Abstract
Duplication of the inferior vena cava (DIVC) is an uncommon embryological anatomic phenomenon.
We report a 63-year-old woman with extensive right leg deep vein thrombosis who required an IVC filter due to contraindications for anticoagulation, but was found to have DIVC which required the placement of two IVC filters with good result. This report will review and summarise past reports of DIVC management to provide a guide for future clinicians, and review the embryological development, diagnosis and IVC filter placement options as they are based on the type of anatomic malformation encountered.
Keywords: interventional radiology, vascular surgery
Background
DIVC is an uncommon phenomenon with an incidence of 0.2%–3%1 2 and only 14 prior cases were identified in the literature for DIVC and caval interruption. Future clinicians and patients can benefit from publishing the management decisions that were made in real time, combined with a summary of the literature.
Case presentation
A 63-year-old woman presented to the emergency department from an assisted living facility with shortness of breath, subjective fevers and cough productive of white sputum. Her medical history included chronic obstructive pulmonary disease (COPD) and tracheostomy placed 4 years prior to admission related to ventilator-dependent respiratory failure from severe COPD exacerbation, chronic kidney disease stage IV, type 2 diabetes mellitus, hypertension and obstructive sleep apnoea. Her examination was notable for respiratory rate (RR) of 24/min, oral temperature 99.2F (37.3C), pulse 90/min, blood pressure 138/68 mm Hg and room air pulse oximetry (O2Sat) 94%. Lung examination revealed bilateral expiratory wheezing, and her extremities were without oedema or tenderness. Laboratory evaluation revealed normal electrolytes, creatinine 2.2 mg/dL (194 μ mol/L) (baseline 2.2–2.4 mg/dL (194–212 μmol/L]), white blood count 16 400/μL (4000–12 000/μL) and right lower lobe infiltrate on chest radiograph. She was admitted with a diagnosis of COPD exacerbation, diagnosed with healthcare-associated pneumonia, and treated with nebulised albuterol, intravenous corticosteroids and intravenous levofloxacin. On hospital day 3, her room air O2Sat dropped to 80%, she was tachypnoeic with RR 32/min and repeat chest X-ray was unchanged. Bronchoscopy done on the same day found a mucus plug with small amount of blood which was thought to be due to traumatic suctioning. On hospital day 5, her O2Sat dropped and urgent bronchoscopy again found mucus plugging. Her O2Sat improved significantly when the plug was cleared. Both times the drop in oxygen levels improved after the clearance of the mucus plugs, supporting the clinical diagnosis of pneumonia, so the clinical team did not suspect an alternate diagnosis, such as pulmonary embolism, at that point. On hospital day 7, she complained of right calf tenderness and diagnostic studies were obtained.
Investigations
Hospital day 1: chest radiograph: right lower lobe infiltrate.
Hospital day 7: venous Doppler/ultrasound on day 7 revealed extensive deep vein thrombosis (DVT) involving right femoral, posterior tibial and peroneal veins with the patent popliteal vein.
Treatment
On hospital day 7, the acute DVT was treated with a high-intensity unfractionated heparin drip, but 12 hours later she developed copious bloody secretions on suctioning of the tracheostomy. The amount of blood was extensive, therefore anticoagulation was stopped and interventional radiology was consulted for placement of an IVC filter. Day 9, a mapping venogram was performed and she was noted to have DIVC with continuation of left IVC into the azygos and hemiazygos system (figures 1 and 2). On day 10, she underwent placement of two infrarenal IVC filters, one in each IVC (figure 3).
Figure 1.
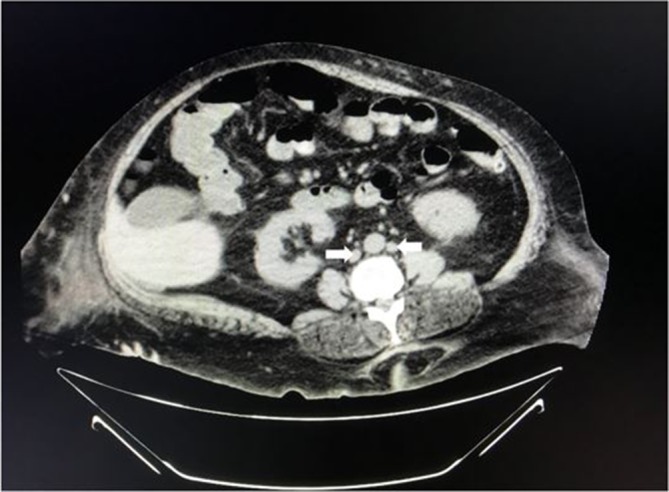
CT scan of the abdomen/pelvis showing duplicated IVC (white arrows). IVC, inferior vena cava.
Figure 2.
