Abstract
Free-floating right heart thrombus (RHT) is an extreme medical emergency in the context of acute massive pulmonary embolism (PE). Despite the advances in early diagnosis, the management is still very debatable due to lack of consensus. We reported the case of a 66-year-old male, with a history of moderate renal dysfunction and dilated cardiomyopathy, who presented to the emergency department for acute dyspnea. His angiographic magnetic resonance imaging revealed bilateral extensive PE. Transthoracic echocardiography showed RHT with moderate right ventricular dysfunction and pulmonary hypertension. Venous Doppler of the lower extremities noted the presence of a floating clot in the right common femoral vein. The patient was managed successfully by thrombolytic therapy with tenecteplase. To the best of our knowledge, this is the first case report of RHT and PE from Lebanon. Published cases from Middle Eastern countries are scarse.
Keywords: Echocardiography, pulmonary embolism, right heart thrombus, thrombectomy, thrombolysis
INTRODUCTION
The concomitant presence of right heart thrombus (RHT) and pulmonary embolism (PE) is an extreme emergency.[1] The prevalence of RHT in the setting of PE is 4%–18%.[2,3] The mortality rate is increased beyond PE alone. Treatment options include surgical thrombectomy of the right atrium or the pulmonary artery and/or medical therapy such as thrombolysis and anticoagulation.[1,2,3,4] Among these options, thrombolysis is a fast readily available treatment that is showing promising outcomes.[5]
CASE REPORT
We report herein the case of a 66-year-old man with a history of noncomplicated ischemic stroke 2 years ago, and a stable dilated nonischemic cardiomyopathy. He presented to the emergency department of our tertiary care center for acute dyspnea that has been increasing progressively over the past 3 days. On admission, the patient was afebrile and his work up showed a mean arterial pressure of 85 mmHg, sinus tachycardia (110/min) and oxygen saturation on room air of 85%. The rest of the physical examination was unremarkable. Transthoracic echocardiography (TTE) using the commercially available machine (GE, Vivid E9 Vingmed Ultrasound, Horten, Norway) with the M5Sc-D probe showed large highly mobile right atrial thrombus protruding to the right ventricle [Figure 1 and Video 1], with moderate systolic right ventricular dysfunction (RVD) and pulmonary hypertension (pulmonary artery systolic pressure of 55 mmHg). We also noted global left ventricular hypokinesia (ejection fraction of 35%). PE was suspected, so he was given 5000 units bolus of unfractionated heparin, followed by continuous intravenous (IV) heparin infusion. Venous Doppler of the lower extremities showed the presence of a floating clot in the right common femoral vein extending for 5 cm to the right superficial femoral vein and to the sapheno-femoral junction.
Figure 1.

Transthoracic echocardiogram subcostal view showing a serpiginous highly mobile right atrial thrombus (black arrowheads)
Blood analysis revealed slightly positive Troponin-T value of 0.074 (n < 0.014 ng/ml) and high creatinine level of 2.1 (n < 1.3 mg/dl). Angiographic computed tomography (CT) of the chest could not be done due to moderate renal dysfunction, chest magnetic resonance imaging (MRI) showed signs of massive PE in proximal bilateral pulmonary arteries with extension to segmental and subsegmental arteries [Figure 2]. The patient was transferred to the cardiac surgical unit for thrombolysis. Weight optimized dose regimen of tenecteplase was given as an IV single bolus, and Vitamin K antagonist was started 24 h later.
Figure 2.
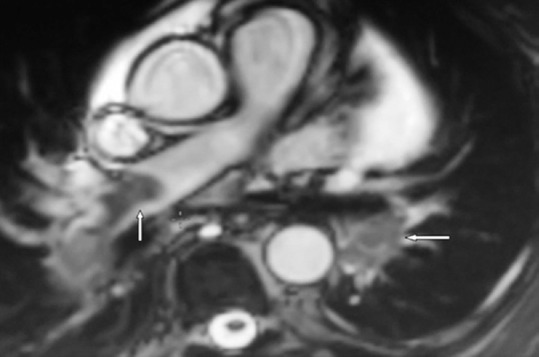
Chest magnetic resonance imaging showing embolism in the right and left main pulmonary arteries (white arrows)
Six hours after thrombolysis, repeated TTE revealed complete regression of the right atrial thrombus and improvement of the right systolic dysfunction and of pulmonary hypertension. Repeated Venous Doppler of the lower extremities showed marked resorption of the right common femoral vein thrombus. Chest MRI was performed 24 h postthrombolysis and revealed bilateral disappearance of the PE from the main pulmonary arteries [Figure 3]. Total body CT scan excluded the presence of underlying malignancy. Screening for thrombophilia was negative. The patient was discharged on day 7.
