Abstract
Background
The long‐term incidence of acute appendicitis has been reported to be declining in Europe and North America. Recent reports, however, indicate stabilized or even increased rates. The aim of this study was to investigate the present epidemiology of acute appendicitis and appendicectomy in a population‐based cohort of Swedish children.
Methods
The Swedish National Patient Register was queried for all children with acute appendicitis and/or appendicectomy in 1987–2013. Population‐based incidence rates were calculated. Rates were age‐ and sex‐adjusted, and analysed for temporal and regional trends.
Results
Some 56 774 children with acute appendicitis were identified, of whom 53 478 (94·2 per cent) underwent appendicectomy. The incidence rate of acute appendicitis declined by 43·7 per cent over 26 years, from 177·7 to 100·1 per 100 000 person‐years between 1987 and 2013. The most significant reduction was for non‐perforated appendicitis, from 138·5 to 68·4 per 100 000 person‐years between 1987 and 2009. The incidence rate of perforated appendicitis decreased from 28·0 to 19·9 per 100 000 person‐years and negative appendicectomies reduced from 48·5 to 3·6 per 100 000 person‐years during the study interval.
Conclusion
The incidence rates of acute appendicitis and negative appendicectomy have reduced markedly in Swedish children over time, with significantly different trends amongst non‐perforated appendicitis and perforated appendicitis. The full explanation for the observed findings is unclear.
Introduction
The epidemiology and natural course of acute appendicitis are still not fully understood. The life‐time risk of acute appendicitis is estimated to be 7–8 per cent1. Studies from Europe and North America report decreasing rates of acute appendicitis, both in general1, 2, 3, 4 and in children5 6. There have been, however, more recent reports of stabilized7 8 or even increased9, 10, 11 incidence rates during the first decade of the 21st century.
Since the late 20th century, strategies for diagnosing and treating acute appendicitis have changed. Novel diagnostic modalities including ultrasonography and CT have been introduced12 13. More expectant strategies regarding the treatment of acute appendicitis have gradually been adopted, replacing previous standards of performing emergency surgery in all patients with suspected appendicitis, accepting a high rate of negative appendicectomy to avoid possible perforation14 15.
The aim of this study was to investigate the epidemiology of acute appendicitis and appendicectomy in a population‐based cohort of Swedish children, to reveal whether the previously described decreasing incidence rate of appendicitis continues. Secondary aims were to analyse appendicitis subtype epidemiology and to identify regional trends and differences.
Methods
Data collection
This was a population‐based retrospective cohort study. Data were collected from the Swedish National Patient Register (NPR), which contains data on all patients admitted to hospital in Sweden from 1987. The NPR was queried for all children in Sweden aged 0–14 years, discharged from hospital with a diagnosis of acute appendicitis and/or appendicectomy between 1987 and 2013. Population statistics including annual population base, with age and sex distributions, were retrieved from Statistics Sweden.
The study was approved by the Regional Ethics Review Board in Stockholm (reference number 2014/1018‐31/4). Results are reported in accordance with the STROBE guidelines16.
Definitions
Definitions of acute appendicitis and appendicitis subtypes were based on discharge diagnoses reported to the NPR, according to the Swedish version of ICD‐9 and ICD‐10 classifications. The degree to which discharge diagnoses reported to the NPR were based on clinical diagnosis or histopathological examinations was not specified. Non‐perforated appendicitis was defined by codes 540X, 541X, 542X, K359, K369, K379 or K389, and perforated appendicitis by codes 540A, 540B, K350 or K351. Appendicectomy was defined by codes 4510, 4511, JEA00 or JEA10 (open appendicectomy) and 4517 or JEA01 (laparoscopic appendicectomy). Negative appendicectomy was defined by the combination of appendicectomy without acute appendicitis diagnosis plus one of several discharge diagnoses indicating that appendicectomy had been performed owing to suspected appendicitis (mesenteric lymphadenitis 289c, i880 or i889, non‐specific abdominal pain 789a or R100–R104). Incidental appendicectomies, defined by the combination of appendicectomy not accompanied by an acute appendicitis diagnosis or a diagnosis code indicating appendicitis‐suspected abdominal pain, were excluded from the study. Appendicitis treated without surgery, defined by appendicitis diagnosis without appendicectomy, was registered for descriptive purposes but, owing to the poor definition of this group, these data were not analysed further. Negative laparoscopies for suspected appendicitis without appendicectomy were not possible to identify in the NPR and were therefore not analysed.
