Abstract
Purpose
To evaluate effectiveness of Welch Allyn Spot Vision Screener in detecting refractive error in all age groups and amblyopia risk factors in children in a tribal district of India.
Methods
All participants received dry retinoscopy and photorefraction; children also received cycloplegic retinoscopy. Statistical analysis included Bland-Altman and coefficient of determination (R2).
Results
Photoscreener could not elicit a response in 113 adults and 5 children of 580 recruited participants. In Bland-Altman analysis mean difference of Spot screener spherical equivalent (SSSE) and dry retinoscopy spherical equivalent (DRSE) was 0.32 diopters (D) in adults and 0.18 D in children; this was an overestimation of hyperopia and underestimation of myopia. In Bland-Altman analysis of SSSE and cycloplegic retinoscopy spherical equivalent (CRSE) the mean difference was −0.30 D in children; this was an overestimation of myopia and underestimation of hyperopia. In regression analysis the relationship between SSSE and DRSE was poor in adults (R2 = 0.50) and good in children (R2 = 0.92). Cubic regression model for Spot versus cycloretinoscopy in children was: CRSE = 0.34 + 0.85 SSSE − 0.01 SSSE2 + 0.006 SSSE3. It was 87% accurate. Sensitivity and specificity of Spot in detecting amblyopia risk factors (2013 American Association for Pediatric Ophthalmology and Strabismus [AAPOS] criteria) was 93.3% and 96.9% respectively. Sensitivity of Spot screener in detection of amblyopia was 72%.
Conclusions
Photoscreener has 87% accuracy in refraction in children. Its value could be used for subjective correction tests.
Translational Relevance
Photoscreening could complement traditional retinoscopy to address refractive error in children in a resource-limited facility region.
Keywords: refraction, photoscreener, children's vision
Introduction
Uncorrected refractive error is the most common cause of visual impairment and second common cause of blindness in the world.1,2 Refractive error impacts the quality of life in all age groups.3 The problem is more serious in children as it is likely to also impact their mental wellbeing and intellectual development.4 Amblyopia is a reversible deficit of vision that should be treated within the sensitive period for visual development.5 Risk factors for amblyopia include strabismus, ametropia, anisometropia, and optical deprivation.6 The benefits of screening for refractive error are always beyond refractive error (including presbyopia) correction itself. In adults, it helps in detecting many blinding disorders, such as cataract, glaucoma, and diabetic retinopathy; in children, it helps in detection of amblyopia, strabismus, and childhood cataract.7,8
Traditionally, objective retinoscopy and subjective corrections are the essential steps of screening for refractive error. Classically, it is performed using a streak retinoscope and neutralizing lenses, which needs training and has a significant learning curve.9 An autorefractor could be a convenient alternative to retinoscopy. Photorefraction is a technique of autorefraction that uses a camera to take images of undilated eyes. The estimate of the eye's defocus is derived from the distribution of reflected light across the subject's pupil.10 The Welch Allyn Spot Vision Screener (Skaneateles Falls, NY) is a photoscreener.11 It is a noninvasive, handheld, portable device that automatically captures vision data for both eyes concomitantly in all ages. The device creates a diagram with the location of the eyes, demonstrating strabismus when present as well as an autorefractive reading. The measuring range extends up to ±7.50 diopters (D) for spherical errors and ±3.50 D for cylindrical errors. Additionally, it also measures pupil size, interpupillary distance, and gaze deviation. This device also flags a referral for complete eye examination if significant refractive error, anisometropia, anisocoria, or strabismus exists.12,13 The additional advantages include its portability, power supply from batteries, little time (∼10 seconds) to complete refraction, simultaneous capture of both eyes, and minimal training to operate.14,15
We evaluated the effectiveness of Spot in detecting refractive error in all age groups in Raygada, a tribal district of Odisha, India. We chose this district because we had planned for a district-wise school children screening. Additionally, we used the American Association of Pediatric Ophthalmology and Strabismus (AAPOS) 2013 guidelines to measure its ability to detecting amblyopia risk factors in children 4- to 7-years old.
