocardiographic (TTE) examination and Doppler study were realized using feasible equipment (MyLab Alpha, Esaote, Florence, Italy; Vivid 7 or Vivid E9, GE Healthcare, Milwaukee, USA). Pulsed and continuous-wave Doppler examinations were performed both on the left and on right cardiac valves (mitral and aortic valves, tricuspid and pulmonary valves, respectively). All examinations were evaluated offline by two independent observers, and detailed measures were determined.
M-mode and B-mode measurements
M-mode parameters (LV diastolic and systolic diameters, interventricular septum, and posterior wall thickness) were estimated in parasternal long-axis section. LV mass was determined as the Penn convention[10] and related to height (LV mass index [LVMI]) (Cornell adjustment).[11]
Right ventricular end-diastolic dimensions were determined calculating basal right ventricular diameter from the apical four-chamber section at end-diastole. Tricuspid annular plane systolic excursion (TAPSE), considered as a parameter related to right ventricular longitudinal systolic movement, was performed putting the transducer on apical four-chamber section with M-mode cursor placed on the tricuspid annulus and determining the distance enclosed by end-diastolic and end-systolic longitudinal excursion (in mm).[12]
Color Doppler analysis
Doppler-derived LV diastolic inflow was performed in apical four-chamber section putting the sample volume on the tip level.
The LV diastolic parameters measured are the following:
E and A peak velocities and their ratio E/A
E-wave deceleration time
Using TD, the early (e') diastolic velocities were assessed at the septal and lateral insertion of the annulus of mitral valve, and the average value between two measurements was determined.
As a rule, the sample volume should be collocated at or 1 cm to the septal and lateral insertion place of the mitral leaflets and modified as necessary (usually 5–10 mm) including the longitudinal movement of mitral valve annulus occurring in both systole and diastole. Mitral E velocity, performed considering the influence of relaxation (i.e., the E/mean e' ratio), was determined to evaluate LV filling pressures[13] [Figure 2].
Figure 2.
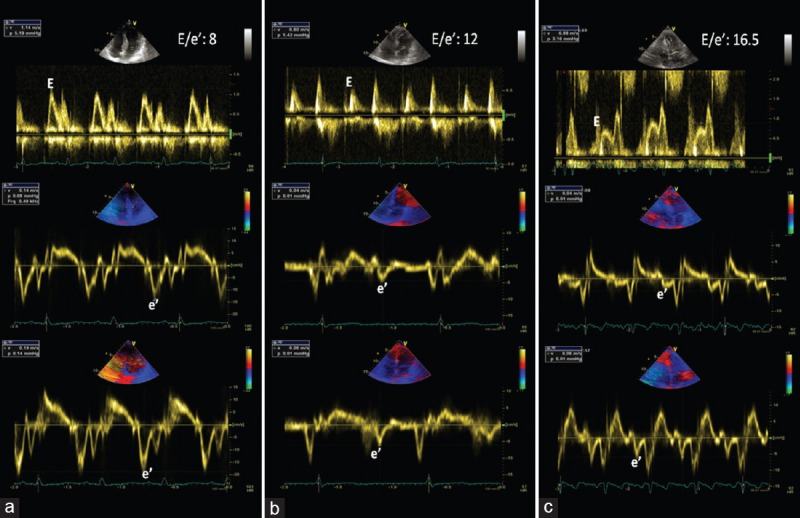
Echocardiographic diastolic measurements in three healthy subjects. (a) 25-year-old-female; (b) 58-year-old male; (c) 81-year-old female
Moreover, LV stroke volume (SV) was determined considering the product of LV outflow tract area and outflow tract time–velocity integral.[14] Furthermore, pulmonary artery systolic pressure (sPAP) was measured with classical formulas.[15]
Statistical analysis
All the analyses were determined using Statistical Package for social science SPSS for Windows release 21.0 (Chicago, IL, USA). Variables were considered as mean ± standard deviation (SD). Analyses of variance (ANOVA) as Newman–Keuls post hoc test for multiple comparisons were realized to determine differences occurring among the groups. Correlation test according to Pearson's method and Spearman's rank correlation coefficient was performed to determine univariate relations between continuous and/or binary variables. To establish in healthy adults independent determinants of E' and E/e' which were statistically significative, their individual relationship with clinically relevant and echocardiographic parameters was performed by multivariable linear regression analysis.
The subsequent variables were enclosed within the analysis:
Clinical data including age, gender, body mass index, and blood pressure (BP)
TTE parameters (LV volumes, LVMI, LV SV, LV ejection fraction, Doppler transmitral and transtricuspid inflow measurements, and sPAP).