Figure 3.
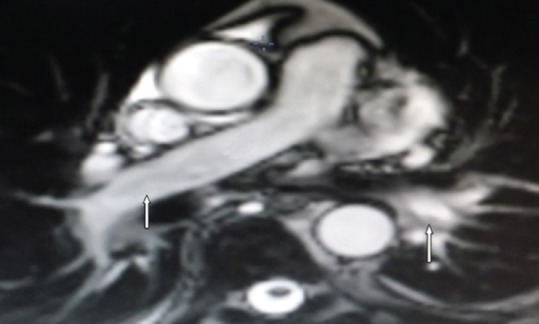
Chest magnetic resonance imaging showing marked resorption of the right and left main pulmonary artery embolism (white arrows)
DISCUSSION
The coexistence of RHT with acute PE is an extreme medical emergency. This combination carries a high mortality rate when compared to acute PE alone. The mortality rate was reported to be 27% and goes up to 100% with the absence of treatment.[1] The prevalence of RHT in the setting of acute PE is 4%–18%.[2] Three types of RHT have been described. Type A thrombi are captured in transit within the right cardiac cavities, morphologically serpiginous, highly mobile, and associated with deep vein thrombosis and PE. Type B thrombi are nonmobile, formed in situ and are associated with underlying cardiac abnormalities. Type C thrombi have intermediate characteristics of both Type A and Type B.
Therapeutic options include surgical embolectomy, thrombolysis, anticoagulation, or percutaneous retrieval technique [Table 1].[4] Successful surgical embolectomy, by exploration of the right heart and pulmonary arteries under cardiopulmonary bypass, has been widely used, mainly in hemodynamically unstable patients.[5] Good outcomes were reported in published articles on RHT and PE.[6,7,8,9,10,11,12] Lohrmann et al.[6] in their study reported the case of an RHT with bilateral proximal PE that has been treated with RHT thrombectomy and bilateral pulmonary endarterectomy. This type of treatment is not available in many centers; however, it should be considered in patients who have a contraindication for thrombolysis or ineffective thrombolysis.
Table 1.
Therapeutic options summary for studies on right heart thrombus-pulmonary embolism
| Study | Type of therapy | Outcome | |||
|---|---|---|---|---|---|
| Surgical embolectomy | Thrombolysis | Anticoagulation alone | Percutaneous retrieval techniques | ||
| Akili et al., 2013 | + | + | |||
| Ando et al., 2011 | + | + | |||
| Dzudovic et al., 2013 | + | + | |||
| Burns et al., 2009 | + | + | |||
| Cuccia et al., 1998 | + | + | |||
| D’Aloia et al., 2013 | + | + | |||
| Debney et al., 2011 | + | + | |||
| Eweda et al., 2011 | + | + | |||
| Fischer et al., 2013 | + | + | |||
| Hisatomi et al., 2013 | + | + | |||
| Huang et al., 2008 | + | + | |||
| Karabay et al., 2011 | + | + | |||
| Lampropoulos et al., 2013 | + | + | |||
| Lohrmann et al., 2014 | + | + | |||
| Momose et al., 2012 | + | + | |||
| Naeem et al., 2015 | + | + | |||
| Nkoke et al., 2015 | + | + | |||
| Pellegrini et al., 2012 | + | + | |||
| Puls et al., 2014 | + | + | |||
| Satirogluo et al., 2014 | + | + | |||
| Sharma et al., 2012 | + | + | |||
| Temtanakitpaisan et al., 2013 | + | + | |||
| Yamuchi et al., 2006 | + | + | |||
+=Symbol denotes successful treatment
Thrombolytic therapy is a readily available treatment option associated with the excellent immediate outcome as well.[5,13,14,15,16,17,18,19,20,21,22] Nkoke et al.[2] described the case of RHT and bilateral massive PE, which was treated successfully with tenecteplase. Moreover, Puls et al.[17] reported three cases of highly mobile right heart mass and PE; two cases were treated successfully with thrombolytic therapy, whereas the third case was treated with surgical removal of the mass that revealed myxoma of the right ventricle. Thrombolytic therapy is highly recommended for high risk and intermediate-high risk patients.