Methods
The ethics committee of L V Prasad Eye Institute, Bhubaneswar, India (2016-15-CB-14) approved this study. The research protocol adhered to the provision of the Declaration of Helsinki for research involving human beings. Written informed consent was obtained from all adult participants and accompanying relations of children.
All patients attending the outpatient department of Naraindas Morbai Budhrani eye centre and JK Centre for Tribal Eye Health, Rayagada, Odisha (India) in April 2017 were recruited for the study. We excluded the patients who had received any intraocular surgery within 1 month and those unwilling to sign the informed consent. A comprehensive examination included a detailed history, measurement of presenting (with spectacles, when available) and corrected distance and near vision, photoscreening, dry retinoscopy, lid and adnexal examination, Hirschberg test, cover–uncover and prism cover test, slit-lamp examination, and dilated fundus examination. Dilatation in the adults was performed with tropicamide 0.8% and phenylephrine hydrochloride 5%; in children (<16 years) dilatation was performed with cyclopentolate 1%. Additionally, a cycloplegic photoscreening, traditional cycloplegic retinoscopy, and subjective correction after cycloplegic examination were performed in children.
In every stage, the photorefraction was performed by an optical dispensing person, not trained in refraction, but trained to using the Spot instrument. The procedure of examination was as per the manual.16 While an optometrist performed the retinoscopy, a comprehensive ophthalmologist performed the rest of the ocular examinations. The data obtained from photorefraction was masked to the optometrist during both objective refraction (using a streak retinoscope) and subjective correction. Refraction obtained by the Spot screener and retinoscopy was converted into median spherical equivalent (M), J45, and J180 vectors for statistical analysis.
The formula for calculating these 3 parameters were as follows:
 |
 |
 |
where 2α represents the cylindrical axis.
Statistical Analysis
The data were entered into an Excel sheet (Microsoft, Redmond, WA) and were analyzed using R statistics version 3.2.5 (2016-04-14; Vienna, Austria). The mean refractive error was calculated with the Spot screener and dry retinoscopy for adults. The mean refractive error was calculated with the Spot screener, dry retinoscopy, cycloplegic retinoscopy, and Spot cycloplegic retinoscopy in children. A paired t-test was applied to test if the difference between the results obtained from Spot photoscreener and retinoscopy was significant. Dry retinoscopy in adults and cycloplegic retinoscopy in children were considered the gold standards. Linear, quadratic, and cubic models were constructed to assess the correlation between the results obtained from these methods. The coefficient of determination (R2) was used to determine the close relationship of variables in the curve estimation regression. Bland-Altman plots were used to assess the agreement between Spot and retinoscopy. The spherical equivalent (SE) with Spot was compared with dry retinoscopy in adults and with both dry and cycloplegic retinoscopy in children. SE of cycloplegic refraction using the Spot was also compared with the cycloplegic retinoscopy using the streak retinoscope in children. Calculation was performed for myopes and hyperopes separately. Percentage of participants with a difference within ±1 D between the Spot screener and retinoscopy were assessed.
Amblyopia risk factors based on the AAPOS 2013 guidelines for ages over 4 years were as follows: hyperopia greater than 3.5 D in any meridian, myopia greater than 1.5 D in any meridian, astigmatism greater than 1.5 D in any meridian, anisometropia greater than 1.5 D, and manifest strabismus greater than 8 prism diopters (PD) in primary position.17 The results of both Spot and retinoscopy were analyzed based on these criteria.
Myopia was defined as refractive error more than 0.5 D and hypermetropia as more than 1.0 D. Emmetropia was defined as refractive error between −0.5 D and 1.0 D. A child was considered emmetrope only when both eyes did not have refractive error; otherwise the child was grouped under one of the refractive errors, myopia or hypermetropia, as per the refraction.