The selection of these variables was determined by their clinical relevance and potential effect on diastolic function, as documented according to the previous reports. Variable choice was determined according to the multivariable linear regression, and it was performed as an interactive step by step backward elimination method. On every occasion, the one variable with the highest P value (according to Wald statistics) was excluded. To reduce the inflation of the Type 1 error percentage due to multiple testing, the statistical significance was fixed at two-sided P < 0.01.
Reproducibility of calculations was performed in all the patients. The readers (physicians) blindly reevaluated all examinations to minimize the intrareader reproducibility estimation. Intra- and interobserver variability was investigated applying Pearson's bivariate two-tailed correlations and Bland–Altman method. Correlation coefficients, mean discrepancy (bias), and limits of agreement (mean difference ± 1.96 SDs of the mean difference) were described.
RESULTS
Demographic parameters of the study population are described in Tables 1 and 2. Men were younger, heavier, and taller with respect to women. Moreover, our study showed that men have higher systolic and diastolic BP but lower heart frequency than women.
Table 1.
Demographic characteristics of the study population
| Overall (n=1168) | Male (n=555) | Female (n=613) | P (male vs. female) | |
|---|---|---|---|---|
| Age, years (range) | 45.40±15.60 (12.00-92.00) | 44.10±15.70 (16.00-91.0) | 46.00±15.40 (12.00-92.00) | 0.075 |
| Height, cm (range) | 168.67±9.5 (144.00-198.00) | 175.50±7.10 (150.00-198.00) | 162.40±6.70 (144.00-184.00) | 0.0001 |
| Weight, kg (range) | 69.70±12.08 (41.00-113.00) | 77.30±10.40 (45.00-113.00) | 62.70±8.80 (41.00-92.00) | 0.0001 |
| BMI, kg/m2 (range) | 24.40±3.10 (16.71-32.89) | 25.10±2.80 (16.71-31.83) | 23.80±3.24 (16.85-32.89) | 0.0001 |
| BSA, m2 (range) | 1.79±0.19 (1.06-2.76) | 1.92±0.16 (1.06-2.60) | 1.67±0.14 (1.30-2.76) | 0.0001 |
| Systolic BP, mmHg (range) | 123.90±12.15 (84.00-160.00) | 126.10±10.90 (90.00-150.00) | 121.90±12.80 (84.00-160.00) | 0.0001 |
| Diastolic BP, mmHg (range) | 76.20±8.67 (44.00-98.00) | 77.40±8.60 (50.00-98.00) | 75.10±8.60 (44.00-95.00) | 0.0001 |
| Mean BP, mmHg (range) | 92.10±8.83 (57.33-113.33) | 93.60±8.20 (67.00-113.30) | 90.70±9.10 (57.33-113.33) | 0.0001 |
| HR, bpm (range) | 71.00±11.78 (35.00-105.00) | 68.20±12.10 (38.00-105.00) | 73.20±10.97 (35.00-102.00) | 0.0001 |
BMI=Body mass index, BSA=Body surface area, BP=Blood pressure, HR=Heart rate
Table 2.
Study population according to age and sex
| Age (years) | <39 | 40-49 | 50-59 | >60 |
|---|---|---|---|---|
| Overall | 445 | 265 | 266 | 204 |
| Female | 208 | 128 | 116 | 91 |
| Male | 238 | 137 | 150 | 113 |
Left and right heart parameters
On TTE examination [Table 3], the overall male study population had higher LV systolic and diastolic volumes, higher LV mass, and higher LV ejection fraction. Furthermore, LA volumes were bigger in male with respect to female. On the other hand, no differences were documented calculating LV E/A ratio and cardiac output/cardiac index, while E/e' ratio appeared to be higher in women versus men. Conversely, TRV, estimated sPAP, and TAPSE were higher in males with respect to females [Table 4].
Table 3.
