Abstract
An 88-year-old woman presented to our emergency room with complaints of fever, coryza, barking cough and generalised fatigue for 2 days. Physical examination showed stridor, tachypnoea with use of accessory muscles of respiration on admission. Laboratory tests were unremarkable except for monocytosis with a normal total white cell count. Rapid influenza diagnostic test was positive for influenza A. Chest X-ray showed subglottic narrowing of the trachea suggestive of steeple sign. A diagnosis of influenza A-induced croup was made. She was given humidified oxygen, nebulised racemic epinephrine, intravenous dexamethasone and oseltamivir. Stridor resolved within minutes of giving nebulised epinephrine. Work of breathing improved within 4–6 hours. She was discharged 2 days later on a tapering dose of steroids.
Keywords: influenza, radiology
Background
Croup is rarely seen in the adult population, ours being the 17th reported case based on a thorough review of literature. Furthermore, this is the first case of influenza A presenting as croup in an adult. This paper emphasises the importance of early detection and intervention in order to prevent escalation of care. We also aim to differentiate the management of croup in an adult to that of the paediatric population.
Case presentation
An 88-year-old woman presented to our emergency room with complaints of fever, coryza, barking cough and generalised fatigue for 2 days. Medical history was significant for diabetes mellitus, hypertension and hyperlipidaemia. Her vital signs were unremarkable except for 101.2°F temperature and respiratory rate of 26. Her oxygen saturation was 98% on room air with no evidence of cyanosis. She was in moderate respiratory distress with supraclavicular and substernal retractions. She had an audible inspiratory stridor. Other than the inspiratory stridor, there were no crackles or adventitious sounds in the lung examination. Laboratory tests were unremarkable except for monocytosis of 1.2×103/mm3 with a total white cell count of 9×103/mm3. Nasopharyngeal swab was sent for rapid influenza detection test which came out positive for influenza A. Chest X-ray showed subglottic narrowing of the trachea suggestive of the ‘steeple sign’ (figure 1). A diagnosis of laryngotracheitis, also known as croup, was then made.
Figure 1.
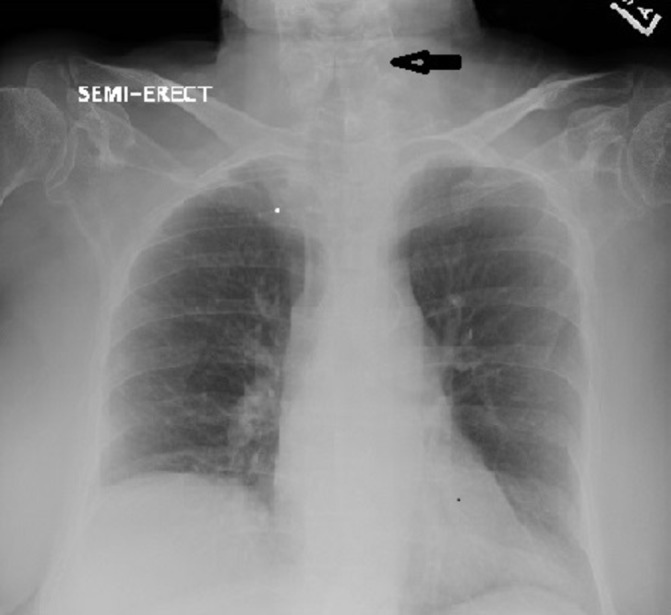
Portable anterior-posterior view chest X-ray showing subglottic narrowing suggestive of ‘steeple sign’ with clear lung fields.
Treatment
She was given humidified oxygen and nebulised racemic epinephrine along with 10 mg intravenous dexamethasone once. Oseltamivir (75 mg two times per day) for a course of 5 days was started for influenza A treatment. Stridor resolved within minutes of giving racemic epinephrine. Her work of breathing improved visibly over the course of 4 to 6 hours. Initial decision to transfer to medical intensive care unit for airway management was deferred as patient responded to the treatment quickly. She did not require any further doses of nebulised racemic epinephrine and only a tapering dose of oral prednisone was initiated.
Outcome and follow-up
Chest X-ray repeated a day later showed resolution of the subglottic narrowing (figure 2). She was discharged 2 days later with complete resolution of symptoms. On a follow-up phone call a week later, she mentioned she did not have any further episodes of barking cough and all her symptoms had resolved.
Figure 2.
