Abstract
Background
The Intercollegiate Membership of the Royal College of Surgeons (MRCS) examination is undertaken by large numbers of trainees in the UK and internationally as a mandatory step within surgical training. Unlike some high‐stakes medical examinations, the MRCS is yet to be validated. A quantitative study was undertaken to assess its predictive validity by investigating the relationship between MRCS (Parts A and B) and national selection interview scores for general and vascular surgery in the UK.
Methods
Pearson correlation coefficients were used to examine the linear relationship between each assessment, and linear regression analyses were employed to identify potential independent predictors of the national selection score. All UK medical graduates who attempted the interview in 2011–2015 were included.
Results
Some 84·4 per cent of the candidates (1231 of 1458) were matched with MRCS data. There was a significant positive correlation between the first attempt score at Part B of the MRCS examination and the national selection score (r = 0·38, P < 0·001). In multivariable analysis, 17 per cent of variance in the national selection first attempt score was explained by the Part B MRCS score and number of attempts (change in R 2 value of 0·10 and 0·07 respectively; P < 0·001). Candidates who required more than two attempts at Part B were predicted to score 8·1 per cent less than equally matched candidates who passed at their first attempt.
Conclusion
This study supports validity of the MRCS examination, and indicates its predictive value regarding entry into specialist training.
Introduction
The Intercollegiate Membership of the Royal College of Surgeons (MRCS) examination is one of the most widely offered postgraduate surgical examinations in the world, with up to 6000 doctors in the UK and overseas taking the examination each year1 2. An overview of the medical education and surgical training pathway in the UK is provided in Fig. 1. Upon graduating from medical school, newly qualified doctors enter the 2‐year Foundation Programme. Most doctors will continue their training in one of three broad specialist areas: general practice, medicine or surgery. To be considered for higher medical or surgical training, UK doctors must also complete core training and pass the relevant postgraduate examination, MRCS or Membership of the Royal Colleges of Physicians (MRCP). Overviews of the content of the MRCS examination and the specialty training selection process for general and vascular surgery have been described elsewhere2 3. The MRCS examination is designed to safeguard patients and ensure high standards for practising surgeons. It is a prerequisite for progression to higher specialty training in the UK, a mandatory examination for all aspiring surgeons who wish to train or work in the UK and a means for overseas candidates to improve their opportunities in their home country2 4.
Figure 1.

Surgical training pathway in the UK. MRCS, Membership of the Royal College of Surgeons; FRCS, Fellowship of the Royal College of Surgeons; GP, general practice
The Intercollegiate Committee for Basic Surgical Examinations (ICBSE), which is responsible for the continued development, quality assurance and standards of MRCS in the UK, produces an annual report highlighting examination reliability5. To date, there has been no analysis of the predictive validity of the MRCS examination, and it is not known whether performance at this examination predicts outcomes as a surgeon in training or beyond.
Given that MRCS is a prerequisite for progression to higher specialty training in the UK, it is important to determine the relationship between MRCS examination scores and outcomes in the higher specialty training national selection process. The aim of this study was to examine the predictive validity of MRCS in relation to outcomes in this selection process, and, specifically, whether the results of this mandatory examination can predict how candidates will perform at the national selection interview for a large surgical specialty, general surgery (which included vascular surgery in the UK until 2013).
Methods
In the absence of a specific ethics committee responsible for postgraduate surgical examinations, both the ICBSE and its Internal Quality Assurance subcommittee, which monitors standards, approved the study.
The sample included all UK medical graduates who had attempted Part B of the MRCS examination from its institution in October 2008 to May 2015. Data were extracted by the lead administrator from the intercollegiate MRCS database held by the Royal College of Surgeons (RCS) of England. Each candidate's Part A score was merged with their Part B score to create a complete MRCS history, which included the self‐declared demographics of sex, ethnicity, first language and date of birth.
Candidates were anonymized by a unique identifier before data were released for analysis. This identifier corresponded to each candidate's General Medical Council number, which could be accessed only by the RCS lead administrator and not by the research team.