Left ventricular architecture and function
| Overal (n=1168) | Male (n=555) | Female (n=613) | P (male vs. female) | |
|---|---|---|---|---|
| LA volume index, ml/m2 (range) | 20.44±5.67 (9.00-46.00) | 20.83±6.106 (9.00-46.00) | 20.08±5.234 (9.00-40.00) | 0.001 |
| Relative wall thickness (range) | 0.36±0.07 (0.20-0.61) | 0.36±0.06 (0.20-0.61) | 0.37±0.06 (0.21-0.59) | 0.794 |
| LVM index, g/m2 (range) | 89.12±21.31 (41.65-193.55) | 97.11±21.28 (42.14-193.55) | 81.89±18.81 (41.65-150.51) | 0.001 |
| LV ED volume, ml (range) | 80.51±25.85 (41.00-158.00) | 94.68±25.81 (47.00-158.00) | 67.73±18.06 (41.00-139.00) | 0.0001 |
| LV ES volume, ml (range) | 29.45±11.08 (11.00-72.00) | 34.74±11.67 (16.00-72.00) | 24.69±7.93 (11.00-59.00) | 0.0001 |
| LV EF, % (range) | 63.97±5.71 (47.00-79.00) | 63.74±6.07 (47.00-79.00) | 64.17±5.3 (51.00-79.00) | 0.003 |
| E/A ratio (range) | 1.44±0.65 (0.00-6.00) | 1.47±0.634 (0.00-5.00) | 1.42±0.66 (0.00-6.00) | 0.478 |
| E/E’ ratio (range) | 6.5±3.7 (2.6–16.5) | 6.25±2.7 (2.6-16.20) | 6.8±3.9 (2.9-16.5) | 0.015 |
| LVOT diameter, mm (range) | 20.06±1.99 (16.00-30.00) | 21.2±1.86 (16.00-30.00) | 19.02±1.486 (16.00-24.00) | 0.0001 |
| SV/BSA, ml/m2 (range) | 37.218.09 (18.00-73.00) | 8.49±0.36 (18.00-72.00) | 36.97±7.71 (18.00-73.00) | 0.03 |
| Cardiac output, L (range) | 4.67±1.24 (2.71-9.62) | 4.86±1.282 (2.71-9.62) | 4.50±1.18 (2.84-9.47) | 0.454 |
| Cardiac index, L/min/m2 (range) | 2.62±0.68 (1.73-5.74) | 2.53±0.65 (1.83-5.74) | 2.70±0.70 (1.73-5.74) | 0.065 |
LA=Left atrium, LV=Left ventricle, ED=End diastolic, ES=End systolic, LVM=Left ventricular mass, EF=Ejection fraction, IVS=Interventricular septum, FS=Fraction shortening, DeCT=Mitral deceleration time, CW=Continuous wave, PuW=Pulsed wave, PW=Posterior wall, SV=Stroke volume, BSA=Body surface area, LVOT=Left ventricular outflow tract
Table 4.
Right ventricular architecture and function
| Overall (n=1168) | Male (n=555) | Female (n=613) | P (male vs. female) | |
|---|---|---|---|---|
| TRV (range) | 1.96±0.39 (0.67-3.03) | 1.93±0.43 (0.67-3.03) | 1.98±0.34 (0.75-2.82) | 0.0001 |
| sPAP (range) | 20.99±5.95 (6.81-41.72) | 20.72±6.53 (6.81-41.72) | 21.23±5.37 (7.25-36.81) | 0.0001 |
| TAPSE (range) | 23.69±3.39 (17.00-38.00) | 24.16±3.69 (17.00-38.00) | 23.26±3.04 (17.00-35.00) | 0.0001 |
| RV base (range) | 33.29±3.61 (20.00-46.00) | 34.78±3.36 (21.00-46.00) | 32.07±3.34 (20.00-39.00) | 0.951 |
| E/A ratio (range) | 1.52±0.61 (0.54-6.60) | 1.55±0.61 (0.54-4.83) | 1.50±0.61 (0.60-6.60) | 0.498 |
TRV=Tricuspid regurgitation velocity, sPAP=Systolic pulmonary artery pressure, TAPSE=Tricuspid annular plane systolic excursion, RV=Right ventricle, LAP=Left atrial pressure, RA=Right atrium
Left E/e' ratio
The ratio between E/e' constantly raises among all the age classes (P < 0.0001, ANOVA for both males and females) [Figure 3] with a strong statistically significant linear positive correlation with age [Table 5]. In Figure 4, E/e' values are plotted with age.
Figure 3.