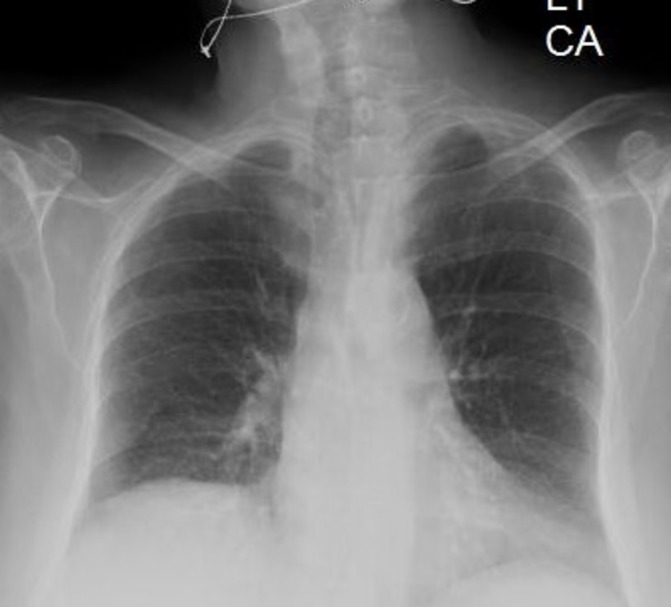
Posterior-anterior view chest X-ray repeated 1 day later showing resolution of subglottic narrowing.
Discussion
Croup (laryngotracheobronchitis) is a respiratory disease seen most commonly in childhood. It is characterised by fever, barking cough and inspiratory stridor. The hallmark of the disease is the presence of subglottic tracheal narrowing usually detected by a chest X-ray. The most common aetiological agents are parainfluenza virus and rhinovirus.1 However, influenza A and B virus have been reported as a cause of croup in the paediatric population especially during influenza epidemics. Furthermore, in a study by Peltola et al, it was found that croup in children caused by influenza virus was associated with more severe symptoms, longer hospital stay and higher readmission rates when compared with croup caused by parainfluenza virus.2
Adult croup is exceedingly rare; only 16 cases have been previously reported in English literature. In 1990, Deeb and Einhorn reported the first seven cases of croup in adults.3 They mentioned that most of the patients recovered within 48 to 72 hours likely indicative of a viral aetiology. This is the largest case series published. In 1996, Tong et al reported three cases of adult croup, one of which had a rise in antibody titre against influenza B.4 Fibreoptic laryngoscopy was performed in all of these patients to confirm diagnosis. In our experience, when symptoms and signs are highly suggestive of croup, laryngoscopy can be avoided if treatment with nebulised epinephrine and steroids is started without any delay. This is similar to paediatric cases of croup, wherein the diagnosis is mostly clinical and laryngoscopy is often reserved for cases of recurrent croup.5
Woo et al reported a case of a 71-year-old woman who presented with croup and tested positive for parainfluenza virus type 3.6 They compared 11 cases of adult croup published in the English literature with 43 children hospitalised with severe croup described in a paper by Postma et al, and concluded that adult croup is a more severe disease entity as compared with paediatric croup. They recommended that all adults with croup should be looked after in an intensive care unit. Though our patient presented with moderate respiratory distress, she did not have oxygen desaturation and immediate management with a dose of nebulised racemic epinephrine and a dose of intravenous dexamethasone were able to stabilise and improve the patient’s condition. Hence, escalation to intensive care was avoided and patient was monitored on regular medical floor with continuous pulse oximetry.
In the present era, rapid detection of viral antigens via a nasopharyngeal swab is possible with the help of antigen testing using PCR techniques or monoclonal antibodies.7 We were able to detect influenza A using a rapid influenza diagnostic test and start treatment with oseltamivir immediately. While respiratory syncytial virus, parainfluenza type 3 and influenza B have been reported to cause croup in adults, this is the first case report of influenza A causing croup.4 5 8 With the advent of rapid detection of viral antigens, it is becoming evident that adult croup, similar to childhood croup, is often caused by a viral pathogen. In rare instances, a bacterial pathogen has been recognised as a causative agent of croup. One of the seven cases reported by Deeb et al, grew Hemophilus influenza, it was postulated to be a bacterial superinfection with underlying viral inflammation. Parimon et al reported a severe case of adult croup wherein the throat swab was negative for group A streptococci, influenza A and B; however, blood cultures grew Streptococcus pneumoniae and the patient responded well to antibiotics.9 Pathological evaluation of autopsy specimens of 100 patients in the USA with confirmed 2009 H1N1 virus infection showed inflammation and oedema in the trachea and/or bronchi in 66% patients. This data suggest that perhaps influenza A is an underdiagnosed cause of laryngotracheitis in adults.10
Influenza can present with nasopharyngeal symptoms, tracheal and bronchial symptoms or even viral pneumonia. This varied manifestation can be explained by the distribution gradients of certain receptors for the virus such as sialic acid on the respiratory mucosal membrane. Presence of 2–6 sialic acids on the trachea can probably lead to a croup-like presentation.11
