Abstract
Automated dispensing cabinet (ADC) use within hospitals is designed to replace or partially replace medication cabinets or carts to allow for a more decentralized model of medication distribution. This project was designed to improve medication delivery by decreasing the burden of dispensing patient-specific medications from a centralized inpatient pharmacy while decreasing overall inventory cost. This single-center pilot analysis evaluated ADC inventory optimization in a mixed medical population. Data collected included inventory cost on ADC, medications removed from or added to ADC, patient-specific medications sent from central pharmacy, and the rate of medication stock outs on ADC.
Keywords: administration, cost, cost-containment, economics, drug distribution
Introduction
Automated dispensing cabinet (ADC) use within hospitals is designed to replace or partially replace medication cabinets or carts to allow for a more decentralized model of medication distribution. ADC use improves inventory management, streamlines patient billing, and increases caregiver and patient satisfaction.1 In one analysis, the implementation of automated dispensing machines increased the percentage of time spent on clinical activities from 36.1% to 49.1% among decentralized pharmacists.2 Further optimization of said cabinets specific to patient care areas could only further increase opportunities for pharmacists to provide additional pharmaceutical care while also reducing pharmacy technician workload.
This project was designed to improve medication delivery by decreasing the burden of dispensing patient-specific medications from a centralized inpatient pharmacy while decreasing overall inventory cost on unit-specific ADCs through a clinical pharmacist–driven ADC stewardship pilot program.
Methods
This single-center descriptive pilot analysis evaluated ADC inventory optimization in a medical population of 40 patient beds in 2 adjoining patient care areas. Each patient care area contained one ADC for the unit’s respective patients (an Omnicell Three-Cell cabinet). One unit had a total of 264 bins and the other had 246 bins for mediation storage. Both ADCs had additional storage in the attached refrigerator.
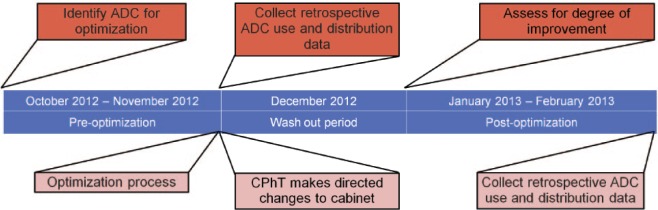
Two separate 2-month time periods between October 2012 and February 2013 were evaluated during this analysis, one prior to the inventory optimization and one after. A 2-week washout between the data collection periods was utilized to limit the possibility of the same patients being captured within both time periods (Figure 1). The endpoints evaluated in this analysis were the following: pre- and postoptimization inventory cost on the ADCs, the quantity of medications removed from or added to the ADC during the optimization intervention, the amount of patient-specific medications dispensed from central pharmacy, and the rate of medication stock outs on the ADCs during each data collection period.
Figure 1.
Automated dispensing cabinet stewardship timeline.
At our institution, pharmacists are encouraged to utilize all available items on the ADCs when approving patient medication orders. For those medications that are not available on the ADC located in a specific patient’s care area, the orders are labeled, filled, checked in our centralized pharmacy, and delivered to the patient care areas every hour on the half-hour by a pharmacy technician. The ADC inventory, excluding schedule II to IV medications, is restocked thrice daily based on previously established par levels, which vary based on each ADC and its respective patient care area. The restocking of an ADC and the delivery of patient-specific medications to that ADC are all handled by the same pharmacy technician. Our institution has 4 delivery technicians for the morning and evening shifts, each of which is responsible for 24 ADCs on average.
In this stewardship program, a clinical pharmacist directed and worked collectively with 2 certified pharmacy technicians to evaluate ADC inventory and centrally dispensed medications for patients on the specific medical units being evaluated. The necessary reports were obtained by the pharmacy technicians and then evaluated and edited by the clinical pharmacist. Once the changes were outlined in paper, the technician would make the physical changes to the cabinet as directed.
Prior to the optimization intervention, the reports obtained contained a snapshot of the current inventory of noncontrolled medications stocked on each ADC. Based on this inventory snapshot, the total cost on each ADC was calculated. The reports of the 2-month preintervention time period also showed the number of low-quantity and zero-quantity (stock out) days for each medication on the ADCs. This provided direction for medications that required an increase in the par level maintained on the ADC. Moreover, the reports provided information on medications that had lower utilization and few stock outs or low-quantity days, in which decreasing par levels or removing from the ADC would decrease the overall cost on the cabinet.
The clinical pharmacist reviewed the reports and made several decisions to optimize the cabinets. Several multi-unit of use medications, such as inhalers and topical products, were removed, as they typically were higher cost items and do not require daily dispensing. The pharmacist also evaluated stocked items that are available in multiple strengths, and streamlined the available inventory for these products. For example, levothyroxine tablets come in multiple dosage strengths. By taking advantage of using half-tablet increments or multiple tablets to make up patient-specific doses, only 25 µg, 100 µg, and 88 µg doses were left stocked on the cabinet to cover a high percentage of potential doses rather than having every possible dosage strength stocked on the ADC. The focus on utilizing minimum and maximum dosage strengths to cover all possible doses makes it possible to add other medications to the cabinet to achieve optimization.
Another avenue of utilization on ADCs is to take into account drawers with varying pocket size and number to accommodate different sizes and amounts of medications to be stocked. The pharmacist reviewed the reports for administration frequencies to determine what medications could have a decreased maximum par level, based on usage. After reducing the maximum par, some items were able to be moved to smaller pocket and drawer locations, opening up space for larger pockets to hold bulkier items, such as epidural cassettes and liquid formulations dispensed in unit-dosed cups.