Venogram depicting patient’s duplicated IVC anatomy. Image on the left shows right external iliac vein extending into the right caval system (arrow). Image on right shows patient’s left external iliac vein (arrow) and extending into left caval system (arrow). Inter-iliac communicating vein extending (star). IVC, inferior vena cava.
Figure 3.
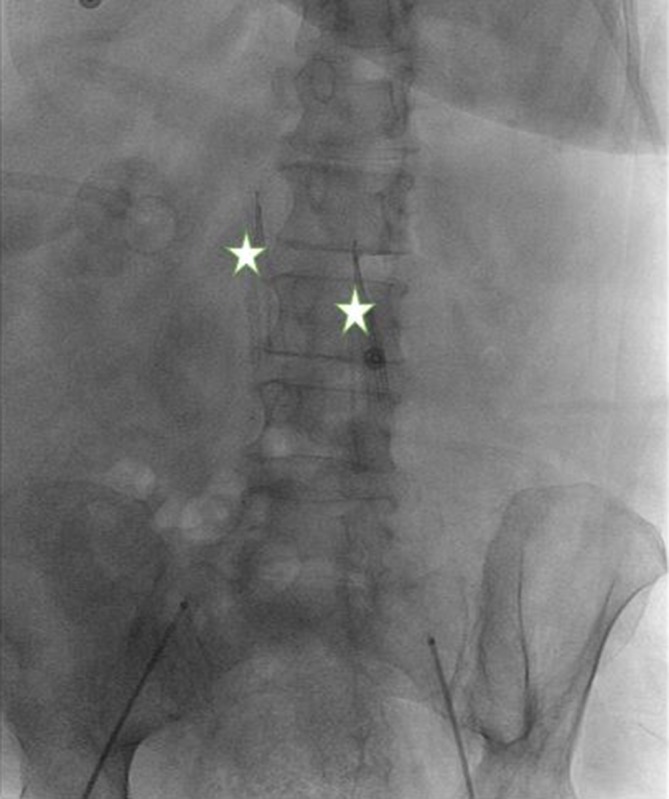
Placement of dual IVC filters (stars). IVC, inferior vena cava.
Outcome and follow-up
On hospital day 12, her respiratory status was stable on 28% oxygen by tracheostomy collar and she was transferred back to her assisted living facility. In the setting of a provoked DVT, guidelines recommend 3 months of anticoagulant treatment, and in patients who had an IVC filter placed, to consider a full 3 months when the contraindication to anticoagulation has been resolved. This decision was deferred to her outpatient physician, and they were advised to have her evaluated her for IVC filter removal in 3 months.
Discussion
The embryological formation of the IVC involves the anastomosing of pairs of primitive veins. The IVC consists of four segments: the suprarenal, hepatic, renal and infrarenal. The primitive veins that form the final IVC are the posterior cardinal, subcardinal and supracardinal. Posterior cardinal veins form the distal IVC and common iliac veins, right subcardinal veins form the suprarenal portion, the renal segment of the IVC develops from the right suprasubcardinal and postsubcardinal anastomoses and the right supracardinal vein forms infrarenal IVC.2–6 The alteration of any of these steps can result in IVC anatomic abnormalities. DIVC results from persistence of the left supracardinal vein and can have multiple anatomic variations such as left IVC, retrocaval IVC, IVC with drainage through the azygos vein and IVC interruption with continuation through the azygos vein.7–10 DIVC is clinically silent and therefore diagnosis is often incidental.
If suspected or detected, multidetector CT is less costly and less invasive than a conventional angiography, fast, easily applicable and reliable in terms of identification of thoracoabdominal vascular structures. Two-dimensional and three-dimensional images can aid in the visualisation and understanding of complex vascular malformations of the IVC.11
A PubMed search with terms ‘Duplicated Inferior Vena Cava’ and ‘Inferior Vena Cava filter’ returned 14 cases utilising three options for caval interruption: (1) placement of bilateral IVC filters (10 cases); (2) filter insertion in large right IVC and steel coil embolisation of the smaller IVC (2 cases); (3) filter insertion in large right IVC and catheter-directed thrombolysis12–24 (see table 1).
Table 1.