Statistical analysis
Population‐based incidence rates of diagnosed and operated acute appendicitis, appendicitis subtypes and negative appendicectomy were calculated. Incidence rates were also calculated for age groups (categorized into 5‐year intervals) and by sex. In addition, incidence rates were analysed on a regional basis according to the six healthcare regions of Sweden.
To estimate incidence rate trends, a Poisson regression model was created with time (year of event) as the explanatory variable and 100 000 person‐years per year as the offset variable. The surgical method, open or laparoscopic appendicectomy, was introduced to the model to exclude bias imposed on the incidence rates or trends of overall acute appendicitis, appendicitis subtypes and negative appendicectomy. For analysis of differences between age groups, incidence rates were standardized for sex. For analyses by sex, data were standardized for age (categorized). For analysis of regional differences and trends, incidence rates were standardized for both age (categorized) and sex distributions using the Stockholm region as reference.
Differences in incidence rates and trends between age groups, sex and healthcare regions were estimated by adding these variables to the regression model, testing for interaction by year of event.
Owing to revised definitions in the ICD‐10 subclassification of perforated and non‐perforated appendicitis, data on appendicitis subtype were not reliable from 201017. Therefore, analyses on overall acute appendicitis, overall appendicectomy and negative appendicectomy included data for the years 1987–2013; subanalyses of perforated and non‐perforated appendicitis included data for 1987–2009. Accordingly, either the incidence rate year 2013 or 2009 was used as reference in the Poisson regression analysis.
Statistical analyses were performed in R statistical software (R Foundation for Statistical Computing, Vienna, Austria)18.
Results
Patient characteristics and clinical features are presented in Table 1. Some 64 971 children registered in the NPR between 1987 and 2013 were eligible for the study; 56 774 had a diagnosis of acute appendicitis, 3296 (5·8 per cent) of whom were treated without surgery. The incidence rate of appendicitis treated without surgery was stable over the study interval. Appendicectomy was performed in 61 675 children, 53 478 (86·7 per cent) with a diagnosis of acute appendicitis and 8197 (13·3 per cent) who had a negative appendicectomy; their details were further analysed in the Poisson model. When restricted to 1987–2009, 37 887 appendicectomies (79·5 per cent) were performed for non‐perforated and 9790 (20·5 per cent) for perforated appendicitis.
Table 1.
Demographic and clinical characteristics of the cohort
| All appendicectomies 1987–2013 | Appendicectomy with appendicitis 1987–2009 | |||||
|---|---|---|---|---|---|---|
| Appendicitis all grades (n = 53 478) | Negative appendicectomy (n = 8197) | Total (n = 61 675) | Non‐perforated appendicitis (n = 37 887) | Perforated appendicitis (n = 9790) | Total (n = 47 677) | |