All scores (recorded as percentages) for candidates who had attempted the national selection interview for general and vascular surgery since its origin in May 2011 were then cross‐linked with the MRCS database. The national selection first attempt score was used as the main outcome variable.
As the Part B examination underwent changes, three periods were considered: October 2008 to February 2010, May 2010 to October 2012, and February 2013 to present. Each of these periods was considered as one of the variables of interest.
As part of national selection, candidates are divided into three groups at the portfolio station based on how many years they are from graduation: less than 5 years, 5–7 years and more than 7 years. Years from graduation was also considered as a variable of interest.
As older doctors (aged at least 29 years at graduation from medical school) have been shown to have problems with their Annual Review of Competence Progression compared with younger colleagues6, this age‐related variable was also considered in the analyses.
Candidates were categorized based on their total number of attempts required to pass each part of the MRCS examination (1, 2, or 3 or more attempts).
Statistical analysis
All analyses were conducted using SPSS® version 24.0 (IBM, Armonk, New York, USA). Pearson correlation coefficients were used to examine the linear relationship between both parts of the MRCS examination and the national selection first attempt score. The magnitude of correlation was in accordance with Cohen's guidelines7 (r = 0·01–0·29, low or weak correlation; r = 0·30–0·49, moderate correlation; r ≥ 0·50, strong correlation). An independent‐samples t test or ANOVA was used to examine the relationship between MRCS and national selection scores and demographic variables, dependent on the number of categories being compared.
Linear regression analysis was used to identify potential independent predictors of the national selection score. All potential predictors with P < 0·100 in univariable analysis were entered simultaneously into the regression models. Any variable with P > 0·050 in the full model was subsequently removed until only statistically significant predictors remained in each model.
Stepwise linear regression analysis was used to measure the change in R2 when single predictors were added to the model in order to assess the magnitude of the contribution of new predictors in explaining variance in national selection score.
There were no violations of the assumptions for any of the regression models and no collinearity was evident in the data.
Results
A total of 1231 (84·4 per cent) of 1458 candidates long‐listed for the general and vascular surgery national selection process in the UK from May 2011 to May 2015 were matched with MRCS data (Fig. 2). Some 454 candidates could not be included: 305 were non‐UK graduates, nine had no GMC number available, four were duplicate entries and 136 had sat the MRCS examination in place before 2008. Of the remaining 777 candidates, three had incomplete Part A data available and were also excluded, so that 774 candidates were matched on MRCS and national selection data, and entered into the analysis.
Figure 2.
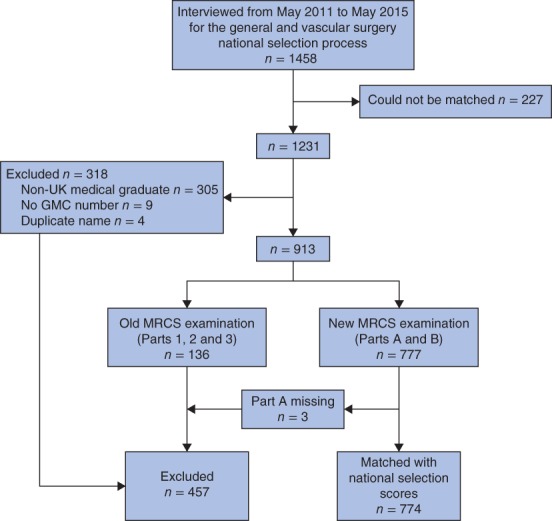
Flow diagram of surgical trainees in the study. GMC, General Medical Council; MRCS, Membership of the Royal College of Surgeons
The majority of national selection candidates were: white British (353 of 598, 59·0 per cent), men (440 of 772, 57·0 per cent), spoke English as their first language (571 of 611, 93·5 per cent) and graduated from medical school before the age of 29 years (734 of 772, 95·1 per cent). Only 13 (1·7 per cent) of 773 candidates attempted the national selection interview for the first time more than 7 years after graduating from medical school. More than half (423 of 773, 54·7 per cent) of the UK graduates in the cohort had passed the Part B MRCS examination between May 2010 and October 2012 (Table 1).