Summary of past cases reporting management of dual IVC variants in patients with acute DVT and/or PE
| Reference | Year | Presentation | Method of caval interruption | Anatomy |
| 12 | 2013 | DVT | Dual IVC filter placement | L IVC originated from normal iliac confluence and drains into the left renal vein |
| 13 | 2011 | DVT and PE | Dual IVC filter placement | L IVC originated from the L common iliac vein with the interiliac vein communicating with R IVC |
| 13 | 2011 | DVT and PE | Dual IVC filter placement | L IVC originated from the L common iliac vein with the interiliac vein communicating with R IVC |
| 14 | 2012 | DVT | Dual IVC filter placement | L IVC originated from the L common iliac vein with no communication with R IVC, draining into the L renal vein |
| 15 | 2010 | DVT | Dual IVC filter placement | L IVC and L renal vein joined R IVC below the superior mesenteric vein |
| 16 | 2009 | DVT and PE | Dual IVC filter placement | L IVC originated from the L common iliac vein with no communication with R IVC, draining into the L renal vein |
| 17 | 2006 | DVT | Dual IVC filter placement | L IVC originated from the L common iliac vein with the interiliac vein communicating with R IVC |
| 18 | 2005 | DVT | R IVC filter and L IVC coil embolisation | L IVC and L renal vein join R IVC below the superior mesenteric vein |
| 19 | 2001 | DVT and PE | Dual IVC filter placement | L IVC originated from the R common iliac vein and receives the L common iliac vein. No interiliac vein communication with R IVC. L IVC drains in the L renal vein and two IVCs join |
| 20 | 1992 | DVT | Dual IVC filter placement | L IVC originated from the L common iliac vein and continued as the hemiazygos vein. R IVC originating from the R common iliac vein and continued as the azygos vein. No interiliac communication |
| 21 | 1992 | DVT | R IVC filter and L IVC steel coil embolisation | L IVC and L renal vein joined R IVC below the superior mesenteric vein |
| 22 | 1988 | DVT | Dual IVC filter placement | L IVC and L renal vein joined R IVC below the superior mesenteric vein |
| 23 | 2014 | DVT and PE | R IVC filter placement and catheter-directed thrombolysis | L IVC and L renal vein joined R IVC below the superior mesenteric vein |
| 24 | 2011 | Caval interruption for prophylaxis post-trauma | Dual IVC filter placement | Not mentioned |
DVT, deep venous thrombosis; L, left; LIVC, left inferior vena cava; PE, pulmonary embolism; R, right; RIVC, right inferior vena cava.
In addition to the three treatment options listed, the other potential intervention for DIVC include placement of a single suprarenal IVC filter post the confluence of DIVC. However, none of the cases reported used that intervention.
In our case, the indication for the IVC filter over anticoagulation was tracheal bleeding secondary to traumatic suction. IVC filters are typically deployed below the renal veins using the femoral or jugular approach, both of which can also be used to retrieve a recoverable filter. Venography is performed prior to filter placement to determine the approach, and in this case detected the anomaly allowing the clinical team to develop the proper plan for our patient (1). As our patient had a continuation of the left IVC into the azygos and hemiazygos system, two infrarenal IVC filters were placed, one each IVC. The reasons were the size of the IVCs and the interventional radiologist determined that technically this would offer the highest chance of successful filter deployment while avoiding the longer procedure time, fluoroscopy time and complications associated with coil embolisation. Our management was similar to 11/14 previously reported cases that deployed two IVC filters (table 1), therefore, this summary offers information for future clinicians regarding management of this uncommon finding.
Learning points.
Duplication inferior vena cava (DIVC) is due to an uncommon embryologic anatomic phenomenon that can have various clinical implications.
DIVC is often diagnosed incidentally during venogram prior to IVC filter placement, but when suspected multidetector CT can be useful.
Footnotes
Contributors: SP: contributed in collecting radiology images, getting consent and final review of the article along with writing of the article. AC: contributed in writing the article and collecting references for the discussion of the article. TK: contributed in writing and editing this article. MC: contributed in editing the article and selection of appropriate radiology images.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Masood J, Barua JM. Images in clinical medicine. Duplication of the inferior vena cava. N Engl J Med 2007;356:e17 10.1056/NEJMicm061036 [DOI] [PubMed] [Google Scholar]