| Age (years)* | 10·8(2·9) | 10·3(3·1) | 10·7(2·9) | 11·1(2·7) | 9·9(3·5) | 10·8(2·9) |
| Age group (years) | ||||||
| 0–4 | 2566 (81·4) | 585 (18·6) | 3151 | 1019 (46·7) | 1161 (53·3) | 2180 |
| 5–9 | 15 966 (85·5) | 2701 (14·5) | 18 667 | 10 912 (76·8) | 3300 (23·2) | 14 212 |
| 10–14 | 34 946 (87·7) | 4911 (12·3) | 39 857 | 25 956 (83·0) | 5329 (17·0) | 31 285 |
| Sex ratio (M : F) | 30 570 : 22 908 | 3449 : 4748 | 34 019 : 27 656 | 21 816 : 16 071 | 5285 : 4505 | 27 101 : 20 576 |
| Type of surgery | ||||||
| Laparoscopic | 5137 (95·3) | 252 (4·7) | 5389 | 2097 (82·6) | 441 (17·4) | 2538 |
| Open | 48 341 (85·9) | 7945 (14·1) | 56 286 | 35 790 (79·3) | 9349 (20·7) | 45 139 |
| Healthcare region | ||||||
| Northern | 5569 (85·2) | 964 (14·8) | 6533 | 4065 (79·7) | 1035 (20·3) | 5100 |
| Stockholm | 10 245 (91·1) | 997 (8·9) | 11 242 | 6514 (74·7) | 2203 (25·3) | 8717 |
| South‐Eastern | 5884 (84·6) | 1073 (15·4) | 6957 | 4268 (79·6) | 1095 (20·4) | 5363 |
| Southern | 8334 (85·7) | 1387 (14·3) | 9721 | 6012 (80·7) | 1435 (19·3) | 7447 |
| Uppsala/Örebro | 12 225 (86·0) | 1996 (14·0) | 14 221 | 8946 (80·8) | 2122 (19·2) | 11 068 |
| Western | 11 221 (86·3) | 1780 (13·7) | 13 001 | 8082 (81·0) | 1900 (19·0) | 9982 |
| Year of treatment | ||||||
| 1987–1989 | 7198 (77·9) | 2045 (22·1) | 9243 | 5961 (82·8) | 1237 (17·2) | 7198 |
| 1990–1994 | 10 708 (81·1) | 2498 (18·9) | 13 206 | 8661 (80·9) | 2047 (19·1) | 10 708 |
| 1995–1999 | 11 298 (87·6) | 1592 (12·4) | 12 890 | 8890 (78·7) | 2408 (21·3) | 11 298 |
| 2000–2004 | 10 688 (90·5) | 1121 (9·5) | 11 809 | 8336 (78·0) | 2352 (22·0) | 10 688 |
| 2005–2009 | 7785 (92·8) | 607 (7·2) | 8392 | 6039 (77·6) | 1746 (22·4) | 7785 |
| 2010–2013 | 5801 (94·6) | 334 (5·4) | 6135 | † | † | 5801 |
Values in parentheses are percentages unless indicated otherwise;
values are mean(s.d.).
Data in the National Patient Register on subclassification into non‐perforated and perforated appendicitis were not valid from 201017.
Overall appendicitis and appendicitis subtypes
The overall incidence rate of acute appendicitis declined by 43·7 per cent over 26 years in children in Sweden, from 177·7 to 100·1 per 100 000 person‐years between 1987 and 2013 (Fig. 1). The greatest reduction was for non‐perforated appendicitis, with a 50·6 per cent reduction from 138·5 to 68·4 per 100 000 person‐years between 1987 and 2009. The incidence rate of perforated appendicitis was also reduced by 28·9 per cent, from 28·0 to 19·9 per 100 000 person‐years between 1987 and 2009. Estimated incidence rates remained significantly reduced after adjusting for age, sex and operative method in the Poisson regression model (Fig. 2). Estimated trends of non‐perforated appendicitis and perforated appendicitis incidence rates diverged significantly (P = 0·007), indicating different epidemiological features of the two.
Figure 1.
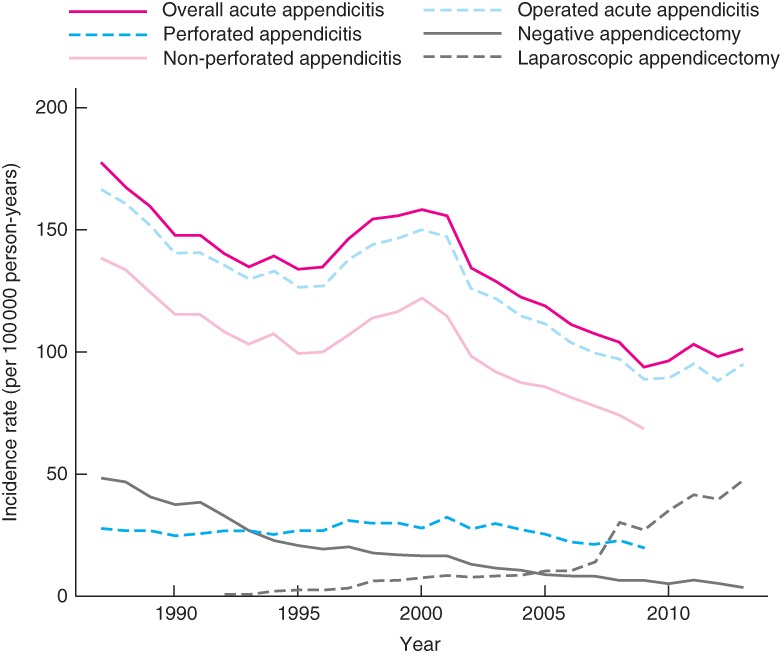
Crude incidence rates for overall appendicitis and appendicitis subtypes in children in Sweden in 1987–2013
Figure 2.