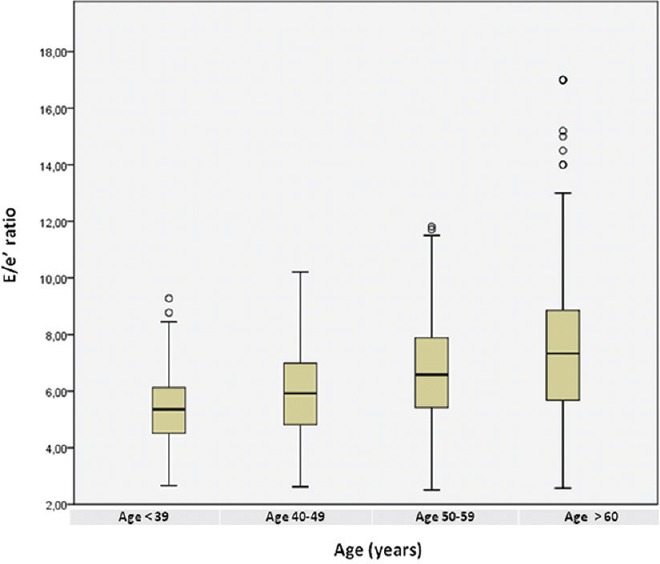
Boxplots of distribution of E/e' ratio measurements according to age in the overall study population
Table 5.
Reference ranges according to sex and age of E/e’ mean, septal and lateral ratios
| Age | All subjects | P* | ||||
|---|---|---|---|---|---|---|
| <39 | 40-49 | 50-59 | >60 | |||
| E/e’ mean | ||||||
| Overall (range) | 5.35±1.3 (2.7-9.2) | 5.94±1.6 (2.8-10.3) | 6.87±3.1 (2.9-12.8) | 7.82±3.7 (3.2-17) | 6.5±3.7 (2.6-17) | 0.0001 |
| Male (range) | 5.13±1.4 (2.7-9) | 5.78±1.4 (2.8-9.8) | 6.75±3.4 (2.9-11.5) | 7.6±4.2 (3.22-16.2) | 6.25±2.7 (2.6-16.2) | 0.0001 |
| Female (range) | 5.52±1.8 (3-9.2) | 6.12±1.9 (3.3-10.3) | 7.12±2.8 (2.9-12.8) | 7.9±3.7 (3.5-17) | 6.8±3.9 (2.9-17) | 0.0001 |
| E/e’ septal | ||||||
| Overall (range) | 5.35±1.3 (2.7-9.2) | 5.94±1.6 (2.8-10.3) | 6.87±3.1 (2.9-12.8) | 7.82±3.7 (3.2-17) | 6.5±3.7 (2.6-17) | 0.0001 |
| Male (range) | 5.13±1.4 (2.7-9) | 5.78±1.4 (2.8-9.8) | 6.75±3.4 (2.9-11.5) | 7.6±4.2 (3.22-16.2) | 6.25±2.7 (2.6-16.2) | 0.0001 |
| Female (range) | 5.52±1.8 (3-9.2) | 6.12±1.9 (3.3-10.3) | 7.12±2.8 (2.9-12.8) | 7.9±3.7 (3.5-17) | 6.8±3.9 (2.9-17) | 0.0001 |
| E/e’ lateral | ||||||
| Overall (range) | 5.35±1.3 (2.7-9.2) | 5.94±1.6 (2.8-10.3) | 6.87±3.1 (2.9-12.8) | 7.82±3.7 (3.2-17) | 6.5±3.7 (2.6-17) | 0.0001 |
| Male (range) | 5.13±1.4 (2.7-9) | 5.78±1.4 (2.8-9.8) | 6.75±3.4 (2.9-11.5) | 7.6±4.2 (3.22-16.2) | 6.25±2.7 (2.6-16.2) | 0.0001 |
| Female (range) | 5.52±1.8 (3-9.2) | 6.12±1.9 (3.3-10.3) | 7.12±2.8 (2.9-12.8) | 7.9±3.7 (3.5-17) | 6.8±3.9 (2.9-17) | 0.0001 |
*ANOVA by Newman–Keuls post hoc test for multiple comparisons was performed to estimate differences between groups. ANOVA=Analysis of variance
Figure 4.
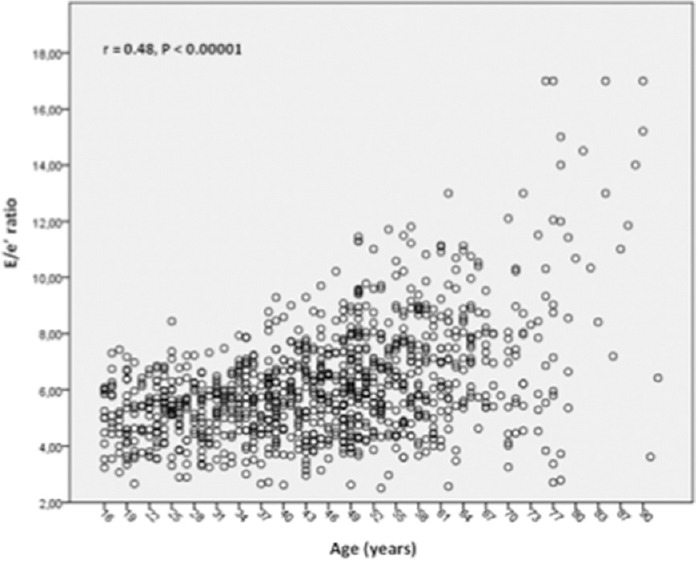
Scatterplots between age and E/e' ratio in the overall population of healthy subjects
On univariate analysis, E/e' with a statistically significant correlation was related to age (r = 0.48, P < 0.00001) [Figure 3], female gender (r = 0.28, P < 0.05), body surface area (r = 0.21, P < 0.01), LA volume (r = 0.4, P < 0.00001), LV end-diastolic volume (r = 0.34, P < 0.001), and LVMI (r = 0.38, P < 0.0001).