Results
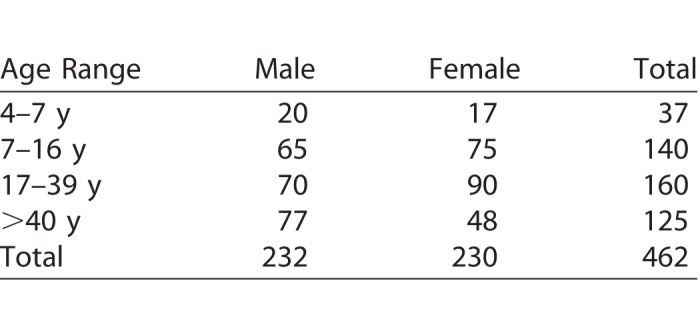
In the study period of 1 month, 580 people were recruited. Photoscreener failed to elicit usable response in 118 participants (5 children and 113 adults). The causes of failure in these people were cataract (n = 72), small pupil (n = 34), pseudophakia (n = 4), high hypermetropia (n = 3), pterygium involving the visual axis, microcornea (n = 2 each), and adherent leukoma and corneal scar (n = 1 each). Thus, the following photoscreener results were obtained from 462 participants (924 eyes): 177 children (mean age: 10.56 ± 2.89, range: 4–16 years) and 285 adults (mean age: 37.48 ± 13.95, range: 17–75 years). There were 230 males including 85 children, and 232 females including 92 children. The age and sex distribution is shown in Table 1. The range of refractive errors (SE) measured with dry retinoscopy in adults and cycloplegic retinoscopy in children was from −9.5 D to +8.75 D. Seventy-eight children also received Spot screener examination after cycloplegic dilatation.
Table 1.
Age and Sex Distribution of Study Cohort
The distribution of refractive error in 177 children was as follows: hypermetropia, 34; myopia, 28; and emmetropia, 115. Amblyopia risk factors as defined by 2013 AAPOS criteria16 were detected in 24 eyes of 17 children between 4 and 7 years of age. Few children had more than one amblyopic risk factor, and 18 children had amblyopia. The Spot could help detect amblyopia in 11 children (sensitivity 61%), including four ametropic amblyopia (4/4), four anisometric amblyopia (4/9), one meridionial amblyopia (1/1), two strabismic amblyopia greater than 8PD (2/2). The Spot could not detect two stimulus deprivation amblyopia (status