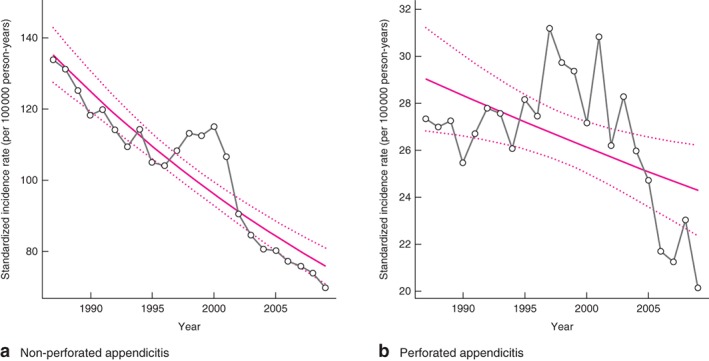
Incidence rates and estimated trends with 95 per cent confidence intervals for a non‐perforated and b perforated appendicitis in children in Sweden in 1987–2009. Estimated trends were significantly different from zero (no change over time). a P < 0·001, b P = 0·015 (Poisson regression model)
Sex
Absolute incidence rates of acute appendicitis reduced for both boys and girls during the study period. The reduction was more pronounced in girls, resulting in an increased difference between the sexes over time; in 2013 there was a 30 per cent lower estimated incidence rate of acute appendicitis in girls (P < 0·001) (Fig. 3).
Figure 3.
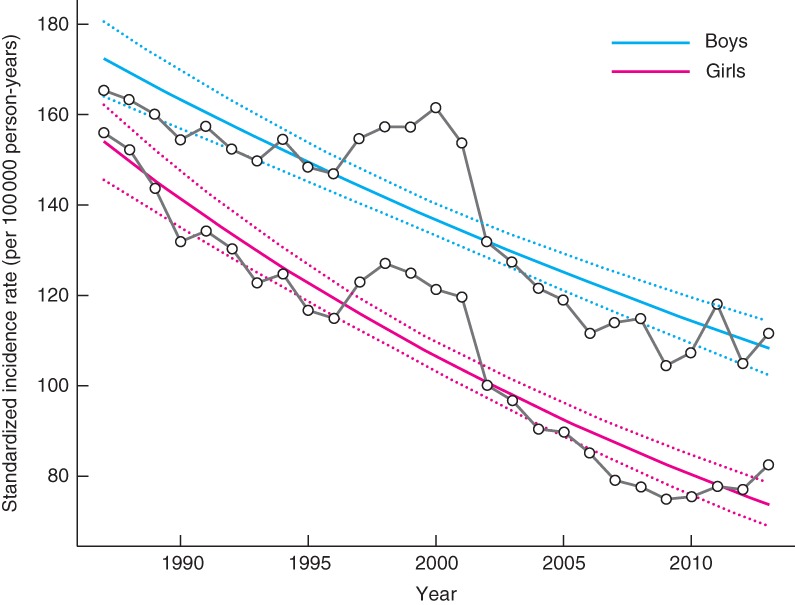
Incidence rates and estimated trends with 95 per cent confidence intervals for acute appendicitis in girls and boys in Sweden in 1987–2013. Estimated trends were significantly different from zero (no change over time). P < 0·001 for both boys and girls (Poisson regression model)
Age
Absolute incidence rates of acute appendicitis decreased in all age groups during the study interval, as did those for non‐perforated and perforated appendicitis. For non‐perforated appendicitis, the magnitude of the estimated reduction correlated positively with patient age, with a more pronounced reduction in older children. A similar, non‐significant, correlation was found between perforated appendicitis and age (Fig. 4).
Figure 4.