By the use of stepwise multiple linear regression analysis, age (beta-coefficient = 0.39, P < 0.0001), LV mass (beta-coefficient = 0.29, P < 0.001), LV end-diastolic volume (beta-coefficient = 0.24, P < 0.01), and LA volume (beta-coefficient = 0.31, P < 0.001) could be considered as the only independent parameters to determine E/e' ratio (model R2 = 0.54, P < 0.0001).
Reproducibility of measurements
Our inter- and intra-observer variability to assess transmitral E velocity to e' ratio was good. For interobserver variability, we reported in detail the following: r = 0.88; P < 0.00001 (as Pearson's correlations); mean bias = 1.1 ± 0.4; and limits of agreement = 0.4, 1.8 (evaluated through Bland–Altman analysis).
Similarly, for intra-observer variability, we determined: r = 0.90; P < 0.00001 (as Pearson's correlations); mean bias = 0.8 ± 0.3; and limits of agreement = 0.3, 1.5 (evaluated through Bland–Altman analysis).
DISCUSSION
Transthoracic Doppler echocardiographic examination is usually performed to define the diastolic ventricular function because it is widely available, noninvasive, and inexpensive with respect to other diagnostic imaging modalities.[16,17] A recent Joint Task Force of the EACVI and the ASE published an updated recommendation for the evaluation of LV diastolic function in 2016. The primary goal of this update was to simplify the approach and increase the utility of the guidelines in daily clinical practice [Figure 1].[8] Even if sex- and ethnic-appropriate echocardiographic reference values have been recently indicated for many measurements of LA and LV size,[18] the spectrum of age-associated diastolic parameters has not been fully investigated and validated in healthy individuals.
Our study presents for the first time an exhaustive data report to define reference range for normal e' value and E/e' ratio according to age and gender in a large cohort of healthy adults.
E/e' ratio: Previous studies
In a milestone study, Sohn et al. distinguished patients with pseudonormal from normal filling based on e' velocity <8.5 cm/s and e'/a' ratio <1, reporting a sensitivity of 88% and a specificity of 67%, respectively.[19]
Moreover, in 1997, Nagueh et al. reported that e' can identify relaxation modifications not related to filling pressures and, as a consequence, discriminated the pseudonormal group from the normal group. What's more, they described that the ratio E/e' was related to mean pulmonary capillary wedge pressure (PCWP) with a statistically significant correlation. As a result, this simple parameter can be considered as an indirect indicator of filling pressures[13,20] and a transmitral E velocity to e' ratio >10 identified a mean PCWP >15 mmHg with a sensitivity of 97% and a specificity of 78%, respectively.
De Sutter et al. in 2005 studied, in a small sample of subjects including patients with hypertension and previously documented LV hypertrophy, the effect of aging on echo estimated LV filling pressure. In a multivariate analysis, e' was only predicted by age showing a steep decrease with age while E/e' was predicted by age and gender but not by LVMI. Transmitral E velocity to e' ratio raised with age, in details every decade from 7.8 for age 18–35 years to 10.9 for age ≥75 years (P < 0.0001).[21]
In this study, an E/e' ratio >10 was frequently encountered in normal individuals < 65 years (15% in the group <45 years, 26% in the group 45–54 years, and 48% in the group 55–64 years). Moreover, most asymptomatic individuals ≥65 years showed a ratio >10 (63% for age 65–74 years and 71% for age >74 years), suggesting that cutoff is probably too low for the evaluation of elderly subjects. In addition, transmitral E velocity to e' ratio >15 was not frequently reported in normal asymptomatic individuals aged <65 years. However, in individuals ≥65 years, an E/e' ratio >15 was more frequently encountered (14% for age 65–74 years and 24% for age >74 years). Especially in women older than 74 years, the normal data suggest that possibly an even higher cutoff for E/e' should be used.