Anticoagulation should be used in all cases of RHT and PE as an adjunctive treatment after thrombolysis or surgical embolectomy. However, the increased mortality rate was reported in patients treated with anticoagulation alone. Athappan et al.[23] reported a higher mortality rate in patients treated with anticoagulation alone compared to those treated with thrombolytic therapy or surgical embolectomy. Nevertheless, anticoagulation alone was successfully used in elderly patients who are considered at high risk for bleeding with thrombolytic therapy.[24,25,26] Temtanakitpaisan et al.[24] described the case of a 92-year-old man who had RHT with PE and was successfully treated with heparin alone. A case of RHT and PE on right atrial pacemaker leads were successfully treated with heparin alone in an another 80-year-old man resulting in a complete disappearance of the RHT after 6 days of treatment.[26]
Percutaneous interventional techniques can also be a good therapeutic option [Table 1].[27] Treatment should be individualized according to the patient's bleeding risk, hemodynamic parameters, and laboratory data.[5] Based on what has been mentioned in the literature review, there is still no consensus regarding the best treatment. The study is clinical evidence of the efficacy of thrombolysis in the case of RHT complicated by PE.
CONCLUSION
This case is the first report from Lebanon describing RHT and acute massive PE with DVT that was successfully treated with thrombolysis. Such extreme medical emergency highlights the importance of urgent TTE in the diagnosis of RHT and RVD. The study findings confirm the effect of thrombolysis on the disappearance of the RHT, the PE and the thrombus of the common femoral vein. Thrombolysis improved the RVD and pulmonary hypertension with no bleeding complications. Randomized clinical trials that compare the various modes of treatment are needed.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Video available on: www.jcecho.org
REFERENCES
- 1.Rose PS, Punjabi NM, Pearse DB. Treatment of right heart thromboemboli. Chest. 2002;121:806–14. doi: 10.1378/chest.121.3.806. [DOI] [PubMed] [Google Scholar]
- 2.Nkoke C, Faucher O, Camus L, Flork L. Free floating right heart thrombus associated with acute pulmonary embolism: An unsettled therapeutic difficulty. Case Rep Cardiol. 2015;2015:364780. doi: 10.1155/2015/364780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferrari E, Benhamou M, Berthier F, Baudouy M. Mobile thrombi of the right heart in pulmonary embolism: Delayed disappearance after thrombolytic treatment. Chest. 2005;127:1051–3. doi: 10.1378/chest.127.3.1051. [DOI] [PubMed] [Google Scholar]
- 4.Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N, et al. 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35:3033. [Google Scholar]
- 5.Chartier L, Béra J, Delomez M, Asseman P, Beregi JP, Bauchart JJ, et al. Free-floating thrombi in the right heart: Diagnosis, management, and prognostic indexes in 38 consecutive patients. Circulation. 1999;99:2779–83. doi: 10.1161/01.cir.99.21.2779. [DOI] [PubMed] [Google Scholar]
- 6.Lohrmann GM, Peters F, van Riet S, Essop MR. Double trouble – A case report of mobile right atrial thrombus in the setting of acute pulmonary thromboembolism. Heart Lung Circ. 2014;23:e214–6. doi: 10.1016/j.hlc.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 7.Cuccia C, Campana M, Centurini PB, Bolognesi R, Costa F, Zogno M, et al. A rare case of massive pulmonary embolism and in transit cardiac thrombosis. G Ital Cardiol. 1998;28:1028–31. [PubMed] [Google Scholar]
- 8.Fischer JI, Huis in ‘t Veld MA, Orland M, Harvey P, Panebianco NL, Dean AJ, et al. Diagnosis of near-fatal pulmonary embolus-in-transit with focused echocardiography. J Emerg Med. 2013;45:232–5. doi: 10.1016/j.jemermed.2013.03.015. [DOI] [PubMed] [Google Scholar]
- 9.Hisatomi K, Yamada T, Onohara D. Surgical embolectomy of a floating right heart thrombus and acute massive pulmonary embolism: Report of a case. Ann Thorac Cardiovasc Surg. 2013;19:316–9. doi: 10.5761/atcs.cr.12.01987. [DOI] [PubMed] [Google Scholar]
- 10.Ando T, Abe H, Nagata T, Sakurai Y, Chikada M, Kobayashi T, et al. Reports of four surgical treatments of acute pulmonary embolism with a floating thrombus in the right atrium. Gen Thorac Cardiovasc Surg. 2011;59:705–8. doi: 10.1007/s11748-010-0732-6. [DOI] [PubMed] [Google Scholar]
