Abstract
The lateral meniscus is vital in dissipating the force in the lateral compartment of the knee. A complete radial tear of the meniscus can lead to extrusion, rendering it nonfunctional and resulting in deleterious arthritic changes to the lateral compartment. Arthroscopic repair of a complete radial tear of the lateral meniscus poses a challenge to orthopaedic surgeons. Although some would advocate for meniscectomy, we present a technique for an outside-in repair using 3 sutures and standard arthroscopic portals. Overall, this provides for an excellent reduction of the meniscus.
The meniscus is vital in load bearing and force distribution in the knee. This is of particular importance in the lateral compartment due to the convexity of the lateral tibial plateau. The meniscus is a fibrocartilaginous structure composed of type I cartilage arranged in mostly circumferential fibers that are suited to resist hoop stresses.1 A complete radial tear transects these fibers, rendering the meniscus nonfunctional.2 This results in a decreased contact area of 45% to 50% and an increased contact pressure of approximately 50%.3 These biomechanical changes have a detrimental effect on the knee, predisposing to degenerative wear and arthritis.2, 4 Repair of radial tears can improve the contact area and restore the contact pressure back to the intact state of the meniscus.3 Multiple techniques for the repair of lateral meniscus radial tears have been described.2, 4, 5, 6, 7, 8, 9, 10 We present a technique for outside-in repair using a crossing horizontal mattress suture to reapproximate the lateral meniscus.
Surgical Technique
Patient Positioning and Preparation
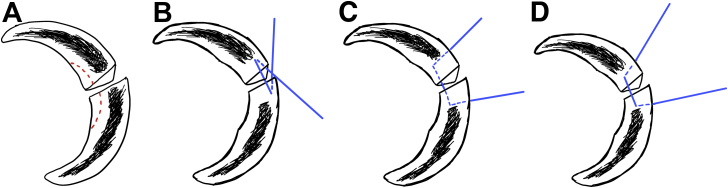
Lateral meniscus repair (Video 1) is performed under general anesthesia. Preoperative regional anesthesia is not performed because of the relative proximity of the procedure to the peroneal nerve and the need for a postoperative physical examination to document intact neurologic function. The patient is positioned supine with a well-padded pneumatic tourniquet placed to the upper thigh. The operative leg is prepped and draped in the usual sterile fashion. The leg is exsanguinated and the tourniquet inflated. A standard anterolateral portal is created first followed by an anteromedial portal under direct arthroscopic visualization. A diagnostic arthroscopy is conducted to ensure that there is no additional intra-articular pathology. Once this is completed, the leg is placed in the figure-of-4 position and the lateral meniscus addressed. The entire meniscus is thoroughly evaluated for any additional injury. In this case, there is an additional 2-mm radial tear of the posterior horn that is treated with a partial meniscectomy (Fig 1). The complete radial tear of the body is first addressed by debriding the central portion of the meniscus at the tear in a semilunar pattern (Fig 2A). A PassPort Cannula (Arthrex, Naples, FL) is introduced into the anterolateral portal and the meniscus repair is addressed.
Fig 1.
Viewing from the anterolateral portal with the leg in the figure-of-4 position, a 2-mm partial radial tear of the posterior horn of the left lateral meniscus is identified (arrow). This is addressed with a partial meniscectomy.
Fig 2.
Technique for outside-in repair of a complete radial tear of the left lateral meniscus in chronological order. (A) Debridement of the central portion of the meniscus surrounding the complete radial tear is performed in a semilunar pattern before the placement of the first suture. (B) The first suture is a crossing horizontal mattress. This suture is essential for providing reduction vectors on the tear without lateral displacement of the meniscus. (C) The second suture is a noncrossing, horizontal mattress that enters the peripheral body of the meniscus and exits on the undersurface. (D) The third and final suture is also a noncrossing, horizontal mattress exiting on the top surface of the meniscus, more centrally located than the first suture.