According to the previous 2009 Guidelines EAE/ASE concerning the Evaluation of LV Diastolic Function by Echocardiography, the criteria to define an abnormal LV diastolic dysfunction are based also on evaluation of TD annular early diastolic velocities:[8,20] age determines both normal values of TD-derived velocities and similarly other indices of LV diastolic function. In fact, in relation to age, e' velocity decreases, whereas a' velocity and transmitral E velocity to e' ratio raise. Hence, the authors assumed that adopting the septal transmitral E velocity to e' ratio, a ratio <8 is usually related to normal LV filling pressures, while a ratio >15 is correlated to increased filling pressures.[22,23] An analysis including gender- and age-matched reference values was not presented.
Recently, the NORRE study contributed to give more exhaustive reference values of Doppler parameters to estimate heart physiologic function related to age and gender in 449 European volunteers between 20s and 75s.[24] It was demonstrated that an E wave velocity is higher in female than in males with no differences in E/A ratio and E wave deceleration times. Moreover, while there was a gradual decrease with age concerning E and e' wave velocities, A wave and E wave deceleration time, and E/e' ratio increase.
In the subgroup of hypertensive subjects, ESH/ESC Guidelines for management for arterial hypertension recommended the use of echocardiography for detecting diastolic dysfunction.[25] Typically, in hypertensive heart conditions, by TD analysis, both the reduction of early diastolic velocity (e') and often the decrease of the septal e' more than the lateral e' are described.
According to the recent 2016 Joint Task Force of EACVI/ASE,[8] to diagnose and to establish the grade of diastolic alteration, it is necessary to calculate e' (average of measurements on septal and lateral mitral annulus), the E/e' ratio, and LA dimensions. The prognostic information related to e' velocity is well known also in the hypertensive conditions, and transmitral E velocity to e' ratio ≥13 is considered to improve cardiac risk conditions in hypertensive subjects, independent of LV mass and relative wall thickness.
Our group previously underlined that in healthy individuals also, LA dimensions change related to age and with a statistically significant correlation and are greater in subjects older than 50 years[26] confirming in a larger population previous data and suggesting that this finding might be the morphological physiologic expression of chronic diastolic dysfunction.[27,28]
Peculiarity of this study
we describe for the first time in a large sample of 1.168 healthy adults age- and sex-related cutoff values of transmitral E velocity to e' ratio performed by standard TTE examination and delineate the effect of distinct clinical and echocardiographic determinants.
In our study, E/e' parameters were higher in many healthy subjects over 60 years [Table 5 and Figure 3]. In detail, E/e' measurements higher than the actually considered reference values of normality (>10) were detected in almost 40% of subjects over 60 years.
Moreover, multivariate analysis provided supplementary information related to these parameters by regulating for several confounders, selected in relation to the heart physiologic function. Gender should not be considered as an independent predictor of E/e' ratio. Conversely, in the pooled sample, stepwise multiple linear regressions analyses established that age, LV mass, LV end-diastolic volume, and LA volume should be considered as powerful independent predictors of E/e' ratio. The underlying factors which can determine these modifications are still discussed.[26,27,28] Due to the presence of LV diastolic dysfunction, occurring typically in older subjects, LV stiffness and pressure raise together with an increment in E/e' ratio.[2,3,4] Hence, LA pressure increases to permit effective LV filling, and the elevated tension of atrial thin wall can determine increased atrial dimensions and stretch of the atrial myocardium.[26]
Moreover, old age has been related to impaired LA passive emptying function, and consequently, LA dilation provides to augment atrial ejection force and blood ejection occurring in LA systole, determining a relevant compensatory mechanism in most elderly subjects.[29]
In addition, the degree of ventricular remodeling (i.e., LV end-diastolic volume), mitral regurgitation, and the existence of atrial fibrillation have been considered as important, well-defined determinants of E/e' ratio.[16] As a result, we can assert that in most of healthy subjects over 60 years, the increment of E/e' ratio could be evaluated as a physiologic effect of age-linked LV remodeling and of LV diastolic progressive impairment.
Limitations
In this study, we include only Caucasian individuals so that these results cannot realistically be applied to other ethnic population. Moreover, we are not able to correlate our findings to invasive measurements, but it would be unethical to submit healthy individuals to invasive procedures for this purpose.
Although all individuals appeared in good health, we cannot ignore the likelihood of subclinical disease such as coronary artery disease or cardiomyopathies, which may influence the assessment of systolic and diastolic measurements even if the selected sample size should minimize this risk.