post cataract surgery) because there is no criteria in Spot to detecting such amblyopia. Thirteen children had intermittent strabismus. The Spot detected constant strabismus in seven children (2 exotopia 4.5°–6.0°; 2 exotopia 7.0°–15.0°; 1 esotropia 7.0°–15.0°, 1 each hyper- and hypotropia 4.5°–6.0°). The ophthalmologists confirmed three patients with strabismus in three patients, all with 7.0°–15.0°.
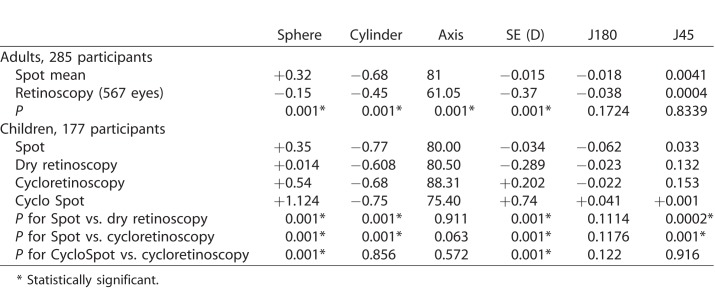
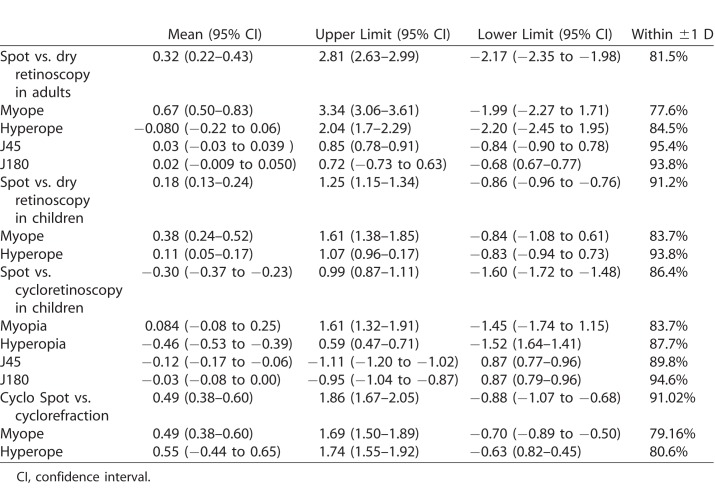
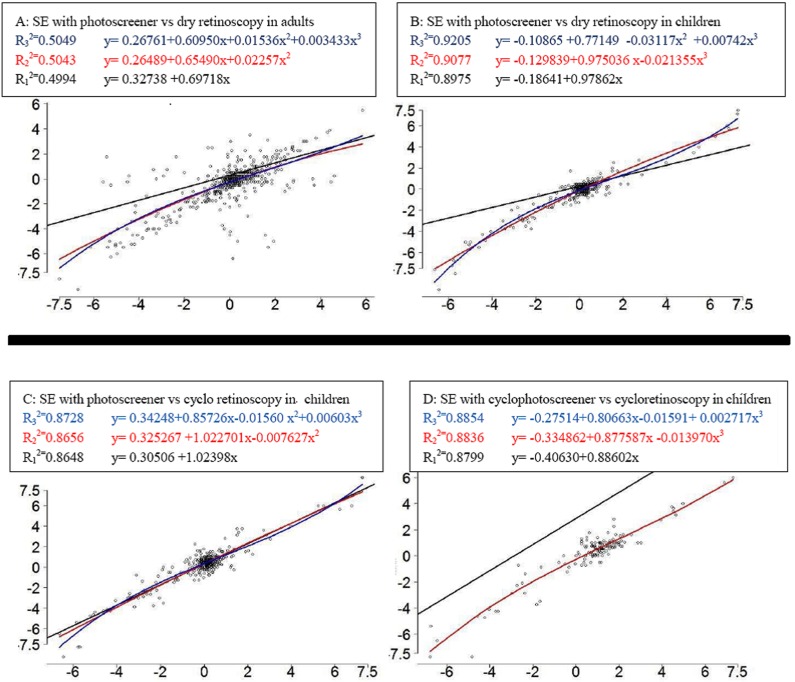
The mean refractive errors measured with Spot photoscreener and dry retinoscopy for adults and Spot screener, dry retinoscopy, cycloplegic retinoscopy, and cycloplegic Spot screener retinoscopy in children is shown in Table 2. There were statistically significant differences of sphere, cylinder, and SE results obtained from the two methods (P < 0.01, paired t-test) but the J180 and J45 did not have any difference in adults. In children, there was statistically significant difference between Spot and cycloretinoscopy for sphere, cylinder, SE, and J45, but no difference in J180. But there is no clinical significance for difference up to 0.50 D. From this perspective there was no clinical significance. The mean difference of refractive errors between different methods is shown in Table 3. The difference in the Spot screener SE and cycloplegic retinoscopy spherical equivalent is plotted against the average in Bland-Altman plot (Fig. 1).
Table 2.
Mean Refractive Error Measured by Different Methods
Table 3.
Mean Difference, Lower Limit, and Upper Limit of Spherical Equivalent Between Different Methods
Figure 1.
Bland-Altman plots showing agreement between different methods.