Outside-in Meniscus Repair
With the knee still in the figure-of-4 position and the arthroscope in the anteromedial portal, the lateral joint line is palpated and transilluminated. The Meniscus Mender II Meniscal Repair System (Smith & Nephew, London and Hull, UK) needle is advanced through the lateral capsule and into the meniscus. The intention of the first suture is to provide reduction vectors on the tear. The first needle is passed at an oblique angle to the tear, anterior-to-posterior, and enters the posterior segment of the meniscus through the tear, exiting on the top surface. A 2- to 3-cm transverse incision, directly on the joint line, is then made. Skin flaps are gently elevated exposing the capsule. The suture passer that comes with the Meniscus Mender II system is substituted with a Chia Percpasser (DePuy Synthes, Raynham, MA). This is longer and has the advantage of being able to be brought out of the anterolateral portal while having its tail remain outside of the lateral knee. The loop of the Chia is introduced into the knee joint through the needle and brought out of the anterolateral portal using an atraumatic grasper. A 0-nonabsorbable suture is passed through the Chia loop and pulled through the meniscus and lateral capsule. One limb of the suture still remains through the anterolateral cannula. A second outside-in pass is undertaken. This is in the opposite direction to the first pass and, therefore, has a starting point on the lateral capsule more posterior to the first pass. The needle is advanced through the lateral capsule and into the anterior segment of the meniscus through the tear at an oblique angle, posterior-to-anterior, and exits on the top surface (Fig 2B). The insertion and retrieval of the Chia suture passer is repeated, and the loop pulled out of the anterolateral cannula. The suture limb is inserted through the loop and brought out of the lateral capsule. By gently pulling on both limbs simultaneously while viewing arthroscopically, the meniscus tear should begin to reduce. If not, an additional crossing suture may need to be placed. Both suture limbs are then tagged for ease of identification. During the process of inserting the needles, the meniscus can be stabilized with a spinal needle introduced into the knee via the anterolateral portal (Fig 3).
Fig 3.
Viewing from the anteromedial portal in the left knee, a spinal needle (white arrow) may be introduced through the anterolateral portal to stabilize the lateral meniscus during needle insertion.
The second suture is placed in a standard horizontal mattress fashion. The needle (parallel or straight) is inserted through the skin opening and into the meniscus, parallel to and slightly posterior to the tear, exiting on the undersurface of the meniscus. The Chia suture passer is used and a 0-nonaborbable suture passed. The second needle is inserted parallel to the first, anterior to the tear, and exits on the undersurface of the meniscus (Fig 2C). The suture limb is passed and both limbs are tagged. During the process of inserting the needles, tension can be placed on the first suture passed to stabilize the meniscus.
The final suture is also placed in a standard horizontal mattress fashion, similar to the second suture, but this time exiting on the top surface of the meniscus (Fig 2D). It should either be slightly more central or peripheral than the first crossing suture, depending on the first suture's placement.
Relax the knee to a neutral position and tie the sutures over the lateral capsule in the order they were placed. It is important for the first 2 sutures that 1 limb is pulled gently and the other shortened so that if it was partially torn during the insertion of a needle, the partial tear is brought out of the knee. In this way the knot is not compromised. Reinsert the arthroscope and inspect the repair (Fig 4A). In this case, before repair, the lateral meniscus could be seen extruded into the lateral gutter (Fig 4B). With the repair complete, the meniscus was no longer extruded.
Fig 4.
(A) After all suture limbs are tied down, the left lateral meniscus is inspected and gently probed while viewing from the anteromedial portal. A stable repair can be appreciated (arrow). (B) Before repair, the left lateral meniscus is seen extruded into the lateral gutter when viewing from the anterolateral portal. The meniscus is no longer functional when extruded. This leads to increased force across the joint and degenerative arthritic changes of the lateral compartment.
Rehabilitation
For the first 5 weeks after surgery, the knee range of motion is limited to 90° of flexion and weight bearing to 50%. A hinged knee brace is worn at all times. After 5 weeks, the use of the brace is discontinued and the patient may begin full knee range of motion and full weight bearing. Sport-specific drills are allowed around 3 months after surgery. Full return to sport involving pivoting, squatting, twisting, and running is typically allowed at 5 months postoperatively.
Discussion
Complete radial tears of the lateral meniscus have deleterious and irreversible effects on the lateral compartment of the knee. Repair of such tears can restore the protective biomechanical effects of the meniscus. Varying techniques including all-inside, inside-out, or outside-in can be used for repair. Regardless of the technique, good results have been reported in a number of smaller studies.5, 7, 8
Choi et al.5 described an all-inside repair technique in 14 consecutive patients with lateral meniscus midbody radial tears. A suture hook was used to pass the absorbable suture in a side-to-side manner spanning the tear. Follow-up magnetic resonance imaging performed on all 14 patients demonstrated complete or partial healing in all but one patient. Ra et al. reported on 12 patients with complete radial tears of the meniscus that were treated with inside-out repair and fibrin clot. All patients received a follow-up magnetic resonance imaging at an average of 14 months postoperatively that showed complete healing.7
The outside-in repair technique is effective for most meniscal tears and has indications similar to those for the inside-out technique.9, 10 We find it particularly useful for radial tears of the body and anterior horn. An advantage of the outside-in technique is that it gives the surgeon the ability to control the distance between suture limbs when tying over the lateral capsule (Table 1). This is difficult to achieve when performing an inside-out repair. All-inside repair requires either a permanent knot to be tied inside the joint or absorbable suture to be used. All-inside devices do not allow for proper reduction vectors, especially of tears involving the anterior horn body junction. The success of our reduction is predicated on the crossing, horizontal mattress suture. The force vectors applied by the crossing pattern bring the posterior leaflet anterior and the anterior leaflet posterior. The repair is further backed up by 2 horizontal mattress sutures. With proper tensioning, this creates an excellent reduction of the tear.