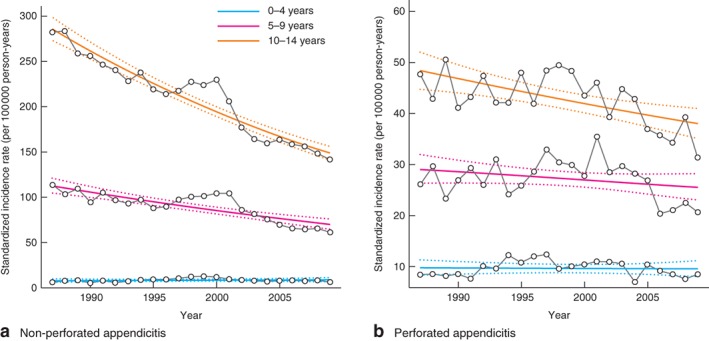
Incidence rates and estimated trends with 95 per cent confidence intervals for a non‐perforated and b perforated appendicitis in children in Sweden in 1987–2009 in the three age groups: 0–4, 5–9 and 10–14 years
Negative appendicectomy
The incidence rate of negative appendicectomy fell by 92·6 per cent, from 48·5 to 3·6 per 100 000 person‐years between 1987 and 2013. The incidence rate of negative appendicectomy was two times higher in girls than in boys in 1987, but a significantly greater reduction of negative appendicectomy in girls resulted in similar incidence rates and converged estimated trends of negative appendicectomy between the sexes in 2013 (P = 0·136) (Fig. 5).
Figure 5.
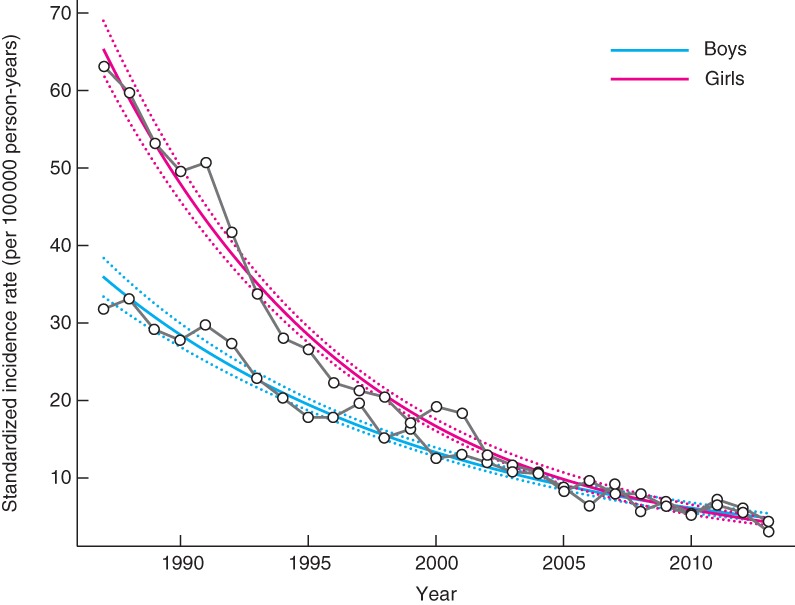
Incidence rate and estimated trends with 95 per cent confidence intervals for negative appendicectomy in girls and boys in Sweden in 1987–2013. Estimated trends were significantly different from zero (no change over time). P < 0·001 for both boys and girls (Poisson regression model)
Healthcare regions
In the early study period, the estimated incidence rates of acute appendicitis were higher in all other healthcare regions in Sweden compared with the Stockholm region. Over time, incidence rates decreased proportionately more in these other healthcare regions, and in the later study period incidence rate trends were converging across Sweden, including Stockholm. In 2013, estimated incidence rates were comparable in the four central/northern regions, but lower in the Southern and South‐Eastern healthcare regions (Fig. 6).
Figure 6.
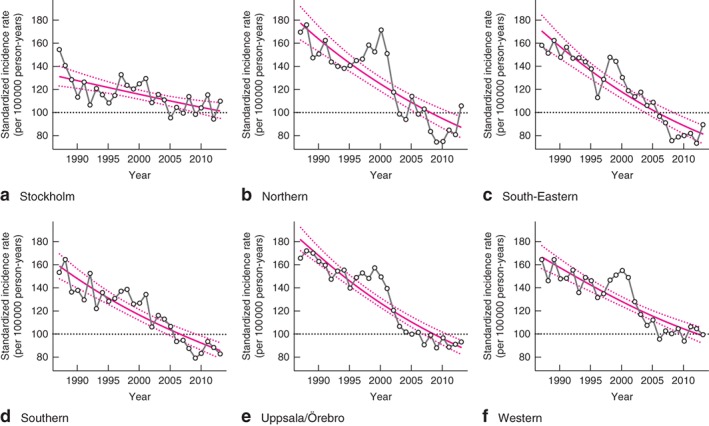
Incidence rates and estimated trends with 95 per cent confidence intervals for overall appendicitis in children in Sweden on 1987–2013 according to healthcare region: a Stockholm, b Northern, c South‐Eastern, d Southern, e Uppsala/Örebro, f Western
Transiently increased rates in 1997–2002
Incidence rates of overall acute appendicitis and appendicitis subtypes increased transiently between 1997 and 2002 (Fig. 1). This finding remained after adjusting for available confounders including birth cohort changes, sex distribution, operative technique (open versus laparoscopic appendicectomy) and healthcare region. The transient increase was more pronounced for non‐perforated than for perforated appendicitis, and differed in magnitude between healthcare regions, being less evident in the Stockholm region (Fig. 6).