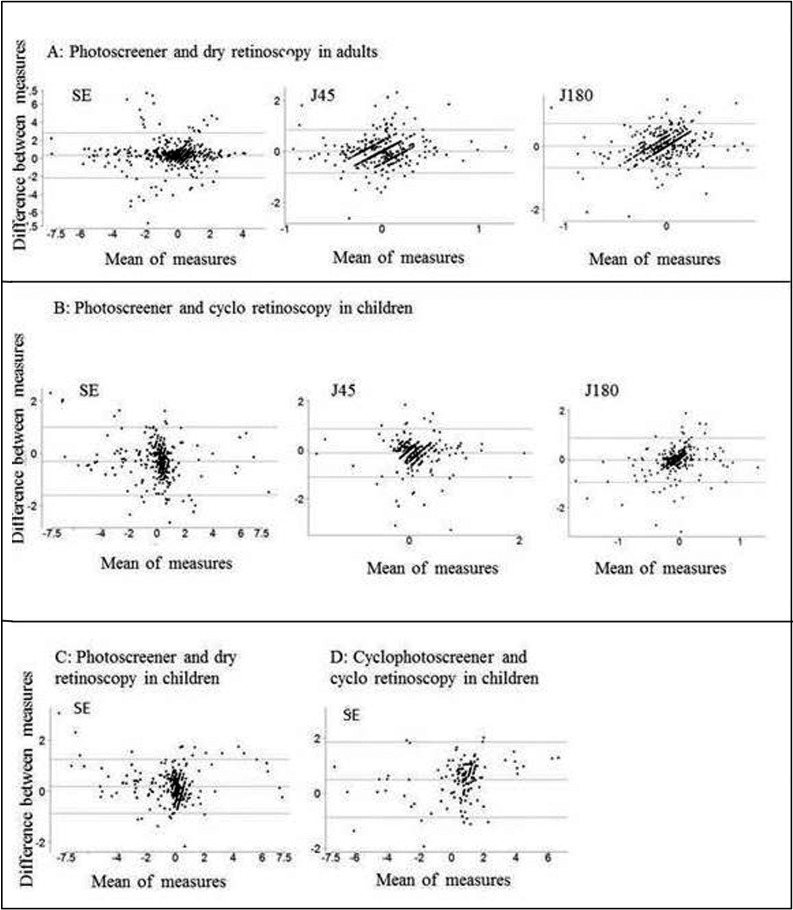
Regression was used to evaluate the quantitative relationship between the results of the Spot and cycloplegic retinoscopy (Table 4, Fig. 2). Because cycloplegic retinoscopy is considered the gold standard in children, and because using Spot screener after instilling cycloplegics is cumbersome, we derived the relationship between the cycloplegic retinoscopy and the Spot screener retinoscopy (before cycloplegia) with the cubic model; the cubic model had the best fitting (R2 = 0.8728).
Table 4.
Coefficient of Determination (R2) Values to Determine the Relationships Between Various Measurements
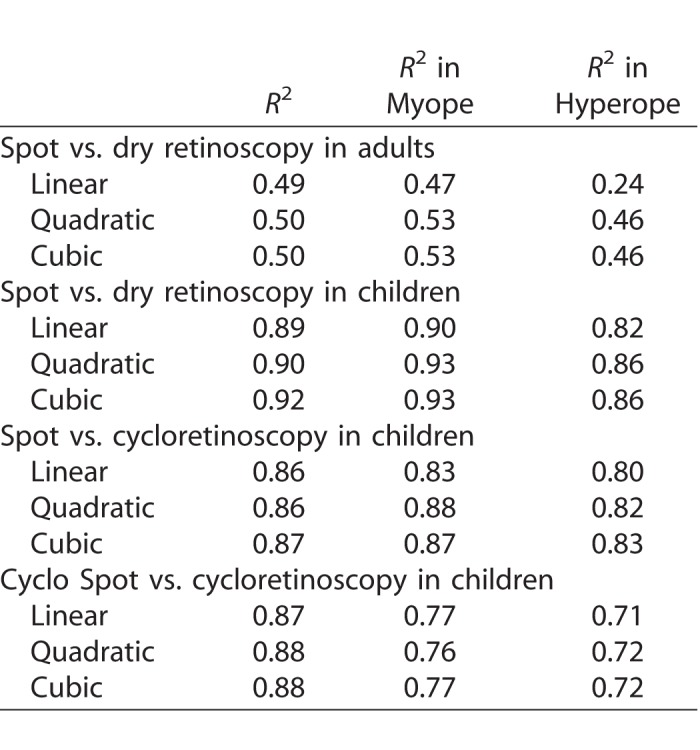
Figure 2.
Curve estimation regression for quantitative relationship between results.
The cubic regression model is Y = 0.342 + 0.85X − 0.015X2 + 0.006X3.
Clinically, the ‘X' and ‘Y' represented Spot screener spherical equivalent (SSSE) and cycloplegic retinoscopy spherical equivalent (CRSE), respectively, that is,
 |
Thus, one could predict the cylcoplegic retinoscopy when the Spot value is known with 87% accuracy using the cubic regression model or with 86% accuracy with the linear model.