Table 1.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
|
|
A disadvantage of this technique is the need for an additional incision. Although it is only slightly larger than a standard portal, it has the potential for wound issues. An additional disadvantage is the technical difficulty in performing this technique. Sutures need to be placed at a precise location so as to reduce the meniscus and avoid piercing previously placed sutures (Table 2).
Table 2.
Pearls and Pitfalls
|
Footnotes
The authors report the following potential conflicts of interest or sources of funding: D.R.D. receives consultancy fees from Depuy Mitek; and has patent (planned, pending, or issued) in Smith & Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Outside-in repair technique for a complete radial tear of the left lateral meniscus in a 17-year-old boy who sustained an acute noncontact twisting injury during a basketball game. The success of the repair is predicated on a crossing, horizontal mattress suture, which applies force vectors on the meniscus that bring the anterior and posterior leaflets of the meniscus together, reducing the tear. Two additional horizontal mattress sutures, one on the top and one on the undersurface of the meniscus, are placed to supplement the repair. The crossing suture is the first to be tied down over the lateral capsule, followed by the remaining sutures.
References
- 1.Wojtys E.M., Chan D.B. Meniscus structure and function. Instr Course Lect. 2005;54:323–330. [PubMed] [Google Scholar]
- 2.LaPrade C.M., Jansson K.S., Dornan G., Smith S.D., Wijdicks C.A., LaPrade R.F. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96:471–479. doi: 10.2106/JBJS.L.01252. [DOI] [PubMed] [Google Scholar]
- 3.Ode G.E., Van Thiel G.S., McArthur S.A. Effects of serial sectioning and repair of radial tears in the lateral meniscus. Am J Sports Med. 2012;40:1863–1870. doi: 10.1177/0363546512453291. [DOI] [PubMed] [Google Scholar]
- 4.Bhatia S., Civitarese D.M., Turnbull T.L. A novel repair method for radial tears of the medial meniscus: Biomechanical comparison of transtibial 2-tunnel and double horizontal mattress suture techniques under cyclic loading. Am J Sports Med. 2016;44:639–645. doi: 10.1177/0363546515615565. [DOI] [PubMed] [Google Scholar]
- 5.Choi N.H., Kim T.H., Son K.M., Victoroff B.N. Meniscal repair for radial tears of the midbody of the lateral meniscus. Am J Sports Med. 2010;38:2472–2476. doi: 10.1177/0363546510376736. [DOI] [PubMed] [Google Scholar]
- 6.Yoo J.C., Ahn J.H., Lee S.H., Lee S.H., Kim J.H. Suturing complete radial tears of the lateral meniscus. Arthroscopy. 2007;23:1249.e1–1249.e7. doi: 10.1016/j.arthro.2006.07.056. [DOI] [PubMed] [Google Scholar]
- 7.Ra H.J., Ha J.K., Jang S.H., Lee D.W., Kim J.G. Arthroscopic inside-out repair of complete radial tears of the meniscus with a fibrin clot. Knee Surg Sports Traumatol Arthrosc. 2013;21:2126–2130. doi: 10.1007/s00167-012-2191-3. [DOI] [PubMed] [Google Scholar]
- 8.Moulton S.G., Bhatia S., Civitarese D.M., Frank R.M., Dean C.S., LaPrade R.F. Surgical techniques and outcomes of repairing meniscal radial tears: A systematic review. Arthroscopy. 2016;32:1919–1925. doi: 10.1016/j.arthro.2016.03.029. [DOI] [PubMed] [Google Scholar]
- 9.Menge T.J., Dean C.S., Chahla J., Mitchell J.J., LaPrade R.F. Anterior horn meniscal repair using an outside-in suture technique. Arthrosc Tech. 2016;30:e1111–e1116. doi: 10.1016/j.eats.2016.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thompson S.M., Spalding T., Church S. A novel and cheap method of outside-in meniscal repair for anterior horn tears. Arthrosc Tech. 2014;3:e233–e235. doi: 10.1016/j.eats.2013.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Outside-in repair technique for a complete radial tear of the left lateral meniscus in a 17-year-old boy who sustained an acute noncontact twisting injury during a basketball game. The success of the repair is predicated on a crossing, horizontal mattress suture, which applies force vectors on the meniscus that bring the anterior and posterior leaflets of the meniscus together, reducing the tear. Two additional horizontal mattress sutures, one on the top and one on the undersurface of the meniscus, are placed to supplement the repair. The crossing suture is the first to be tied down over the lateral capsule, followed by the remaining sutures.