Table 1.
National selection descriptive statistics and the relationship between demographic variables and national selection first attempt score for general and vascular surgery
| National selection descriptive statistics (n = 774)* | National selection first attempt score (%)† | Test statistic‡ | d.f. | P | |
|---|---|---|---|---|---|
| Age (years)† | 29·18(2·68) | ||||
| Sex | 0·25§ | 754 | 0·804 | ||
| M | 440 (57·0) | 73·27(9·19) | |||
| F | 332 (43·0) | 73·43(8·01) | |||
| Missing | 2 | ||||
| Ethnicity | 6·22 | 4 | < 0·001 | ||
| White British | 353 (59·0) | 74·92(7·52) | |||
| Asian | 156 (26·1) | 71·32(8·14) | |||
| Black | 20 (3·3) | 72·09(9·67) | |||
| Other | 69 (11·5) | 71·43(10·33) | |||
| Missing | 176 | ||||
| First language | 2·70§ | 609 | 0·007 | ||
| English | 571 (93·5) | 73·72(8·11) | |||
| Not English | 40 (6·5) | 70·10(9·37) | |||
| Missing | 163 | ||||
| Mature medical graduate | 1·26§ | 770 | 0·209 | ||
| No (age < 29 years) | 734 (95·1) | 73·42(8·67) | |||
| Yes (≥ 29 years) | 38 (4·9) | 71·61(8·99) | |||
| Missing | 2 | ||||
| No. of Part A MRCS attempts | 4·64 | 2 | 0·010 | ||
| 1 | 598 (77·3) | 73·85(8·69) | |||
| 2 | 90 (11·6) | 71·14(8·45) | |||
| ≥ 3 | 86 (11·1) | 72·24(8·59) | |||
| No. of Part B MRCS attempts | 27·04 | 2 | < 0·001 | ||
| 1 | 581 (75·1) | 74·50(7·93) | |||
| 2 | 150 (19·4) | 71·01(10·10) | |||
| ≥ 3 | 43 (5·6) | 66·10(8·33) | |||
| Years from graduation | 1·64 | 2 | 0·196 | ||
| < 5 | 668 (86·4) | 73·49(8·61) | |||
| 5–7 | 92 (11·9) | 72·86(9·31) | |||
| > 7 | 13 (1·7) | 69·32(8·07) | |||
| Missing | 1 | ||||
| Part B examination date | 1·20 | 2 | 0·301 | ||
| October 2008 to February 2010 | 111 (14·4) | 73·14(11·07) | |||
| May 2010 to October 2012 | 423 (54·7) | 73·02(8·41) | |||
| February 2013 to present | 239 (30·9) | 74·09(7·91) | |||
| Missing | 1 |
Values in parentheses are
percentages and
mean(s.d.). n.a., Not applicable; MRCS, Membership of the Royal College of Surgeons.
ANOVA, except
t test.
Approximately three‐quarters of national selection candidates had passed Part A (598 of 774, 77·3 per cent) and Part B (581 of 774, 75·1 per cent) of the MRCS examination at the first attempt. There were significant, weak correlations between Part A first and passing attempt scores and the national selection first attempt score (r = 0·19 and 0·20 respectively; P < 0·001). The correlations between Part B first and passing attempt scores and the national selection score were stronger (r = 0·38 and 0·30 respectively; P < 0·001) (Table 2).
Table 2.
Correlations between Membership of the Royal College of Surgeons examination scores and national selection first attempt score for general and vascular surgery
| National selection first attempt (n = 774) | |
|---|---|
| Part A | |
| First attempt | 0·19 |
| Passing attempt | 0·20 |
| Part B | |
| First attempt | 0·38 |
| Passing attempt | 0·30 |
Values are Pearson correlation coefficients; all are significant at P < 0·001 level.
The relationship between demographic factors and the number of attempts at each part of the MRCS examination, and how they affected the national selection first attempt score, are presented in Table 1.