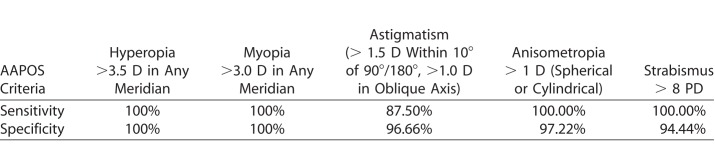
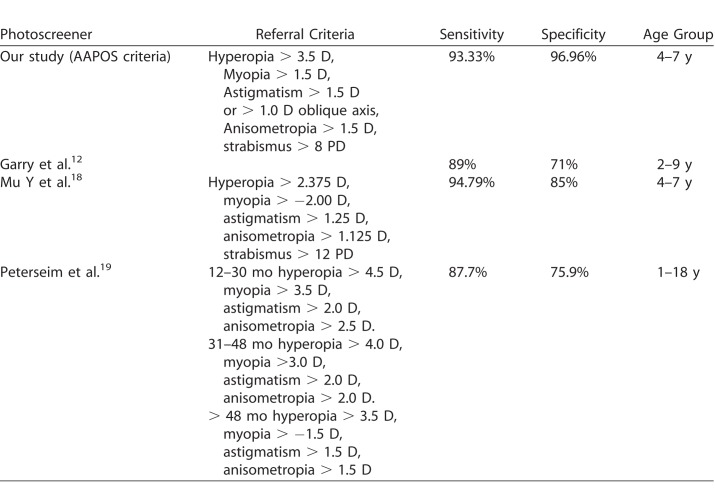
The sensitivity and specificity of the Spot in detecting amblyopia risk factors according to the AAPOS 201317 criteria in the age group of 4 to 7 years are shown in Table 5 and the comparison with other studies using a photo screener is shown in Table 6.
Table 5.
Sensitivity and Specificity of Spot Screener in Detection of Amblyopia Risk Factors in the Current Study as Per AAPOS Criteria
Table 6.
Comparison of Various Studies Using Spot Screener
Discussion
Refractive error is a common disorder in all age groups and it is easy to ameliorate with appropriate refraction and dispensing a pair of spectacles. A faster and accurate refraction is the first step, and this could be done rapidly with autorefraction or photorefraction. We tested one such device (Welch Allyn Spot Vision Screener) and compared it with traditional retinoscopy in adults and with cycloplegic retinoscopy in children.
The mean difference of Spot versus dry retinoscopy was 0.32 D in adults and 0.18 D in children with the Bland-Altman analysis. This indicated an overestimation of hyperopia and underestimation of myopia in Spot retinoscopy. The difference between the adults and children was clinically not significant. The mean difference of Spot retinoscopy from the cycloplegic retinoscopy was −0.3 D, indicating underestimated hyperopia and overestimated myopia. Again the difference was not clinically significant. This difference is possibly explained by the amount of accommodation a child exerts during refraction without cycloplegia. This is validated by the fact that the difference was 0.49 D in postcycloplegic Spot and traditional retinoscopy. The mean difference of Spot versus dry retinoscopy in adults and the Spot versus cycloretinoscopy in children for J180 and J45 was less; this indicates a better performance of Spot screener in detection of cylinder and confirms with another other study.18
We also detected that the cycloplegic retinoscopy, considered the gold standard in children, was closer to the Spot photoscreener refraction in undilated eyes. Our findings confirm the reports from other studies either using the Spot17 or other photoscreeners.20–25 We documented a differential response in adults (performed better in eyes with hyperopia) and in children (performed better eyes with myopia) using the Spot photoscreening device. The photoscreener retinoscopy was within +1 D of dry retinoscopy in 81.5% adults and within +1 D of cycloplegic retinoscopy in 86.4% children. The relationship between Spot screener and dry retinoscopy was comparatively poor in adults even in the cubic model fitting (adults: R2 = 0.50; children: R2 = 0.92; Table 3). Additionally, the dry retinoscopy had better fitting (R2 = 0.92) than cycloretinoscopy (R2 = 0.87) in children with the Spot screener, which is similar to18 or better than other studies.26 In general, Spot screener performed better in eyes with myopia than in eyes with hyperopia in logistic regression.