Operative technique
The first laparoscopic appendicectomies in children in Sweden were performed in 1992, and the minimal‐access surgical method has been used increasingly since then. In 2013, every second appendicectomy in Swedish children was performed laparoscopically. The introduction and increased use of laparoscopic operations did not correlate statistically with the incidence reductions of overall appendicitis, appendicitis subtype or negative appendicectomy (Fig. 1).
Discussion
This is the largest population‐based epidemiological study on acute appendicitis in children to date, including 65 000 children over a 26‐year period. The study found markedly decreasing incidence rates of non‐perforated appendicitis and perforated appendicitis in children, with significantly different trends indicating epidemiological differences between the two. Further, for non‐perforated appendicitis the decreasing incidence rate was more pronounced in older children. Due to a more pronounced reduction of the incidence rate in girls, appendicitis in Swedish children is now more common in boys. The incidence rate of negative appendicectomy decreased dramatically over the study period, and for negative appendicectomy differences between the sexes diminished. Finally, regional differences were reduced over time, indicating converging strategies in the diagnosis and treatment of appendicitis.
The NPR has a near 100 per cent coverage and yields highly valid data, allowing high‐quality longitudinal epidemiological studies on a population basis19. Reliable, detailed population data from Statistics Sweden for standardization and adjustments further reduced potential bias. However, register‐based cohort studies are subjected to potential confounding by the information bias introduced using register data. The distinction between non‐perforated and perforated appendicitis was based on ICD‐9 or ICD‐10 discharge diagnoses derived from clinical diagnosis at appendicectomy in most cases. Surgeon grading has been shown previously20 21 to correlate imperfectly with histopathological diagnosis. The 2010 revision of the ICD‐10 confounded subsequent subgroup coding into non‐perforated and perforated appendicitis17, reducing the length of the study interval available for subgroup analysis. In addition, the definition of negative appendicectomy was introduced retrospectively, as there was no separate ICD coding for that event.
A significant number of children (5·8 per cent of those with appendicitis) were discharged with an appendicitis diagnosis without having an appendicectomy, possibly indicating non‐operative treatment for simple or complex appendicitis and appendiceal abscess or spontaneously resolving appendicitis. The incidence rate of appendicitis treated without surgery was stable throughout the study period, but this was not investigated further owing to plausible heterogeneity within the group and unreliable diagnostic criteria.
After the introduction of laparoscopic surgery for suspected appendicitis, a proportion of patients were probably subjected to laparoscopy for suspected appendicitis with negative finding, and thus no appendicectomy. These patients would, before the laparoscopic era, have been classified as having had a negative appendicectomy, and the new operative technique may possibly have contributed to the observed reduction of registered negative appendicectomies. However, a major reduction in negative appendicectomies was observed before the introduction of laparoscopic appendicectomy, and the reduction rate of negative appendicectomy did not correlate with the increased use of laparoscopic surgery.