In univariable analysis, there were significant differences in national selection first attempt score between the variables: number of attempts at Part A MRCS (t = 4·64, 2 d.f., P = 0·010), number of attempts at Part B MRCS (t = 27·04, 2 d.f., P < 0·001), ethnicity (t = 6·22, 4 d.f., P < 0·001) and first language (t = 2·70, 609 d.f., P = 0·007). As these variables were all below the 10 per cent significance level in univariable analysis, they were included in the multivariable analysis to identify independent predictors of national selection score for general and vascular surgery (Table 3).
Table 3.
Multivariable linear regression analysis of predictors of national selection first attempt score for general and vascular surgery
| Unstandardized coefficients | |||
|---|---|---|---|
| B | s.e. | P | |
| Constant* | 69·67 | 0·97 | < 0·001 |
| How well candidates passed Part B MRCS (% above pass mark)† | 0·28 | 0·04 | < 0·001 |
| No. of Part B MRCS attempts | |||
| 1 | Reference | ||
| 2 | −2·93 | 0·79 | < 0·001 |
| ≥ 3 | −8·11 | 1·31 | < 0·001 |
| Ethnicity | |||
| White British | Reference | ||
| Asian | −1·77 | 0·75 | 0·019 |
| Black | −1·08 | 1·74 | 0·536 |
| Other | −1·30 | 1·02 | 0·201 |
Maximum predicted first attempt score, calculated using the reference variables (a white candidate who passed Part B Membership of the Royal College of Surgeons (MRCS) at the first attempt is expected to score 69·67 per cent at the national selection interview for general and vascular surgery).
A candidate who just achieved the pass mark would have a value of zero. Model: R 2 = 0·18, n = 598.
The Part B MRCS passing attempt score and the number of attempts required to pass Part B were significant predictors of the general and vascular surgery national selection first attempt score (change in R 2 value of 0·10 and 0·07 respectively; P < 0·001). The model also predicted that candidates who required three or more attempts at Part B of the examination would obtain a national selection score 8·1 per cent lower than equally matched candidates who passed Part B at their first attempt. Ethnicity had much less influence on national selection score than number of attempts (change in R 2 = 0·01, P = 0·038), although Asian candidates were predicted to perform slightly worse than white candidates (national selection first attempt score for general and vascular surgery: 67·9 versus 69·7 per cent respectively; P = 0·019).
Discussion
Several groups have assessed the predictive validity of other high‐stakes medical examinations, including the United States Medical Licensing Examination® (USMLE®)8, 9, 10, the Quebec Licensing Examination11, the Medical Council of Canada Qualifying Examination12, 13, 14, the MRCP examination15, 16, 17 and Membership of the Royal College of General Practitioners examination15. Performance in these examinations predicts performance in clinical practice and other medical assessment processes11 18, 19. For example, each part of the MRCP examination predicts the next17, and candidates who score higher in all parts of the MRCP examination do better in workplace‐based assessments than those who underperform16. Similarly, USMLE® scores predict performance in the American Board of Surgery In‐Training Examination among general surgery residents20, and higher USMLE® scores have been associated with higher pass rates in the general surgery board examination10. This may explain why surgical programme directors in the USA regard USMLE® performance as the most important factor for preliminary screening of general surgery residents21.
In keeping with these observations, the present study has identified that performance in Part B of the MRCS examination predicts 17 per cent of the variance in national selection first attempt score for general and vascular surgery. In addition, candidates who required more than two attempts at Part B were predicted to score substantially less at the national selection interview than those who passed at their first attempt. This difference in score would have been below previous years' minimum appointable scores, suggesting that candidates who require more than two attempts at Part B are unlikely to be offered a national training number in general or vascular surgery.