Reports for all patient-specific medications dispensed from our centralized pharmacy were obtained during this stewardship project. These reports evaluated trends in any items repeatedly sent that could be stocked on the ADC. Items specifically targeted for addition were low cost and had long expiration dating.
Based on the aforementioned data collected in the requested reports, the stewardship pharmacist made additions, deletions, and par adjustments on the ADCs in an effort to decrease overall cost on the ADCs and decrease the volume of centrally dispensed patient-specific medications. The same data as previously mentioned were collected and analyzed during the 2-month postoptimization period, after the 2-week washout period. The inventory cost on the ADCs, number of low-quantity days and stock outs, and the volume of patient-specific medications dispensed from the centralized pharmacy were compared against the data collected prior to the optimization.
Results
When comparing the separate 2-month time periods, post–inventory optimization cost on the ADCs was reduced from $11963.05 to $6562.79, which represents a 45% reduction in costs on cabinets. Total cabinet inventory was increased by 8% from 526 items to 567 items, through optimization. These results followed the removal of 52 items, 42 multiple strength deletions, as well as the addition of 104 items. The total number of patient-specific medication units dispensed over a 2-month period from the central pharmacy decreased from 6489 to 4408 units, a 32% decrease after the inventory optimization. The number of medication stock outs increased from 1.52 items per day to 1.56 items per day over this same period.
Discussion
Several governing bodies disclose general recommendations for cabinet deployment; however, a practical and stepwise approach to maintaining a population-specific optimized ADC inventory is not well described in the literature.1,3 What makes our analysis distinctively different is the development of an ADC stewardship program under the direction of a clinical pharmacist. Making changes to ADCs can affect both the patients they support as well as the nursing staff that utilize them; therefore, it is vital that all changes to those cabinets be managed by the unit-specific clinical pharmacist servicing the area.
The Institute for Safe Medication Practices provides specific guidelines and recommendations on the maintenance of ADC inventory, specifically stating routine review of prescribing patterns and inventory utilization should guide inventory adjustments on ADCs.1 However, these guidelines favor a Pharmacy and Therapeutics committee or other medication safety committee being responsible for the evaluation and adjustments of ADC inventory. Rather than a committee or operational staff member, we deployed a clinical pharmacist to lead the ADC stewardship group. The clinical pharmacist was able to tailor the ADC inventory adjustments to the direct needs of the patients being cared for in their assigned patient care areas. This collaboration of a clinical pharmacist with operational personnel streamlined the implementation of changes needed to optimize the unit-specific ADCs.
Through this pharmacist-driven ADC inventory optimization stewardship program, the total inventory was increased on the ADCs, limiting the volume of centrally dispensed patient-specific medications. While not measured directly in our study, it has been shown previously that the availability of medications on ADCs may result in fewer delays in medication administration and an increase in on-time administration of scheduled medications.4
Although the absolute total cabinet inventory increased by only 8%, the true inventory turnover was 35% when taking into account the removal and addition of items. By targeting the removal of high-cost bulk or rare use items the total cabinet cost dropped significantly. Also, the additional removal of items with multiple strengths allowed our group to add numerous low-cost generic medications to the ADC that would have otherwise been dispensed from the central pharmacy as a patient-specific medication. Since our medication charge model is on distribution rather than at patient administration, having more medications being dispensed from unit ADCs may reduce the possibility in credit errors, credit losses, and waste of pharmacy technician time allocation. By reducing the quantity of patient-specific medication labels being printed, the multistep process of getting a medication from central pharmacy to patient would be eliminated.
Par levels adjustments on medications that were either in excess or had low usage was a significant driver in the reduction of cabinet inventory costs. Decreasing maximum par levels on ADCs has the ability to prevent multifold overdosing medication errors.1 That being said, one concern with a reduction in par levels is the potential for increased medication stock outs. Our results determine that a well-planned and thorough par level adjustment does not affect stock out and does not negatively affect patient care.
One limitation with our analysis was that it was designed to measure data over the course of 2 separate 2-month periods before and after the ADC optimization. With that, there are some concerns regarding sustainability of results. Our study did not address the necessary frequency for regular surveillance and monitoring after the optimization. Furthermore, it must be recognized that organizing and implementing ADC optimization could have a large impact on time and personnel resources if expanded outside of the limited studied patient care area. Additionally, as this was a pilot analysis, our results may not be reproducible in other or more patient care areas, in patient care areas that use different types of medications or care for a less medically diverse patient population, or in institutions that have a lesser amount of ADCs.
Conclusion
Automated dispensing cabinet inventory optimization by the bedside clinical pharmacist at a tertiary academic medical center decreased the overall cabinet cost while increasing medication inventory. This resulted in increased efficiency and a decrease in patient-specific medication units being dispensed from a centralized pharmacy.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Institute for Safe Medication Practices. Guidance on the interdisciplinary safe use of automated dispensing cabinets. http://www.ismp.org/tools/guidelines/ADC_Guidelines_final.pdf. Published 2008. Accessed March 13, 2014.
- 2. Guerrero RM, Nickman NA, Jorgenson JA. Work activities before and after implementation of an automated dispensing system. Am J Health Syst Pharm. 1996;53:548-554. [DOI] [PubMed] [Google Scholar]
- 3. American Society of Health-System Pharmacists. ASHP guidelines on the safe use of automated dispensing devices. Am J Health Syst Pharm. 2010;67:483-490. [DOI] [PubMed] [Google Scholar]
- 4. Shirley KL. Effect of an automated dispensing system on medication administration time. Am J Health Syst Pharm. 1999;56:1542-1545. [DOI] [PubMed] [Google Scholar]