Irrespective of the aetiology, the aim of treatment in croup is to decrease the subglottic swelling. The mainstay of treatment for childhood croup is steroids. Dexamethasone is preferred, as a single dose.12 Additionally, nebulised racemic epinephrine can be used. It acts by mucosal vasoconstriction and reduction of oedema, thus relieving obstruction. Studies in the paediatric population have shown that it reduces severity of symptoms, need for admission, need for intubation and length of stay. Its duration of action is short-lived ranging from 1 to 2 hours; thus, it is given in addition to long-acting steroids.13 We treated our patient with both steroids and racemic epinephrine and were able to avoid intubation. As compared with children, adults have a wider and less compliant trachea. Therefore, appearance of the steeple sign on X-ray signifies a more severe airway obstruction and we recommend the use of both intravenous dexamethasone and nebulised epinephrine in adults without delay. This is unlike the management in children where nebulised epinephrine is given only in moderate to severe cases. In the absence of improvement in symptoms within 2 hours of administration of nebulised epinephrine and intravenous dexamethasone, a bacterial superinfection should be suspected. Complications of viral croup include bacterial superinfection, toxic shock syndrome, respiratory failure requiring intubation and even death.9 Diagnostic delay can lead to tracheal stenosis in the long run.11
Adult croup is a rare presentation of upper respiratory tract infection. Prompt diagnosis and intervention can lead to early recovery with minimum morbidity.
Learning points.
Croup is a clinical diagnosis and usually presents with fever, barking cough and stridor.
Although croup is a disease of childhood, it can be seen in adults.
It is treated with intravenous steroids and nebulised racemic epinephrine.
Prompt diagnosis and intervention can lead to early recovery.
Footnotes
Contributors: NS and PD were on call and admitted the patient. They provided management. AB was the resident taking care of the patient while she was admitted for 2 days. SS was the attending physician taking care of the patient. The manuscript was written by NS and AB and edited by PD and SS.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Petrocheilou A, Tanou K, Kalampouka E, et al. Viral croup: Diagnosis and a treatment algorithm. Pediatr Pulmonol 2014;49:421–9. 10.1002/ppul.22993 [DOI] [PubMed] [Google Scholar]
- 2.Peltola V, Heikkinen T, Ruuskanen O. Clinical courses of croup caused by influenza and parainfluenza viruses. Pediatr Infect Dis J 2002;21:76–8. 10.1097/00006454-200201000-00020 [DOI] [PubMed] [Google Scholar]
- 3.Deeb ZE, Einhorn KH. Infectious adult croup. Laryngoscope 1990;100:457–7. 10.1288/00005537-199005000-00002 [DOI] [PubMed] [Google Scholar]
- 4.Tong MC, Chu MC, Leighton SE, et al. Adult croup. Chest 1996;109:1659–62. 10.1378/chest.109.6.1659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kwong K, Hoa M, Coticchia JM. Recurrent croup presentation, diagnosis, and management. Am J Otolaryngol 2007;28:401–7. 10.1016/j.amjoto.2006.11.013 [DOI] [PubMed] [Google Scholar]
- 6.Woo PC, Young K, Tsang KW, et al. Adult croup: a rare but more severe condition. Respiration 2000;67:684–8. 10.1159/000056301 [DOI] [PubMed] [Google Scholar]
- 7.Vemula SV, Zhao J, Liu J, et al. Current approaches for diagnosis of influenza virus infections in humans. Viruses 2016;8:96 10.3390/v8040096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel JJ, Kitchin E, Pfeifer K. A narrowing diagnosis: a rare cause of adult croup and literature review. Case Rep Crit Care 2017;2017:1–3. 10.1155/2017/9870762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parimon T, Charan NB, Anderson DK, et al. A catastrophic presentation of adult croup. Am J Respir Crit Care Med 2013;187:e23–e24. 10.1164/rccm.201207-1306IM [DOI] [PubMed] [Google Scholar]
- 10.Shieh WJ, Blau DM, Denison AM, et al. 2009 pandemic influenza A (H1N1): pathology and pathogenesis of 100 fatal cases in the United States. Am J Pathol 2010;177:166–75. 10.2353/ajpath.2010.100115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blot M, Bonniaud-Blot P, Favrolt N, et al. Update on childhood and adult infectious tracheitis. Med Mal Infect 2017;47:443–52. 10.1016/j.medmal.2017.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bjornson CL, Johnson DW. Croup in children. Can Med Assoc J 2013;185:1317–23. 10.1503/cmaj.121645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown JC. The management of croup. Br Med Bull 2002;61:189–202. 10.1093/bmb/61.1.189 [DOI] [PubMed] [Google Scholar]