Although many candidates take several attempts to pass high‐stakes medical examinations5 17, most studies have focused on the relationship between examination scores and future performance without distinguishing between candidates on the basis of number of attempts needed to pass, despite evidence of a relationship between number of attempts and performance indicators15 18, 22. For example, McDougle and colleagues23 compared graduates who initially failed Step 1 of the USMLE® with those who passed it first time, finding that the relative risk of not being specialty board certified was 2·2. Multiple attempts at the Medical College Admission Test (MCAT) have also been associated with an increased risk of failing Step 2 of the USMLE®24, whereas multiple attempts at the Professional and Linguistic Assessments Board (PLAB) test have been shown to be independently predictive of unsatisfactory training performance25. The relationship between the number of attempts required to pass a postgraduate UK medical examination and performance in other medical assessments is unknown, but one study17 found that as the number of attempts at each part of the MRCP examination increased, final passing score decreased. The present results add to the evidence that candidates who require more attempts to pass high‐stakes postgraduate medical examinations are of poorer calibre than those who require fewer attempts.
Although ethnicity was an independent predictor of the national selection score in multivariable analysis in the present study, it accounted for only 1 per cent of the variance in score, and nearly one‐quarter of ethnicity data were missing from the cohort. Reassuringly, the other non‐modifiable variables (sex, age and first language) had no effect on national selection performance and together with the ethnicity data provides further evidence that the national selection process for general and vascular surgery in the UK is both fair and unbiased.
Examination performance is not currently used as part of the selection criteria for entering specialty training in the UK. In a recent survey26 of US residency programme directors spanning all specialties, 93 per cent cited the USMLE® Step 1 score as the most important factor in selection. USMLE® scores have been shown to be related to MCAT performance, with one study27 finding that 17·7 per cent of the variance in Step 1 of the USMLE® score was explained by MCAT performance. Given that 17 per cent of the variance in the national selection first attempt score in the present study is explained by Part B of the MRCS examination, there may be an argument for using the (currently mandatory) Part B examination as part of the selection criteria for entry into general and vascular specialty training in the UK. Given the small effect sizes and the moderate positive correlation found, it would seem sensible for other candidate factors to be considered in conjunction with Part B performance. It is also important to acknowledge that the association between MRCS performance and national selection score could be due to an inherent problem with the MRCS examination and the assessment process for national selection. The demographic of examiners, for example, is likely to be broadly similar; thus, the same unconscious bias that may occur at Part B of the MRCS examination may also apply at national selection.
This study also has implications for policy and practice. In keeping with other studies22, 23, 24, 25, these results suggest that candidates who require multiple attempts at a postgraduate medical examination are more likely to struggle with other medical assessment processes (in this case, assessment via a selection process). This information may identify doctors who will require additional support through their training and guide national bodies when considering borderline candidates or appeals. The study has implications for the number of times UK candidates should be encouraged to attempt the MRCS examination. If those requiring more than two attempts at Part B are unlikely to be offered a national training number in general or vascular surgery, this is important information for those setting out on their postgraduate medical career.
The strengths of this study are the size of the study population and that the data are from multiple cohorts and various versions of the MRCS examination. Although the examination is undertaken by more international than UK candidates, the present study focused on UK medical graduates for three reasons: UK candidates are the most homogeneous group that take the MRCS examination; the examination has been designed to assess trainees who have been through the UK training system and who are likely to continue their surgical training in the UK; and there was an available outcome measure for this group as the UK national selection process for entry into general and vascular specialty training has been shown to be reliable and fair28. Future research might usefully look at the whole population of those who sit the MRCS examination to compare MRCS performance across different groups. Other surgical specialty selection committees could carry out similar studies, to examine whether the MRCS examination can predict how candidates will perform in the respective national selection interviews. The study was limited by missing data for self‐declared first language (163 of 774, 21·1 per cent) and ethnicity (176 of 774, 22·7 per cent), which reduced the total number of candidates included in the multivariable analysis. Although the rate of missing data is similar to that (15–20 per cent) seen in other educational studies29, future research should aim to gather a more complete data set.
This study has examined only the relationship between MRCS examination performance and national selection performance for general and vascular surgery. To assess the predictive validity of the MRCS examination further it will be necessary to analyse the relationship between MRCS and other surgical training outcomes. Further research should therefore focus on the relationship between MRCS examination results and performances in clinical practice and the postgraduate exit examination that awards the diploma of Fellowship of the Royal College of Surgeons (FRCS).