- 11.Eweda II, Samir S, Abbas O, El-Gohary GM, Nammas W. Right heart thrombus-in-transit with pulmonary embolism in a patient with primary hypercoagulable state. Cardiol J. 2010;17:408–11. [PubMed] [Google Scholar]
- 12.Yamauchi S, Maruyama Y, Sakamoto S, Imura H, Ogasawara H, Yamada K, et al. Surgical treatment of free-floating thrombi in the right side of the heart in patients with pulmonary thromboembolism. J Nippon Med Sch. 2006;73:33–7. doi: 10.1272/jnms.73.33. [DOI] [PubMed] [Google Scholar]
- 13.Dzudovic B, Obradovic S, Rusovic S, Gligic B, Rafajlovski S, Romanovic R, et al. Therapeutic approach in patients with a floating thrombus in the right heart. J Emerg Med. 2013;44:e199–205. doi: 10.1016/j.jemermed.2012.02.087. [DOI] [PubMed] [Google Scholar]
- 14.Satiroǧlu O, Durakoǧlugil ME, Uǧurlu Y, Sahin I, Doǧan S, Ergül E, et al. Successful thrombolysis using recombinant tissue plasminogen activator in cases of severe pulmonary embolism with mobile thrombi in the right atrium. Interv Med Appl Sci. 2014;6:89–92. doi: 10.1556/IMAS.6.2014.2.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akıllı H, Gül EE, Arıbaş A, Özdemir K, Kayrak M, Erdoǧan HI, et al. Management of right heart thrombi associated with acute pulmonary embolism: A retrospective, single-center experience. Anadolu Kardiyol Derg. 2013;13:528–33. doi: 10.5152/akd.2013.173. [DOI] [PubMed] [Google Scholar]
- 16.Naeem K. Floating thrombus in the right heart associated with pulmonary embolism: The role of echocardiography. Pak J Med Sci. 2015;31:233–5. doi: 10.12669/pjms.311.6219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Puls M, Hünlich M, Schillinger W. Free-floating right heart thrombi in pulmonary embolism: Therapeutic options and differential diagnosis. Dtsch Med Wochenschr. 2014;139:887–91. doi: 10.1055/s-0034-1369945. [DOI] [PubMed] [Google Scholar]
- 18.Pellegrini L, Le Dolley Y, Marot B, Riberi A, Bellezza M, Kerbaul F, et al. Interest of echocardiography in the diagnosis and monitoring of a pulmonary embolism complicating a free-floating thrombus in right heart cavities. Ann Fr Anesth Reanim. 2012;31:246–50. doi: 10.1016/j.annfar.2011.10.032. [DOI] [PubMed] [Google Scholar]
- 19.Debney MT. Acute pulmonary embolus with visible right heart thrombus in transit. BMJ Case Rep 2011. 2011 doi: 10.1136/bcr.07.2011.4553. pii: bcr0720114553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karabay CY, Kocabay G, Kalayci A, Zehir R, Mert M, Kirma C, et al. Snake-like thrombus in the right atrium causing pulmonary embolism. Cardiovasc J Afr. 2011;22:206–7. doi: 10.5830/CVJA-2010-060. [DOI] [PubMed] [Google Scholar]
- 21.Burns KE, McLaren A. Catheter-related right atrial thrombus and pulmonary embolism: A case report and systematic review of the literature. Can Respir J. 2009;16:163–5. doi: 10.1155/2009/751507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huang SL, Chien CH, Chang YC. A floating thrombus of the right ventricle in severe massive pulmonary embolism. Am J Emerg Med. 2008;26:1071e1–2. doi: 10.1016/j.ajem.2008.03.045. [DOI] [PubMed] [Google Scholar]
- 23.Athappan G, Sengodan P, Chacko P, Gandhi S. Comparative efficacy of different modalities for treatment of right heart thrombi in transit: A pooled analysis. Vasc Med. 2015;20:131–8. doi: 10.1177/1358863X15569009. [DOI] [PubMed] [Google Scholar]
- 24.Temtanakitpaisan Y, Mahatanan R, Rishikof DC, Young DZ. Use of heparin alone in treating pulmonary emboli found in association with in-transit right-heart thrombi in a nonagenarian. Tex Heart Inst J. 2013;40:487–8. [PMC free article] [PubMed] [Google Scholar]
- 25.Lampropoulos KM, Bonou M, Theocharis C, Barbetseas J. Treatment of mobile right heart thrombi with low-molecular-weight heparin. BMJ Case Rep 2013. 2013 doi: 10.1136/bcr-2012-008272. pii: bcr2012008272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.D'Aloia A, Bonadei I, Vizzardi E, Curnis A. Right giant atrial thrombosis and pulmonary embolism complicating pacemaker leads. BMJ Case Rep 2013. 2013 doi: 10.1136/bcr-2012-008017. pii: bcr2012008017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Momose T, Morita T, Misawa T. Percutaneous treatment of a free-floating thrombus in the right atrium of a patient with pulmonary embolism and acute myocarditis. Cardiovasc Interv Ther. 2013;28:188–92. doi: 10.1007/s12928-012-0141-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