The sensitivity and specificity of Spot in detection of amblyopia risk factors were high and were higher in comparison to other studies using the same photoscreener (Table 6).12,18,19 The different referral criteria and different age group taken in different studies could explain a part of it. The weakness of the study lies in the fact that we used only one type of photoscreener device and the sample size was small. Hence, our recommendation should be confined to the device we tested (in this case, Welch Allyn Spot Vision Screener). The small sample size did not permit detection of amblyopia risk factors. The strength of the study lies in the fact that the study recruited people in all age groups. The photoscreener refraction done both before and after cycloplegic dilatation in children helped further establish its accuracy and usefulness.
Conclusion
The Welch Allyn Spot screener overestimated hyperopia and underestimates myopia in adults and it underestimated hyperopia and overestimated myopia in children. It performed better in eyes with hyperopia in dry retinoscopy and in children with cycloplegic retinoscopy, and in general, it performed better in eyes with myopia. Overall accuracy was higher in children than adults. Regression could predict refraction with 87% accuracy in children but not in adults. Spot screener's better performance in children is most likely related to the following three factors: (1) it is calibrated to take into account some accommodation, (2) children's pupils are larger than adults and the current technology requires a moderately dilated pupil, and (3) better media clarity in children. Vision testing is a better parameter in adults and so the Spot screener is not required.
We recognize that retinoscopy is a time-tested method. Cycloplegic refraction is the standard of care for refractive error correcting in children. The photorefraction system is useful in remote locations for providing eye care services in children who have no access or are unable to visit nearest eye care facility. We believe this will reduce refractive error and amblyopia burden to a great extent in children. It is not as useful in adults. We also recognize that photorefraction has a limited range and as such a spectacles prescription should not be made without adequate subjective verification.
Acknowledgments
Supported by grants from the Hyderabad Eye Research Foundation, Hyderabad.
Disclosure: L. Panda, None; U. Barik, None; S. Nayak, None; B. Barik, None; G. Behera, None; R. Kekunnaya, None; T. Das, None
References
- 1. Bourne RRA, Flaxman SR, Braithwaite T,et al. . for the Vision Loss Expert Group. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. Lancet Glob Health. 2017; 5: e888– e897. [DOI] [PubMed] [Google Scholar]
- 2. American Academy of Ophthalmology Pediatric Ophthalmology/Strabismus Panel: Wallace DK, Repka MX, Lee KA,et al. . Amblyopia PPP - 2017. Available from: https://www.aao.org/preferred-practice-pattern/amblyopia-ppp-2017. Accessed August 9, 2017.
- 3. Lamoureux EL, Saw SM, Thumboo J,et al. . The impact of corrected and uncorrected refractive error on visual functioning: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci. 2009; 50: 2614– 2620. [DOI] [PubMed] [Google Scholar]
- 4. Aghai G, Dibajnia P, Ashkesh E,et al. . Behavior disorders in children with significant refractive errors. J Curr Ophthalmol. 2016; 28: 223– 225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Powell C, Hatt SR. . Vision screening for amblyopia in childhood. Cochrane Database Syst Rev. 2009; (3) :CD005020. [DOI] [PubMed] [Google Scholar]
- 6. Lagrèze WA. . Vision screening in preschool children: do the data support universal screening? Dtsch Arztebl Int. 2010; 107: 495– 459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. US Preventive Services Task Force, Grossman DC, Curry SJ,et al. . Vision screening in children aged 6 months to 5 years: US Preventive Services Task Force Recommendation Statement. JAMA. 2017; 318: 836– 844. [DOI] [PubMed] [Google Scholar]
- 8. American Academy of Pediatrics; Section on Ophthalmology; American Association for Pediatric Ophthalmology And Strabismus; American Academy of Ophthalmology; American Association of Certified Orthoptists. Red reflex examination in neonates, infants, and children. Pediatrics. 2008; 122: 1401– 1404. [DOI] [PubMed] [Google Scholar]
- 9. Lee OL. . Retinoscopy 101. 2015. Available from: https://www.aao.org/young-ophthalmologists/yo-info/article/retinoscopy-101. Accessed August 9, 2017.