In our study, we did not perform LA longitudinal strain derived from speckle tracking echocardiography, which is another parameter sensitive in estimating intracavitary pressures.[8] Further studies are needed about this evaluation in a large population of healthy individuals.
CONCLUSIONS
In healthy individuals, transmitral E velocity to e' ratio changes in relation to the age: it increases with a statistically significant correlation especially in individuals older than 60 years. In the overall population, multivariate analyses evidenced age, LV mass, LV end-diastolic volume, and LA volume as powerful independent predictors of E/e' ratio. Hence, differences related to demographic and anthropometric measurements may potentially develop a misclassification of otherwise normal individuals when established on dichotomically suggested normal reference values. As a consequence, when evaluating increased E/e' ratio values in healthy individuals, in addition to echocardiographic data such as LV and LA measurements, clinical parameters, such as age and gender, should always be considered in clinical practice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to thank Dr. Marco Maglione (Esaote, Florence, Italy) for his technical support during the study.
REFERENCES
- 1.Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–394. doi: 10.1016/j.echo.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Morley JE, Reese SS. Clinical implications of the aging heart. Am J Med. 1989;86:77–86. doi: 10.1016/0002-9343(89)90233-7. [DOI] [PubMed] [Google Scholar]
- 3.Brutsaert DL, Sys SU, Gillebert TC. Diastolic failure: Pathophysiology and therapeutic implications. J Am Coll Cardiol. 1993;22:318–25. doi: 10.1016/0735-1097(93)90850-z. [DOI] [PubMed] [Google Scholar]
- 4.Redfield MM, Jacobsen SJ, Burnett JC, Jr, Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: Appreciating the scope of the heart failure epidemic. JAMA. 2003;289:194–202. doi: 10.1001/jama.289.2.194. [DOI] [PubMed] [Google Scholar]
- 5.Kane GC, Karon BL, Mahoney DW, Redfield MM, Roger VL, Burnett JC., Jr Progression of left ventricular diastolic dysfunction and risk of heart failure. JAMA. 2011;306:856–63. doi: 10.1001/jama.2011.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2012;14:803–69. doi: 10.1093/eurjhf/hfs105. [DOI] [PubMed] [Google Scholar]
- 7.Arques S, Roux E, Luccioni R. Current clinical applications of spectral tissue Doppler echocardiography (E/e' ratio) as a noninvasive surrogate for left ventricular diastolic pressures in the diagnosis of heart failure with preserved left ventricular systolic function. Cardiovasc Ultrasound. 2007;5:16. doi: 10.1186/1476-7120-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, 3rd, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2016;17:1321–60. doi: 10.1093/ehjci/jew082. [DOI] [PubMed] [Google Scholar]
- 9.Vriz O, Aboyans V, D'Andrea A, Ferrara F, Acri E, Limongelli G, et al. Normal values of aortic root dimensions in healthy adults. Am J Cardiol. 2014;114:921–7. doi: 10.1016/j.amjcard.2014.06.028. [DOI] [PubMed] [Google Scholar]
- 10.Devereux RB, Reichek N. Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation. 1977;55:613–8. doi: 10.1161/01.cir.55.4.613. [DOI] [PubMed] [Google Scholar]
- 11.de Simone G, Daniels SR, Devereux RB, Meyer RA, Roman MJ, de Divitiis O, et al. Left ventricular mass and body size in normotensive children and adults: Assessment of allometric relations and impact of overweight. J Am Coll Cardiol. 1992;20:1251–60. doi: 10.1016/0735-1097(92)90385-z. [DOI] [PubMed] [Google Scholar]
- 12.Kaul S, Tei C, Hopkins JM, Shah PM. Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J. 1984;107:526–31. doi: 10.1016/0002-8703(84)90095-4. [DOI] [PubMed] [Google Scholar]
- 13.Nagueh SF, Sun H, Kopelen HA, Middleton KJ, Khoury DS. Hemodynamic determinants of the mitral annulus diastolic velocities by tissue Doppler. J Am Coll Cardiol. 2001;37:278–85. doi: 10.1016/s0735-1097(00)01056-1. [DOI] [PubMed] [Google Scholar]