The findings of declining acute appendicitis incidence rates during the study period are consistent with previous findings of long‐term reduced incidence rates of appendicitis, in both adults and children. Arnbjörnsson2 showed a steadily increasing incidence of acute appendicitis during the first half of the 20th century. This may be related to the development of modern medicine with increasing healthcare standards and better availability of surgical care. The incidence rate was reported to decrease markedly between 1950 and 1965, with a less steep decrease between 1965 and 1980. Several studies1 3, 4 22, 23 have reported further reduced incidence rates of acute appendicitis in North America and Europe. In addition, in studies with a paediatric focus, the incidence rate of acute appendicitis has previously been reported to decline. In a study based on data from the Danish National Patient Register, Andersen and colleagues5 reported a 13–36 per cent reduction in non‐perforated appendicitis in children over a 9‐year period from 1996 to 2004, and a 10 per cent reduction in perforated appendicitis. Reduced incidence of acute appendicitis in children was also reported by Aarabi and co‐workers6 in New England in 2000–2006. In contrast to these reports of declining rates, increased rates of appendicitis were reported from Norway8 and the USA10 11, and Livingston et al.9 identified a J‐shaped incidence rate trend, with increasing acute appendicitis rates in children in the USA up to 2004. The present study revealed a corresponding, but transient, increased incidence rate in Swedish children between 1997 and 2002, followed by a continued reduction. This temporary increase may be argued to have coincided with the introduction of radiological tools for the diagnosis of acute appendicitis in children. There are no general data on the introduction or use of radiology in diagnosing acute appendicitis in Sweden. Ultrasonography, and subsequently CT, was introduced for diagnosing appendicitis in adults in the late 1980s12. In Stockholm, Kaiser and colleagues13 reported the outcome of the introduction of ultrasonography and CT for diagnosing acute appendicitis in children, finding stable incidence rates during the introduction. Most importantly, the increased incidence rates in the present study were transient, proving that, in the long term, the introduction of ultrasonography and CT did not increase the incidence rate of diagnosed acute appendicitis in children. The transient increase also coincides with the conversion in coding systems from ICD‐9 to ICD‐10. However, there were no major changes in the coding that could explain such an influence.
The main findings of this study may reflect a true reduction of acute appendicitis in children, but the NPR data used for the study do not reveal any clear explanations for the findings. The reduced incidence rates may also reflect a long‐term change in attitudes towards acute appendicitis and its consequences, resulting in more expectant treatment strategies, subsequently leading to a reduced proportion of true acute appendicitis cases being diagnosed, operated on, and hence registered. This would be likely only if a considerable proportion of mild cases of acute appendicitis underwent spontaneous resolution if not actively diagnosed and treated, as proposed by Andersson14. Moreover, that assumption also fits well with the pronounced reduction of non‐perforated appendicitis compared with perforated cases demonstrated. The finding of marked differences in the epidemiology between non‐perforated and perforated appendicitis also reinforces previous theories that the two subgroups of appendicitis actually are different diseases with different aetiology and pathogenesis24.
Observed sex differences may also be related to changed attitudes in diagnosing and treating acute appendicitis. In boys, with fewer differential diagnoses to acute appendicitis compared with girls, a lower threshold to early appendicectomy may explain the trend of increased incidence rate differences between the sexes. The combination of more expectant strategies and improved specificity of modern diagnostic pathways to rule out differential diagnoses to acute appendicitis in girls probably explains the more marked reduction of negative appendicectomy in girls.
The findings of a continued reduction of the population‐based incidence of acute appendicitis and diverging trends for non‐perforated and perforated appendicitis will have implications for future healthcare provision and appendicitis research. This study provides strong evidence of a continuously reduced incidence rate of acute appendicitis and appendicectomies, but the study design, based on healthcare register data, lacks the tools to provide further aetiological explanations.
Acknowledgements
Grant support was received from the Swedish Research Council, the Swedish Free Masons' Foundation for Children's Welfare, the Her Royal Highness Crown Princess Lovisa's Foundation and the Foundation Sällskapet Barnavård.
Disclosure: The authors declare no conflict of interest.