- 10. Howland HC. . Photorefraction of eyes: history and future prospects. Optom Vis Sci. 2009; 86: 603– 606. [DOI] [PubMed] [Google Scholar]
- 11. SpotTM Vision Screening by Welch Allyn. Available from: http://www.spotvision screening.com. Accessed August 25, 2014.
- 12. Garry GA, Donahue SP. . Validation of Spot screening device for amblyopia risk factors. J AAPOS. 2014; 18: 476– 480. [DOI] [PubMed] [Google Scholar]
- 13. Silbert DI, Matta NS. . Performance of the Spot vision screener for the detection of amblyopia risk factors in children. J AAPOS. 2014; 18: 169– 172. [DOI] [PubMed] [Google Scholar]
- 14. Alley CL. . Preschool vision screening: update on guidelines and techniques. Curr Opin Ophthalmol. 2013; 24: 415– 420. [DOI] [PubMed] [Google Scholar]
- 15. Ottar WL, Scott WE, Holgado SI. . Photoscreening for amblyogenic factors. J Pediatr Ophthalmol Strabismus. 1995; 32: 289– 295. [DOI] [PubMed] [Google Scholar]
- 16. Spot. Welch Allyn. Vision Screeener Model VS100. Available from: https://www.welchallyn.com/content/dam/welchallyn/documents/sap-documents/LIT/80021/80021889LITPDF.pdf. Acccessed October 17, 2017.
- 17. Donahue SP, Arthur B, Neely DE,et al. . Guidelines for automated preschool vision screening: a 10-year, evidence-based update. J AAPOS. 2013; 17: 4– 8. [DOI] [PubMed] [Google Scholar]
- 18. Mu Y, Bi H, Ekure E,et al. . Performance of Spot photoscreener in detecting amblyopia risk factors in Chinese pre-school and school age children attending an eye clinic. PLoS One. 2016; 11: e0149561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Peterseim MM, Papa CE, Wilson ME,et al. . The effectiveness of the Spot Vision Screener in detecting amblyopia risk factors. J AAPOS. 2014; 18: 539– 542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dahlmann-Noor AH, Vivian AJ. . A comparison of photorefraction and retinoscopy in children. J AAPOS. 2008; 12:104; author reply104–105. [DOI] [PubMed]
- 21. Moghaddam AA, Kargozar A, Zarei-Ghanavati M,et al. . Screening for amblyopia risk factors in pre-verbal children using the Plusoptix photoscreener: a cross-sectional population-based study. Br J Ophthalmol. 2012; 96: 83– 6. [DOI] [PubMed] [Google Scholar]
- 22. Rajavi Z, Parsafar H, Ramezani A,et al. . Is noncycloplegic photorefraction applicable for screening refractive amblyopia risk factors? J Ophthalmic Vis Res. 2012; 7: 3– 9. [PMC free article] [PubMed] [Google Scholar]
- 23. Ayse YK, Onder U, Suheyla K. . Accuracy of Plusoptix S04 in children and teens. Can J Ophthalmol. 2011; 46: 153– 157. [DOI] [PubMed] [Google Scholar]
- 24. Paff T, Oudesluys-Murphy AM, Wolterbeek R,et al. . Screening for refractive errors in children: the plusoptiX S08 and the Retinomax K-plus2 performed by a lay screener compared to cycloplegic retinoscopy. J AAPOS. 2010; 14: 478– 483. [DOI] [PubMed] [Google Scholar]
- 25. Mirzajani A, Heirani M, Jafarzadehpur E,et al. . A comparison of the Plusoptix S08 photorefractor to retinoscopy and cycloretinoscopy. Clin Exp Optom. 2013; 96: 394– 399 [DOI] [PubMed] [Google Scholar]
- 26. Yan XR, Jiao WZ, Li ZW,et al. . Performance of the Plusoptix A09 photoscreener in detecting amblyopia risk factors in Chinese children attending an eye clinic. PLoS One. 2015; 10: e0126052. [DOI] [PMC free article] [PubMed] [Google Scholar]