- 2. Bass JE, Redwine MD, Kramer LA, et al. . Spectrum of congenital anomalies of the inferior vena cava: cross-sectional imaging findings. Radiographics 2000;20:639–52. 10.1148/radiographics.20.3.g00ma09639 [DOI] [PubMed] [Google Scholar]
- 3. Lucas MF. A case of double inferior vena cava. J Anat 1916;51(Pt 1):69–70. [PMC free article] [PubMed] [Google Scholar]
- 4. Banerjee A, Maharana S, Kumar IA, et al. . Duplication of the inferior vena cava-report of a rare congenital variation. Int J Anat Var 2012;5:141–3. [Google Scholar]
- 5. Natsis K, Apostolidis S, Noussios G, et al. . Duplication of the inferior vena cava: anatomy, embryology and classification proposal. Anat Sci Int 2010;85:56–60. 10.1007/s12565-009-0036-z [DOI] [PubMed] [Google Scholar]
- 6. Chen H, Emura S, Nagasaki S, et al. . Double inferior vena cava with interiliac vein: a case report and literature review. Okajimas Folia Anat Jpn 2012;88:147–51. 10.2535/ofaj.88.147 [DOI] [PubMed] [Google Scholar]
- 7. Babaian RJ, Johnson DE. Major venous anomalies complicating retroperitoneal surgery. South Med J 1979;72:1254–8. 10.1097/00007611-197910000-00012 [DOI] [PubMed] [Google Scholar]
- 8. Mathews R, Smith PA, Fishman EK, et al. . Anomalies of the inferior vena cava and renal veins: embryologic and surgical considerations. Urology 1999;53:873–80. 10.1016/S0090-4295(99)00007-2 [DOI] [PubMed] [Google Scholar]
- 9. Senecail B, Lefevre C, Person H, et al. . Radiologic anatomy of duplication of the inferior vena cava: a trap in abdominal imaging. A report of 8 cases. Surg Radiol Anat 1987;9:151–7. 10.1007/BF02086600 [DOI] [PubMed] [Google Scholar]
- 10. Xue HG, Yang CY, Asakawa M, et al. . Duplication of the inferior vena cava associated with other variations. Anat Sci Int 2007;82:121–5. 10.1111/j.1447-073X.2006.00153.x [DOI] [PubMed] [Google Scholar]
- 11. Coco D, Cecchini S, Leanza S, et al. . Inferior vena cava duplication: incidental case in a young woman. Case Rep Radiol 2016;2016:1–4. 10.1155/2016/3071873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pineda D, Moudgill N, Eisenberg J, et al. . An interesting anatomic variant of inferior vena cava duplication: case report and review of the literature. Vascular 2013;21:163–7. 10.1177/1708538113478731 [DOI] [PubMed] [Google Scholar]
- 13. Malgor RD, Oropallo A, Wood E, et al. . Filter placement for duplicated cava. Vasc Endovascular Surg 2011;45:269–73. 10.1177/1538574410395041 [DOI] [PubMed] [Google Scholar]
- 14. Leong S, Oisin F, Barry JE, et al. . Bilateral inferior vena cava filter insertion in a patient with duplication of the infrarenal vena cava. Ir J Med Sci 2012;181:389–91. 10.1007/s11845-010-0492-4 [DOI] [PubMed] [Google Scholar]
- 15. Cheng D, Zangan SM. Duplication of the inferior vena cava in a patient presenting for IVC filter placement. J Vasc Access 2010;11:162–4. 10.1177/112972981001100215 [DOI] [PubMed] [Google Scholar]
- 16. Moubarak G, Schleich JM, Daubert JC. Long-term efficacy of two vena cava filter implants for congenital duplicated inferior vena cava. Arch Cardiovasc Dis 2009;102:77–8. 10.1016/j.acvd.2008.06.009 [DOI] [PubMed] [Google Scholar]
- 17. Sartori MT, Zampieri P, Andres AL, et al. . Double vena cava filter insertion in congenital duplicated inferior vena cava: a case report and literature review. Haematologica 2006;91(6 Suppl):ECR30. [PubMed] [Google Scholar]
- 18. Anne N, Pallapothu R, Holmes R, et al. . Inferior vena cava duplication and deep venous thrombosis: case report and review of literature. Ann Vasc Surg 2005;19:740–3. 10.1007/s10016-005-5674-6 [DOI] [PubMed] [Google Scholar]
- 19. Spivack S, Kalker E, Samuels D, et al. . Filter placement in duplicated inferior vena cava. Isr Med Assoc J 2001;3:459–60. [PubMed] [Google Scholar]
- 20. Soltes GD, Fisher RG, Whigham CJ. Placement of dual bird’s nest filters in an unusual case of duplicated inferior vena cava. J Vasc Interv Radiol 1992;3:709–11. 10.1016/S1051-0443(92)72932-7 [DOI] [PubMed] [Google Scholar]
- 21. Smith DC, Kohne RE, Taylor FC. Steel coil embolization supplementing filter placement in a patient with a duplicated inferior vena cava. J Vasc Interv Radiol 1992;3:577–80. 10.1016/S1051-0443(92)72019-3 [DOI] [PubMed] [Google Scholar]
- 22. Rohrer MJ, Cutler BS. Placement of two Greenfield filters in a duplicated vena cava. Surgery 1988;104:572–4. [PubMed] [Google Scholar]
- 23. Wang X, Chen Z, Cai Q. Catheter-directed thrombolysis for double inferior vena cava with deep venous thrombosis: A case report and literature review. Phlebology 2014;29:480–3. 10.1177/0268355513490293 [DOI] [PubMed] [Google Scholar]
- 24. Rogers FB, Rogers A, Miller JA, et al. . Double vena cavas requiring filtration. J Trauma 2011;71:1922 10.1097/TA.0b013e318232a01d [DOI] [PubMed] [Google Scholar]