Funding information
HRH Crown Princess Lovisa's Foundation
The Swedish Free Masons Foundation for Children's Welfare
Foundation Sällskapet Barnavård
Vetenskapsrådet
References
- 1. Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 1990; 132: 910–925. [DOI] [PubMed] [Google Scholar]
- 2. Arnbjörnsson E. [Epidemiology of appendicitis.] Lakartidningen 1983; 80: 4278–4279. [PubMed] [Google Scholar]
- 3. Noer T. Decreasing incidence of acute appendicitis. Acta Chir Scand 1975; 141: 431–432. [PubMed] [Google Scholar]
- 4. Kang JY, Hoare J, Majeed A, Williamson RC, Maxwell JD. Decline in admission rates for acute appendicitis in England. Br J Surg 2003; 90: 1586–1592. [DOI] [PubMed] [Google Scholar]
- 5. Andersen SB, Paerregaard A, Larsen K. Changes in the epidemiology of acute appendicitis and appendectomy in Danish children 1996–2004. Eur J Pediatr Surg 2009; 19: 286–289. [DOI] [PubMed] [Google Scholar]
- 6. Aarabi S, Sidhwa F, Riehle KJ, Chen Q, Mooney DP. Pediatric appendicitis in New England: epidemiology and outcomes. J Pediatr Surg 2011; 46: 1106–1114. [DOI] [PubMed] [Google Scholar]
- 7. Blomqvist P, Ljung H, Nyren O, Ekbom A. Appendectomy in Sweden 1989–1993 assessed by the Inpatient Registry. J Clin Epidemiol 1998; 51: 859–865. [DOI] [PubMed] [Google Scholar]
- 8. Körner H, Söreide JA, Pedersen EJ, Bru T, Söndenaa K, Vatten L. Stability in incidence of acute appendicitis. A population‐based longitudinal study. Dig Surg 2001; 18: 61–66. [DOI] [PubMed] [Google Scholar]
- 9. Livingston EH, Fomby TB, Woodward WA, Haley RW. Epidemiological similarities between appendicitis and diverticulitis suggesting a common underlying pathogenesis. Arch Surg 2011; 146: 308–314. [DOI] [PubMed] [Google Scholar]
- 10. Anderson JE, Bickler SW, Chang DC, Talamini MA. Examining a common disease with unknown etiology: trends in epidemiology and surgical management of appendicitis in California, 1995–2009. World J Surg 2012; 36: 2787–2794. [DOI] [PubMed] [Google Scholar]
- 11. Buckius MT, McGrath B, Monk J, Grim R, Bell T, Ahuja V. Changing epidemiology of acute appendicitis in the United States: study period 1993–2008. J Surg Res 2012; 175: 185–190. [DOI] [PubMed] [Google Scholar]
- 12. Puylaert JB. Acute appendicitis: US evaluation using graded compression. Radiology 1986; 158: 355–360. [DOI] [PubMed] [Google Scholar]
- 13. Kaiser S, Frenckner B, Jorulf HK. Suspected appendicitis in children: US and CT – a prospective randomized study. Radiology 2002; 223: 633–638. [DOI] [PubMed] [Google Scholar]
- 14. Andersson RE. The natural history and traditional management of appendicitis revisited: spontaneous resolution and predominance of prehospital perforations imply that a correct diagnosis is more important than an early diagnosis. World J Surg 2007; 31: 86–92. [DOI] [PubMed] [Google Scholar]
- 15. Howie JG. Too few appendectomies? Lancet 1964; 1: 1240–1242. [DOI] [PubMed] [Google Scholar]
- 16. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; Initiative STROBE. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008; 61: 344–349. [DOI] [PubMed] [Google Scholar]
- 17. Andersson RE. [Confusing diagnosis coding prevents historical and international comparisons. Diagnosing should be unambiguous and consistent.] Lakartidningen 2015; 112: pii: DDWH. [PubMed]
- 18. Core Team R. R: a Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, 2016. [Google Scholar]
- 19. Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C et al External review and validation of the Swedish national inpatient register. BMC Public Health 2011; 11: 450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ponsky TA, Hafi M, Heiss K, Dinsmore J, Newman KD, Gilbert J. Interobserver variation in the assessment of appendiceal perforation. J Laparoendosc Adv Surg Tech A 2009; 19(Suppl 1): S15–S18. [DOI] [PubMed] [Google Scholar]
- 21. Bliss D, McKee J, Cho D, Krishnaswami S, Zallen G, Harrison M et al Discordance of the pediatric surgeon's intraoperative assessment of pediatric appendicitis with the pathologists report. J Pediatr Surg 2010; 45: 1398–1403. [DOI] [PubMed] [Google Scholar]
- 22. Williams NM, Jackson D, Everson NW, Johnstone JM. Is the incidence of acute appendicitis really falling? Ann R Coll Surg Engl 1998; 80: 122–124. [PMC free article] [PubMed] [Google Scholar]
- 23. Al‐Omran M, Mamdani M, McLeod RS. Epidemiologic features of acute appendicitis in Ontario, Canada. Can J Surg 2003; 46: 263–268. [PMC free article] [PubMed] [Google Scholar]
- 24. Livingston EH, Woodward WA, Sarosi GA, Haley RW. Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg 2007; 245: 886–892. [DOI] [PMC free article] [PubMed] [Google Scholar]