Acknowledgements
The authors acknowledge I. Targett from the Royal College of Surgeons of England for his help with data collection, and both L. Smith and G. Ayre from the Intercollegiate Committee for Basic Surgical Examinations for their support during this project. This study was funded by the Royal Colleges of Surgeons of England, Ireland and Edinburgh, and the Royal College of Physicians and Surgeons of Glasgow.
Disclosure: The authors declare no conflict of interest.
Funding information
Royal College of Surgeons of England
Royal College of Surgeons of Ireland
Royal College of Surgeons of Edinburgh
Royal College of Physicians and Surgeons of Glasgow
Presented at the Association of Surgeons of Great Britain and Ireland 2017 International Surgical Congress, Glasgow, UK, May 2017 and the Scottish Medical Education Conference, Edinburgh, May 2017
References
- 1. Brennan PA, Scrimgeour DS, Patel S, Patel R, Grif G, Croke DT et al Changing Objective Structured Clinical Examinations stations at lunchtime during all day postgraduate surgery examinations improves examiner morale and stress. J Surg Educ 2017; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 2. Brennan PA, Sherman KP. The MRCS examination – an update on the latest facts and figures. Br J Oral Maxillofac Surg 2014; 52: 881–883. [DOI] [PubMed] [Google Scholar]
- 3. Rahbour G, Hogben K. How to Succeed in ST3 General Surgery National Recruitment; 2014. http://careers.bmj.com/careers/advice/view-article.html?id=20016482 [accessed 4 January 2017]. [Google Scholar]
- 4. Brennan PA, Smith L, Sherman KP. ICBSE: who are we and where are we going? Bull R Coll Surg Engl 2014; 96: 288–289. [Google Scholar]
- 5. Brennan PA, Smith L. Intercollegiate Committee for Basic Surgical Examinations. 2015/16 Annual Report; 2016. http://www.intercollegiatemrcs.org.uk/new/pdf/Annual-Report_2015-16.pdf [accessed 2 January 2017].
- 6. Pyne Y, Ben‐Shlomo Y. Older doctors and progression through specialty training in the UK: a cohort analysis of General Medical Council data. BMJ Open 2015; 5: 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hemphill JF. Interpreting the magnitudes of correlation coefficients. Am Psychol 2003; 58: 78–79. [DOI] [PubMed] [Google Scholar]
- 8. McCaskill QE, Kirk JJ, Barata DM, Wludyka PS, Zenni EA, Chiu TT. USMLE Step 1 scores as a significant predictor of future board passage in pediatrics. Ambul Pediatr 2007; 7: 192–195. [DOI] [PubMed] [Google Scholar]
- 9. Hojat M, Paskin DL, Callahan CA, Nasca TJ, Louis DZ, Veloski J et al Postgraduate training components of postgraduate competence: analyses of thirty years of longitudinal data. Med Educ 2007; 41: 982–989. [DOI] [PubMed] [Google Scholar]
- 10. Sutton E, Richardson JD, Ziegler C, Bond J, Burke‐Poole M, McMasters KM et al Is USMLE Step 1 score a valid predictor of success in surgical residency? Am J Surg 2014; 208: 1029–1034. [DOI] [PubMed] [Google Scholar]
- 11. Tamblyn R, Abrahamowicz M, Brailovsky C, Maison PG, Lescop J, Norcini J et al Association between licensing examination scores and resource use and quality of care in primary care practice. JAMA 1998; 280: 989–996. [DOI] [PubMed] [Google Scholar]
- 12. Brailovsky C, Rainsberry P, Allen T, Slade S. Predicting Family Medicine Specialty Certification Status Using Standardized Measures for a Sample of International Medical Graduates Engaged in a Practice‐Ready Assessment Pathway to Provisional Licensure Medical Council of Canada, College of Family Physicians of Canada and Canadian Post‐MD Education Registry document. http://mcc.ca/wp-content/uploads/reports-predictive-validity-journal-article.pdf [accessed 1 February 2017].