- 14.Dubin J, Wallerson DC, Cody RJ, Devereux RB. Comparative accuracy of Doppler echocardiographic methods for clinical stroke volume determination. Am Heart J. 1990;120:116–23. doi: 10.1016/0002-8703(90)90168-w. [DOI] [PubMed] [Google Scholar]
- 15.Bossone E, D'Andrea A, D'Alto M, Citro R, Argiento P, Ferrara F, et al. Echocardiography in pulmonary arterial hypertension: From diagnosis to prognosis. J Am Soc Echocardiogr. 2013;26:1–4. doi: 10.1016/j.echo.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 16.Abbate A, Arena R, Abouzaki N, Van Tassell BW, Canada J, Shah K, et al. Heart failure with preserved ejection fraction: Refocusing on diastole. Int J Cardiol. 2015;179:430–40. doi: 10.1016/j.ijcard.2014.11.106. [DOI] [PubMed] [Google Scholar]
- 17.Gillebert TC, De Pauw M, Timmermans F. Echo-Doppler assessment of diastole: Flow, function and haemodynamics. Heart. 2013;99:55–64. doi: 10.1136/heartjnl-2012-301961. [DOI] [PubMed] [Google Scholar]
- 18.Echocardiographic Normal Ranges Meta-Analysis of the Left Heart Collaboration. Ethnic-specific normative reference values for echocardiographic LA and LV size, LV mass, and systolic function: The EchoNoRMAL study. JACC Cardiovasc Imaging. 2015;8:656–65. doi: 10.1016/j.jcmg.2015.02.014. [DOI] [PubMed] [Google Scholar]
- 19.Sohn DW, Chai IH, Lee DJ, Kim HC, Kim HS, Oh BH, et al. Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol. 1997;30:474–80. doi: 10.1016/s0735-1097(97)88335-0. [DOI] [PubMed] [Google Scholar]
- 20.Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr. 2009;10:165–93. doi: 10.1093/ejechocard/jep007. [DOI] [PubMed] [Google Scholar]
- 21.De Sutter J, De Backer J, Van de Veire N, Velghe A, De Buyzere M, Gillebert TC, et al. Effects of age, gender, and left ventricular mass on septal mitral annulus velocity (e') and the ratio of transmitral early peak velocity to e' (E/E') Am J Cardiol. 2005;95:1020–3. doi: 10.1016/j.amjcard.2005.01.021. [DOI] [PubMed] [Google Scholar]
- 22.Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, et al. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: A comparative simultaneous Doppler-catheterization study. Circulation. 2000;102:1788–94. doi: 10.1161/01.cir.102.15.1788. [DOI] [PubMed] [Google Scholar]
- 23.Marwick TH, Gillebert TC, Aurigemma G, Chirinos J, Derumeaux G, Galderisi M, et al. Recommendations on the use of echocardiography in adult hypertension: A report from the European Association of Cardiovascular Imaging (EACVI) and the American Society of Echocardiography (ASE) J Am Soc Echocardiogr. 2015;28:727–54. doi: 10.1016/j.echo.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 24.Caballero L, Kou S, Dulgheru R, Gonjilashvili N, Athanassopoulos GD, Barone D, et al. Echocardiographic reference ranges for normal cardiac Doppler data: Results from the NORRE study. Eur Heart J Cardiovasc Imaging. 2015;16:1031–41. doi: 10.1093/ehjci/jev083. [DOI] [PubMed] [Google Scholar]
- 25.Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: The task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) J Hypertens. 2013;31:1281–357. doi: 10.1097/01.hjh.0000431740.32696.cc. [DOI] [PubMed] [Google Scholar]
- 26.D'Andrea A, Riegler L, Rucco MA, Cocchia R, Scarafile R, Salerno G, et al. Left atrial volume index in healthy subjects: Clinical and echocardiographic correlates. Echocardiography. 2013;30:1001–7. doi: 10.1111/echo.12217. [DOI] [PubMed] [Google Scholar]
- 27.D'Andrea A, Riegler L, Cocchia R, Scarafile R, Salerno G, Gravino R, et al. Left atrial volume index in highly trained athletes. Am Heart J. 2010;159:1155–61. doi: 10.1016/j.ahj.2010.03.036. [DOI] [PubMed] [Google Scholar]
- 28.Ploumen MA, Baur LH, Streppel MJ, Lodewijks-van der Bolt CL, Winkens B, Winkens RA, et al. Age is an independent risk factor for left atrial dysfunction: Results from an observational study. Neth Heart J. 2010;18:243–7. doi: 10.1007/BF03091770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thomas L, Levett K, Boyd A, Leung DY, Schiller NB, Ross DL, et al. Compensatory changes in atrial volumes with normal aging: Is atrial enlargement inevitable? J Am Coll Cardiol. 2002;40:1630–5. doi: 10.1016/s0735-1097(02)02371-9. [DOI] [PubMed] [Google Scholar]