- 13. Tamblyn R, Abrahamowicz M, Dauphinee D, Wenghofer E, Jacques A, Klass D et al Physician scores on a national clinical skills examination as predictors of complaints to medical regulatory authorities. JAMA 2007; 298: 993–1001. [DOI] [PubMed] [Google Scholar]
- 14. Wenghofer E, Klass D, Abrahamowicz M, Dauphinee D, Jacques A, Smee S et al Doctor scores on national qualifying examinations predict quality of care in future practice. Med Educ 2009; 43: 1166–1173. [DOI] [PubMed] [Google Scholar]
- 15. Wakeford R, Denney M, Ludka‐Stempien K, Dacre J, McManus IC. Cross‐comparison of MRCGP & MRCP(UK) in a database linkage study of 2284 candidates taking both examinations: assessment of validity and differential performance by ethnicity. BMC Med Educ 2015; 15: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Levy JB, Mohanaruban A, Smith D. The relationship between performance in work place based assessments, MRCP exam and outcome from core medical training. Med Educ 2011; 45(Suppl 2): 5. [Google Scholar]
- 17. McManus I, Ludka K. Resitting a high‐stakes postgraduate medical examination on multiple occasions: nonlinear multilevel modelling of performance in the MRCP(UK) examinations. BMC Med 2012; 10: 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tamblyn R, Abrahamowicz M, Dauphinee WD, Hanley JA, Norcini J, Girard N et al Association between licensure examination scores and practice in primary care. JAMA 2002; 288: 3019–3026. [DOI] [PubMed] [Google Scholar]
- 19. Norcini JJ, Boulet JR, Opalek A, Dauphinee WD. The relationship between licensing examination performance and the outcomes of care by international medical school graduates. Acad Med 2014; 89: 1157–1162. [DOI] [PubMed] [Google Scholar]
- 20. Spurlock DR, Holden C, Hartranft T. Using United States Medical Licensing Examination (USMLE) examination results to predict later in‐training examination performance among general surgery residents. J Surg Educ 2010; 67: 452–456. [DOI] [PubMed] [Google Scholar]
- 21. Makdisi G, Takeuchi T, Rodriguez J, Rucinski J, Wise L. How we select our residents – a survey of selection criteria in general surgery residents. J Surg Educ 2011; 68: 67–72. [DOI] [PubMed] [Google Scholar]
- 22. Dewhurst NG, McManus C, Mollon J, Dacre JE, Vale AJ. Performance in the MRCP(UK) examination 2003–4: analysis of pass rates of UK graduates in relation to self‐declared ethnicity and gender. BMC Med 2007; 5: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McDougle L, Mavis BE, Jeffe DB, Roberts NK, Thomas L, Andriole DA. Academic and professional career outcomes of medical school graduates who failed USMLE Step 1 on the first attempt. Adv Health Sci Educ Theory Pract 2013; 18: 279–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ogunyemi D, Taylor‐Harris DS. Factors that correlate with the US medical licensure examination Step‐2 scores in a diverse medical student population. J Natl Med Assoc 2005; 97: 1258–1262. [PMC free article] [PubMed] [Google Scholar]
- 25. Tiffin PA, Illing J, Kasim AS, McLachlan JC. Annual Review of Competence Progression (ARCP) performance of doctors who passed Professional and Linguistic Assessments Board (PLAB) tests compared with UK medical graduates: national data linkage study. BMJ 2014; 348: g2622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. National Resident Matching Program (NRMP), Data Release and Research Committee . Results of the 2016 NRMP Program Director Survey http://www.nrmp.org/wp-content/uploads/2016/09/NRMP-2016-Program-Director-Survey.pdf [accessed 6 May 2017].
- 27. Gauer JL, Wolff JM, Jackson JB. Do MCAT scores predict USMLE scores? An analysis on 5 years of medical student data. Med Educ Online 2016; 21: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lamont P, Griffiths G, Cochrane L. National selection into general surgery: a pilot study. Ann R Coll Surg Engl 2011; 93: 1–10. [Google Scholar]
- 29. Enders CK. Using the expectation maximization algorithm to estimate coefficient alpha for scales with item‐level missing data. Psychol Methods 2003; 8: 322–337. [DOI] [PubMed] [Google Scholar]


